Abstract
The efficacy of two topical treatments for painful ulcerative stage (M2) of bovine digital dermatitis (BDD) lesions was compared in a clinical trial conducted on five dairy farms in 2009 to 2010. The first treatment was a water-based gel with active components copper and zinc (Intra Hoof-fit gel [IHF]) and the second treatment was a topical chlortetracycline spray (CTC spray). The experimental unit for this study was the hindleg with the presence of a BDD lesion. Cure was defined as the transition of an M2 lesion into a healed (M0) or a non-painful chronic stage (M4) of BDD at D28. On day 0, cows with M2 BDD lesions were photographed and were treated with either IHF or CTC. Subsequently, feet were photographed and scored on D28. The cure rate of M2 BDD lesions treated with IHF at D28 was 0.92 (CI 0.84 to 0.96) and was significantly better than for M2 BDD lesions treated with CTC, which was 0.58 (CI 0.47 to 0.68).
BOVINE digital dermatitis (BDD) was first described as a clinical condition in 1974 (Cheli and Mortellaro 1974). It appears to have been a ‘true’ emerging disease as no reference had been made to the clinical condition before. The disease is found in housed Holstein-Friesian dairy cows worldwide and is considered an important cause of infectious lameness (Manske and others 2002b, Holzhauer and others 2006, Cramer and others 2008). BDD lesions typically develop on the plantar epidermis of the hindfeet. The ulcerative stage (M2), especially, tends to be very painful. Hence, BDD has been identified as a major welfare concern (Cornelisse and others 1981, Blowey and Sharp 1988). In addition to the improvement of hygienic measurements, optimization of cubical sizes, prevention of overcrowding and regular preventive claw trimming (Wells and others 1999) and rapid and effective treatment of infectious stages, it is necessary to prevent transmission of BDD within a herd. The main causal factor of BDD is infection with Treponema species (Evans and others 2011). The most effective therapeutical treatments use antibiotics (Manske and others 2002a, Nishikawa and Taguchi 2008, Berry and others 2010). Worldwide, there is a call for reduction of use of antibiotics in veterinary medicine (Phillips and others 2004). Although the quantities of antibiotics used in topical treatments of BDD are limited, an alternative would be welcome. The objective of this study was to evaluate the therapeutic effect of Intra Hoof-fit gel (IHF; Intracare b.v.) on M2 BDD lesions, in comparison with chlortetracycline spray (CTC; Eurovet), based on the antibiotic CTC.
Material and methods
Participating herds and dairy cows
The trial was conducted on five commercial dairy farms in the northern part of the Netherlands (see Table 1). All herds participated in biannual routine claw trimming programmes and started their participation in the trial over time. Cows were selected based on regular visits by the claw trimmer. A next planned regular claw trimming was the starting day per herd. Selection criteria for participation of dairy farms were as follows: BDD prevalence >20 to 25 per cent, as assessed during regular previous claw trimming; herd size over 90 lactating dairy cows; free stall with slatted floors and dairy cows of the Holstein-Friesian breed.
Table 1.
Information of the participating dairy herds in the clinical trial
| Herd | Start | End | Number of cows | Number of hindlegs in the trial | Floor |
|---|---|---|---|---|---|
| 1 | September 2009 | October 2009 | 116 | 39 | Slats |
| 2 | October 2009 | December 2009 | 170 | 59 | Slats with scraper |
| 3 | November 2009 | December 2009 | 90 | 10 | Slats |
| 4 | December 2009 | January 2010 | 132 | 20 | Slats |
| 5 | January 2010 | March 2010 | 183 | 54 | Slats with scraper |
All lactating cows with M2 BDD lesions (M2) in their hindfeet at one of these regular claw trimming visits were included in the trial.
Study design and treatments
The trial was designed as a case-control study in which treatment with IHF was compared with treatment with CTC, which is an officially registered product, and this was treated as a positive control. A positive control was chosen for animal welfare reasons as not to deny animals treatment of the painful M2 stage of BDD. All BDD lesions were dry cleaned, macroscopically classified and recorded at D0 and D28. Classification of BDD was performed according to a standardised scoring system comprising five stages (M0 to M4) as developed by Döpfer and others (1997). According to this scoring system, M0 is recorded for feet with normal digital skin where BDD is absent during macroscopic inspection; M1 is the early-stage lesion (0 to 2 cm) that is not painful; M2 is the classical ulcerative stage with a diameter >2 cm that is often painful upon touch; M3 is the healing stage when the lesion is covered by a scab and M4 is the chronic stage characterised by dyskeratosis or proliferation of the surface that is generally not painful. M2 is the most infectious stage (Mumba and others 1999). If different stages of BDD were present, the leg was typed according to the most prominent stage of the lesion. Besides scoring of the lesions, attention was paid to the presence of adverse or side effects with specific attention for redness and swelling of the treated skin. On D0, the first M2 lesion found in a herd was assigned as treatment group A or B by flipping a coin. Subsequent lesions were alternately assigned to group A or B.
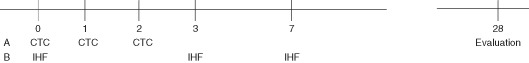
In group A, 5 g of IHF was applied with a brush. The lesion was then covered with cotton wool and held in place by an elastic bandage (CoRip Flexible Cohesive Bandage GB 11). On D3 and D7, again approximately 5 g of IHF was applied by use of a brush, but without a bandage (see time frame, Fig 1). In group B, CTC was applied by spraying twice for three seconds from 15 to 20 cm distance with 30 seconds in-between treatments. This treatment was, accordingly the prescription of the producers,repeated at days 1 and 2. All scores, recordings and treatments were performed in a trimming chute by the same veterinarian (MvB). All hindlegs with M2 lesions were photographed at D0 and D28 for objective evaluation afterwards. No walk-through footbaths or other treatments were applied in the last three weeks before the start of and during the trial period. For reasons of practical feasibility, performance in regular herds and for financial reasons, no further histopathological investigation of the lesions was performed. Daily evaluations were performed by the dairy farmer for the presence of painful lesions. In case of necessary extra treatments, these were always executed with CTC (the registered product). These lesions were not followed up any further and were considered not to be cured. Cows that were treated for other reasons during the trial (eg, mastitis) were excluded.
Fig 1.
Time frame for scorings and treatments of the different products according to protocol
Statistical analysis
The experimental unit was a hindleg with an M2 BDD lesion. Cure was defined as the transition of M2 BDD into a healed (M0) or non-painful chronic stage (M4) at D28. The sample size was calculated to detect a 10 per cent difference between the cure rate of CTC (80 per cent, Holzhauer and others 2008) and IHF (70 per cent; Moore and others 2001) with 95 per cent confidence and 80 per cent power. Based on these assumptions, a sample size of 300 hindlegs with M2 lesions in each group was needed. A Kruskal-Wallis test was used for comparison of the different treatment groups for parity, days in milk and milk yield, where the results might be influenced by these criteria (Holzhauer and others 2006).
A two-sample, two-sided proportion test was used to compare the cure rate of IHF with CTC. Data were analysed in STATA/SE 10.0 comparing the proportions of cured M2 lesions, 28 days after the initial treatment, in cows treated with IHF or CTC. Finally, a Fisher exact test was used to evaluate the transitions from M2 to M0 at D7 for the different treatment groups and a proportion test was used to evaluate the transitions from M2 to M0 at D21 and D28 for the different treatment groups (p-value <0.05).
Results
In total, 205 hindfeet (divided over 172 cows) were treated, 103 with IHF and 102 with CTC. Because the outcomes of the comparison differed considerably from the assumptions, these were less than the 300 hindlegs calculated to be necessary for each group. The study was stopped after executing the trial in five herds where 49, 64, 13, 20 and 59 hindfeet were treated. The comparison of the IHF and CTC group made for parity, days in milk and milk yield were not statistically different (p values were, respectively, 0.48, 0.18 and 0.27).
In 18 dairy cows (23 hindfeet, nine IHF and 14 CTC), the protocol could not be fully executed, for different reasons. The most dominant reason was an extra treatment with CTC, due to a painful lesion (eight hindfeet, all belonging to the CTC group). This represented 8 per cent of the cows treated with CTC. For medical reasons, five cows (3x mastitis, 1x fractured leg and 1x serious sole ulcer) were culled by the farmers. Results of six hindfeet had to be excluded, due to scoring and/or administrative mistakes. The M2 BDD cure rates of IHF and CTC are presented in Tables 2 and 3. The cure rate of M2 BDD lesions treated with IHF was 0.92 (86/94, CI 0.84 to 0.96) and with CTC 0.58 (51/88, CI 0.47 to 0.68), indicating a risk ratio (RR) of 1.58 (95 per cent CI 1.31 to 1.91). The RR per herd was more than unity for IHF over CTC (four out of five herds) and differed statistically significant in three out of five herds (see Tables 2 and 3). In herd 4, the cure rate for IHF was 0.90 and for CTC 1.00. On D7, all M2 (from Day 0) had become non-M2 for IHF compared with 32 remained M2 for CTC (p <0.01). On day 21, 21 per cent were M0 for IHF compared with 2 per cent for CTC and on D28, 51 per cent have become M0 for IHF compared with 10 per cent for CTC (p <0.01).
Table 2.
Estimation of the overall cure at D28 of M2 BDD lesions treated for the different herds and overall
| Number CTC treated | CTC M2 cured* | Cure rate CTC | IHF treated | IHF M2 cured | Cure rate IHF | Cure rate difference | p-Value (Fisher exact test) | |
|---|---|---|---|---|---|---|---|---|
| Herd 1 | 16 | 7 | 0.44 | 23 | 23 | 1.00 | 2.7 | 0.01 |
| Herd 2 | 30 | 18 | 0.60 | 29 | 25 | 0.86 | 1.4 | 0.04 |
| Herd 3 | 4 | 3 | 0.75 | 6 | 6 | 1.00 | 1.3 | 0.4 |
| Herd 4 | 10 | 10 | 1.00 | 10 | 9 | 0.90 | 0.9 | 1.00 |
| Herd 5 | 28 | 13 | 0.46 | 26 | 23 | 0.88 | 1.9 | <0.01 |
| Total | 88 | 51 | 0.58 | 94 | 86 | 0.92 | 1.6 | <0.01 |
All transitions from painful M2 lesions to M0, 1, 3 and 4
CTC Chlortetracycline spray, IHF Intra Hoof-fit gel
Table 3.
Scoring of DD lesions on D7, D21 and D28 after treatment of M2 BDD with IHF and CTC spray
| M0 | M1 | M2 | M3 | M4 | ||
|---|---|---|---|---|---|---|
| Day 7 | IHF | 0 | 30 | 0 | 67 | 0 |
| CTC | 0 | 10 | 32 | 56 | 0 | |
| Day 21 | IHF | 20 | 54 | 2 | 17 | 1 |
| CTC | 2 | 45 | 37 | 11 | 1 | |
| Day 28 | IHF | 48 | 32 | 8 | 2 | 4 |
| CTC | 9 | 37 | 37 | 1 | 4 |
CTC Chlortetracycline spray, IHF Intra Hoof-fit gel, M0 Healed stage, M1 Early-stage lesion,
M2 Ulcerative stage, M3 Healing stage, M4 Chronic stage
Discussion
Individual topical treatment with antibiotics is the most commonly reported method to treat BDD (Laven and Logue 2007). This is widely accepted as the treatment of choice because it is generally accepted as effective and there is a lack of scientific information on the efficacy of non-antibiotic preparations. Topical treatment has the advantage of limited antibiotic usage and it also fulfils the requirements of legislation. However, alternatives for all antibiotic treatments are desirable, because of reasons of possible development of antibiotic resistance and environmental pollution (Tacconelli 2010). In the UK, Pastell and others (2010) found no relationship between lameness and the presence of BDD. In that study, however, BDD was not classified based on the stage of infection. Laven and Hunt (2002) evaluated the effect of two topical antibiotic sprays (with valnemulin and lincomycin) in the treatment of BDD. At D14, a significant reduction in lesion score for both treatment groups was found with cure rates of 28 and 40 per cent. Laven (2006) studied the efficacy of two antibiotics, cefquinome applied parenterally for three days and for five days and erythromycin applied parenterally by injection once. He also compared the results with erythromycin in a walk-through footbath. Only M2 BDD lesions were included in that study. The results of all treatments were comparable with the erythromycin footbath application; only the five-day application of cefquinome had a significantly better result. Unfortunately, the best strategy (five days application) is not only expensive, but also has a higher risk of development of resistance against modern antibiotics, by the increased use of a third-generation cephalosporine. Therefore, this strategy is less desirable. Recently, Potter and Burnell (2010) compared the curative effect of a copper/zinc and aloe vera gel as treatment of M2 BDD lesions, with an antibiotic powder (tylosin tatrate) on 41 foots. At D7, a lesion surface area reduction of 74 per cent was found after treatment with the gel while the antibiotic treatment gave a 48 per cent reduction. The copper/zinc gel used in that study is comparable with the gel used in our study and the results are in line with this study. In the USA, Britt and others (1996) studied the efficacy of three topical sprays (oxytetracycline, acidified ionised copper solution and acidified sodium chlorite solution) on lameness three weeks after treatment. Mean lameness score decreased (that is, cows were less lame) for all three treatment groups but increased for the control group. Berry and others (1999) evaluated the efficacy of a Serpens species bacterin vaccine combined with topical administration of lincomycin HCl for the treatment of the M2 BDD in 30 cows. All cows in that study were examined on D30 and D110 and a cure rate of approximately 60 per cent was found in both groups. Shearer and Hernandez (2000) compared the efficacy of a topical treatment with oxytetracycline solution with the efficacy of a product containing reduced soluble copper and a peroxide compound with increased levels of cationic agent, among 78 dairy cows with M2 BDD. Based on the lesion scores at D28, the copper product appeared most effective for the treatment of BDD. The too low efficacy of the oxytetracycline solution (only 20 per cent cure at D28) was hypothesised by them to be an indication of possible antibiotic resistance. Moore and others (2001) studied the efficacy of treating M2 BBD with a non-antimicrobial cream (soluble copper with peroxide and a cationic agent) in comparison with a lincomycin HCl paste and a negative control group in 98 cows. At D28, the percentage of healed lesions for the different therapies was 45.5, 64.5 and 21.9 per cent and the RR of cure compared with no treatment was 2.08 and 2.95. In a recent study in the USA (Berry and others 2010), the efficacy of lincomycin and oxytetracycline for topical treatment of BDD was examined via gross visual examination, histological evaluation and bacteriologic evaluation in 25 dairy cows with ulcerative BDD. No difference between responses to lincomycin and oxytetracycline were found (73 and 68 per cent, respectively).
In most studies on topical antibiotic treatments, cure rates at D30 around 60 to 70 per cent are found, except in the study of Shearer and Hernandez (2000). Data in the present study indicated that the curative effect of IHF at D28 after the start of treatment was 92 per cent, which is better than antibiotic treatment in other studies (Table 2). Table 3 gives a more detailed insight and it shows that (for IHF) at D7 all lesions were cured (≠M2), but at a later stage some M2 lesions re-occur, where it is not clear if it is reinfection or reoccurrence of a non-healed lesion. The curative effect of topical application of CTC in the present study was in line with cure rates of antibiotics applied topically on BDD lesions in other studies. Thus, the application of IHF seems to be a good alternative for antibiotic treatment of M2 BDD lesions. Although copper and zinc are considered to be toxic for the environment, copper/zinc pollution seems to be limited due to a limited number of individual cows per herd and the amount of gel applied (<5 g) and is expected to have a very limited influence on the environment.
In conclusion, the use of topical IHF gel under a bandage at D0 and additional application at D4 and D7 (without bandage) were effective for the treatment of the M2 stage of BDD and were significantly better than three consecutive days of topical treatment with CTC.
Acknowledgments
We acknowledge the participation and assistance of the dairy farmers and the claw trimmers of ‘Veepedicure Centrum Noord Nederland’ for their patience and accurate trimming of the dairy cows. This study was funded by Intracare b.v., Veghel, The Netherlands.
Footnotes
Provenance not commissioned; externally peer reviewed
References
- Berry S. L., Read D. H., Walker R. L., Famula T. R. (2010) Clinical, histologic, and bacteriologic findings in dairy cows with digital dermatitis (footwarts) one month after topical treatment with lincomycin hydrochloride or oxytetracycline hydrochloride. Journal of the American Veterinary Medical Association 237, 555–560 [DOI] [PubMed] [Google Scholar]
- Berry S. L., Graham T. W., Mangini A., Arana M. (1999) The efficacy of Serpens spp. bacterin combined with topical administration of lincomycin HCl for treatment of (papillomatous) digital dermatitis in cows on a dairy in California. Bovine Practitioner 33, 6–11 [Google Scholar]
- Blowey R. W., Sharp M. W. (1988) Digital dermatitis in dairy cattle. Veterinary Record 122, 505–508 [DOI] [PubMed] [Google Scholar]
- Britt J. S., Gaska J., Garrett E. F., Konkle D., Mealy M. (1996) Comparison of topical application of three products for treatment of papillomatous digital dermatitis in dairy cattle. Journal of Veterinary Medical Association 209, 1134–1136 [PubMed] [Google Scholar]
- Cheli R., Mortellaro C. M. (1974) La Dermatite Digitale del Bovino. Proceedings of the Eighth International Conference on Diseases of Cattle. Milan, Italy: pp 208–13 [Google Scholar]
- Cramer G., Lissemore K. D., Guard C. L., Leslie K. E., Kelton D. F. (2008) Herd- and cow-level prevalence of foot lesions in Ontario dairy cattle. Journal of Dairy Science 91, 3888–3895 [DOI] [PubMed] [Google Scholar]
- Cornelisse J. L., Peterse D. J., Toussaint Raven E. (1981) [A digital disorder in dairy cattle. Dermatitis digitalis? (author's transl)]. Tijdschrift Voor Diergeneeskunde 106, 452–455 [PubMed] [Google Scholar]
- Döpfer D., Koopmans A., Meijer F. A., Szakáll I., Schukken Y. H., Klee W., Bosma R. B., Cornelisse J. L., van Asten A. J., ter Huurne A. A. H. M. (1997) Histopathological and bacteriological evaluation of digital dermatitis in cattle, with special reference to Spirochaetes and Campylobacter faecalis. Veterinary Record 140, 620–623 [DOI] [PubMed] [Google Scholar]
- Evans N. J., Brown J. M., Murray R. D., Getty B., Birtles R. J., Hart C. A., Carter S. D. (2011) Characterization of novel bovine gastrointestinal tract Treponema isolates and comparison with bovine digital dermatitis treponemes. Applied and Environmental Microbiology 77, 138–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzhauer M., Bartels C., Döpfer D., Schaik G. v. (2008) Clinical course of digital dermatitis lesions in an endemically infected herd without preventive herd strategies. Veterinary Journal 177, 222–230 [DOI] [PubMed] [Google Scholar]
- Holzhauer M., Hardenberg C., Bartels C. J., Frankena K. (2006) Herd- and cow-level prevalence of digital dermatitis in the Netherlands and associated risk factors. Journal of Dairy Science 89, 580–588 [DOI] [PubMed] [Google Scholar]
- Laven R. A., Hunt H. (2002) Evaluation of copper sulphate, formalin and peracetic acid in footbaths for the treatment of digital dermatitis in cattle. Veterinary Record 151, 144–146 [DOI] [PubMed] [Google Scholar]
- Laven R. A. (2006) Efficacy of systemic cefquinome and erythromycin against digital dermatitis in cattle. Veterinary Record 159:19–20 [DOI] [PubMed] [Google Scholar]
- Laven R. A., Logue D. N. (2007) Treatment strategies for digital dermatitis for the UK. Veterinary Journal 171, 79–88 [DOI] [PubMed] [Google Scholar]
- Manske T., Hultgren J., Bergsten C. (2002a) Topical treatment of digital dermatitis associated with severe heel-horn erosion in a Swedish dairy herd. Preventive Veterinary Medicine 53, 215–231 [DOI] [PubMed] [Google Scholar]
- Manske T., Hultgren J., Bergsten C. (2002b) Prevalence and interrelationships of hoof lesions and lameness in Swedish dairy cows. Preventive Veterinary Medicine 54, 247–263 [DOI] [PubMed] [Google Scholar]
- Moore D. A., Berry S. L., Truscott M. L., Koziy V. (2001) Efficacy of a nonantimicrobial cream administered topically for treatment of digital dermatitis in dairy cattle. Journal of the American Veterinary Medical Association 219, 1435–1438 [DOI] [PubMed] [Google Scholar]
- Mumba T., Döpfer D., Dreher M., Gaastra W., van der Zeijst B.A. (1999) Detection of spirochetes by polymerase chain reaction and its relation to the course of digital dermatitis after local antibiotic treatment in dairy cattle. Zentralblatt Veterinarmedicin B. 46, 117–126 [DOI] [PubMed] [Google Scholar]
- Nishikawa A., Taguchi K. (2008) Healing of digital dermatitis after a single treatment with topical oxytetracycline in 89 dairy cows. Veterinary Record 163, 574–576 [DOI] [PubMed] [Google Scholar]
- Pastell M., Hänninen L., De Passillé A. M., Rushen J. (2010) Measures of weight distribution of dairy cows to detect lameness and the presence of hoof lesions. Journal of Dairy Science 93, 954–960 [DOI] [PubMed] [Google Scholar]
- Phillips I., Casewell M., Cox T., De Groot B., Friis C., Jones R., Nightingale C., Preston R., Waddell J. (2004) Does the use of antibiotics in food animals pose a risk to human health? A critical review of published data. Journal of Antimicrobial Chemotherapy 53, 28–52 [DOI] [PubMed] [Google Scholar]
- Potter S., Burnell M. (2010) Comparison of a non-antibiotic gel with antibiotic powder for the treatment of digital dermatitis. Proceedings of the Cattle Lameness Conference. Sutton Bonington, April 14, 2010 pp 47–48 [Google Scholar]
- Shearer J. K., Hernandez J. (2000) Efficacy of two modified non-antibiotic formulations (Victory) for treatment of papillomatous digital dermatitis in dairy cows. Journal of Dairy Science 83, 741–745 [DOI] [PubMed] [Google Scholar]
- Tacconelli E. (2009) Antimicrobial use: risk driver of multidrug resistant microorganisms in healthcare settings. Current Opinion in Infectious Diseases 22, 352–358 [DOI] [PubMed] [Google Scholar]
- Wells S. J., Garber L. P., Wagner B. A. (1999) Papillomatous digital dermatitis and associated risk factors in US dairy herds. Preventive Veterinary Medicine 38, 11–24 [DOI] [PubMed] [Google Scholar]