Abstract
Background & objectives:
A retrospective study on chikungunya outbreak in India in five States viz. Delhi, Madhya Pradesh, Orissa, Maharashtra and Kerala was conducted in 2007-2008 to know the distribution and determinants of chikungunya fever outbreak in India.
Methods:
On the basis of high and low incidence of chikungunya fever, two districts from each State and two wards from the selected district were taken for random selection of 1000 households from 10 districts and 5 States. Semi-structured questionnaires were administered to individuals, patients, qualified health professionals and to stakeholders for collecting information.
Results:
The educational background and occupation of the respondents showed variations across the study States. Only in high incidence ward of Maharashtra, water storage period for 3-6 days and emptying, drying of water containers on weekly basis was noted. The study through knowledge, attitude, belief, practice (KABP) obtained individual's perception of chikungunya fever, its prevention and control. Patients’ expenditure on treatment was mainly recorded less than Rs  500 across study States. Health facility survey obtained an overview of the capacity of local health facilities. Stakeholders’ perception regarding chikungunya fever was also noted.
500 across study States. Health facility survey obtained an overview of the capacity of local health facilities. Stakeholders’ perception regarding chikungunya fever was also noted.
Interpretation & Conclusions:
The study revealed differences in awareness of chikungunya, cause of the disease, vector responsible, mode of transmission, biting time and elimination of breeding of mosquitoes statistically significant among high and low incidence wards of all the States. Expenditure on treatment was independent of economically active status and loss of man-days across all the States. Education and occupation did not have any relation with emptying/drying of water containers in high incidence wards. Strengthening of surveillance, information, education and communication (IEC) activities along with case management facilities may be provided by the State health department for prevention of chikungunya outbreaks in future. Stakeholders should be more involved in outbreak management and future planning.
Keywords: Aedes mosquito, case management, chikungunya, health facility, retrospective study, stakeholders, urban areas
Chikungunya disease is a mosquito-borne viral infection causing fever, rash and arthralgia. The name Chikungunya is derived from the Makonde word meaning “that which bends up” in reference to stooped posture developed as a result of the arthritic symptoms of the disease. Chikungunya virus is a mosquito-transmitted single-stranded RNA Alpha virus, from the family Togaviridae.
Since the 1952 Tanzania outbreak1,2 chikungunya virus has caused outbreaks in various parts of Africa3–5. The most recent epidemic re-emergence was documented in 1999-2000 in Kinshasa where an estimated 50,000 persons were infected6. The first documented Asian outbreak took place in 1958 in Bangkok, Thailand. Since then, many outbreaks have been recorded from Cambodia, Vietnam, Laos, Myanmar, Malaysia and Indonesia7–10. There is historical evidence that chikungunya virus originated in Africa and subsequently spread to Asia11. A distinctive feature of chikungunya virus is that it causes explosive outbreaks, before apparently disappearing for a period of several years to decades. In India, epidemics of chikungunya fever were reported during the last millennium viz,. 1963 - Kolkata, W. Bengal12, 1965 - Chennai, Tamil Nadu13,14 and 1973- Barsi, Maharashtra15. Thereafter, sporadic cases continued to be recorded specially in Maharashtra s0 tate during 1983 and 2000. During an epidemic outbreak of chikungunya virus more than 1.39 million suspected cases of chikungunya fever affecting 210 districts in 13 s0 tates have been reported during 200616. Maximum number of cases was recorded from Andhra Pradesh, Karnataka, Kerala, Tamil Nadu, Gujarat, Madhya Pradesh and Maharashtra.
A retrospective study on chikungunya outbreak in India was initiated during 2007. Five States viz. Delhi, Madhya Pradesh (MP), Orissa, Maharashtra and Kerala were selected principally on the basis of incidence of the disease, extent of distribution in terms of time, place, person as well as operational feasibility of prevention and control measures. The objective of the study was to comprehend the distribution and determinants of chikungunya fever outbreak in India.
The specific objectives of the study were to (i) carry out situational analysis of chikungunya fever, its characteristics and distribution vis-à-vis time, place, and person; (ii) explore the determinants of chikungunya fever epidemic, i.e. patient background (domestic, peri-domestic physical, socio-economic environments and health seeking and vector control practices); (iii) study vector habitat within and around households; (iv) assess the control strategies in health facilities and capacity for strategy implementation; and (v) to assess stakeholder views and extent of involvement.
Material & Methods
This retrospective study on chikungunya outbreak in India was initiated during 2007 in five States of India viz. Orissa, Maharashtra, MP, Delhi and Kerala with support from National Vector Borne Disease Control Programme (NVBDCP), New Delhi. The study was conducted strictly following the project protocol and set of questionnaires provided by NVBDCP to National Institute of Malaria Research (NIMR), New Delhi. Chikungunya outbreak during 2006 was spread across urban as well as rural areas. The present report focuses primarily on urban areas.
The sampling frame of the study was determined by arranging the districts of the selected States in descending order of the incidence of chikungunya fever and two districts were selected – one with the highest and another with the lowest incidence. The highest incidence districts in each State were identified as: Sundergarh in Orissa, Latur in Maharashtra, Betul in M.P., Alappuzha in Kerala, Mahavir Enclave Part II in Delhi. The lowest incidence districts identified were Ganjam in Orissa, Ratnagiri in Maharashtra, Katni in M.P., Kannur in Kerala and Dwarka in Delhi. In the selected districts, ward-wise incidence of chikungunya fever was arranged in descending order for selecting one ward with the highest and another with the lowest incidence.
H-H symbolizes high incidence ward under the highest incidence district while L-L stands for low incidence ward under the lowest incidence district. From Sundergarh district of Orissa, Panposh ward (H-H) and from Ganjam district, ward no 8 (L-L) were selected. From Latur district of Maharashtra, Rajiv Nagar ward (H-H) and from Ratnagiri district, Bailbug ward (L-L) were selected. From Betul district of M.P., Ram Nagar ward (H-H) and from Katni district, Indira Gandhi ward (L-L) were selected. From Mahavir Enclave Part II of Delhi ward no 51 (H-H) and from Dwarka, ward no 58 (L-L) were selected. From Alappuzha district of Kerala, ward no 5 (H-H) and from Kannur district, ward no 46 (L-L) were selected.
The populations of the selected wards in different States ranged between 2,000-4,000. In each selected district, 100 households each from the highest and the lowest incidence wards were selected randomly. The household lists of wards served as the universe and random selection of houses was accomplished by using random number Table. Thus, 1000 households were selected in 10 districts and 5 States. From each household, one individual was interviewed who was the prime respondent.
At household level, questionnaires administered to the respondents included: (i) Household survey; (ii) Knowledge, attitude, belief, practice survey regarding chikungunya fever prevention & control; (iii) Patient inventory. For health facility and stakeholder surveys, questionnaires administered included; (iv) Health facility survey; and (v) Stakeholder survey. For health facility surveys, one health facility in each ward was selected. In each health facility, qualified health professional was the key respondent. For stakeholder survey, stakeholders were randomly selected from amongst Councilor, Head Master/Mistress, School Teacher/Professor, Ward Member and Sarpanch. All questionnaires were pre-tested before actual data collection. The pre-test revealed many local issues. These were considered while finalizing the questionnaires according to local conditions.
To carry out surveys, one co-ordinator was selected from each s0 tate to visit selected wards in the respective State with support staff (field investigators, etc.) to fill the questionnaires. Before starting the survey, a training session of all the co-ordinators was conducted to explain and standardize the methodology for data collection. The completed questionnaires were received at NIMR for data processing. Differential analysis was attempted to broadly comprehend the distribution and determinants of chikungunya fever outbreak using standard software package.
Results
Household survey
Socio-demographic profile: The educational background of the respondents showed variations across study States. Overall, in H-H areas of Orissa, the highest percentage (37%) of the respondents had secondary education, while the highest percentage of the respondents in Kerala (30%) and MP (23%) had primary education. In H-H and L-L wards of Orissa, a majority of respondent (range 37 and 42%) belonged to business class (self employed) while in Maharashtra, (range 37 and 46%) were economically inactive. In H-H and L-L wards of MP and Kerala, service class mainly responded. In Delhi, a majority of respondents (range 37 and 54%) belonged to labour class. The monthly household income of the respondents in H-H wards in all study States, except in Delhi was found below  10,000. In Delhi, 54 per cent of respondents were noted having monthly household income of >
10,000. In Delhi, 54 per cent of respondents were noted having monthly household income of > 10,000. In L-L wards in all States, more or less similar picture was noted. Air coolers were observed in both H-H and L-L wards of Delhi, H-H and L-L wards of MP and Kerala, respectively.
10,000. In L-L wards in all States, more or less similar picture was noted. Air coolers were observed in both H-H and L-L wards of Delhi, H-H and L-L wards of MP and Kerala, respectively.
Water supply & storage: Water storage period in all the study s0 tates, except Maharashtra was for 1-2 days. In H-H wards of Maharashtra, 77 per cent of the respondents tend to store water for 3-6 days. Emptying, drying of all water containers was carried out on a daily basis in all study wards, except in H-H areas of Maharashtra where 51 per cent of respondents did the same on weekly basis.
Knowledge, attitude, belief, practice (KABP) regarding chikungunya fever, its prevention & control
Disease, cause, signs and symptoms, mode of transmission: In H-H wards of Maharashtra, MP and Kerala, majority (range 63% in Latur, Maharashtra to 94% in Betul, MP) of respondents were aware of chikungunya fever whereas in Delhi and Orissa, majority (range 56% in Mahavir Enclave Part II, Delhi to 85% in Sundergarh, Orissa) were ignorant. Across L-L wards, majority of the respondents (range 54% in Ganjam, Orissa to 96% in Dwarka, Delhi) were aware of chikungunya fever (Fig. a). The cause of the disease was known to 57 and 54 per cent of the respondents in H-H and L-L wards of Kerala and Delhi, respectively. In other states, majority of the respondents (range 68 to 97%) did not know about it (Fig. b). Majority of the respondents in H-H (range 82% in Alappuzha in Kerala to 100% in Sundergarh, Orissa and Mahavir Enclave Part II, Delhi) and L-L wards (range 90% in Katni, MP to 100% in Ganjam, Orissa) did not know the meaning of chikungunya (Fig. c).
Fig. (a-f).
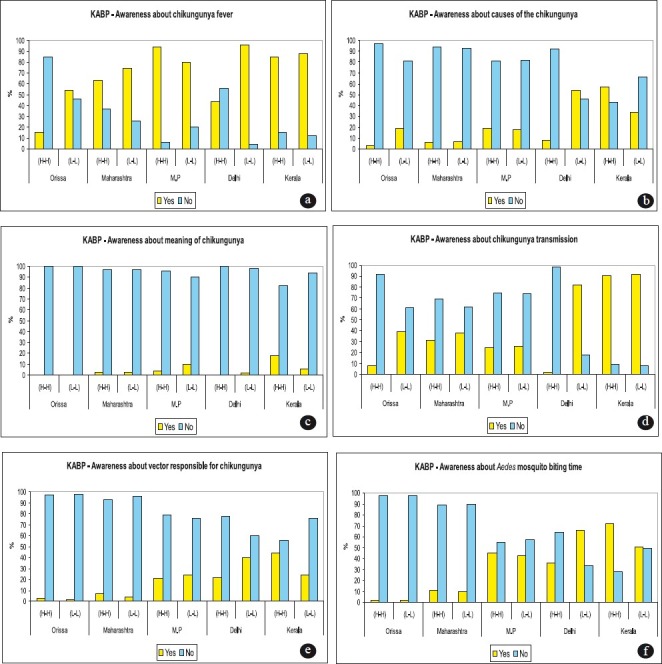
Awareness about chikungunya across five States of India.
In L-L wards of Delhi and Kerala, majority of responds (range 82% in Dwarka, Delhi to 92% in Kannur, Kerala) knew that chikungunya fever is transmitted from mosquitoes to human. In H-H ward of Kerala, 91 per cent knew about chikungunya fever transmission. In H-H wards of other States, majority of population (range 69% in Latur, Maharashtra to 98% in Mahavir Enclave Part II, Delhi) and in L-L wards (range 61% in Ganjam, Orissa, to 74% in Katni, MP) was ignorant (Fig. d). Only a few respondents across H-H wards of all the States (range 3% in Sundergarh, Orissa to 43% in Alappuzha, Kerala) knew the vector responsible for chikungunya transmission (Fig. e). Among H-H wards of all the States, the highest number of respondent (72%) from Kerala and among L-L wards, the highest number of respondents (66%) from Delhi, knew that Aedes mosquito bite during day time (Fig. f).
Signs and symptoms of the disease varied across different States whereas joint pain and swelling was the common among all (Table I).
Table I.
Knowledge, attitude, belief, practice regarding chikungunya fever prevention & control
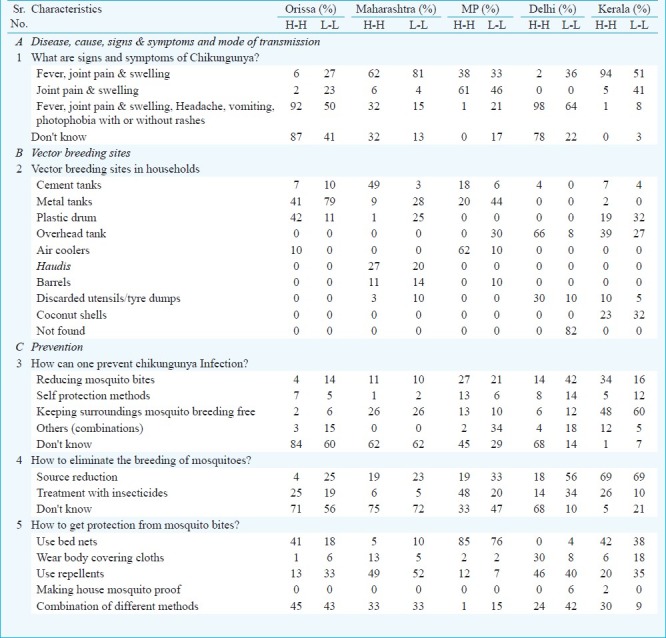
Vector breeding sites: Vector breeding sites varied across the States; in H-H wards, breeding was recorded from cements tanks, plastic drums, overhead tanks, air coolers and coconut shells. In L-L wards, breeding was found in metal tanks, plastic drums and coconut shells (Table I).
Prevention measures: Majority of the respondents in H-H wards of Orissa, Maharashtra, MP and Delhi (range 45% in Betul, MP to 84% in Sundergarh, Orissa) did not know regarding prevention of chikungunya infection. From H-H and L-L wards of Kerala, majority 48 and 60 per cent, respectively preferred keeping surroundings mosquito breeding free to prevent the same (Table I). Majority of the respondents in H-H wards of Orissa, Maharashtra and Delhi (range 68% in Mahavir Enclave Part II, Delhi to 75% in Latur, Maharashtra) did not know how to eliminate the breeding of mosquitoes whereas in MP and Kerala, 48 and 69 per cent, respectively preferred treatment with insecticides and source reduction. Among L-L wards of all the s0 tates, in Maharashtra the highest number of respondents (72%) did not know about it (Table I). Respondents across different States suggested different methods in order to get protection from mosquito bites.
Patient inventory: In all, 578 patients were interviewed from the five States. The highest number of chikungunya patients was recorded from Maharashtra State. Patients in H-H and L-L wards of Orissa, Delhi and Kerala were economically active while patients in Maharashtra and MP were inactive. Overall, 64 to 100 per cent patients in all the five s0 tates mentioned <  500 for expenditure on treatment and 67 to 100 per cent mentioned <
500 for expenditure on treatment and 67 to 100 per cent mentioned <  250 for expenditure on food. The highest loss of man days was recorded from H-H ward of Kerela (> 15 days) followed by Delhi (10-15 days), Orissa and MP (5-10 days) and Maharashtra (1-5 days).
250 for expenditure on food. The highest loss of man days was recorded from H-H ward of Kerela (> 15 days) followed by Delhi (10-15 days), Orissa and MP (5-10 days) and Maharashtra (1-5 days).
Health facility survey: In H-H and L-L wards, 16 and 4 bedded hospitals in Orissa, 60 and 200 bedded in Maharashtra, 150 and 120 bedded in MP, 15 and 50 bedded in Delhi and 251 and 50 bedded hospitals in Kerala, respectively were surveyed.
Chikungunya case management facilities, trained manpower, essential supplies and record keeping were available in the surveyed health facilities located in H-H wards of Maharashtra, MP and Kerala whereas in Orissa and Delhi, no such facilities were found. In L-L wards, such facilities were found in all the surveyed hospitals across five states except in Orissa. ELISA reader was available only in the surveyed hospital of the H-H ward in Kerala, while in L-L wards of the surveyed hospitals, it was found in Maharashtra, Delhi and Kerala (Table II).
Table II.
Results of health facility survey in five States
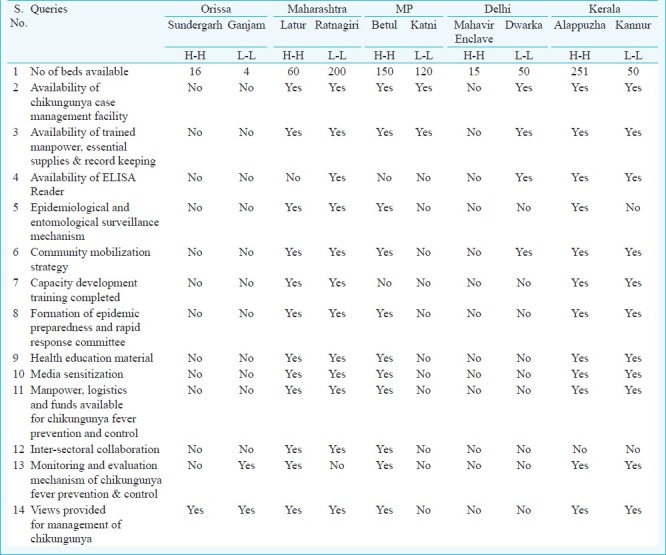
Epidemiological and entomological surveillance mechanisms were available in H-H wards of Maharashtra, MP and Kerala. In L-L wards, these mechanisms were provided only in Maharashtra. Community mobilization strategy was available in H-H wards of Maharashtra, MP and Kerala. In L-L wards, these strategies were provided only in Maharashtra, Delhi and Kerala. Capacity development trainings were completed only in H-H and L-L wards of Maharashtra and Kerala (Table II).
Epidemic preparedness and rapid response committee, health education material, media sensitization and availability of manpower, logistics and funds for chikungunya fever prevention and control were found in surveyed hospitals of H-H wards in Maharashtra, MP, Kerala and L-L wards of Maharashtra and Kerala only. Inter-sectoral collaboration was suggested only in the surveyed health facilities of both H-H and L-L wards of Maharashtra and H-H ward of MP. Monitoring and evaluation mechanism of chikungunya fever prevention and control was suggested in surveyed facilities in H-H wards of Maharashtra, MP and Kerala and in L-L wards of Orissa and Kerala only. Chikungunya fever management views were provided in all the surveyed health facilities of H-H wards of all the s0 tates except in Delhi (Table II).
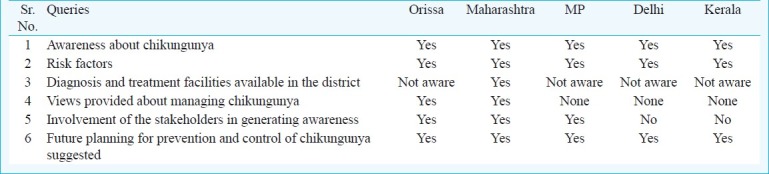
Stakeholder survey: Awareness about chikungunya fever and risk factors was found among all the interviewed stakeholders of five States. Only stakeholders from Maharashtra spoke about the availability of diagnosis and treatment facilities while the stakeholders from other States had no idea about it. Views regarding management of chikungunya were provided by the stakeholders from Orissa and Maharashtra only. All the interviewed stakeholders suggested future planning for prevention and control of chikungunya (Table III).
Table III.
Stakeholders’ views about chikungunya management & control in five States
Discussion
Earlier studies done on chikungunya were related to outbreak investigation17,18 and chikungunya fever case management19; however, this is a retrospective study first of its kind with specific objectives carried out in urban areas of five States.
The study revealed differences in awareness of chikungunya, cause of the disease, vector responsible, mode of transmission, biting time and elimination of breeding of mosquitoes statistical significant among high and low incidence wards of all the States (P<0.05). Expenditure on treatment was independent of economically active status and loss of man days across all the States. Education and occupation did not have association with emptying/drying of water containers in high incidence wards.
The study through the health facility survey obtained an overview of the capacity (technical /managerial and financial) of local health facilities for managing chikungunya cases. In Maharashtra and MP, 22 staff members were involved in epidemiological and entomological surveillance and reporting was on a daily basis; in Kerala, 140 staff members carried out entomological surveillance and three were involved in epidemiological surveillance and reporting was on a daily basis. Chikungunya fever prevention measures suggested were reducing mosquito breeding sites, use of bed nets, survey of containers, use of insecticides for vector control, use of mosquito repellents, health education and media sensitization. Inter-sectoral collaboration was emphasized by involving NSS students, schools, Mahila Panchayat, revenue and education departments, municipal corporation and non government organizations (NGOs) for educating the masses regarding chikungunya fever. Monitoring and evaluation mechanisms of chikungunya fever and control suggested were symptomatic and clinical assessment, container survey, health education and chemical control for source reduction. Views provided for chikungunya management were – symptomatic treatment of patients, training of doctors for disease management, covering of open scrap lying outside to prevent water stagnation, use of insecticides, fogging and health education, alert preparedness, detection and early treatment of the cases, regular vector control mechanism with proper house-to-house survey.
According to stakeholders’ perception risk factors included environmental factors like breeding sites within and outside human habitats and population migration, etc. In addition, enhanced awareness and maintenance of hygiene and sanitation by general public that includes but not limited to covering of water containers, taking precautions from mosquito bites, usage of bed nets by householders are considered important. Strengthening the local health facilities for chikungunya case management was also underscored. The stakeholder's extent of involvement included organization of health camps, rally of students with banners, fogging and insecticide spraying, arranged training of paramedic staff, media sensitization, information, education and communication (IEC) activities for school children and cleaning of surroundings.
Strengthening of surveillance, IEC activities along with case management facilities may be provided by the State health department for prevention of chikungunya outbreak in future. Stakeholders should be more involved and may be provided working funds.
Acknowledgment
The authors acknowledge the Director, National Vector Borne Disease Control Programme, Government of India, for funding the study, and Secretaries & Directors of State Health Services, Municipal Health Officers (MHO), Dy. MHOs, Chief Medical Officers (CMOs), Dy. CMOs, Entomologists, Districts Malaria Officers and Assistant Malaria Officers of the States viz. Orissa, Maharashtra, M.P., Delhi and Kerala for facilitating this study. The authors thank the Medical Officers and other paramedical staff of hospitals for their help in conducting the field level data collection. All stakeholders are acknowledged gratefully for giving their time, suggestions and support to the study. The co-ordinators and field staff are acknowledged for their valuable contributions in conducting the surveys.
References
- 1.Robinson MC. An epidemic of virus disease in Southern Province, Tanganyika territory, in 1952-53. I. Clinical features. Trans R Soc Trop Med Hyg. 1955;49:28–32. doi: 10.1016/0035-9203(55)90080-8. [DOI] [PubMed] [Google Scholar]
- 2.Lumsden WH. An epidemic of virus disease in Southern Province, Tanganyika territory, in 1952-53; II. General description and epidemiology. Trans R Soc Trop Med Hyg. 1955;49:33–57. doi: 10.1016/0035-9203(55)90081-x. [DOI] [PubMed] [Google Scholar]
- 3.Williams MC, Woodall JP, Corbet PS, Gillett JD. O’nyongnyong fever: an epidemic virus disease in East Africa. 8. Virus isolations from Anopheles mosquitoes. Trans R Soc Trop Med Hyg. 1965;59:300–6. doi: 10.1016/0035-9203(65)90012-x. [DOI] [PubMed] [Google Scholar]
- 4.Lanciotti RS, Ludwig ML, Rwaguma EB, Lutwama JJ, Kram TM, Karabatsos N, et al. Emergence of epidemic O’nyong-nyong fever in Uganda after a 35-year absence: genetic characterization of the virus. Virology. 1998;252:258–68. doi: 10.1006/viro.1998.9437. [DOI] [PubMed] [Google Scholar]
- 5.Diallo M, Thonnon J, Traore Lamizana M, Fontenille D. Vectors of Chikungunya virus in Senegal: current data and transmission cycles. Am J Trop Med Hyg. 1999;60:281–6. doi: 10.4269/ajtmh.1999.60.281. [DOI] [PubMed] [Google Scholar]
- 6.Pastorino B, Muyembe-Tamfum JJ, Bessaud M, Tock F, Tolou H, Durand JP, et al. Epidemic resurgence of Chikungunya virus in Democratic Republic of the Congo: identification of a new central African strain. J Med Virol. 2004;74:277–82. doi: 10.1002/jmv.20168. [DOI] [PubMed] [Google Scholar]
- 7.Mathew T, Thiruvengadam KV. Further studies on the isolate of Chikungunya from the Indian repatriates of Burma. Indian J Med Res. 1973;61:517–20. [PubMed] [Google Scholar]
- 8.Laras K, Sukri NC, Larasati RP, Bangs MJ, Kosim R, Djauzi, et al. Tracking the re-emergence of epidemic chikungunya virus in Indonesia. Trans R Soc Trop Med Hyg. 2005;99:128–41. doi: 10.1016/j.trstmh.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 9.Lam SK, Chua KB, Hooi PS, Rahimah MA, Kumari S, Tharmaratnam M, et al. Chikungunya infection - an emerging disease in Malaysia. Southeast Asian J Trop Med Public Health. 2001;32:447–51. [PubMed] [Google Scholar]
- 10.Jupp PG, McIntosh BM. Chikungunya virus disease. In: Monath TP, editor. The arboviruses: epidemiology and ecology. Boca Raton (Florida): CRC Press; 1988. pp. 137–57. [Google Scholar]
- 11.Powers AM, Brault AC, Tesh RB, Weaver SC. Re-emergence of chikungunya and o’nyong-nyong viruses: evidence for distinct geographical lineages and distant evolutionary relationships. J Gen Virol. 2000;81:471–9. doi: 10.1099/0022-1317-81-2-471. [DOI] [PubMed] [Google Scholar]
- 12.Shah KV, Gibbs CJ, Jr, Banerjee G. Virological investigation of the epidemic of haemorrhagic fever in Calcutta: Isolation of three strains of Chikungunya virus. Indian J Med Res. 1964;52:676–83. [PubMed] [Google Scholar]
- 13.Jadhav M, Namboodripad M, Carman RH, Carey DE, Myers RM. Chikungunya disease in infants and children in Vellore: a report of clinical and haematological features of virologically proved cases. Indian J Med Res. 1965;53:764–76. [PubMed] [Google Scholar]
- 14.Thiruvengadam KV, Kalyanasundaram V, Rajgopal J. Clinical and pathological studies on Chikungunya fever in Madras City. Indian J Med Res. 1965;53:729–44. [PubMed] [Google Scholar]
- 15.Padbidri VS, Gnaneswar TT. Epidemiological investigations of chikungunya epidemic at Barsi, Maharashtra state, India. J Hyg Epidemiol Microbiol Immunol. 1979;23:445–51. [PubMed] [Google Scholar]
- 16.Jain SK, Kumar K, Bhattacharya D, Venkatesh S, Jain DC, Lal S. Chikungunya viral disease in district Bhilwara (Rajasthan) India. J Commun Dis. 2007;39:25–31. [PubMed] [Google Scholar]
- 17.Kannan M, Rajendran R, Sunish IP, Balasubramaniam R, Arunachalam N, Paramasivan R, et al. A study on chikungunya outbreak during 2007 in Kerala, south India. Indian J Med Res. 2009;129:311–5. [PubMed] [Google Scholar]
- 18.Kirte RC, Naik DB, Khamgaonkar MB. Clinico-epidemiological profile of fever cases admitted during epidemics of chikungunya fever. J Commun Dis. 2007;39:33–5. [PubMed] [Google Scholar]
- 19.Bouquillard E, Combe B. Rheumatoid arthritis after Chikungunya fever: a prospective follow-up study of 21 cases. Ann Rheum Dis. 2009;68:1505–6. doi: 10.1136/ard.2008.097626. [DOI] [PubMed] [Google Scholar]


