Abstract
On five commercial cattle rearing sites across Europe, a total of 802 young cattle at high risk of developing bovine respiratory disease (BRD) associated with the bacterial pathogens Mannheimia haemolytica or Pasteurella multocida and/or Mycoplasma bovis were enrolled into a multicentre, controlled field trial. Half were treated with a single dose of gamithromycin at 6 mg/kg bodyweight by subcutaneous injection and half received an injection of a saline placebo as the control. All animals were observed daily for 14 days for signs of BRD as defined by set criteria. The proportion of metaphylactic preventive treatment successes, defined as animals surviving to day 14 without signs of BRD, in the gamithromycin-treated group (86 per cent) was significantly (P=0.0012) higher than in the saline-treated controls (61 per cent). Morbidity among the treated animals was reduced by 64 per cent compared with the controls.
THE conditions in which young, confined cattle are kept during the rearing process are conducive to the colonisation and proliferation of pathogens that cause bovine respiratory disease (BRD) (Bryson 2000, Macartney and others 2003, Radostits and others 2007). Typical microorganisms associated with BRD include bacteria (Mannheimia haemolytica, Pasteurella multocida and Histophilus somni), Mycoplasma speciesand viruses (parainfluenza virus type 3, bovine respiratory syncytial virus, bovine viral diarrhoea virus and bovine herpesvirus type 1 [the cause of infectious bovine rhinotracheitis]) (Bryson 2000, Valarcher and Hagglund 2006).
Although BRD is multifactorial in its pathogenesis, morbidity and mortality are usually the result of the pathophysiological responses to colonisation of the respiratory tract by pathogenic bacteria, such as M haemolytica, P multocida and H somni and Mycoplasma species (Mosier 1997), hence the value of antibiotic therapy. The antibacterial agent gamithromycin was developed exclusively for veterinary use as a single dose, 150 mg/ml subcutaneous injectable solution (Zactran; Merial) for the therapeutic and preventive control of BRD associated with M haemolytica, P multocida and H somni. Gamithromycin is a novel semisynthetic macrolide of the azalide subclass. As for the macrolides in general, gamithromycin has a bacteriostatic action through inhibition of bacterial RNA-dependent protein synthesis, but based on in vitro studies it also can act in a bactericidal manner at concentrations that are reached in lung tissue (Retsema and others 1990, Jain and Danziger 2004). The macrolides generally, and the azalides even more so, achieve high concentrations for extended periods in the tissues, particularly lung tissue, compared with their concentrations in plasma (Bryskier and Bergogne-Berezin 1999). They also accumulate readily in host defence cells, including polymorphonuclear leucocytes and macrophages, and readily distribute into extracellular fluid (Mattoes and Nightingale 2002). Gamithromycin shares the dose distribution and pharmacokinetic properties of the azalides (Huang and others 2009). Coupled with its potent bactericidal activity, these properties make gamithromycin a strong candidate antibiotic for the treatment and control of BRD.
This paper describes a multicentre, randomised, controlled field trial designed to evaluate the efficacy of gamithromycin for the preventive treatment of BRD in Europe by comparing gamithromycin-treated cattle with placebo-treated cattle.
Materials and methods
The trial was conducted in accordance with Good Clinical Practice guidelines (Anon 2000) for veterinary product development with the informed consent of the owners of the cattle involved. Five commercial cattle rearing units – one site in France and two sites in each of Germany and Italy – were included. A total of 802 male and female ruminating and younger, preruminating cattle were enrolled in the trial (Table 1). All had been recently assembled and/or commingled with other cattle into loose-housed pens. Routine disease control measures were similar for all animals at a trial site and were limited to administration of (but not necessarily any or all of) viral respiratory vaccines, endectocides and flukicides for the control of internal and external parasites, before or after arrival at the trial sites. None of the animals had received bacterial vaccines for BRD within the previous six months, or antimicrobials within 30 days before enrolment. To minimise bias in the trial results, the investigators and all personnel performing post-treatment evaluations were masked to the treatment assignment of the animals.
Table 1.
Details of cattle at five sites used in a trial of the efficacy of gamithromycin in preventing clinical bovine respiratory disease
| Number enrolled and treated | Number included in efficacy analysis | ||||||
|---|---|---|---|---|---|---|---|
| Trial site | G* | Control† | Breeds | Age (months) | Weight (kg) | G | Control |
| France | 43 | 44 | CH, CC, L, BA, CB | 7-23 | 152-582 | 42 | 43 |
| Germany 1 | 60 | 60 | FV | <1-2 | 73-139 | 60 | 60 |
| Germany 2 | 63 | 63 | FV | <1-3 | 54-88 | 61 | 63 |
| Italy 1 | 121 | 121 | CH, CC | 7-18 | 198-390 | 121 | 121 |
| Italy 2 | 113 | 114 | S, A, L, CH, CC | 4-18 | 200-430 | 113 | 114 |
| Total | 400 | 402 | <1-23 | 54-582 | 397 | 401 | |
Treated with a single dose of 150 mg/ml gamithromycin injectable solution at 6 mg/kg (2 ml/50 kg) bodyweight
Treated with a single injection of sterile 0.9 per cent saline solution at 2 ml/50 kg bodyweight
A Aubrac, BA Blonde d'Aquitaine, CB Crossbred, CC Charolais cross, CH Charolais, FV Fleckvieh (German Simmental), L Limousin, S Saler
At the time of enrolment in the trial, all animals included were considered healthy but with a high risk of BRD, on the basis that at least 10, equivalent to 5 per cent or more, of the cattle within the same airspace at each site had presented with clinical signs of BRD (depression score >0, abnormal respiration score >0 and rectal temperature 40.0°C or more [Fig 1])over the previous 48 to 72 hours, and with M haemolytica, P multocida and/or Mycoplasma bovis isolated on nasopharyngeal swabs (Table 2). Animals presenting with BRD before the start of the trial were treated according to their therapeutic needs with non-test drugs.
Fig 1.
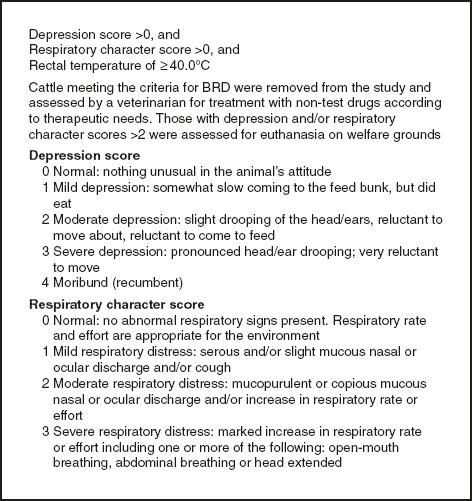
Clinical criteria of bovine respiratory disease (BRD)
Table 2.
Pre-enrolment incidence (%) of bovine respiratory disease (BRD) and isolations of causative bacterial and mycoplasmal pathogens at the five trial sites, and in vitro minimum inhibitory concentration (MIC) of gamithromycin of the isolates
| Number of animals | ||||||||
|---|---|---|---|---|---|---|---|---|
| Number of samples positive for pathogens (MIC gamithromycin range [µg/ml]) | ||||||||
| Trial site | Number of animals in airspace | Number (%) with BRD | Sampled (nasal swabs) | Positive for BRD pathogens | Pm | Mh | Hs | Mb |
| France | 97 | 10 (10.3) | 8 | 2 | 0 | 2 (1.0) | 0 | 1 |
| Germany 1 | 93* | 18 (19.4) | 18 | 12 | 5 (0.125-2.0 | 8 (0.5-1.0) | 0 | 4 |
| Germany 2 | 279 | 34 (12.2) | 34 | 15 | 9 (0.25-2.0) | 2 (0.5-2.0) | 0 | 7 |
| Italy 1 | 281 | 34 (12.1) | 34 | 22 | 0 | 2 (1.0) | 0 | 22 |
| Italy 2 | 249 | 22 (9.0) | 22 | 12 | 0 | 12 (not tested) | 0 | 0 |
| Total | 116 | 63 | 14 (0.125-2.0) | 26 (0.5-2.0) | 0 | 34 (>16)† | ||
Additional study animals were added to the airspace after nasal swabs were collected
MIC range based on one randomly selected isolate per trial site
Hs Histophilus somni, Mb Mycoplasma bovis, Mh Mannheimia haemolytica, Pm Pasteurella multocida
At each site, all animals were maintained within the same airspace in naturally ventilated or controlled environment buildings and in compliance with EU animal welfare regulations. After the trial, all gamithromycin-treated animals were held at the respective trial sites until they had fulfilled the locally approved investigational meat withdrawal period for gamithromycin. Continuous exposure of enrolled animals to BRD pathogens was ensured throughout the trial by the presence of target pathogen carriers in the form of saline-treated control cattle and cattle that were not enrolled in the trial maintained in the same airspace as the gamithromycin-treated cattle.
Trial conduct
At each trial site, once BRD cases had been confirmed within the airspace occupied by the trial animals, cattle that were apparently healthy (those with depression and respiratory character scores of 0; Fig 1) were paired in order of presentation within groups of animals of similar bodyweight. Animals within each pair were randomly allocated to one of two treatment groups. All enrolled cattle were treated by subcutaneous injection on the same day (day 0) at each trial site: one group with 150 mg/ml gamithromycin solution at 6 mg gamithromycin/kg bodyweight, and the other group with 0.9 per cent sterile saline solution at 2 ml/kg bodyweight, as the control. Both treatment groups were commingled at all sites.
Animals were observed daily from the day of treatment for 14 days for signs of BRD and general health. During these health observations, a clinical assessment of each animal was made to determine its BRD status, based on depression and respiratory character scores and the rectal temperature (Fig 1). Following treatment with gamithromycin or saline, enrolled cattle were removed from the study and treated as necessary with appropriate non-test drugs according to their therapeutic needs if they were diagnosed with BRD. Cattle were diagnosed with BRD if they fulfilled the clinical criteria of BRD (depression score >0, respiratory character score >0 and rectal temperature ≥40.0°C) (Fig 1) for one day, or they showed clinical signs of BRD which, while not fulfilling all the clinical criteria of BRD, were considered severe enough by the attending veterinarian to justify removal on welfare grounds starting on day 1 (the day following treatment).
The trial monitoring period of 14 days was selected on the basis of an anticipated duration of antibacterial effect of gamithromycin of up to 15 days (depending on pathogen susceptibility) as estimated from pharmacokinetic, minimum inhibitory concentration (MIC) and total lung concentration data (Huang and others 2009).
Microbiology
At each trial site, before animals were enrolled, two nasopharyngeal samples were collected using sheathed, 20 to 27 cm long swabs (Medical Wire & Equipment) from each animal displaying clinical signs of BRD to confirm that the incidence of BRD at the site was 5 per cent or more. The swabs were cultured to confirm the presence of the target BRD pathogens in the proposed study populations. The swabs were placed in appropriate transport media for the target pathogens, that is, one for culture of M bovis into mycoplasma transport medium (Mycoplasma Experience) and the other for culture of M haemolytica, P multocida and H somni into Amies charcoal transport medium (Medical Wire & Equipment), and cultured and identified using standard procedures (Quinn and others 2002). M bovis isolates were identified by culturing on a M bovis diagnostic agar medium (Mycoplasma Experience) containing 2,3,5-triphenyl tetrazolium chloride to produce red-centred colonies for M bovis only. Confirmed isolates of each pathogen were tested for in vitro susceptibility to gamithromycin (except for M bovis, where only one isolate per trial site was tested) using broth dilution techniques, including quality control reference strains, to determine the MIC of gamithromycin (Table 2).
Data analysis
Data from each site separately and all sites combined were analysed to determine the efficacy of gamithromycin. It was considered appropriate to combine the data for ruminating and preruminating cattle from all sites because of similar gamithromycin pharmacokinetic profiles (Anon 2008) and BRD pathogenesis in both age groups.
On day 14, a treatment success was declared for cattle that were not diagnosed with BRD. Cattle that were removed from the trial for reasons other than BRD were not considered in the analysis of treatment success. The pivotal determinant of preventive efficacy was the proportion of BRD prevention treatment successes on day 14 in the gamithromycin-treated group compared with the saline-treated control group. For each individual site, the proportion of treatment successes on day 14 was compared between the gamithromycin-treated group and controls by Fisher's exact test. The proportion of treatment successes on day 14 combined across all sites was analysed by a generalised linear model with a logit link function and a binomial distribution, where model factors included treatment as a fixed effect, and site and treatment by site interaction as random effects. A two-sided significance level of 0.05 was used for all analyses, which were performed using the procedures of SAS Version 8.2 (SAS Institute).
Results
During the trial, no animals died as a result of BRD, and no adverse events considered to be related to the gamithromycin treatment occurred. Two gamithromycin-treated animals and one saline-treated control animal were removed from the trial on welfare grounds for reasons not related to BRD (abdominal colic and non-specific enteritis), and thus were excluded from the analysis of preventive treatment success. One animal at the site in France was unintentionally underdosed and was also excluded from the data analysis. Consequently, datasets from 397 animals treated with gamithromycin and 401 treated with saline were available for the analysis of preventive treatment success.
The pre-enrolment isolations of intranasal BRD pathogens at the trial sites are shown in Table 2. The ranges of MICs of gamithromycin determined for the isolates of each BRD pathogen species are shown in Table 2.
The proportion of preventive treatment successes in the combined gamithromycin-treated groups (86 per cent) was significantly (P<0.002) higher than in the combined sterile saline-treated controls (61 per cent) (Table 3). The higher success rate in gamithromycin-treated cattle was statistically significant (P<0.0001) at all individual trial sites except the site in France, where the total number of animals was relatively low compared with the other sites, thus reducing the statistical power for the data from this site. The overall BRD morbidity in the trial population (equivalent to the percentage of BRD-affected cattle among the controls) was 39 per cent, ranging from 72 and 63 per cent, respectively, at the two sites in Germany to 26 to 28 per cent at the sites in Italy and France. Morbidity among the treated animals was lower overall by 64 per cent (32 to 82 per cent at individual sites) compared with the controls.
Table 3.
Efficacy of a single dose of gamithromycin in preventing bovine respiratory disease (BRD), shown as the number and proportion of treatment successes and the percentage morbidity, assessed 14 days after treatment
| Gamithromycin* | Control† | |||||
|---|---|---|---|---|---|---|
| Trial site | Number (%) of treatment successes | Morbidity‡ (%) | Number (%) of treatment successes | Morbidity (%) | Morbidity reduction (%) | P |
| France | 34/42 (81) | 19 | 31/43 (72) | 28 | 32 | 0.4444§ |
| Germany 1 | 41/60 (68) | 32 | 17/60 (28) | 72 | 56 | <0.0001§ |
| Germany 2 | 46/61 (75) | 25 | 23/63 (37) | 63 | 60 | <0.0001§ |
| Italy 1 | 113/121 (93) | 7 | 90/121 (74) | 26 | 73 | <0.0001§ |
| Italy 2 | 107/113 (95) | 5 | 82/114 (72) | 28 | 82 | <0.0001§ |
| Total | 341/397 (86) | 14 | 243/401 (61) | 39 | 64 | 0.0012∞ |
Gamithromycin 150 mg/ml injectable solution at 6 mg/kg (2 ml/50 kg) bodyweight
Sterile 0.9 per cent saline solution at 2 ml/50 kg bodyweight
Morbidity is the percentage of BRD cases in the control or gamithromycin-treated groups. Morbidity reduction is the ratio of morbidity in gamithromycin-treated cattle to controls
Probability from Fisher's exact test for the proportion of treatment success in the individual trial site in gamithromycin-treated versus saline-treated control groups
Probability from generalised linear model analysis for the proportion of treatment success in the combined gamithromycin-treated versus saline-treated control groups
Discussion
Based on clinical assessment, this trial showed that gamithromycin is effective in reducing the morbidity of bacterial BRD under field conditions in Europe when administered as a single subcutaneous preventive dose of 6 mg/kg bodyweight to cattle at high risk of developing BRD associated with M haemolytica, P multocida and/or M bovis.
Most isolates collected from cases of BRD at the trial sites before enrolment were considered susceptible to gamithromycin on the basis of the clinical outcomes, despite some M bovis isolate MICs being high (Table 2). It has been demonstrated that for macrolide antimicrobial compounds in particular, in vitro MIC sensitivity tests are greatly affected by methodological differences, such as the pH of the medium, variations in the medium and the inoculum size, with small increases in pH, for example, increasing the MIC by up to four times (Ben Ali and others 2002, Godinho and others 2005). Therefore, some macrolide MICs may be poor indicators of clinical efficacy, as appears to be the case for some M bovis isolates from this trial.
The morbidities in the control cattle at the two sites in Germany were higher (63 to 72 per cent) than at the other three sites (26 to 28 per cent). Also at the German sites, morbidities in the treated animals (25 to 32 per cent) were higher than at other sites (5 to 19 per cent) even though the reduction in morbidity in treated animals compared with controls was high at approximately 60 per cent. At these sites, the animals studied were young calves less than three months old and had a more diverse bacterial flora than older cattle at other sites (Table 2). The bacterial pathogens isolated from the sites in Germany were shown to be susceptible to gamithromycin by in vitro MIC testing (MIC 0.125 to 2.0 µg/ml) (Table 2), so it is assumed that the relatively high morbidity among the test animals in Germany reflected the greater susceptibility of younger animals to BRD and possibly the presence of non-susceptible respiratory pathogens, such as viruses, that were not identified.
The sites of bacterial multiplication and initial pathology for BRD pathogens are thought to be on the surface of bronchiolar and alveolar lining cells and in the adjacent pulmonary epithelial lining fluid (PELF) (Nightingale and Mattoes 2002). Although gamithromycin concentration measurements in whole lung homogenate, as reported by Huang and others (2009), do not provide a quantitative measure of the drug concentration in PELF, a further study (Giguère and others 2011) has reported rapid penetration of all lung tissues within 30 minutes of administration, with mean gamithromycin concentrations in calf PELF and associated cells peaking at 24 hours (4.6 and 17.8 µg/ml, respectively) and remaining above 0.5 µg/ml for at least seven days after treatment. It is probable, therefore, that the concentration of gamithromycin in PELF stays above the in vitro gamithromycin MIC 90 per cent (MIC90) for the principal target BRD pathogens (0.5 to 1.0 µg/ml) (Huang and others 2009) beyond seven days after treatment. The efficacy due to the extended duration of high levels of gamithromycin in PELF is further enhanced by the long postantibiotic effect (the duration of antibacterial effects in vitro after removal of the antibiotic) of up to eight hours, which is typical of modern macrolides (Diarra and others 1999).
In most regions of the world, there are strong initiatives in place to encourage the responsible use of antimicrobials in veterinary practice (European Platform for the Responsible Use of Medicines in Animals 2008, British Veterinary Association 2009). The use of antibiotics in the control of BRD can be broadly classified as either therapeutic, in which animals with clinical disease are treated, or preventive, when groups of animals are treated before the onset of disease in order to limit the potential impact of BRD. Preventive approaches can be further subdivided into prophylactic, when antibiotics are administered before the appearance of clinical disease to groups of cattle judged to be at high risk of developing BRD, and metaphylactic, in which antibiotics are administered to cohorts of apparently healthy animals that are in contact with clinical cases (Brumbaugh 2009). Using these definitions, the present study involved a metaphylactic approach. While the decision by veterinarians to adopt any of these approaches rests on numerous considerations, one of the most important is the welfare of the animals under their care. A therapeutic approach will generally result in the lowest level of antibiotic usage, but this requires a high level of stockmanship in order to detect BRD in its early stages, and adequate labour and facilities with which to handle, examine and treat the affected animals promptly, if their welfare is not to be compromised. When determining what approach should be used, the relative risk of infection and its consequences must be sufficient to outweigh the risks associated with using an antimicrobial drug. Risk of infection is related to the virulence of the organism(s), the amount of exposure of the animal to the organism(s) and the animal's immune defence status (Brumbaugh 2009). The virulence of the organisms and the amount of exposure can be predicted on the basis of previous experience of the disease at the farm/facility, including specific diagnosis and isolation of pathogens, and estimates of morbidity and mortality when possible. The animals' defence status can be predicted by knowledge of the physiological and immunological characteristics of the animals at risk; thus, their age, the stressors to which they are exposed, their previous exposure to disease and their vaccination status should all be considered. In the trial described in this paper, which employed a metaphylactic approach, the risk of BRD was based on 5 per cent or more of the cattle within the airspace having presented with clinical signs of BRD after assembly and/or commingling at the trial site. This resulted in actual morbidities of 28 to 72 per cent among the control animals. The treatment with gamithromycin significantly reduced morbidity by 64 per cent overall (32 to 82 per cent at individual sites), confirming that the predicted consequences of not treating in terms of morbidity in untreated animals justified the use of the product by improving the welfare of the animals.
Part of the rationale for responsible use of antimicrobials is to limit the exposure of bacteria to sublethal levels of antibiotics in order to reduce the selection for antibiotic resistance. The pharmacokinetic/pharmacodynamic profile of 15-membered ring azalides such as gamithromycin is almost unique among antimicrobial agents: high tissue concentrations, rapid accumulation in tissues, retention by macrophages and circulating phagocytes, long elimination half-life and prolonged postantibiotic effect. These properties of azalides, which include gamithromycin, coupled with appropriate use, reduce the potential for development of resistance against this subclass more than for many other antibiotic classes used in veterinary medicine (Retsema 1999).
In conclusion, this European multicentre field trial has shown that gamithromycin, administered as a single treatment using a metaphylactic approach to at-risk cattle kept under a wide range of commercial conditions, significantly reduced the clinical incidence of BRD associated with M haemolytica, P multocida and/or M bovis over the 14-day trial observation period.
Acknowledgments
The authors thank the owners of the animals involved, Fabrizio Solari Basano and all personnel at Arcoblu, Milan, Italy, for coordinating the Italian studies, Mycoplasma Experience Limited for the isolation of Mycoplasma bovis from nasal swabs, and many other colleagues for their assistance with the conduct of the trial and the preparation of the manuscript, in particular A. B. Forbes, B. Somerville and R. K. Tessman. This study was funded by Merial Limited, Duluth, GA 30096, USA.
Footnotes
Provenance not commissioned; externally peer reviewed
References
- Anon (2000) International Cooperation on Harmonisation of Technical Requirements for Registration of Veterinary Medicinal Products (VICH). Guideline (GL9) Good Clinical Practice. European Medicines Agency. www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/10/WC500004343.pdf Accessed February 23, 2010 [Google Scholar]
- Anon (2008) Zactran Summary of Product Characteristics. Committee for Medicinal Products for Veterinary Use, European Medicines Agency [Google Scholar]
- Ben Ali A., Goldstein F. W., Acar J. F. (2002) In vitro activity of macrolides against traditional susceptible bacteria. In Macrolide Antibiotics. Eds Schönfeld W. Kirst H. A. Birkhäuser Verlag; pp 185–200 [Google Scholar]
- British Veterinary Association (2009) Responsible Use of Antimicrobials in Veterinary Practice. http://www.bva.co.uk/public/documents/BVA_Antimicrobials_Poster.PDF Accessed February 23, 2010
- Brumbaugh G. W. (2009) Principles of antimicrobial therapy: prophylactic or metaphylactic use of antimicrobial drugs. In Large Animal Internal Medicine. 4th edn Ed Smith B. P. Mosby Elsevier; pp 1517–1519 [Google Scholar]
- Bryskier A., Bergogne-Berezin E. (1999) Macrolides. In Antimicrobial Agents. Ed Bryskier A. ASM Press; pp 475–526 [Google Scholar]
- Bryson D. G. (2000) The calf pneumonia complex – current thoughts on aetiology. Cattle Practice 8, 103–107 [Google Scholar]
- Diarra M. S., Malouin F., Jacques M. (1999) Postantibiotic and physiological effects of tilmicosin, tylosin, and apramycin at subminimal and suprainhibitory concentrations on some swine and bovine respiratory tract pathogens. International Journal of Antimicrobial Agents 12, 229–237 [DOI] [PubMed] [Google Scholar]
- European Platform for the Responsible use of Medicines in Animals (2008) Best-Practice Framework for the Use of Antimicrobials in Food-producing Animals in the EU. www.epruma.eu/topics/antimicrobials-in-food-producing-animals.html Accessed February 23, 2010
- Giguère S., Huang R., Malinski T., Dorr P., Tessman R. K., Somerville B. (2011) Disposition of gamithromycin in plasma, pulmonary epithelial lining fluid, bronchoalveolar cells, and lung tissue in cattle. American Journal of Veterinary Research (In press) [DOI] [PubMed] [Google Scholar]
- Godinho K. S., Rae A., Windsor G. D., Tilt N., Rowan T. G., Sunderland S. J. (2005) Efficacy of tulathromycin in the treatment of bovine respiratory disease associated with induced Mycoplasma bovis infections in young dairy calves. Veterinary Therapeutics 6, 96–112 [PubMed] [Google Scholar]
- Huang R. A., Letendre L. T., Banav N., Fischer J., Somerville B. (2009) Pharmacokinetics of gamithromycin in cattle with comparison of plasma and lung tissue concentrations and plasma antibacterial activity. Journal of Veterinary Pharmacology and Therapeutics 33, 227–237 [DOI] [PubMed] [Google Scholar]
- Jain R., Danziger L. H. (2004) The macrolide antibiotics: a pharmacokinetic and pharmacodynamic overview. Current Pharmaceutical Design 10, 3045–3053 [DOI] [PubMed] [Google Scholar]
- Macartney J. E., Bateman K. G., Ribble C. S. (2003) Health performance of feeder calves sold at conventional auctions versus special auctions of vaccinated or conditioned calves in Ontario. Journal of the American Veterinary Medical Association 223, 677–683 [DOI] [PubMed] [Google Scholar]
- Mattoes H. M., Nightingale C. H. (2002) Pharmacokinetics/pharmacodynamics of macrolides. In Macrolide Antibiotics. Eds Schonfeld W. Kirst H. A. Birkhauser Verlag; pp 25–36 [Google Scholar]
- Mosier D. A. (1997) Bacterial pneumonia. Veterinary Clinics of North America: Food Animal Practice 13, 483–493 [DOI] [PubMed] [Google Scholar]
- Nightingale C. H., Mattoes H. M. (2002) Macrolide, azalide and ketolide pharmacodynamics. In Antimicrobial Pharmacodynamics in Theory and Clinical Practice. Eds Nightingale C. H. Murakawa T. Ambrose P. G. Marcel Dekker; pp 205–220 [Google Scholar]
- Quinn P. J., Markey B. K., Donnelly W. J., Leonard F. C. (2002) Pathogenic bacteria: Pasteurella species and Mannheimia haemolytica, and Haemophilus species. In Veterinary Microbiology and Microbial Disease. Blackwell Science; pp 137–151 [Google Scholar]
- Radostits O. M., Gay C. C., Hinchcliff K. W., Constable P. D. (2007) Bovine respiratory disease. In Veterinary Medicine: A Textbook of the Diseases of Cattle, Sheep, Pigs, Goats and Horses. 10th edn Saunders Elsevier; pp 923–946 [Google Scholar]
- Retsema J. A. (1999) Susceptibility and resistance emergence studies with macrolides. International Journal of Antimicrobial Agents 11 (Suppl 1), S15–21 [DOI] [PubMed] [Google Scholar]
- Retsema J. A., Girard A. E., Girard D., Milisen W. B. (1990) Relationship of high tissue concentrations of azithromycin to bactericidal activity and efficacy in vivo. Journal of Antimicrobial Chemotherapy 25 (Suppl A), 83–89 [DOI] [PubMed] [Google Scholar]
- Valarcher J. F., Hagglund S. (2006) Viral respiratory infections in cattle. Proceedings of the World Buiatrics Congress. Nice, October 15 to 19, 2006. pp 384–397 [Google Scholar]


