Abstract
Background:
The phenomenon of population ageing is already a major social and health problem in the developed countries. The elderly have their problems of disease and disability due the increasing age and changing social circumstances and the need for social support forms an important aspect of geriatric healthcare.
Aim:
To comparatively study the prevalence and pattern of psychiatric disorders in geriatric population in old age homes with those living with the families; and its association with the sociodemographic variables.
Materials and Methods:
Brief Psychiatric Rating Scale was used to screen the study population for psychotic and non-psychotic symptoms. Mini Mental Status Examination was used to assess the cognitive decline and the Psychiatric diagnosis was made according to International classification of diseases 10th Revision Diagnostic criteria. SPSS-16 was used for statistical analysis.
Results:
Psychiatric disorders were more prevalent in individuals aged >80 years, in females, and illiterates. Mood disorders were the most common Psychiatric disorders. Individuals in old age homes had less prevalence of Psychiatric illness than those living in the community.
Conclusion:
The overall prevalence of Psychiatric disorders was less in the geriatric population in old age homes because of the better availability of care, being engaged in regular activities as per the schedule, group works, etc. This study reflects the importance of delivery of care for better life in geriatric population.
Keywords: Community, geriatric population, old age home, psychiatric morbidity
INTRODUCTION
The geriatric population is defined as population aged 60 years and above.[1] People aged 60 years and over are expected to constitute 10.2% of the total world population by 2025.[2] The phenomenon of population ageing (defined as increase in the median age of the population)[3] is already a major social and health problem in the developed countries. The life expectancy of an average Indian has increased from 54 years in 1981 to 64.6 years in 2002.[4] According to Sharma,[5] the population of people aged 60 years or above is likely to increase to 18.4% of the total population in India by the year 2025.
Improved healthcare promises longevity but social and economic conditions, such as poverty, break up of joint families, and poor services to the elderly, pose a psychiatric threat to them.[6] The feeling of loneliness along with the natural age-related decline in the physical and physiological functioning make the elderly more prone to psychological disturbances.[7] Functional dependency is common among elderly people and many would need assistance in their activities of daily living. Long-term care has become one of the major problems facing an aging society.[8]
In a western study, Bruce et al.[9] found that 13.5% of newly admitted elderly home care patients suffered from major depression. Ritchie et al.[10] found a lifetime prevalence of 26.5% and 30% of major depression and anxiety disorders, respectively, in geropsychiatric patients. Seby et al.,[11] in a study, found that 26.7% of the urban geriatric population suffers from psychiatric illness. Tiwari and Srivastava[12] conducted a study in rural population in Uttar Pradesh and found the prevalence of Psychiatric disorders to be more in geriatric age group (42.21%) when compared with the non-geriatric population (3.97%), depression and the anxiety disorders being the most common. In a comparative study by Tiple et al.,[13] between the people living in old age homes and community, those persons living in old age home perceived a better supportive care than those living with the families.
Most of the elderly people with depression remain undiagnosed and untreated due to the lack of adequate knowledge of these disorders in the public and as these symptoms are considered to be a part of normal ageing.[14] The lack of priority accorded to the healthcare needs of the elderly seems to perpetuate the low level of public awareness about mental health problems of old age. The family is the major provider for long-term care in the elderly, especially in developing country like India, where institutional care is difficult to avail and costly.[15] But, with the changing trend of preference for Nuclear families in India, the population living in old age homes is on rise. The studies done to evaluate the psychiatric illness among the population staying in old age homes are limited. Therefore, with this background, the present study is carried out to explore the psychiatric morbidity in elderly population in old age home and General population living in community.
Aim
To study
The association of the sociodemographic variables and psychiatric disorders in the study population
The prevalence and pattern of psychiatric disorders in geriatric population in old age homes compared with those living in community.
MATERIALS AND METHODS
The study is conducted on a total of 120 geriatric people, among which 60 people are living in old age homes and 60 people from the general population. People from three old age homes in Khammam town are included in the study.
The common reasons for the people staying in old age homes were lack of caregiver, financial problems. The general population included those people who are living with their families residing in Khammam urban region. Khammam is the head quarters of Khammam district in Andhra Pradesh, with a population of nearly two and a half lakhs.
This is a cross-sectional study, conducted for a period of one month from June 1 to June 30, 2011.
The purpose of the study was explained and informed verbal consent was taken from both the person and the caregiver. Each person is assessed using a semi-structured proforma which consists of all the sociodemographic details. Brief Psychiatric Rating Scale (BPRS) was used to measure major psychotic and non-psychotic symptoms in individuals and Mini Mental Status Examination (MMSE) is used to screen the patients with cognitive decline. Those individuals with MMSE scores <23 are further assessed for Dementia. The psychiatric diagnosis is made according to International Classification of Diseases 10th Revision (ICD –10) diagnostic criteria which is first evaluated by a senior resident and later confirmed by consultant Psychiatrist. The statistical analysis of the data is done using SPSS-16.
Tools used
Semi-structured proforma for sociodemographic profile
ICD-10 diagnostic criteria
BPRS. It was developed by JE Overall and DR Gorham to measure the major psychotic and non-psychotic symptoms. It consists of 18 items, rated on a 7-point scale. The ratings are based on both the subjective and objective analysis of the symptoms.
MMSE (developed by The Indo-US Cross National Dementia Epidemiology study) with a maximum score of 30. Those with scores less than 23 are supposed to have mild cognitive decline and should be assessed further.
Inclusion criteria
Age >60 years
Physically fit to answer the questions.
Exclusion criteria
People not giving consent
Those who do not have caregivers.
RESULTS
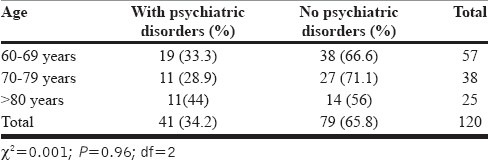
In our study, the population in the age group of >80 years have more prevalence of Psychiatric disorders (44%), followed by those who are in the age groups of 60 to 69 years (33.3%) and 70 to 79 years (28.9%).
Of 53 males, 18 (33.9%) had psychiatric disorder and of 67 females, 23 (34.3%) were suffering from psychiatric illness.
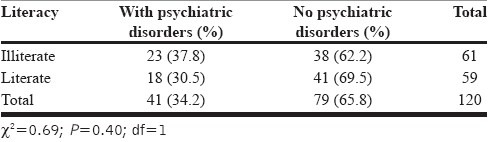
Psychiatric disorders were more prevalent in illiterate population (37.8%), when compared with the literate people (30.5%).
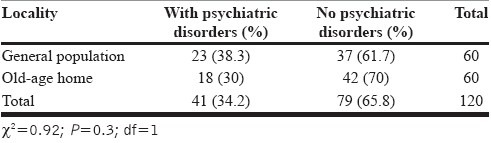
The prevalence of psychiatric illnesses was more among the individuals living in the community (38.3%) than in the people living in old age homes (30%).
Depression was the most common psychiatric disorder in the general population (21.7%) and also in those living in old age homes (25%), followed by anxiety disorders (mean, 5.8%), substance use-related disorders (mean, 4.2%), and organic disorders (mean, 0.9%). Dementia was the only organic disorder and alcohol dependence was the only substance use disorder that was found in our study. 37 (61.7%) of general population and 42 (70%) of the individuals in old age home had no psychiatric illness.
DISCUSSION
For the present study, 63 individuals from community and 64 individuals from old age home were consulted. Totally, seven patients had to be excluded as five of them had hearing problems severe enough to be unable to participate in the study and two of them had no reliable caregiver. Finally, 60 individuals each from old age home and community are included.
In our study, [Table 1] most of the study sample was in the age group of 60 to 69 years, followed by the age groups of 70 to 79 years and >80 years. This could be due to the fact that there will be a gradual decline in the number of persons surviving with increasing age (life expectancy - 64.6 in India, according to 2002). This is in accordance with the study by Seby et al. in which the youngest age group accounted for high sample size, with decreasing number of people with advancing age.[11] The prevalence of psychiatric disorders was more in the population belonging to the age group of >80 years (44%) than those from the age group of 60 to 69 years (33.3%) and 70 to 79 years (28.9%). This finding is in accordance with a study by Singh et al.[16] in which he found that there is no gradual increase of psychiatric morbidity with age in geriatric people. Nandi et al.,[17] in a rural study, found that there is an increase in the prevalence of psychiatric morbidity with age in geriatric population.
Table 1.
Age and psychiatric disorders
The prevalence of psychiatric morbidity in females (34.3%) is little more when compared with males (33.9%) [Table 2]. This finding could be because of the family burden and responsibilities and discriminatory access to health services in females (P>0.05) which would be contributing to increased perception of stress in them. Murphy[18] found that 48% of the patients in hospital setting and 68% of the depression subjects in community had experienced severe stressful event in the preceding year of onset of depressive symptoms. A community study done by Premarajan et al.[19] in urban population also found the higher prevalence of psychiatric illnesses in females than in males. Copeland et al.,[20] in a western community study, and Jain and Aras,[21] in a study conducted in north India also found that females have high prevalence of psychiatric illnesses than males at any age.
Table 2.
Gender and psychiatric disorders
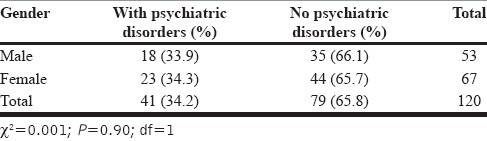
Table 3 shows that the psychiatric disorders are more prevalent in illiterates (37.8%) than in the literate population (30.5%). This could be due to the better comprehension of the illness by the literate people and earlier consultant seeking attitude by them. In India, illiterates may also seek help from other traditional methods which would result in the poor outcome of the disorder with prolonged period of suffering. This finding of increased prevalence of psychiatric illness in illiterates is in accordance with the study in urban population by Seby et al.[11]
Table 3.
Literacy and psychiatric disorders
Psychiatric illness is found to be more prevalent among the population living in the general population than among those from old age homes (P=0.3) [Table 4]. The findings were in accordance with those reported by Tiple et al.[13] in a comparative study, in which the people living in old age home perceived a better supportive care than those living with their families. The changing family circumstances, attitude of the family members to take up the additional burden of elderly people with declining functional levels, and lack of the people with whom they can share their thoughts and emotions could be the probable reasons for the increased prevalence of psychiatric illness in the people living with the families.
Table 4.
Locality and psychiatric disorders
The overall prevalence of psychiatric disorders was found to be 34.2%, which is within the range of prevalence (32.2% - 43.3%) found in other Indian studies.[12,22] Among the psychiatric illnesses, mood disorders were the most prevalent in our study. There were no patients with Bipolar Affective Disorder or Mania and all the patients in the category of mood disorders were diagnosed to have Mild or Moderate Depression. 25% of the people at old age homes and 21.7% of geriatric general population had depression [Table 5]. This higher prevalence of depression in old age home individuals could be due to the loss of spouse in all of them, which is an important stressful factor. The community sample in our study included the people with and without spouse. Multiple stressful factors like loss of physical vigor, occupation, and death of spouse in old age would lead to disturbance in the psychic equilibrium, producing mal-adaptive patterns of adjustment including physical and mental disorders, especially depression.[23] This finding is similar to the study done by Barua and Kar,[24] in rural areas in south India, in which the prevalence of depression was found to be 21.7%.
Table 5.
Pattern of psychiatric disorders
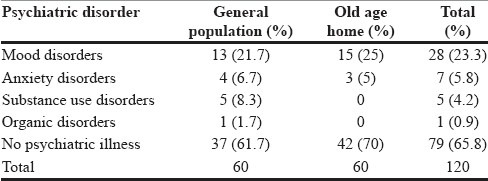
Among the patients who had anxiety disorders in our study, all of them had Generalized Anxiety disorder (5.8%). There were no subjects with Obsessive Compulsive disorders, phobias, and dissociative disorders. Factors related with aging such as social isolation, financial insecurity poor health, and impending death might be expected to increase the prevalence of anxiety in late life. This is in consonance to the finding by Ritchie et al.[10] in a study conducted in French population (4.6% had Generalized Anxiety Disorder).
Alcohol dependence syndrome was present in five people (4.2%). We found that nine individuals have the habit of taking alcohol (15%), but four of them did not meet the criteria for any other disorder of alcohol use. Surprisingly, among all the individuals who were taking alcohol, none of them had any other comorbid psychiatric illness. All of them were males from the general population. This is in concordance with a study by Goswami et al.,[25] in rural population, in which about 16.3% of males were taking alcohol regularly. Among the substance use-related disorders other than alcohol, six individuals were smokers, but none had harmful use or dependence and all of them were from community sample. Three of them were taking alcohol and also had the habit of smoking. No other substance use disorders were found in our study.
Among four patients who scored less than 23 in MMSE, on further evaluation, only one patient had dementia (0.9%) of Alzheimer's type. It was a male, illiterate patient from general population. This finding is not similar to the finding in a study by Seby et al.[11] in which the prevalence of dementia was 14.9%. This difference could be because of the limited size of study sample. In our study, we found no cases of Schizophrenia or Delusional disorders.
Our study came out with a few interesting findings regarding the prevalence and pattern of psychiatric disorders in individuals living in community and those in old age homes. Individuals living in old age homes were devoid of any psychoactive substance use during the study, though a few of them had the history of taking alcohol or smoking before they joined there. This is due to the disciplinary conditions imposed on the people at old age homes. The overall prevalence of psychiatric disorders was also less in them. This could be due to the better availability of care, being engaged in regular activities according to the protocol, like spiritual activities, group works, etc. This study attempted to depict the importance of delivery of care and need for support in geriatric population for their better health.
LIMITATIONS
Small study sample due to a limited time frame
Information regarding the contact with the family members is not assessed in both the groups
The two categories of the population are not matched; hence, conclusions are difficult to be derived
Perceived social support in the study population is not measured
The association of physical illness with psychiatric morbidity is not assessed
It is not a longitudinal study.
SUMMARY AND CONCLUSION
Psychiatric disorders are more prevalent in the females than in the males
People living in old age homes had less psychiatric problems than those from the general population
Mood disorders were the most prevalent psychiatric disorders, in both the groups of population, followed by Anxiety disorders. Substance use disorders were prevalent only in general population
This study emphasizes the importance of care that has to be given to the geriatric population.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Elango S. A study of health and health related social problems in the geriatric population in a rural area of Tamil Nadu. Indian J Public Health. 1998;42:7–8. [PubMed] [Google Scholar]
- 2.Bulletin of the World Health Organization. 2004;82:213–18. [PMC free article] [PubMed] [Google Scholar]
- 3.Bhende A, Kanitkar T. Principles of population studies. 6th revised ed. Mumbai: Himalaya Publishing House; 1997. pp. 137–40. [Google Scholar]
- 4.Annual report: Health plan and policy. New Delhi: Ministry of Health and Family Welfare; 2002. Ministry of Health and Family Welfare, Government of India; p. 15. [Google Scholar]
- 5.Sharma S. Ageing: An Indian experience. Souvenir of ANCIPS 94, Madras. 1994:101–5. [Google Scholar]
- 6.Venkobarao A. Geropsychiatry in Indian culture. Can J Psychiatry. 1979;25:431–6. doi: 10.1177/070674377902400510. [DOI] [PubMed] [Google Scholar]
- 7.Ghosh AB. Psychiatry in India: Need to focus on geriatric Psychiatry. Indian J Psychiatry. 2006;48:4–9. doi: 10.4103/0019-5545.31612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pereira YD, Estibeiro A, Dhume R, Fernandez J. Geriatric patients attending tertiary care Psychiatric hospital. Indian J Psychiatry. 2002;44:326–31. [PMC free article] [PubMed] [Google Scholar]
- 9.Bruce ML, McAvay GJ, Raue PJ, Brown EL, Meyers BS, Keohane DJ, et al. Major depression in elderly home health care patients. Am J Psychiatry. 2002;159:1367–74. doi: 10.1176/appi.ajp.159.8.1367. [DOI] [PubMed] [Google Scholar]
- 10.Ritchie K, Artero S, Beluche I, Ancelin ML, Mann A, Dupuy AM, et al. Prevalence of DSM IV psychiatric disorder in French elderly population. Br J Psychiatry. 2004;184:147–52. doi: 10.1192/bjp.184.2.147. [DOI] [PubMed] [Google Scholar]
- 11.Seby K, Chaudhury S, Chakraborty R. Prevalence of Psychiatric and physical morbidity in an urban geriatric population. Indian J Psychiatry. 2011;53:121–7. doi: 10.4103/0019-5545.82535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tiwari SC, Srvastava S. Geropsychiatric morbidity in rural Uttar Pradesh. Indian J Psychiatry. 1998;40:266–73. [PMC free article] [PubMed] [Google Scholar]
- 13.Tiple P, Sharma SN, Srivastava AS. Psychiatric morbidity in geriatric people. Indian J Psychiatry. 2006;48:88–94. doi: 10.4103/0019-5545.31596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katz IR, Alexopoules GS. Diagnosis and treatment of depression in late life N.I.H consensus statement. Am J Psychiatry. 1996;4:4. [Google Scholar]
- 15.Rao TS, Shaji KS. Demographic aging: Implications for mental health. Indian J Psychiatry. 2007;49:78–80. doi: 10.4103/0019-5545.33251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh GP, Chavan BS, Arun P, Lobraj, Sidana A. Geriatric out patients with Psychiatric illness in a teaching hospital setting- A retrospective study. Indian J Psychiatry. 2004;46:140–3. [PMC free article] [PubMed] [Google Scholar]
- 17.Nandi PS, Banerjee G, Mukherjee SP, Nandi S, Nandi DN. A study of psychiatric morbidity of elderly population of a rural community in west Bengal. Indian J Psychiatry. 1997;39:122–9. [PMC free article] [PubMed] [Google Scholar]
- 18.Murphy E. Social origins of depression in old age. Br J Psychiatry. 1982;141:135–42s. doi: 10.1192/bjp.141.2.135. [DOI] [PubMed] [Google Scholar]
- 19.Premarajan KC, Danabalan M, Chandrasekhar R, Srinivasa DK. Prevalence of Psychiatric morbidity in an urban community of Pondicherry. Indian J Psychiatry. 1993;35:99–102. [PMC free article] [PubMed] [Google Scholar]
- 20.Copeland JR, Dewey ME, Wood N, Searle R, Davidson IA, Mc William C. Prevalence of mental illness among the elderly in the community Prevalence in Liverpool using the GMSAGECAT Package. Br J Psychiatry. 1987;150:815–23. doi: 10.1192/bjp.150.6.815. [DOI] [PubMed] [Google Scholar]
- 21.Jain RK, Aras RY. Depression in Geriatric population in urban slums of Mumbai. Indian J Public Health. 2007;51:112–3. [PubMed] [Google Scholar]
- 22.Mallik AN, Chatterjee AN, Pyne PK. Health status among elderly people in urban setting. Indian J Psychiatry. 2001;43:41. [Google Scholar]
- 23.Agarwal N, Jhingan HP. Life events and depression in elderly. Indian J Psychiatry. 2002;44:34–40. [PMC free article] [PubMed] [Google Scholar]
- 24.Barua A, Kar N. Screening for depression in elderly Indian population. Indian J Psychiatry. 2010;52:150–3. doi: 10.4103/0019-5545.64595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goswami A, Reddaiah VP, Kapoor SK, Singh B, Dwivedi SN, Kumar G. Tobacco and alcohol use in rural elderly Indian population. Indian J Psychiatry. 2005;47:192–7. doi: 10.4103/0019-5545.43050. [DOI] [PMC free article] [PubMed] [Google Scholar]


