Abstract
Background:
To study the clinical profile and co-morbidity in Indian children with attention-deficit/hyperactivity disorder (ADHD).
Materials and Methods:
A prospective analytical study of 2 years duration at the Child Guidance Clinic of a pediatric tertiary care hospital in a south Indian city using Diagnostic and statistical manual of Mental Disorders-1V based questionnaires.
Results:
Of the 251 referrals, 51 (20.3%) children met the inclusion criteria for the diagnosis of ADHD. M:F ratio was 6.3:1. The mean age was 5.7 years. A majority of the children belonged to middle and lower socio-economic class and were first-born children. Most children were brought up in nuclear families. History of delayed speech and language development was commonly seen in these children. Combined type of ADHD was the most common type. At least one co-morbid diagnosis was seen in 86.3% of children, and learning disability was the most common co-morbid diagnosis. The mean IQ was 90 (SD±12).
Conclusion:
Early markers of cognitive dysfunction like delayed speech, language and social and adaptive development may be a pointer towards the diagnosis of ADHD in children. Knowledge about their sociodemographic profile and other co-morbid conditions that are associated with ADHD is necessary to fully understand the magnitude of the problem and to plan effective therapy for them.
Keywords: Attention-deficit/hyperactivity disorder, children, co-morbidity, risk factors
INTRODUCTION
Attention-deficit/hyperactivity disorder (ADHD) is a common neurobehavioral disorder affecting children causing significant limitations in functioning across different settings. The affected children exhibit varied behavioral patterns depending on the type of ADHD, co-morbidities, and the type of care they receive. The parents of these children also face varying degrees of stress and disharmony at home. The objective of this study is to analyze the clinical profile, socio-demographic, and neuropsychological factors, and co-morbidity in children with ADHD referred to the child guidance clinic of a tertiary care hospital in South India.
MATERIALS AND METHODS
A prospective analytical study of 2 years duration conducted at the child guidance clinic of a pediatric tertiary care hospital in a South Indian city. All children diagnosed as ADHD based on the Diagnostic and statistical manual of Mental Disorders-1V (DSM-1V) text revision (TR) criteria using the modified swanson, nolan and pelham (SNAP) IV rating scale. Children who satisfy DSM IV criteria,[1] but found to have mental retardation based on tested intelligence quotient (IQ), children with gross neurological abnormalities, visual and hearing loss, epilepsy, autism, and other pervasive developmental disorders were excluded from the study. Children with features of ADHD in the referral population for a period of at least 6 months were enrolled and subjected to a detailed and structured interview, using a structured, pretested questionnaire, focusing on antenatal risk factors, delivery details, postnatal risk factors, child's behavior during early infancy and childhood, developmental history, history suggestive of co-morbid disorders, type of family, socio-economic status, based on the revised Kuppuswamy Scale,[2] parental habits, psychiatric illness in family and history of ADHD in parents, siblings, or relatives. After a thorough history, a detailed examination was carried out, with particular attention to dysmorphology examination, neurological examination, and soft neurological signs. An interview related to common co-morbid disorder was then conducted based on initial history using structured questionnaires based on DSM IV TR criteria in conjunction with a pediatric psychiatrist. Then the children were administered the modified SNAP IV rating scales[3] with advice to parents to fill the forms in conjunction with the school teacher, to avoid discrepancy, if he/she was a school going child, otherwise on their own. In that case we compared our screening reports with that of parent questionnaire and any discrepancy that could arise were sorted out after discussing them with the parents. The SNAP IV scale was modified in our study by omitting the questions pertaining to oppositional defiant disorder (ODD), since we did a separate interview for the co-morbidity of ODD.
The parents and teachers were asked to rate the symptoms (9 for inattention and 9 for hyperactivity and impulsivity) as (1) not at all - 0 points,(2) just a little - 1 point, (3) quite a bit - 2 points, (4) very much - 3 points. The total number of points acquired in each group was divided by 9 to find out the average rating per item. This average rate was compared with the 95th percentile for that symptom, if the values in both groups were more than 95th percentile; they were included under the combined group. During the next visit, the parents were reviewed back with the SNAP IV reports. They were then subjected to detailed neuropsychometric testing, using scales appropriate to the age and development of the child. They were also screened for learning disability (LD) with self-administered tests which were appropriate for age and educational level. The LD was classified based on DSM IV as reading, writing, or mathematical disorder. A diagnosis of developmental coordination disorder (DCD) was considered, if there was history of clumsiness or hypotonia in the child and motor developmental delay substantially less for the measured intelligence of the child. The results were then tabulated and analyzed Using SPSS (Statistical Package for Social Sciences) for windows version 11 (SPSS, Inc., Chicago, IL.).
RESULTS
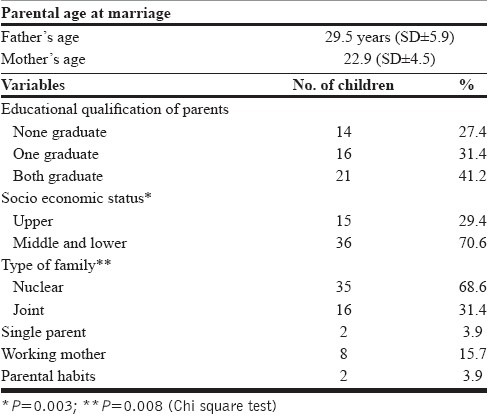
During the study period between May 2002 and April 2004, 251 children were registered in our Child Guidance Clinic. Among them, 51 children met the inclusion criteria for diagnosis of ADHD. Of the diagnosed children, 19.6% were less than 3 years, 35.3% of children were between 3 and 5 years of age, 41% were between 5 and 9 years of age and 12% were above 9 years of age. The mean age for boys was 5.8 years (SD±2.9). The mean age for girls was 4.9 years (SD±1.9). Out of the 51 children with ADHD, 44 (86.3%) were boys and 7 (13.7%) were girls with a ratio of 6.3:1 with a statistically significant distribution P<0.001. The sociodemographic characteristics of the study population are given in [Table 1]. Six (21.6%) children with ADHD had parents with symptoms suggestive of ADHD in their childhood. Three (5.9%) children with ADHD had a sibling history of ADHD. Five (9.8%) children with ADHD had a close relative with ADHD. Eleven (21.6%) children were born out of consanguineous marriage. Thirty (58.8%) children were first born in sib ship. Nine (17.6%) children were delivered prematurely and had low birth weight (LBW). Sixteen (31.4%) children had one or more antenatal risk factors. These observations were not statistically significant. In our study, we also found that 10 (19.6%) children had history of excessive crying or irritability during infancy, 5 (9.8%) children had sustained head injury with brief loss of consciousness without seizures or neurological deficits and 9 (17.6%) children were very much interested in watching television commercials.
Table 1.
Socio demographic characteristics
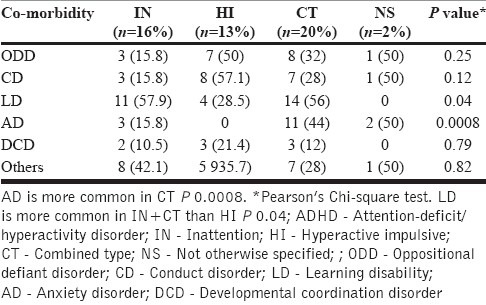
Thirty-two (62.7%) children had history of delayed attainment of one or more milestones. Delayed attainment of language milestones was the most common and was seen in 30 (58.8%) children. Isolated language delay was seen in 17 (33.3%) children. Only 1 (1.9%) child had delayed development of all four milestones. Fine motor and adaptive social skills were significantly delayed in children belonging to (hyperactivity and impulsive (HI) type of ADHD (P=0.0002 and P=0.003, respectively). Eighteen (60%) children with language delay were less than 5 years of age (P=0.03) [Table 2]. The most common type of ADHD in our study was combined type (CT) of ADHD and was seen in 20 (40%) children [Table 3]. Sixteen (31%) children had In attentive (IA) type of ADHD. HI type was seen in 13 (25%) children. In 2 (4%) children, the symptoms were sub-threshold and they were categorized under not otherwise specified (NS) type of ADHD. IA was the most common type among girls 4 (57.1%), whereas CT was the most common type among boys 18 (40.9%). HI was more common in children <5 years of age being present in 10 (41.7%) children. CT was more common in children between 5 and 9 years of age [Table 4]. Forty four (86.3%) children had one or more co-morbid conditions in our study [Table 5]. The most common co-morbid disorder was LD features of which was seen in 29 (56.9%) of children. Nineteen (37.3%) children had features of ODD and conduct disorder (CD) each. ODD was more common in boys 18 (41%) as against 1 (19%) in girls which was statistically significant (P<0.05). ODD and CD were more common in HI. LD was more common in IA and CT and less common in HI [Table 6]. Features of anxiety disorder (AD) were seen in 16 (31.4%) children. There was no significant difference between the sexes. DCD was seen in 8 (15.7%) children. 4 (50%) children had either gross or fine motor delay and 4 (50%) children had soft neurological signs. Twenty-one (41.2%) children had other behavioral problems including 17 (33.3%) nocturnal enuresis. In our study, the mean IQ was 90 (SD±12) with range 71-117. IQ for children <5 years was 87 (SD±11), for children 5-9 years was 92 (SD±14), and for >9 years was 92 (SD±5). The mean IQ for children with IA was 91 (SD±14) for HI 85 (SD±10) and for CT was 91 (SD±11). Children with developmental delay had lower IQ than children without development delay. Similarly, there was no significant IQ difference between LD and other co-morbid disorders.
Table 2.
Developmental delay in different age groups
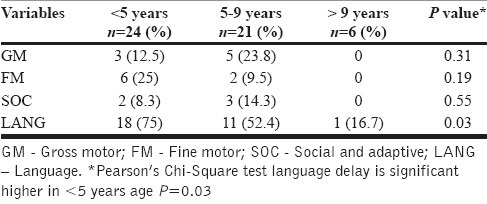
Table 3.
Type of ADHD
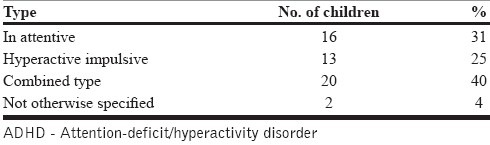
Table 4.
Type of ADHD in different age groups
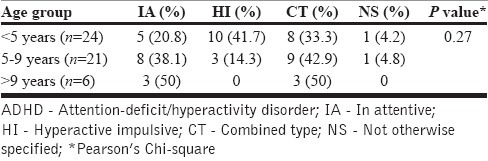
Table 5.
Co-morbidity in relation to age
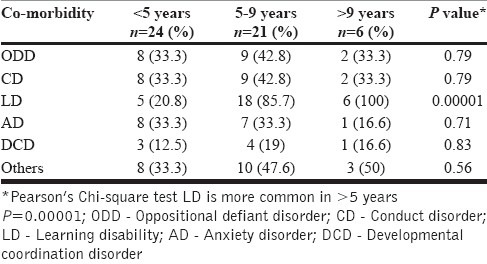
Table 6.
Co-morbidity in different types of ADHD
DISCUSSION
Our study differs from the other Indian studies[4–6] with respect to inclusion of young children. One fifth of the children with ADHD in our study belonged to less than 3 years of age which shows that ADHD is widely prevalent even in preschool children and toddlers. Similar observations have been made by Palfrey and co-authors[7] in their prospective longitudinal study in which 13% of children aged 14 to 29 months had definite features suggesting the possibility of ADHD. Preschool children with developmental delay or attention deficit disorder or both have high risk of symptoms continuity.[8,9] Possible reasons for the increased number of preschool children in our study may be due to hyperactivity rather than in attention in these children which could have forced their parents to get an early consultation. It could also represent the mother's knowledge on child rearing which can be a key factor in early identification. These children need to be followed up to look into persistence of symptoms in their mid childhood and adolescence. From our study we find that ADHD in boys is considerably higher than girls. Similar results were seen in other Indian studies.[4,6,10] In our study, we find that educational qualification of parents and age of parents are not significant risk factors for ADHD. Similar observations have been reported in a Turkish study,[11] according to which there was no co-relation between ADHD, parental age, or profession.
Indian studies[6,7] also quote that ADHD is highly prevalent in lower and middle socio-economic class. We also find that though children with ADHD frequently belonged to middle and lower socio-economic class; the significance was not maintained when individual social classes were taken for risk factor analysis. Behavioral problems have been reported to be high in Indian children belonging to nuclear families.[12] Similarly, in our study too we found ADHD to be more common in children belonging to nuclear families. In a nuclear family, a child can be affected by anxiety and tension between parents which can result in increased behavioral problems in them. The number of children with single parent, parental substance abuse, and psychiatric illness in family were not significantly high in children with ADHD in our study in comparison to community samples from west.[13] This needs to be analyzed in population-based studies as our study group may not be representative of the society. There was no significant association between type of ADHD and socio-economic class, prematurity, or perinatal adversity in our study. Similarly, the Kolkata study[4] study did not find increased incidence of ADHD in LBW children and studies by Godman and co-authors[14] also have not found significant perinatal risk factors contributing to ADHD. Persistent crying in infancy, traumatic brain injury, and excessive television viewing have been postulated as risk factors for development of ADHD by a few studies.[15–17] However, in our study we did not find any significant association between any of those risk factors and ADHD.
Regarding developmental profile of children with ADHD, observations similar to our study have been reported by others as well.[4,11] The most common co-morbid disorder in our study was LD. This is in concordance with the wide variability in the reported degree of overlap between LD and ADHD ranging from 10% to 92% in literature.[18] LD was more common in IA and CT similar to the Chandigarh study.[6] Less number of children in the age group of less than 5 years and with HI has LD and this was statistically significant. Regarding the prevalence of other co-morbidities, our findings correlate with other studies.[19–21] Behavioral problems were seen in 41.2% of the children in comparison to 60% behavioral problems in the Chandigarh study.[6] These manifestations are seen as an expression of underlying emotional problems due to frustration and failure these children experience. In our study, nocturnal enuresis was more common than reported by the Kolkata study.[4] Studies by Robson and co-authors[22] have shown that children with ADHD at age 6 were 2.7 times more likely than controls to have nocturnal enuresis. Children with developmental delay had lower IQ than children without development delay and there was no significant IQ difference between LD and other co-morbid disorders with that of types of ADHD similar to the Turkish study.[11]
CONCLUSION
ADHD is a highly prevalent neurobehavioral disorder in children with marked heterogeneity in clinical presentation. No specific etiologic factor was found to be significantly associated with this disorder. Speech and language delay especially in preschool children with normal hearing may be a pointer toward ADHD. There is a high incidence of learning disability with other co-morbid mental health problems in these children which may have a negative influence on their behavior. Identification of these co-morbidities would help in planning effective and comprehensive treatment strategies for them.
ACKNOWLEDGMENT
The authors would like to acknowledge with gratitude, the services of late Dr. S. Viswanathan who helped with psychiatric interview and assesement of co-morbidities.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Diagnostic and statistical manual of mental disorders. 4th edition. Washington, DC: American Psychiatric Association; 2000. American Psychiatric Association. text revision. [Google Scholar]
- 2.Mishra D, Singh HP. Kuppuswamy's socio economic status scale: A revision. Indian J Pediatr. 2003;70:273–4. doi: 10.1007/BF02725598. [DOI] [PubMed] [Google Scholar]
- 3.Swanson J, Learner M, March J, Gresham FM. Assesement and intervention for attention-deficit/hyperactivity disorder in the schools: Lessons from the MTA study. Pediatr Clin N Am. 1999;46:993–1009. doi: 10.1016/s0031-3955(05)70168-1. [DOI] [PubMed] [Google Scholar]
- 4.Mukhopadhyay M, Misra S, Misra T, Niyogi P. Attention deficit hyperactivity disorder. Indian J Pediatr. 2003;70:789–92. doi: 10.1007/BF02723796. [DOI] [PubMed] [Google Scholar]
- 5.Bhatia MS, Choudhary S, Sidana A. Attention deficit hyperactivity disorder among psychiatric out patients. Indian Pediatr. 1999;36:583–7. [PubMed] [Google Scholar]
- 6.Malhi P, Singhi P. Spectrum of attention deficit hyperactivity disorders in children among referrals to psychology services. Indian Pediatr. 2000;37:1256–60. [PubMed] [Google Scholar]
- 7.Palfrey JS, Levine MD, Walker DK, Sullivan M. The emergence of attention deficits in early childhood: A prospective study. J Dev Behav Pediatr. 1985;6:339–48. [PubMed] [Google Scholar]
- 8.Beitchman JH, Wekerle C, Hood J. Diagnostic continuity from preschool to middle childhood. J Am Acad Child Adolesc Psychiatry. 1987;26:694–9. doi: 10.1097/00004583-198709000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Blackman JA. Attention - Deficit/Hyperactivity disorder in preschoolers. Does it exist and should we treat it? Pediatr Clin N Am. 1999;46:1011–25. doi: 10.1016/s0031-3955(05)70169-3. [DOI] [PubMed] [Google Scholar]
- 10.Bhatia MS, Nigam VR, Bohra N, Malik SC. Attention deficit disorder with hyperactivity among pediatric out patients. J Child Psychol Psychiatry. 1991;32:297–306. doi: 10.1111/j.1469-7610.1991.tb00308.x. [DOI] [PubMed] [Google Scholar]
- 11.Gross - Tsur V, Shaler RS, Amir N. Attention deficit disorder: Association with familial - genetic factors. Pediatr Neurol. 1991;7:258–61. doi: 10.1016/0887-8994(91)90041-i. [DOI] [PubMed] [Google Scholar]
- 12.Verghese A, Beig A, Senseman LA, Rao SS Sunder, Benjamin V. A social and Psychiatric study of a representative group of families in vellore town. Indian J Med Res. 1973;61:608–19. [PubMed] [Google Scholar]
- 13.Scahill L, Schwab-stone M, Merikangas KR, Leckman JF, Zhang H, Kasl S. Psychosocial and clinical correlates of ADHD in a community sample of school - age children. J Am Acad Child Adolesc psychiatry. 1999;38:976–84. doi: 10.1097/00004583-199908000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Godman R, Stevenson J. A twin study of hyperactivity - II. The etiological role of genes, family relationships and perinatal adversity J. Child Psychol Psychiatry. 1989;30:691–709. doi: 10.1111/j.1469-7610.1989.tb00782.x. [DOI] [PubMed] [Google Scholar]
- 15.Wolke D, Rizzo P, Woods S. Persistent infant crying and hyperactivity problems in middle childhood. Pediatrics. 2002;109:1054–60. doi: 10.1542/peds.109.6.1054. [DOI] [PubMed] [Google Scholar]
- 16.Max JE, Lansing AE, Koele SL, Castillo CS, Bokura H, Schachar R, et al. Attentiondeficit hyperactivity disorder in children and adolescents following traumatic brain injury. Dev Neuropsychol. 2004;25:159–77. doi: 10.1080/87565641.2004.9651926. [DOI] [PubMed] [Google Scholar]
- 17.Biedermen J, Milberger S, Faraone SV, Kiely K, Guite J, Mick E, et al. Family - environment risk factors for attention - deficit hyperactivity disorder. A test of Rutter's indicators of adversity. Arch General Psychiatry. 1995;52:464–70. doi: 10.1001/archpsyc.1995.03950180050007. [DOI] [PubMed] [Google Scholar]
- 18.Semrud - Clikeman MS, Biederman J, Sprich-Buckminster S, Lehman BK, Faraone SV, Norman D. Co-morbidity between ADDH and learning disability: A review and report in a clinically referred sample. J Am Acad Child Adolesc Psychiatry. 1992;31:439–48. doi: 10.1097/00004583-199205000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Biederman J, Newcorn J, Sprich S. Co-morbidity of attention deficit hyperactivity disorder with conduct, depression, anxiety and other disorders. Am J Psychiatry. 1991;148:564–77. doi: 10.1176/ajp.148.5.564. [DOI] [PubMed] [Google Scholar]
- 20.Newcorn JH, Halperin JM, Jensen PS, Abikoff HB, Arnold E, Cantwell DP. Symptom profiles in children with ADHD: Effects of co-morbidity and gender. J Am Acad Child Adolesc Psychiatry. 2001;40:137–46. doi: 10.1097/00004583-200102000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Jensen P, Shervette RE, 3rd, Xenakis SN, Richters J. Anxiety and depressive disorder in attention deficit disorder with hyperactivity: New findings. Am J Psychiatry. 1993;150:1203–9. doi: 10.1176/ajp.150.8.1203. [DOI] [PubMed] [Google Scholar]
- 22.Robson WL, Jackson HP, Blackhurst D, Leung AK. Enuresis in children with attention - deficit hyperactivity disorder. South Med J. 1997;90:503–5. doi: 10.1097/00007611-199705000-00007. [DOI] [PubMed] [Google Scholar]


