Abstract
Background & objectives:
Fluorescence in situ hybridization (FISH) is increasingly being recognized as the most accurate and predictive test for HER2/neu gene amplification and response to therapy in breast cancer. In the present study we investigated HER-2/neu gene amplification by FISH in breast carcinoma tissue specimens and compared the results with that of immunohistochemical (IHC) analysis.
Methods:
A total of 90 breast carcinoma tissue samples were used for immunohistochemical (IHC) and FISH analysis. IHC was performed by using mouse monoclonal antibody to the intracellular domain of HER-2/neu protein. Each slide was scored in a blinded fashion by two pathologists according to the manufacturer's recommended criteria. FISH analysis was performed on paraffin embedded breast tumour tissue sections. The polysomy for centromere 17 (Spec green signal) was read as green signals less than 4 as moderate polysomy, and more than 4 as highly polysomy.
Results:
Thirty of the 90 patients had negative results by IHC and FISH. Of the 28 patients with the score of 2+ by IHC, 20 were FISH positive for HER-2/neu gene amplification, three were FISH negative and five patients showed equivocal (1.8-2.2) results by FISH. These five cases were retested for IHC and FISH on different paraffin embedded tissue blocks, and all five were found positive for HER-2/neu gene amplification. Twenty five patients with the score of 3+ by IHC were FISH positive for HER-2/neu gene amplification (>2.2). Seven cases with the score of 3+ by IHC were FISH negative for HER-2/neu gene amplification (>2.2), and showed polysomy of chromosome number 17 high polysomy > 4.
Interpretation & conclusions:
Our results indicated that HER-2/neu status by FISH should be performed in all cases of breast tumour with a 2+ score by IHC. Cases demonstrating a 3+ score by IHC may be subjected to FISH to rule out polysomy of chromosome 17 which could be falsely interpreted as HER-2/neu overexpression by IHC analysis. There is also a need for establishing a clinically validated cut-off value for HER-2/neu FISH amplification against IHC which may be further compared and calibrated.
Keywords: Breast cancer, HER2/neu gene amplification, fluorescence in situ hybridization (FISH), immunohistochemistry (IHC)
Breast cancer ranks as the second most common cancer for women in India and its incidence peaks between the ages of 40 and 50 yr, with a mean age of occurrence at 47 yr1,2. Since the first report of erb-b2 as a poor prognostic factor for breast cancer in 19873, the significance of HER-2/neu oncogene as an adverse prognostic factor has been noted in many other cancers, such as ovary, lung, stomach, and pancreas3–6. Amplification of the erb-b2 gene or over-expression of the erb-b2 protein has been detected in 10 to 30 per cent of breast cancers3–13 and, together with the associated topoisomerase IIα (TOP2) gene aberrations, shows no change over time4–6 after treatment, and no difference between primary and metastatic lesions5,6.
Several techniques like immunohistochemistry (IHC) on paraffin-embedded tissues for HER-2/neu protein detection, Southern blot analysis, a reverse transcription-polymerase chain reaction (RT-PCR) technique chromogenic in situ hybridization (CISH) technique and fluorescence in situ hybridization (FISH) to quantify HER2/neu are now available. HER-2/neu testing is used as a prognostic marker to determine the aggressiveness of breast cancer tumour. Serum HER-2/neu level is sometimes evaluated to establish a baseline and if elevated, is used to monitor cancer treatment. However, this method is not widely used because HER-2/neu levels are elevated only when a large tumour is present at an advanced stage; so early cancers are likely to be negative for serum HER-2/neu. FISH is widely used for diagnosis as well as to monitor the response to therapy, such as hormone therapy and chemotherapy. In this study we investigated HER-2/neu gene amplification by FISH in breast carcinoma specimens and compared the results of FISH analysis with IHC.
Material & Methods
In this retrospective study, paraffin-embedded tissue sections of breast carcinoma from 90 consecutive female patients who had undergone surgery at the Department of Oncology between July 2008 - April 2009 and referred to the Department of Molecular Biology and Cytogenetics, Apollo Health City, Hyderabad, India, for FISH analysis were included in the study. The mean age of patients ranged between 30-50 yr (47.94 ± 13.7). The histopathological diagnosis of breast carcinoma was established by standard light-microscopic evaluation of sections stained with Hematoxylin and Eosin in each case and diagnosed as invasive ductal carcinoma grade I, II and III. Estrogen and progesterone receptor (ER, PR) status was also noted.
Immunohistochemical (IHC) analysis: IHC of HER-2/neu protein was performed on 3 to 4 μm thick paraffin embedded tissue sections placed on poly-L-Lysine coated slides. After deparaffinization and blocking of endogenous peroxidase, HER-2/neu immunostaining was performed using rabbit anti-human c-erbB-2 oncoprotein as primary antibody (Dako, Copenhagen, Denmark) at 1 : 100 dilution. Binding of the primary antibody was checked by Dako Quick-Staining, Labelled Streptavidin-Biotin System (LSAB; Dako, USA), followed by the addition of diaminobenzidine (DAB) as a chromogen. Each slide was scored in a blinded fashion by two pathologists according to the manufacturer's recommended criteria. The immunostaining was read in a semiquantitative manner and graded as follows: 0, 1+, 2+ and 3+. Intensity scores of 0 or 1+ were designated as negative expression and 3+ were designated as positive expression for HER-2/neu. Scores of 2+ were taken as equivocal cases, which were further recommended for FISH analysis.
Fluorescence in situ hybridization (FISH) analysis: FISH analysis was performed using the PathVysion HER-2 probe kit (Vysis, USA). There were two fluorescent-labelled probes:LSI (locus-specific identifier) HER-2 specific for the HER-2 gene locus (17q11) and CEP (chromosome enumeration probe) 17 specific for the α satellite DNA sequence at the centromeric region of chromosome 17. Paraffin sections of 3-4 mm thickness using a microtome were cut and were floated in a protein- free water bath at 40°C. The sections were mounted on poly-L-Lysine coated slides and allowed to dry. The slides were kept in oven overnight at 56°C. The slides were deparaffinized in xylene at room temperature for 20 min and dehydrated in 100 per cent ethanol for 15 min at room temperature and air dried. The slides were treated with pretreatment solution (sodium thiocyanite) and protease solution for 15 min, and were dehydrated with 70, 80 and 100 per cent alcohol for 5 min each and air dried. The probe was denatured at 80°C for 5 min and applied on to the slide and cover slipped, and placed in humidified chamber for overnight incubation. After that post-hybridization washes were given with 0.4 per cent 2XSCC (sodium saline citrate) 40 at 37°C. After removing cover slips the slides were dipped in post- hybridization buffer for 18 sec, dried completely in dark and 10 μl DAPI was applied and coverslip is gently placed. The slides were screened under florescent microscope (Olympus, USA) using appropriate filters (DAPI, FITC, TRITC dual and triple band pass filters). Signals were counted in at least 200 cells for both the HER-2/neu gene and chromosome 17 centromere signals under oil immersion at x 1000 magnification using recommended filters. Results were expressed as the ratio of HER-2/neu signal (orange) to centromere 17 signal (green) and the readings were read as follows: the expected ratio 1-1.8 indicates no gene amplification (negative), a ratio of >2.2 as HER-2/neu gene amplification (positive), and a ratio between 1.8-2.2 as equivocal cases. The polysomy 17 was also recorded in the cells as four spec green signals as moderate polysomy and >4 spec green signals as high polysomy.
Results
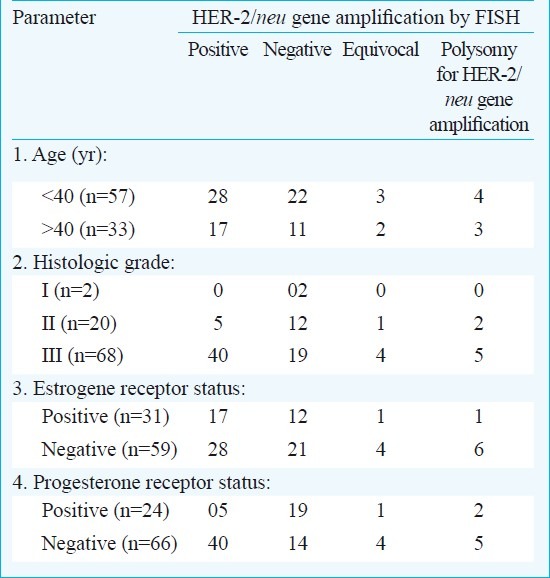
Of the 90 patients, 30 with a score of 0/1+ (negative) by IHC were FISH negative for HER-2/neu gene amplification (ratio between 0.6-1.6) (Fig. 1 A, B, Fig. 2 A, B). Of the 28 patients with the score of 2+ by IHC (Fig. 2C), 20 were FISH positive for HER-2/neu gene amplification (>2.2), three were FISH negative and five patients showed equivocal (1.8-2.2) results by FISH (Fig. 1C). These five cases were retested for IHC and FISH on different paraffin embedded tissue blocks, where all five patients were found eligible for trastuzumab-based therapy. Twenty five patients with the score of 3+ by IHC (Fig. 2D) were FISH positive for HER-2/neu gene amplification with the ratio of >3.9 (>2.2) (Fig. 1D). Seven cases with the score of 3+ by IHC were FISH negative for HER-2/neu gene amplification (>2.2). These cases showed polysomy of chromosome number 17 (spec green signals > 4) which could have been the reason for IHC 3+ (Fig. 3). The association of HER-2/neu status in these 90 patients with histological grade of tumour and estrogen and progesterone receptor status is shown in the Table.
Fig. 1.
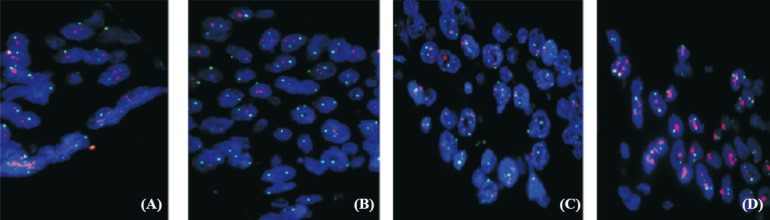
Fluorescence in situ hybridization (FISH) images showing negative, equivocal and positive results for HER-2/neu gene amplification. (A) Ratio of HER-2/neu(orange) signal to centromere 17 (green) signal 0.6-1.1 negative by FISH, (B) Ratio 1.6 negative by FISH, (C) Ratio 1.8-2.2, equivocal by FISH, (D) Ratio 3.9 positive by FISH.
Fig. 2.
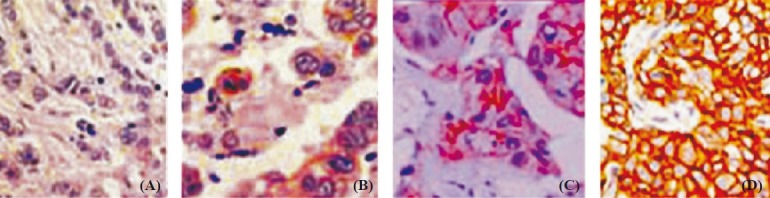
Immunohistochemical (IHC) analysis results showing immunostaining grades image with rations 0 to 1+ are negative for HER-2/neu membrane staining and 2+ are equivocal and 3+ are positive for HER-2/neu membrane staining. (A) Score 0, normal by IHC, (B) Score 1+ normal by IHC, (C) Score 2+ equivocal by IHC, (D) Score 3+ abnormal.
Fig. 3.
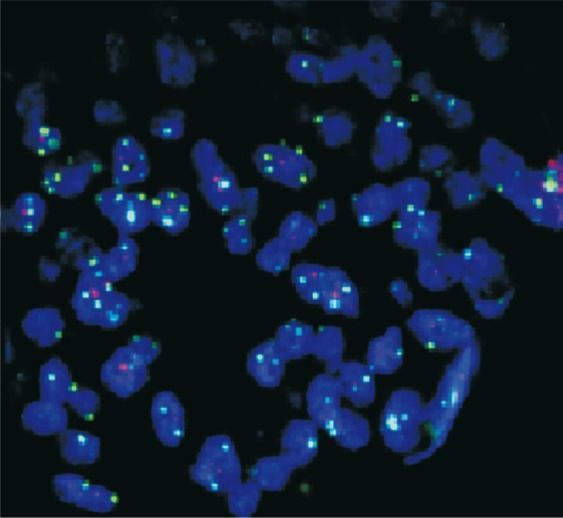
Polysomy 17 showing CEP 17 spec green signals= 4 by FISH.
Table.
Association of HER-2/neu status with clinical, estrogen and progesterone receptor (ER, PR) status and histological parameters
Discussion
The HER-2/neu gene is located on the long arm of chromosome 17 (17q12-21.32). It encodes p185 oncoprotein which is a receptor tyrosine kinase that can be associated with multiple signal transduction pathways. It has been found to be overexpressed in many types of human malignancies, notably breast, ovarian, gastric, pancreatic, prostatic, colorectal, cancers of the female genital tract and lung cancer. HER-2/neu, also known as erbB-2 oncoprotein is overexpressed in 25 to 30 per cent of breast cancers14. HER-2/neu overexpression in patients with breast cancer and positive lymph nodes is linked to poor prognosis with a reduced disease-free interval and shortened survival time, and similar linkage may exist in node-negative cases14–16. HER-2/neu gene expression level seems to be a significant predictor for response to some therapeutic agents14,17. Trastuzumab (Herceptin), a humanized monoclonal anti-HER-2/neu antibody, was approved by the US Food and Drug Administration as an adjuvant therapeutic agent for patients with metastatic breast cancer overexpressing HER-2/neu protein18,19–22. As a result, evaluation of HER-2/neu status has become pivotal in determining patient's eligibility for trastuzumab treatment.
In clinical laboratories, HER-2/neu status is usually assessed in formalin-fixed and paraffin-embedded specimens using either IHC or FISH. Wang et al22 achieved a high concordance rate of 98 per cent with two FISH assays, Inform (Ventana Medical Systems, Tucson, AZ) and PathVysion (Vysis). All IHC negative cases and nearly all IHC low positive (1+) cases showed no gene amplification, whereas most IHC high positive (3+) cases had gene amplification. However, the IHC medium positive (2+) cases demonstrated significant discordance with the FISH assay, i.e., some showed HER-2/neu gene amplification and others did not. Similar discordant results were seen in our patients; 30 patients with the score of 0/1+ by IHC were FISH negative for HER-2/neu gene amplification (ratio between 0.6-1.6), among 28 patients with the score of 2+ by IHC, 20 were FISH positive, three were FISH negative and five showed equivocal (1.8-2.2) results by FISH. The most appropriate HER-2 status for such patients falls in this gray zone (now defined as a FISH ratio of 1.8-2.2) and remains unclear. To address this, the new American Society of Clinical Oncology/ College of American Pathologists (ASCO/CAP) HER2 guidelines23 have added equivocal categories for FISH results, similar to those for immunohistochemical analysis, in the hope that this will prompt further study to better define the potential benefit from HER2-directed therapy for patients with FISH results that fall within this equivocal or borderline category24,25. In our study, the five cases retested by IHC and FISH on different paraffin embedded tissue blocks, were positive for HER-2/neu gene amplification and were eligible for trastuzumab-based therapy. The reason could be due to the heterogeneous nature of the tumour showing variation in results. Thus, FISH equivocal cases can be rechecked on different tissue block of the same patient.
In our study, younger breast cancer patients were reported to have higher frequency of HER-2 gene amplification. Panjwani et al26 showed positive correlation of grade III with HER-2/neu amplification which was concordant with existing literature. An inverse association was noted between hormone receptor status and HER-2 gene amplification in the present study. The reason could be the complex signaling between ER and other growth factor signaling pathways in breast cancer cells26. In our study, 18 per cent cases showed both expression of ER and HER2 amplification. HER2 amplification in these tumours is reported to be associated with resistance to tamoxifen therapy25. It is postulated that in these tumours, tamoxifen functions as an estrogen agonist to enhance growth in breast cancer cells which express high levels of HER2 and estrogen receptor co-activator resulting in de novo resistance for tamoxifen26.
Seven cases with the score of 3+ by IHC were FISH negative for gene amplification (>2.2). Earlier studies have shown similar results23,27–29. Although there is good correlation between HER-2 gene amplification and protein overexpression, many studies23 also have shown that 3 to 15 per cent of breast carcinomas over- express the HER-2 protein without gene amplification and a small subset of breast carcinomas amplify the HER-2 gene without overexpression. Various theories have been proposed to account for these discrepancies. Increased receptor expression in breast cancer without genetic alterations has been reported in approximately 10 per cent of cases, probably caused by transcriptional or post-translational activation. Other proposed explanations for the phenomenon of overexpression without amplification include artifactual high sensitivity of immunohistochemical assays, single copy overexpression of the HER-2 gene at the messenger RNA (mRNA) transcription level, or gene amplification below the level of detection of FISH assays30,31. The presence of chromosome 17 polysomy is not uncommon in breast carcinomas and has been suggested to account for overexpression without amplification23. We found that average chromosome 17 copy number when compared to average HER-2/neu copy number, was significantly higher in FISH interpreted as polysomy of chromosome 17, and this could be falsely interpreted as HER2/neu overexpression by IHC analysis. This would be reasonable to examine whether these IHC 3+/FISH-negative tumours with polysomy 17 are biologically distinct from other FISH-negative tumours and more similar to tumours with conventional HER-2/neu amplification, especially in terms of their response to Herceptin-based therapy. Hence, all breast cancer cases with an HER2 immunohistochemical score of 2+ should be reflex tested for HER2/neu gene amplification using FISH.
The discussion on the best method to determine HER-2/neu status in these samples continues, with the FISH method gaining popularity due to the recent evidence that it, in comparison with IHC, may more accurately predict clinical responses to trastuzumab-based therapies28. Investigation of HER-2/neu amplification along with frequent genetic changes would be valuable in determining prognostic factors. The equivocal cases evaluated by IHC and FISH should be interpreted with caution and such patients should be monitored on follow up. The current study found that a combined approach using both IHC and FISH methodologies can optimize HER-2/neu testing on breast carcinomas. There is also a need for establishing a clinically validated cut-off value for HER-2/neu FISH amplification against which IHC may be further compared and calibrated. This would potentially allow for more accurate and clinically meaningful HER-2/neu testing in the future.
Acknowledgment
The authors acknowledge the patients for sharing the clinical information and samples, the oncologists for referring the patients for the HER-2/neu testing and the management of Apollo hospitals for support.
References
- 1.Cancer Registry Annual Report 2000. Yuan, Republic of China: Department of Health; 2003. Bureau of Health Promotion, Department of Health, Executive Yuan, Republic of China. [Google Scholar]
- 2.National Cancer Institute. SEER Cancer Statistics Review, 1975-2001: Female Breast Cancer (invasive): Age-adjusted SEER Incidence and US Death Rates by Race/ethnicity and sex. [accessed on February 8, 2012]. Available from: http://seer.cancer.gov/csr/1975_2001/results_merged/topic_race_ethnicity.pdf .
- 3.Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987;235:177–82. doi: 10.1126/science.3798106. [DOI] [PubMed] [Google Scholar]
- 4.Dagrada GP, Mezzelani A, Alasio L, Ruggeri M, Romano R, Pierotti MA, et al. HER-2/neu assessment in primary chemotherapy treated breast carcinoma: no evidence of gene profile changing. Breast Cancer Res Treat. 2003;80:207–14. doi: 10.1023/A:1024579206250. [DOI] [PubMed] [Google Scholar]
- 5.Lear-Kaul KC, Yoon HR, Kleinschmidt-DeMasters BK, McGavran L, Singh M. HER-2/neu status in breast cancer metastases to the central nervous system. Arch Pathol Lab Med. 2003;127:1451–7. doi: 10.5858/2003-127-1451-NSIBCM. [DOI] [PubMed] [Google Scholar]
- 6.Durbecq V, Di Leo A, Cardoso F, Rouas G, Leroy JY, Piccart M, et al. Comparison of topoisomerase-IIalpha gene status between primary breast cancer and corresponding distant metastatic sites. Breast Cancer Res Treat. 2003;77:199–204. doi: 10.1023/a:1021874224490. [DOI] [PubMed] [Google Scholar]
- 7.Rudlowski C, Friedrichs N, Faridi A, Fuzesi L, Moll R, Bastert G, et al. HER-2/neu gene amplification and protein expression in primary male breast cancer. Breast Cancer Res Treat. 2004;84:215–23. doi: 10.1023/B:BREA.0000019953.92921.7e. [DOI] [PubMed] [Google Scholar]
- 8.Jones BA, Kasl SV, Howe CL, Lachman M, Dubrow R, Curnen MM, et al. African-American/White differences in breast carcinoma: p53 alterations and other tumor characteristics. Cancer. 2004;101:1293–301. doi: 10.1002/cncr.20500. [DOI] [PubMed] [Google Scholar]
- 9.Owens MA, Horten BC, Da Silva MM. HER2 amplification ratios by fluorescence in situ hybridization and correlation with immunohistochemistry in a cohort of 6556 breast cancer tissues. Clin Breast Cancer. 2004;5:63–9. doi: 10.3816/cbc.2004.n.011. [DOI] [PubMed] [Google Scholar]
- 10.Gancberg D, Jarvinen T, di Leo A, Rouas G, Cardoso F, Paesmans M, et al. Evaluation of HER-2/neu protein expression in breast cancer by immunohistochemistry: an interlaboratory study assessing the reproducibility of HER-2/neu testing. Breast Cancer Res Treat. 2002;74:113–20. doi: 10.1023/a:1016146130767. [DOI] [PubMed] [Google Scholar]
- 11.McCormick SR, Lillemoe TJ, Beneke J, Schrauth J, Reinartz J. HER2 assessment by immunohistochemical analysis and fluorescence in situ hybridization: comparison of HercepTest and PathVysion commercial assays. Am J Clin Pathol. 2002;117:935–43. doi: 10.1309/3643-F955-7Q6B-EWWL. [DOI] [PubMed] [Google Scholar]
- 12.Sauer T, Wiedswang G, Boudjema G, Christensen H, Karesen R. Assessment of HER-2/neu overexpression and/or gene amplification in breast carcinomas: should in situ hybridization be the method of choice? APMIS. 2003;111:444–50. doi: 10.1034/j.1600-0463.2003.t01-1-1110210.x. [DOI] [PubMed] [Google Scholar]
- 13.Ogura H, Akiyama F, Kasumi F, Kazui T, Sakamoto G. Evaluation of HER-2 status in breast carcinoma by fluorescence in situ hybridization and immunohistochemistry. Breast Cancer. 2003;10:234–40. doi: 10.1007/BF02966723. [DOI] [PubMed] [Google Scholar]
- 14.Revillion F, Bonneterre J, Peyrat JP. ERBB2 oncogene in human breast cancer and its clinical significance. Eur J Cancer. 1998;34:791–808. doi: 10.1016/s0959-8049(97)10157-5. [DOI] [PubMed] [Google Scholar]
- 15.Naber SP, Tsutsumi Y, Yin S, Zolnay SA, Mobtaker H, Marks PJ, et al. Strategies for the analysis of oncogene overexpression: studies of the neu oncogene in breast carcinoma. Am J Clin Pathol. 1990;94:125–36. doi: 10.1093/ajcp/94.2.125. [DOI] [PubMed] [Google Scholar]
- 16.Kallioniemi OP, Kallioniemi A, Kurisu W, Thor A, Chen LC, Smith HS, et al. ERBB2 amplification in breast cancer analyzed by fluorescence in situ hybridization. Proc Natl Acad Sci USA. 1992;89:5321–5. doi: 10.1073/pnas.89.12.5321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCann AH, Dervan PA, O’Regan M, Codd MB, Gullick WJ, Tobin BM, et al. Prognostic significance of c-erbB-2 and estrogen receptor status in human breast cancer. Cancer Res. 1991;51:3296–303. [PubMed] [Google Scholar]
- 18.Gusterson BA, Gelber RD, Goldhirsch A, Price KN, Save-Soderborgh J, Anbozhagen R, et al. Prognostic importance of c-erbB-2 expression in breast cancer. International (Ludwig) Breast Cancer Study Group. J Clin Oncol. 1992;10:1049–56. doi: 10.1200/JCO.1992.10.7.1049. [DOI] [PubMed] [Google Scholar]
- 19.Press MF, Bernstein L, Thomas PA, Meisner LF, Zhou JY, Ma Y, et al. HER-2/neu gene amplification characterized by fluorescence in situ hybridization: poor prognosis in node-negative breast carcinomas. J Clin Oncol. 1997;15:2894–904. doi: 10.1200/JCO.1997.15.8.2894. [DOI] [PubMed] [Google Scholar]
- 20.Baselga J, Norton L, Albanell J, Kim YM, Mendelsohn J. Recombinant humanized anti-HER2 antibody (Herceptin) enhances the antitumor activity of paclitaxel and doxorubicin against HER2/neu overexpressing human breast cancer xenografts. Cancer Res. 1998;58:2825–31. [PubMed] [Google Scholar]
- 21.Slamon D, Leyland-Jones B, Shak S, et al. Addition of Herceptin (humanized anti-HER2 antibody) to first line chemotherapy for HER2 overexpressing metastatic breast cancer (HER2+/MBC) markedly increases anticancer activity: a randomized, multinational controlled Phase III trial. Proc Am Soc Clin Oncol. 1998;17:98a. [Google Scholar]
- 22.Wang S, Saboorian MH, Frenkel E, Hynan L, Gokaslan ST, Ashfaq R. Laboratory assessment of the status of Her-2/neu protein and oncogene in breast cancer specimens: comparison of immunohistochemistry assay with fluorescence in situ hybridization assays. J Clin Pathol. 2000;53:374–81. doi: 10.1136/jcp.53.5.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lal P, Salazar PA, Ladanyi M, Chen B. Impact of polysomy 17 on HER-2/neu immunohistochemistry in breast carcinomas without HER-2/neu gene amplification. J Mol Diagn. 2003;5:155–9. doi: 10.1016/S1525-1578(10)60467-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Allred DC, Swanson PE. Testing for erbB-2 by immunohistochemistry in breast cancer. Am J Clin Pathol. 2000;113:171–5. doi: 10.1309/9x6x-1el6-5qb1-yld2. [DOI] [PubMed] [Google Scholar]
- 25.Gunn S, Yeh IT, Lytvak I, Tirtorahardjo B, Dzidic N, Zadeh S, et al. Clinical array-based karyotyping of breast cancer with equivocal HER2 status resolves gene copy number and reveals chromosome 17 complexity. BMC Cancer. 2010;10:396. doi: 10.1186/1471-2407-10-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Panjwani P, Epari S, Karpate A, Shirsat H, Rajsekharan P, Basak R, et al. Assessment of HER-2/neu status in breast cancer using fluorescence in situ hybridization & immunohistochemistry: Experience of a tertiary cancer referral centre in India. Indian J Med Res. 2010;132:287–94. [PubMed] [Google Scholar]
- 27.Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, et al. American Society of Clinical Oncology; College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007;25:118–45. doi: 10.1200/JCO.2006.09.2775. [DOI] [PubMed] [Google Scholar]
- 28.Tubbs RR, Pettay JD, Roche PC, Stoler MH, Jenkins RB, Grogan TM. Discrepancies in laboratory testing of eligibility for trastuzumab therapy: apparent immunohistochemical false-positives do not get the message. J Clin Oncol. 2001;19:2714–21. doi: 10.1200/JCO.2001.19.10.2714. [DOI] [PubMed] [Google Scholar]
- 29.Birner P, Oberhuber G, Stani J, Reithofer C, Samonigg H, Hausmaninger H, et al. Austrian Breast & Colorectal Cancer Study Group. Evaluation of the United States Food and Drug Administration-approved scoring and test system of Her-2 protein expression in breast cancer. Clin Cancer Res. 2001;7:1669–75. [PubMed] [Google Scholar]
- 30.Wang S, Saboorian MH, Frenkel E, Hynan L, Gokaslan ST, Ashfaq R. Laboratory assessment of the status of Her-2/neu protein and oncogene in breast cancer specimens: comparison of immunohistochemistry assay with fluorescence in situ hybridisation assays. J Clin Pathol. 2000;53:374–81. doi: 10.1136/jcp.53.5.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pauletti G, Dandekar S, Rong H, Ramos L, Peng H, Seshadri R, et al. Assessment of methods for tissue-based detection of the Her-2/neu alteration in human breast cancer: a direct comparison of fluorescence in situ hybridization and immunohistochemistry. J Clin Oncol. 2000;18:3651–64. doi: 10.1200/JCO.2000.18.21.3651. [DOI] [PubMed] [Google Scholar]


