Abstract
Objectives
To determine the disease burden, measured by resource utilization, of four urologic conditions among veteran users of VA health care services and to assess variations by selected socio-demographic characteristics.
Methods
We applied expert-derived diagnosis clusters to establish four patient cohorts from a population of U.S. veterans age 18 and older with at least 1 outpatient visit in a VA health care facility in Fiscal year 2001 (n=3,691,519): (1) benign prostatic hyperplasia/lower urinary tract symptoms (BPH/LUTS), (2) kidney stones (KS), (3) urinary tract infections (UTI), and (4) urinary incontinence (UI). We identified patients with qualifying diagnosis codes associated with outpatient visits in the national VA Outpatient Clinic file thereby generating case counts for each diagnostic category.
Results
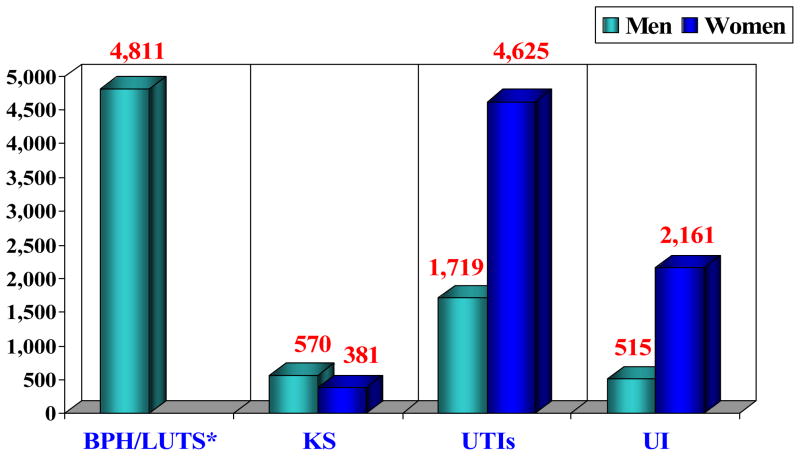
Among veteran users of VA health care services, when defined as the primary reason for the visit, the prevalence of BPH/LUTS was 4,811 per 100,000 veterans (4.8%); the prevalence of KS was 597 per 100,000 (0.6%); the prevalence of UTI was 4,265 and 1,719 per 100,000 female and male veterans, respectively (4.3% and 1.7%); and the prevalence of UI was 2,161 and 515 per 100,000 female and male veterans, respectively (2.2% and 0.5%). Prevalence of these conditions when ascertained by capturing diagnoses appearing as secondary reasons for a physician visit was much higher.
Conclusions
Although we expected the prevalence of urologic conditions to be high among veterans who use the VA system for care, we found the burden of urologic disease among veterans to be comparable to other national data sets. Prevalence estimates based on primary diagnosis, rather than secondary or “any” diagnosis, significantly underestimated the disease burden among veterans.
INTRODUCTION
Urologic disease encompasses a wide variety of conditions of the genitourinary tract that affect individuals at all stages of life. Estimates from existing data sources suggest that urologic diseases account for well over $20 billion in health care costs per year in the U.S. alone1. However, lack of a systematic approach to assessing available data has placed urologic health outside the principal health care and quality improvement initiatives that have been forwarded by the Institute of Medicine (IOM)2 and the National Committee for Quality Assurance (NCQA)3 in favor of conditions that have been more thoroughly studied.
In response to this gap in knowledge, the National Institute of Diabetes, Digestive and Kidney Diseases (NIDDK), designed and subsequently funded the Urologic Diseases in America (UDA) Project to create a synthesis of existing data concerning the burden of urologic disease. The goal of the UDA project was to use the best available data sources throughout the U.S. to create the first national compendium that delineates changes in the epidemiology, practice patterns, health and economic impact for urologic diseases that fall within the scope of urologic practice1. This omnibus has provided the necessary evidence base for identifying variations in prevalence and practice that, in turn, have served as the foundation for generating evidence-based strategic planning for public and private funding of basic, clinical and health services research.
Veterans are a national cohort at risk for a variety of common urologic problems. The Department of Veterans Affairs (VA) is the largest health care system in the U.S., comprised of over 160 VA hospitals and over 600 community-based outpatient clinics. According to the 2000 U.S. Census, veterans comprise approximately 13% of the U.S. population, numbering 26.5 million men and women4. Overall, the VA also serves over 75% of the all disabled and low income veterans nationwide4. As such, veteran users of VA health care have substantially lower physical and mental health scores than veteran non-users or their civilian counterparts5,6. Given the demographic profile of US Veterans, we hypothesized that the VA healthcare system would bear a large burden of urologic disease. Specifically, we hypothesized that urologic diseases would be more prevalent among veterans than their civilian counterparts, at least partially because veterans of all ages do not face access to care issues associated with a lack of health insurance.
To test our hypothesis, we turned to resources available through the Urological Diseases in America project to examine prevalence among veteran users of the VA health care system of four major urologic conditions: (1) benign prostatic hyperplasia/lower urinary tract symptoms (BPH/LUTS), (2) urolithiasis or kidney stones (KS), (3) urinary tract infections (UTI), and (4) urinary incontinence (UI). Though we later expanded to all of the most common urologic conditions, herein we report on the first four conditions analyzed by the UDA. We also aimed to describe the extent of variations in these conditions by age, by gender (where appropriate) and by race-ethnicity. As used in this context, ‘prevalence’ refers to disease burden expressed through use of healthcare resources, as opposed to ‘population-based’ prevalence.
MATERIALS & METHODS
Institutional Review Board approval was obtained through UCLA and the Sepulveda VA in the greater Los Angeles area. The VA maintains a centralized data repository for the entire VA health care system, providing a comprehensive resource to examine burden. Each VA medical center sends computerized excerpts of every health care encounter to the Austin Automation Center, where centralized SAS file extracts are created. For these analyses, we focused on the VA Outpatient Clinic or OPC files, which are patient-level databases organized by fiscal year and include demographics, type of visit, clinic stops and, since 1997, outpatient diagnoses.
We examined four urologic conditions: benign prostatic hyperplasia/lower urinary tract symptoms (BPH/LUTS), kidney stones (KS), urinary tract infections (UTI), and urinary incontinence (UI). Physician experts derived inclusion and exclusion ICD-9 diagnosis code-based criteria for each urologic condition. These algorithms in turn were reviewed and refined by nationally recognized experts in urology. We identified patients with qualifying diagnosis codes associated with outpatient visits from October 1, 2000 through September 30, 2001 (FY 2001) in the national VA Outpatient Clinic (OPC) file thereby generating case counts for each diagnostic category.
The population studied included all U.S. veterans age 18 and older with at least 1 outpatient visit in any VA health care facility nationwide in FY 2001 (n=3,691,519). We eliminated redundant patients seen at more than one facility to arrive at unique patient counts for our denominators. We first identified the base population at risk in the same year (male veterans 40+ for BPH; male and female patients 18+ for other conditions). We used similar approaches to stratify diseases burden by risk categories, including age, gender, and race-ethnicity. We also examined the differences in case counts based on use of primary diagnosis (the main reason for the specific encounter) vs. any listed diagnoses (secondary diagnoses that are not the chief reason for a patient’s visit). We measured prevalence as the number of existing cases per 100,000 unique outpatients.
RESULTS
Among veteran users of VA health care services, the prevalence among patients ages 40 and older with a primary diagnosis of BPH/LUTS was 4,811 per 100,000 unique patients in FY2001 (4.8%, Table 1). The number of patients diagnosed with kidney stones was much lower at 605 cases per 100,000; 570 and 381 cases per 100,000 patients for men and women (0.6% and 0.4%, respectively). UTIs were more than twice as common among women veterans compared to men (4,265 female and 1,719 male UTIs per 100,000, Figure 1). This was due to the high frequency of visits for cystitis among women. The prevalence of outpatient visits for pyelonephritis was only slightly higher in women. Urinary incontinence was over four times more prevalent among women than men (2,161 female and 515 male UIs per 100,000, Figure 1).
TABLE 1.
Overview of Prevalence of Selected Urologic Conditions among U.S. Veteran Users of Veterans Health Administration (VHA) Facilities in Fiscal Year 2001 (Primary and All Diagnoses)
| Urologic Condition and Sub- Conditions | Unweighted Frequency (# cases) | Base Population (# SSNs per strata) | Rate per 100,000 (# cases per 100,000 unique outpatients) | ||
|---|---|---|---|---|---|
| Primary Diagnosis | All Diagnoses | Primary Diagnosis | All Diagnoses | ||
| BPH/LUTS | 159,325 | 377,701 | 3,311,450 | 4,811 | 11,406 |
| URINARY TRACT STONES | 22,055 | 35,376 | 3,691,533 | 597 | 958 |
| Upper Tract Stones | 20,717 | 33,702 | 3,691,533 | 561 | 913 |
| Lower Tract Stones | 2,107 | 2,748 | 3,691,533 | 57 | 74 |
| URINARY TRACT INFECTIONS | |||||
| Adult Female UTI (18+) | 7,033 | 9,156 | 164,906 | 4,265 | 5,552 |
| Cystitis | 773 | 1,033 | 164,906 | 469 | 626 |
| Pyelonephritis | 105 | 129 | 164,906 | 64 | 78 |
| Other | 6,404 | 8,369 | 164,906 | 3,883 | 5,075 |
| Adult Male UTI (18+) | 60,622 | 82,326 | 3,526,627 | 1,719 | 2,334 |
| Cystitis | 3,911 | 5,671 | 3,526,627 | 111 | 161 |
| Pyelonephritis | 1,397 | 2,105 | 3,526,627 | 40 | 60 |
| Orchitis | 3,482 | 11,780 | 3,526,627 | 99 | 334 |
| Other | 47,644 | 65,891 | 3,526,627 | 1,351 | 1,868 |
| URINARY INCONTINENCE | |||||
| Adult Female UI (18+) | 3,563 | 6,196 | 164,906 | 2,161 | 3,757 |
| Stress incontinence | 3,545 | 6,174 | 164,906 | 2,150 | 3,744 |
| Fistulae | 22 | 32 | 164,906 | 13 | 19 |
| Adult Male UI (18+) | 18,149 | 34,377 | 3,526,627 | 515 | 975 |
Source: Outpatient Clinic File (OPC), VA Austin Automation Center (FY2001).
Figure 1.
Prevalence of BPH, KS, UTIs and UI among Veteran Users of VA Health
We measured the absolute number of cases as another means to assess disease burden. BPH/LUTS had the highest absolute burden with nearly 160,000 cases identified in 2001 alone (Table 1). While visits for UTIs were more frequent among women veterans, there were over 60,000 men with an outpatient visit for a UTI in the same year and only 7000 such women. Similar patterns existed for urinary incontinence, where the high prevalence rate was not associated with a number of cases because women represented only 5–7% of the user population during that time period.
We also examined the impact of defining prevalence using visits for which the condition of interest was a primary diagnosis (the primary reason for the encounter) versus defining prevalence using visits for which the condition was a secondary diagnosis (found in any diagnosis position in the outpatient records). Prevalence based on “any” diagnosis resulted in significantly higher rates for each condition. The highest increases were for female urinary incontinence, for which use of “any diagnosis” nearly doubled the estimated prevalence (from 2.2% to 3.8%), and BPH/LUTS, which increased by 136% (from 4.8% to 11.4%, Table 1). Using “any” diagnosis had the least impact on female kidney stones and UTIs.
The age distribution for each of these urologic conditions varied by disease. BPH/LUTS increased linearly with age, from 808 to 7,136 per 100,000 for 40–44 vs. 85+ age groups, with a small decline for patients 85 and older. The age distribution for patients with kidney stones was roughly normally distributed, with peak prevalence among 45–64 year olds (838/100,000). There was no significant variation in the prevalence of urinary tract infections by age. Urinary incontinence in men increased with age, from 87 per 100,000 for men ages 25 years and younger to 1,365 per 100,000 for men 85 years an over. However, UI rates rose at a much earlier age for women veterans than for male veterans.
Our examination of racial-ethnic differences revealed that Hispanic veterans had the highest prevalence of BPH/LUTS and kidney stones, followed by Caucasians (Table 2). Among women veterans, Hispanic women had the highest UTI rates, whereas Hispanic and black male veterans had the highest UTI rates among men. White female veterans had the highest rates of urinary incontinence, while black women had the lowest, a pattern that is reversed for male veterans.
Table 2.
Racial-Ethnic Variations in Prevalence of BPH, KS, UTI, UI among VA Users (number unique cases per 100,000 outpts)
| White | Black | Hispanic | Other | Unknown | |
|---|---|---|---|---|---|
| BPH | 5,889 | 5,126 | 6,131 | 4,302 | 3,481 |
| KS | 762 | 470 | 918 | 692 | 346 |
| UTI | |||||
| Female | 5,322 | 4,942 | 5,666 | 3,630 | 3,048 |
| Male | 2,139 | 2,912 | 2,888 | 1,764 | 925 |
| UI | |||||
| Female | 3,283 | 1,680 | 2,511 | 2,530 | 1,272 |
| Male | 688 | 876 | 571 | 536 | 251 |
COMMENT
Our study had several important findings. Each of the four urologic diseases studied poses a large burden on the health of both female and male veterans and on the health care system caring for them. However, we found the utilization rates for each of the four diseases among veterans to be similar to data from the National Ambulatory Medical Care Survey (NAMCS), a national sample of data collected from non-federally employed physicians engaged in direct patient care7. This contradicts our hypothesis that veterans, who have full access to healthcare resources through the VA, might have been be more likely to use more resources and therefore have higher rates of utilization (a phenomenon known as “moral hazard”8). Many veterans receiving care in the VA system seek additional care outside of the VA system, and therefore may be newly diagnosed with a condition, such as an acute episode of renal colic from a kidney stone, elsewhere. This might explain why the use of “any” (secondary) diagnoses resulted in a lower prevalence for each disease compared to other utilization studies.
BPH/LUTS was identified in 11.4% of veterans over 40, including men with both a primary and secondary diagnosis, with a linear increase in prevalence with age. This utilization rate was lower than that in NAMCS (14.5%)9. Data from the Massachusetts Male Aging Study (MMAS) showed the prevalence of BPH, as identified by clinical diagnosis or history of surgery for BPH, to range from 8.4% in men 40 to 49 years of age to 33.5% in men aged 60 to 709,10. This linear increase in age was similar to that seen in our study. We also found a higher prevalence of BPH/LUTS among Hispanic veterans, followed by Caucasians and African Americans. In a comparison of data from the Olmsted County Study of Urinary Symptoms and Health Status and the Flint Men's Health Study, Sarma et al. found that 34% of white men reported moderate/severe LUTS compared with 41% of black men11- a finding that contrasts with our findings for black and white men. The black men in the Flint study may have lacked access to care such as that provided by the VA, explaining the worse symptoms among those men.
Primary diagnoses of UTIs were more than twice as common among women veterans compared to men (4,265 female and 1,719 male UTIs per 100,000), yet prevalence was high in both men and women. NAMCS data from 2000 similarly reported a rate of 6,013 per 100,000 (6.0%) office visits by women with a primary diagnosis of UTI and a rate of 1,342 per 100,000 (1.3%) visits by men12,13. The rates of outpatient care-seeking for stone disease as a primary diagnosis among veterans (597 per 100,000, or 0.6%) also compared closely to rates from NAMCS, 668 per 100,000 population, or 0.7%, in the year 20009.
The utilization rates for a primary diagnosis of urinary incontinence were similar between the VA system (2.2% for women and 0.5% for men) and NAMCS (1.1% for women and 1.1% for men). However, rates in both datasets were lower than expected, given the very high prevalence of the condition in the community14–17. The differences in clinical utilization rates and community-based questionnaire data are likely due to the fact that the majority of people with incontinence do not seek treatment for it17. Interestingly, the racial distribution of urinary incontinence in the VA system paralleled that found by the 1999–2001 National Health and Nutrition Examination Survey (NHANES)14–17; Caucasian women and African American men had the highest prevalence. This may be due to more stress incontinence among Caucasian women and more urge incontinence among African Americans14.
This study faces a number of important limitations. First, the diagnosis codes in the VA databases may have variable accuracy. VHA providers are not reimbursed for specific diagnoses or treatment, and therefore may have less incentive to accurately code all conditions18. Second, race-ethnicity data in the VA administrative datasets are based historically on observation, which may result in misclassification. Race-ethnicity is also missing in many records, and missing data rates are sometimes as high as 30%, biased towards complete data for patients with a history of hospitalization. Furthermore, regional differences in race/ethnicity may explain some of the variability we identified. For example, if there are more Hispanics in the southern U.S., the higher prevalence of stone disease in Hispanics may be attributed to location and weather rather than ethnicity. Also, the comparisons we made with data from NAMCS should be interpreted with a degree of caution, as the data were obtained in a different manner, and physicians who participated in NAMCS may have been more thorough in coding the primary and secondary diagnoses, resulting in higher prevalence rates. Nonetheless, the urologic disease burden here provides a portrait of the annual impact on the VA system.
CONCLUSIONS
This study represents a national assessment of the disease burden of common urologic conditions among veteran users of the VA health care system. The urologic disease burden among veteran users of VA health care services is high and poses a significant burden not only among veterans but to the VA health care system responsible for caring for them. We found that use of primary diagnosis in these administrative datasets significantly underestimated urologic disease burden. The aging of veteran users will only further increase the urologic disease burden. At this early juncture, more research is needed on patterns of care and quality in terms of disease detection, diagnosis, treatment and health outcomes in VA settings.
Acknowledgments
Funded by: Urologic Diseases in America (UDA) Project, National Institutes of Diabetes, Digestive and Kidney Diseases (NIDDK).
References
- 1.Litwin MS, Saigal CS, editors. Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Washington, DC: US Government Publishing Office; 2007. 2004 NIH Publication No. 04-5512. Also accessible at www.uda.niddk.nih.gov. [Google Scholar]
- 2.Institute of Medicine (U.S.). Committee on Quality of Health Care in America. Crossing the quality chasm : a new health system for the 21st century. Washington, D.C: National Academy Press; 2001. p. xx.p. 337. [Google Scholar]
- 3.National Committee for Quality Assurance. The State of Health Care Quality. Washington, D. C: 2006. Also available at http://web.ncqa.org/ [Google Scholar]
- 4.Richardson C, Veterans Waldrop J. Census 2000 Brief. 2000 Issued May 2003. Available at: http://www.census.gov/prod/2003pubs/c2kbr-22.pdf.
- 5.Kazis LE, Ren XS, Lee A, Skinner K, Rogers W, Clark J, Miller DR. Health status in VA patients: results from the Veterans Health Study. Am J Med Qual. 1999;14:28–38. doi: 10.1177/106286069901400105. [DOI] [PubMed] [Google Scholar]
- 6.Rogers WH, Kazis LE, Miller DR, Skinner KM, Clark JA, Spiro A, 3rd, Fincke RG. Comparing the health status of VA and non-VA ambulatory patients: the veterans' health and medical outcomes studies. J Ambul Care Manage. 2004;27:249–62. doi: 10.1097/00004479-200407000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Saigal C, Joyce G, Geschwind S, Litwin M, Saigal CS, Joyce GF, Geschwind SA, Litwin MS. Methods. In: Litwin MS, Saigal CS, editors. Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Washington, DC: US Government Publishing Office; 2004. pp. 283–316. NIH Publication No. 04-5512. Also accessible at www.uda.niddk.nih.gov. [Google Scholar]
- 8.Nyman JA. Is 'moral hazard' inefficient? The policy implications of a new theory. Health Aff (Millwood) 2004;23:194–199. doi: 10.1377/hlthaff.23.5.194. [DOI] [PubMed] [Google Scholar]
- 9.Wei JT. Benign Prostatic Hyperplasia. In: Litwin MS, Saigal CS, editors. Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Washington, DC: US Government Publishing Office; 2004. pp. 43–70. NIH Publication No. 04-5512. Also accessible at www.uda.niddk.nih.gov. [Google Scholar]
- 10.Meigs JB, Mohr B, Barry MJ, Collins MM, McKinlay JB. Risk factors for clinical benign prostatic hyperplasia in a community-based population of healthy aging men. J Clin Epidemiol. 2001;54:935–44. doi: 10.1016/s0895-4356(01)00351-1. [DOI] [PubMed] [Google Scholar]
- 11.Sarma AV, Wei JT, Jacobson DJ, Dunn RL, Roberts RO, Girman CJ, Lieber MM, Cooney KA, Schottenfeld D, Montie JE, et al. Comparison of lower urinary tract symptom severity and associated bother between community-dwelling black and white men: the Olmsted County Study of Urinary Symptoms and Health Status and the Flint Men's Health Study. Urology. 2003;61:1086–91. doi: 10.1016/s0090-4295(03)00154-7. [DOI] [PubMed] [Google Scholar]
- 12.Griebling TL. Urinary Tract Infection in Women. In: Litwin MS, Saigal CS, editors. Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Washington, DC: US Government Publishing Office; 2004. pp. 587–619. NIH Publication No. 04-5512. Also accessible at www.uda.niddk.nih.gov. [Google Scholar]
- 13.Griebling TL. Urinary Tract Infection in Men. In: Litwin MS, Saigal CS, editors. Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Washington, DC: US Government Publishing Office; 2004. pp. 621–645. NIH Publication No. 04-5512. Also accessible at www.uda.niddk.nih.gov. [Google Scholar]
- 14.Anger JT, Saigal CS, Litwin MS. The prevalence of urinary incontinence among community dwelling adult women: results from the National Health and Nutrition Examination Survey. J Urol. 2006;175:601–4. doi: 10.1016/S0022-5347(05)00242-9. [DOI] [PubMed] [Google Scholar]
- 15.Anger JT, Saigal CS, Stothers L, Thom DH, Rodriguez LV, Litwin MS. The prevalence of urinary incontinence among community dwelling men: results from the National Health and Nutrition Examination survey. J Urol. 176:2103–8. doi: 10.1016/j.juro.2006.07.029. discussion 2108, 2006. [DOI] [PubMed] [Google Scholar]
- 16.Stothers L, Thom DH, Calhoun EA. Urinary Incontinence in Men. In: Litwin MS, Saigal CS, editors. Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Washington, DC: US Government Publishing Office; 2004. pp. 193–222. NIH Publication No. 04-5512. Also accessible at www.uda.niddk.nih.gov. [Google Scholar]
- 17.Nygaard I, Thom DH, Calhoun EA. Urinary Incontinence in Women. In: Litwin MS, Saigal CS, editors. Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Washington, DC: US Government Publishing Office; 2004. pp. 157–192. NIH Publication No. 04-5512. Also accessible at www.uda.niddk.nih.gov. [Google Scholar]
- 18.Sohn MW, Zhang H, Taylor BC, Fischer MJ, Yano EM, Saigal C, Wilt TJ. Prevalence and trends of selected urologic conditions for VA healthcare users. BMC Urol. 2006;6:30. doi: 10.1186/1471-2490-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]