Abstract
Background
Yoga therapy (YT) improves cognitive function in healthy individuals, but its impact on cognitive function among persons with schizophrenia (SZ) has not been investigated.
Aims
Evaluate adjunctive YT for cognitive domains impaired in SZ.
Methods
Patients with SZ received YT or treatment as usual (TAU; n = 65, n = 23, respectively). Accuracy and speed for seven cognitive domains were assessed using a computerized neurocognitive battery (CNB), thus minimizing observer bias. Separately, YT was evaluated among patients with Bipolar I disorder (n = 40), Major Depressive Disorder (n = 37), and cardiology outpatients (n = 68). All patients also received routine pharmacotherapy. Patients were not randomized to YT or TAU.
Results
Compared with the SZ/TAU group, the SZ/YT group showed significantly greater improvement with regard to measures of attention following corrections for multiple comparisons; the changes were more prominent among the men. In the other diagnostic groups, differing patterns of improvements were noted with small to medium effect sizes.
Conclusions
Our initial analyses suggest nominally significant improvement in cognitive function in schizophrenia with adjunctive therapies such as YT. The magnitude of the change varies by cognitive domain and may also vary by diagnostic group.
Keywords: schizophrenia, cognition, yoga
Introduction
Cognitive impairment represents a prominent feature of several psychiatric illnesses, including schizophrenia (SZ), major depressive disorder and bipolar disorder (1, 2) (3). Deficits in long-term memory, working verbal memory, executive functioning, and vigilance have been consistently associated with poor functional outcome in persons with SZ (4) (5) (6) (7) (8). As pharmacological treatment is not routinely efficacious (9), there is ongoing interest in adjunctive non-pharmacological interventions for ameliorating cognitive deficits (10) (11) (12).
Compared with conventional therapies, yoga represents a different approach. It is a set of mental and physical practices that have been evolving in India for several millennia. Yoga is viewed by many practitioners as a systematic process designed to purify the body and the mind from toxins accumulated due to improper lifestyle choices and negative thinking patterns. Yoga includes components centered on meditation, breathing, and activity or postures designed to balance the body's ‘energy centers’ (13). Intensive yoga exercises may improve cognitive function among psychiatrically ill and healthy adults (14, 15) (16) (17) (18) (19) (20). There are several mechanisms by which the practice of yoga may improve cognitive function. Yoga emphasizes body awareness and involves focusing one's attention on breathing or specific muscles or parts of body, so yoga may improve more general as well as focused attention. Yoga practice also influences perception by increasing perceptual sensitivity, by selectively ‘shutting out’ undesirable stimuli, and by changing distorted perception. Practicing yoga improved auditory and visual perception, by increasing sensitivity to various characteristics of the stimuli (e.g., intensity, frequency) (21). A recent study (20) observed that memory functions of male volunteers improved after yoga. In an open trial of yoga (n = 21) versus physical therapy (n = 20) among patients with SZ in India, greater improvement in psychopathology was reported with YT compared with physical therapy. Improvement in clinical severity was noted following three weeks of YT, but cognitive function was not evaluated (22). In another study (23), yoga was found to improve facial emotion recognition deficits. The precise physiological basis for the beneficial effects of yoga is unknown and continues to be investigated. Selvamurthy et al. have found that yoga helps to achieve a stable autonomic balance (24). Others have reported that the practice of yoga reduces autonomic arousal (25) (26). Since increased physical activity reduces autonomic reactivity to mental stressors (27), it is possible that some of the beneficial effects of yoga are related to stabilization / normalization of autonomic function.
The studies reviewed above were conducted by highly trained therapists or clinicians in structured academic centers. Their utility in routine clinical practice is uncertain. Moreover, YT has typically not been used as a cognitive remediation strategy for individuals with impaired cognition. In the present pilot study, we evaluated the impact of YT among individuals with severe psychiatric illnesses. Cognitive domains known to be impaired in these disorders were assessed.
Methods
Design
We conducted an open, non-randomized pilot study of adjunctive YT in comparison with treatment as usual (TAU) among patients with SZ. Cognitive function was evaluated using an automated computerized battery that evaluates cognitive variables known to be impaired in SZ. Group-wise comparisons were conducted between the YT and the TAU SZ groups using non-parametric tests. YT was also administered to individuals with other disorders, in order to evaluate whether the changes among SZ patients were also observed in non-SZ groups. A pair-wise design was also used to evaluate temporal changes in each participant. As we are not aware of publications regarding YT and diverse neuro-cognitive functions in SZ patients, the potential effect size and hence the required sample size could not be estimated. We therefore based our target sample size on the prior Yoga study of SZ in India that reported improvement in facial emotional recognition deficits (23).
Eligibility criteria
The participants were outpatients at Dr Ram Manohar Lohia Hospital (RMLH), Delhi, a publicly funded general hospital. All participants were over 18 years of age and resided in Delhi. Persons dependent on alcohol / illicit substances or individuals with neurological disorders that interfered with diagnosis or cognitive evaluations were excluded. At the psychiatric outpatient clinics of RMLH, all patients clinically diagnosed with psychoses who fulfilled these criteria were invited to participate in the study over a period of three years, during which treatment was provided (February 2006 to August 2009). Consenting individuals who were willing and able to come to RMLH to participate in the structured YT program were included in the YT groups. Individuals with SZ who could not participate in YT for logistical reasons but consented to the research project participated as the TAU group. Patients in the other diagnostic categories were included if they fulfilled diagnostic criteria and could participate in YT. There were several reasons for non-participation, including cumbersome commutes, difficulty in traveling alone / lack of companion for travel, inability to get time off from work and availability of preferred neighborhood yoga centers.
Ethical approval for the study was obtained from Institutional Ethics Committee (IEC) at Dr. Ram Manohar Lohia Hospital (Delhi), India and the Institutional Review Board, University of Pittsburgh, Pittsburgh, USA.
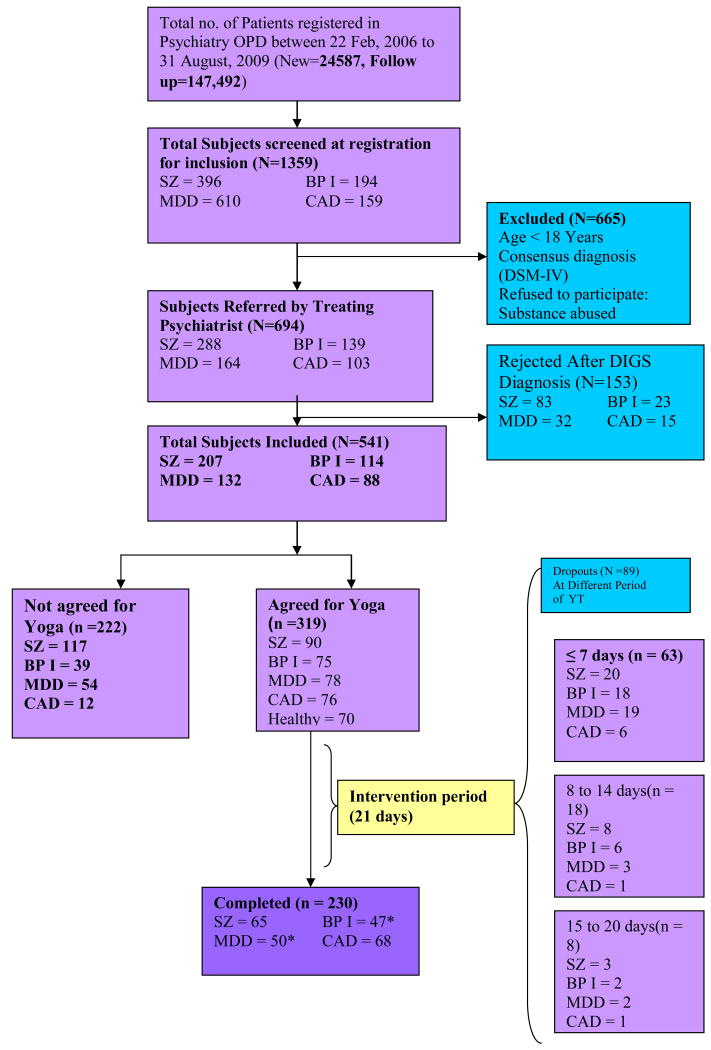
Flow of potential participants in the study
The detailed recruitment is illustrated in the flow chart (Figure 1). Briefly, a total of 24587 new and 147,492 repeat outpatients visited the RML outpatient clinics during the recruitment period. Of these, 1359 subjects had suitable clinical diagnoses assigned by their physicians on the basis of unstructured interviews. Following structured diagnostic interviews, a total of 541 participants were recruited to the study. Of these, 319 individuals agreed to participate in YT, of whom 230 completed the entire regimen (SZ=65; BP1=47; MDD=50; CAD=68). There were no significant differences with regard to age, sex, marital status and occupation between SZ patients who participated in yoga (YYT) and those who refused yoga (NYT), but the former had significantly longer periods of education (Table 1). The YYT/SZ group did not differ with regard to age at onset, duration of illness, or scores on the Modified Mini Mental State Examination, but had significantly poorer GAF scores at the worst point during a recent episode (t=3.264, p 0.001, Table 1). The distribution of patients in the other diagnostic groups who consented to YT or declined were not significantly different; there were also no significant differences between the patients who consented to YT or declined YT with regard to diagnostic or available key clinical variables in these groups (data not shown).
Figure 1. Sample Recruitment Flow Chart.
*We have pre-post CNB data for SZ=65, BP1=40 and MDD=37
Table 1. Demographic and clinical characteristics of patients who consented or did not consent to Yoga therapy.
| Variable | Consented to Yoga (YYT*) (n=90) | Not consented to Yoga (NYT*) (n=117) | Statistical significance (p= 0.05) | |
|---|---|---|---|---|
| t/ χ² Values | p - Values | |||
| Age in Years (Mean ±SD) | 33.27±9.815 | 32.75(±12.065) | 0.121 | 0.729 |
| Education in years (Mean ±SD) | 10.24±4.557 | 8.79(±5.150) | 4.852 | 0.029 |
| Number of Children (Mean ±SD) | 1.95±1.64 | 2.56(±1.996) | 3.337 | 0.070 |
| Sex (Male/Female) | 60(66.7%)/30(33.3%) | 71(62.3%)/43(37.7%) | 0.465 | 0.575 |
| Marital Status (Ever Married/Never Married) | 47(51.8%)/43(48.2%) | 63(55.3%)/51(44.7%) | 0.260 | 0.687 |
|
Occupation [Employed/ (Unemployed or Retired)/ Housewife/Student] |
18/53/14/5 (20%/59%/15%/6%) | 28/63/15/7 (25%/56%/13%/6%) | 0.666 | 0.896 |
| Age at onset in Years (Mean ±SD) | 25.1±8.0 | 25.1±9.3 | -0.001 | 0.990 |
| Current GAF* (Mean ±SD) | 23.41±7.9 | 22.72±6.4 | 0.713 | 0.476 |
| Most recent episode GAF* (Mean ±SD) | 32.10±13.6 | 26.94±9.4* | 3.264 | 0.001 |
| GAF* at worst point of illness (Mean ±SD) | 23.45±6.0 | 22.34±5.3 | 1.301 | 0.195 |
| Duration of Illness (Mean ±SD) | 384.54±324.5 | 318.97±314.8 | 1.478 | 0.141 |
| MMMSE*(Mean ±SD) | 26.01±6.1 | 26.40±6.51 | -0.42 | 0.675 |
YYT: agreed to Yoga; NYT: declined Yoga; GAF: Global Assessment of Functioning; MMMSE: Modified Mini Mental State Examination;
Lower GAF scores reflected more severe illness.
Participants evaluated for the study
A total of 65 outpatients with SZ completed YT. There were 117 patients who were assessed at baseline but did not participate in yoga. Of these, a sub-group were re-evaluated after two months (TAU group, N = 23). The demographic and cognitive variables of this sub-group were compared with individuals who were not re-evaluated after 2 months; there was no significant difference between these groups on age, gender, education and cognitive variable (data not shown).
Patients with bipolar I disorder (BP1, n = 40) and major depressive disorder (MDD, n = 37) also participated in the study and received YT. A group of outpatients at the RMLH cardiology clinic were also recruited to receive adjunctive YT (n = 68). All participants provided written, informed consent.
Diagnostic evaluations
Participants were evaluated using the Hindi version of the Diagnostic Interview for Genetic Studies (DIGS) (28) (29). The DIGS is a comprehensive interview schedule, which acquires extensive clinical as well as demographic information. Information from the DIGS was integrated with available information from medical records and family interviews conducted using the Family Interview for Genetic Studies (FIGS) (30). This information was discussed with board certified psychiatrists and psychologists who established consensus diagnoses.
Adjunctive Treatment
Yoga
Participants completed a prescribed YT protocol daily for approximately one hour on twenty-one consecutive days, excluding Sundays. The YT protocol was designed for the study in consultation with the Central Council of Research and Naturopathy (AYUSH), Ministry of Health and Family Welfare, Government of India. YT protocol was uniform for all participants and is uploaded on website http://www.indouspgp.info/publications/400. YT was conducted by a qualified yoga instructor who was trained to provide the customized YT, under the supervision of an accredited physician. A Professor of Yogic Studies affiliated with AYUSH also supervised the yoga instructor and observed the YT sessions periodically. The YT comprised combinations of ‘Asanas’ (postures or exercises) and ‘Pranayam’ (Breathing protocols). Each session commenced with ‘Om’ chanting (Deep breathing with prayer), followed by warm up exercises and breathing exercises. The Pranayama was designed to correct movements and synchronize movement with breathing. The Asanas comprised different postures, including standing (Kati chakrasan, Tadasan, Trikonasan); supine lying postures (Savasana, Uttanpadasan, Naukasan, Pawanmuktasan- Ardha and poorna); prone position postures (Makarasan, Bhujangasan, Shalabhasan, Dhanurasan); sitting postures (Pashimottanasan, Ushtrasan, Gomukhasan, Ardha Matsyendrasan, Vajrasana). On Saturdays, patients exercised a simple practice known as Kriya or Jalneti (a cleansing practice of the sinus passages with warm saline water, thought to provide physical and psychological benefits).
Medication management
All participants received conventional pharmacological and non-pharmacological treatment from their psychiatrists and therapists throughout the study. No changes in medications were required as part of YT. The therapists were not told whether patients were in the YT or TAU groups.
Neurocognitive Assessment
Cognitive functions were assessed with a Hindi version of the Penn Computerized Neuropsychological Battery (CNB) (31). The CNB includes neurocognitive domains known to be impaired among individuals with SZ (32). Data are acquired in an automated fashion, reducing observer bias. It is also possible to measure both accuracy and response times. The construct validity of the Penn CNB has been established and it has been used extensively (33) (31). The battery assesses the following neurocognitive domains: Abstraction and mental flexibility (ABF), Attention (ATT), Working Memory (WM), Verbal Memory (VMEM), Face memory (FMEM), Spatial memory (SMEM), Spatial processing (SPA), Language (LAN), Sensorimotor dexterity (SM), Emotion processing (EMO). The verbal domains are available only in English. As many Indian participants did not speak English, the verbal domains were excluded. For each domain, three summary functions are calculated: (1) accuracy, which reflects the number of correct responses; (2) speed, which reflects the median reaction time for correct responses; and (3) efficiency, which reflects both accuracy and speed (accuracy / log of speed). Participants can be differentially sensitive to these indices. The battery was administered in a fixed order using a web browser interface. The CNB was administered twice to all participants (before and after completion of YT). Accuracy estimates for sensorimotor accuracy were not analyzed in this sample, as the majority of patients obtained perfect scores at baseline. Participants need not be computer literate in order to complete the Penn CNB, as the evaluations are straight forward. In addition, each participant is required to complete a practice session designed for familiarization with the computer mouse and the video monitor. All CNBs were administered under the supervision of research staff.
Timeline for cognitive assessments
The YT group was assessed at baseline, 21 days after yoga therapy, and two months following completion of YT. The TAU Group was assessed at baseline and after two months.
Statistical Analysis
The demographic, clinical and cognitive variables of the Yoga and TAU groups were compared at baseline using Mann Whitney U-test. CNB scores were normalized using data obtained from Indian control individuals (33). The Kruskal Wallis test was used to evaluate the difference between SZ/YT and SZ/TAU groups with regard to changes in the cognitive domains. Separately, pair-wise comparisons between baseline and post-treatment values for CNB domains were compared in each diagnostic group, using the Wilcoxon's signed rank test (two-tailed). Effect sizes were calculated by dividing the differences between baseline and post assessment means with the standard deviation of baseline separately for each index of all domains (Cohen's d) (34) (35). Corrections for multiple comparisons were applied as recommended by Hochberg (36).
Results
Comparisons at baseline
The demographic and clinical details of the SZ/YT and SZ/TAU groups are presented in Table 2. The SZ/YT group included individuals who were evaluated on completion of YT (3 weeks post baseline) and those who were also evaluated 2 months post-treatment. There were no significant differences between SZ/YT (either group) versus the SZ/TAU group with regard to age, education or duration of illness. There were proportionately more men in the SZ/YT groups compared with the SZ/TAU. Though the age at onset of illness (a proxy for illness severity) was similar in the entire SZ/YT group compared with the TAU group, the GAF scores during the past month were significantly higher in the TAU group, suggesting more severe impairment in the TAU participants at baseline. The smaller SZ/YT group (2 month evaluation post-baseline) had mean GAF scores similar to the TAU group, though the former had later mean ages at onset. Using the Mann Whitney U-test, there were no significant differences with regard to cognitive domains between the SZ/YT and the SZ/TAU groups, apart from working memory (speed) domain, which was significantly better in the YT group (p = 0.033, uncorrected).
Table 2. Demographic and clinical characteristics of the schizophrenia YT and TAU samples.
| Diagnosis and Treatment | SZ/YT# N=65 |
SZ/YT## N=30 |
SZ/TAU N=23 |
SZ/YT# vs. TAU | SZ/YT## vs. TAU | ||
|---|---|---|---|---|---|---|---|
| p value | p value | ||||||
| Gender (M/F) | 43/22* | 21/9 | 11 / 12 | Chi=3.00 | 0.222 | 2.676 | 0.102 |
| Age (years) | 31.50±9.82 | 33.2±10.36 | 31.38±11.14 | -0.5 | 0.617 | -1.024 | 0.306 |
| Education (School years) | 10.78±3.91 | 9.83±4.11 | 11.26±3.16 | -0.385 | 0.7 | -1.482 | 0.138 |
| Age at onset | 24.37±7.95 | 26.04±8.44 | 21.23±6.458 | -1.675 | 0.094 | -2.518 | 0.012 |
| GAF during past month | 34.33±12.78 | 26.76±8.16 | 27.22±6.266 | -0.283 | 0.037 | -1.782 | 0.075 |
| Duration of illness (weeks) | 291.43±275.21 | 305.22±309.59 | 360.38±325.04 | -0.702 | 0.482 | -0.398 | 0.69 |
Variables are listed as mean ± standard deviation. All p values are uncorrected for multiple comparisons. M: male, F: female, YT: Yoga Therapy as an adjunct to pharmacotherapy, TAU: treatment as usual, including routine pharmacotherapy, GAF: Global Assessment of Functioning.
Individuals who were evaluated on completion of YT (3 weeks post baseline).
Individuals who were evaluated 2 months post-treatment.
The demographic features of the other diagnostic groups are as follows: BP1 (mean age 36.43±15.34 years, mean education 10.77±3.39 years, 27 men); MDD (mean age 41.05±10.68 years, mean education 10.77±4.60 years, 19 men); cardiac outpatients (mean age 66±9.84 years, mean education 13.00±3.63 years, 54 men). There was a relative excess of men in these diagnostic groups. The cardiology outpatient group was significantly older (cardiac vs. SZ: Z = 8.85, p < 0.001; cardiac vs. BP1: Z = 6.23, p < 0.001; cardiac vs. MDD: Z = 5.42, p < 0.001) and more educated than the other diagnostic groups (cardiac vs. SZ: Z = 3.03, p = 0.002; cardiac vs. BP1: Z = 6.23, p = 0.004; cardiac vs. MDD: Z = 2.21, p = 0.027).
Changes in cognitive domains following treatment in the SZ/YT group compared with the SZ/TAU groups
The Kruskal Wallis test was used. Since efficiency is derived from the accuracy and speed estimates, the efficiency estimates were not compared in order to limit the number of comparisons. At the three week assessment point, greater improvement was present in the SZ/YT group on speed indices for abstraction (χ2 = 4.228, p = 0.040) and attention (χ2 = 4.913, p = 0.027). After Hochberg correction, attention (speed) remained significant (p = 0.025). As significantly more men were present in the SZ/YT group, differences in cognitive changes were also analyzed separately by gender. Among men, accuracy for emotional processing (χ2=5.076, p=0.024) and speed for attention (χ2=4.269, p=0.039) and sensorimotor (χ2=3.903, p=0.048) improved to a greater extent in the SZ/YT group compared with the SZ/AU group. Following Hochberg correction, only the emotion variable remained significant (p = 0.05). Among the women, only sensorimotor (speed measure) was nominally better in the SZ/YT group (χ2=3.84, p=0.05); it remained same following Hochberg correction.
The preceding analyses compared the SZ/YT group at 3 weeks post-treatment with the TAU group, which was assessed two months after the baseline assessment. Assessments at 2 month post-treatment in the SZ/YT group (n = 30) were also compared with the SZ/TAU group (n = 23). There was significantly greater improvement in the SZ/YT sample compared with the SZ/TAU group with regard to attention (accuracy) (χ2 = 4.603, p = 0.032); abstraction (speed) (χ2 = 4.971, p = 0.026) and attention (speed) (χ2 = 6.001, p = 0.014). After Hochberg correction, attention (speed, p=0.025) remained significant. Separate comparisons between men and women were also conducted. Among the men, there was significant improvement in attention accuracy (χ2=4.63, p=0.031); face memory accuracy (χ2=6.14, p=0.013); emotion accuracy (χ2=4.885, p=0.027); attention speed (χ2=4.594, 0.032) and sensorimotor speed (χ2=6.216, p=0.013). After Hochberg correction, face memory accuracy (p=0.025) and sensorimotor speed (p=0.05) were significant. There was no significant difference between the female SZ/YT and SZ/TAU groups.
We also estimated effect sizes (Cohen's d) in the YT/SZ and TAU/SZ groups using pair-wise pre- and post-treatment comparisons (Table 3 and Supplementary Tables). Comparisons of pre- and post-treatment values for cognitive domains by diagnostic group are illustrated in Figure 2. Pre and post-treatment means, standard deviations, Cohen's d and Wilcoxon Z with p values for all cognitive domains of all groups (YT/SZ, BP 1, MDD, Cardiac controls, TAU/SZ) are enumerated in Supplementary Table 1. The YT/SZ values for pre- and post-21 days yoga and also after two months follow up are also included in this table.
Table 3. Comparison of CNB domain effect sizes and Wilcoxon Z scores among persons with schizophrenia following Yoga Therapy or Treatment as usual.
| Yoga Therapy (YT) | Treatment as usual (TAU) | |||||
|---|---|---|---|---|---|---|
| ES, 21 days post YT | Wilcoxon p value | ES, 60 days post YT | Wilcoxon p value | ES, 60 days post-TAU | Wilcoxon p value | |
| Domains | (N=65) | (N=30) | (N=23) | |||
| Accuracy | ||||||
| Abstraction and mental flexibility | 0.3335 | 0.0090 | 0.4155 | 0.0839 | 0.0841 | 1.0000 |
| Attention | 0.0892 | 0.0201 | 0.6190 | 0.0116 | -0.2399 | 0.8900 |
| Face memory | 0.0897 | 0.2048 | 0.5790 | 0.0143 | 0.0376 | 0.7211 |
| Spatial memory | -0.0401 | 0.3563 | -0.0072 | 0.2009 | 0.3177 | 0.4236 |
| Working memory | -0.0728 | 0.7281 | -0.2314 | 0.8628 | 0.1662 | 0.3113 |
| Spatial ability | -0.1932 | 0.4408 | -0.1165 | 0.8111 | -0.4599 | 0.1270 |
| Sensorimotor | 0.2390 | 0.0812 | 0.2627 | 0.2365 | 0.0719 | 0.4844 |
| Emotion | -0.0096 | 0.8727 | 0.1288 | 0.3447 | -0.2524 | 0.0696 |
| Speed | ||||||
| Abstraction and mental flexibility | 0.5530 | 0.0001 | 0.8471 | 0.0016 | -0.1698 | 0.8382 |
| Attention | 0.1731 | 0.1439 | 0.3434 | 0.0665 | -0.3344 | 0.1439 |
| Face memory | 0.4584 | 0.0001 | 0.5692 | 0.0014 | -0.1625 | 0.1982 |
| Spatial memory | 0.4075 | 0.0006 | 0.4347 | 0.0046 | 0.4991 | 0.0071 |
| Working memory | 0.4194 | 0.0149 | 0.3823 | 0.1594 | -0.0666 | 0.6705 |
| Spatial ability | 0.4265 | 0.0595 | 0.8091 | 0.2402 | -0.0177 | 1.0000 |
| Sensorimotor | 0.2645 | 0.0069 | 0.5634 | 0.0080 | -0.0050 | 0.6095 |
| Emotion | 0.4180 | 0.0001 | 0.5429 | 0.2002 | 0.1681 | 0.1231 |
| Efficiency | ||||||
| Abstraction and mental flexibility | 0.3832 | 0.0022 | 0.5895 | 0.0233 | 0.0948 | 0.8382 |
| Attention | 0.1055 | 0.0176 | 0.6523 | 0.0047 | -0.0919 | 0.9799 |
| Face memory | 0.2370 | 0.0064 | 0.7180 | 0.0017 | 0.0331 | 1.0000 |
| Spatial memory | 0.0553 | 0.0965 | 0.2792 | 0.0296 | 0.4300 | 0.1134 |
| Working memory | 0.0723 | 0.4680 | 0.1031 | 0.4954 | 0.1700 | 0.2288 |
| Spatial ability | -0.0663 | 0.8480 | 0.5577 | 0.1230 | -0.4759 | 0.1309 |
| Sensorimotor | 0.2028 | 0.1784 | 0.3631 | 0.0822 | 0.0497 | 0.3692 |
| Emotion | 0.0777 | 0.6097 | 0.3697 | 0.0738 | -0.2850 | 0.0362 |
ES: Effect size (Cohen's d). p values computed with the Wilcoxon's sum of ranks test.
Figure 2. Cognitive evaluations.
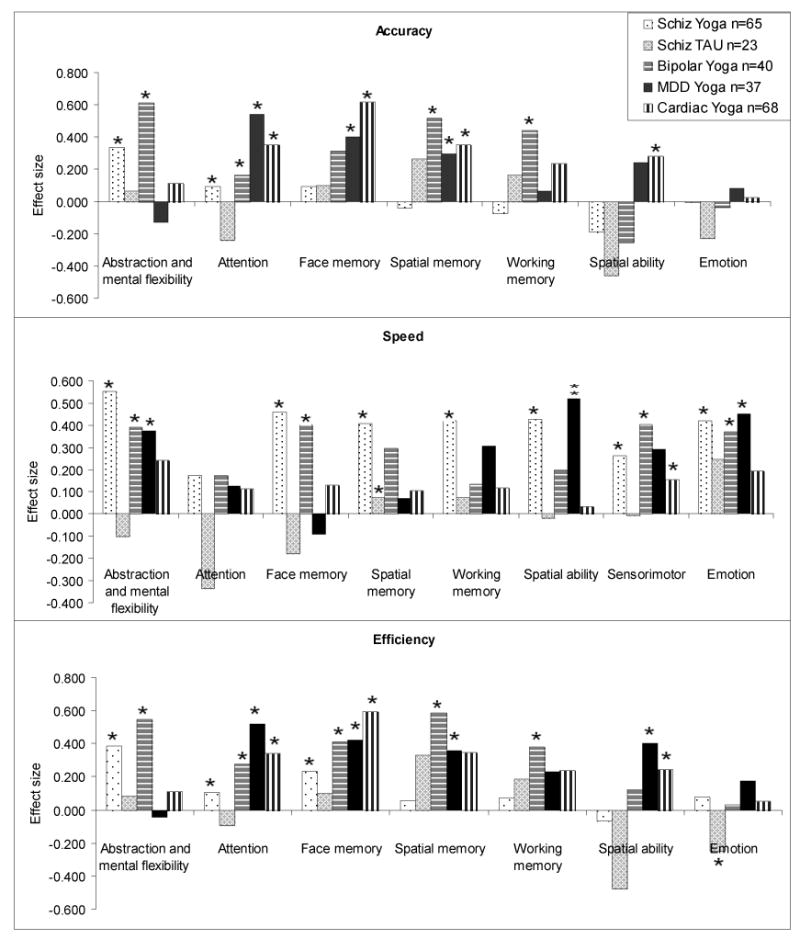
In the SZ/YT group, there was significant improvement on speed indices for all the domains, except attention and spatial ability. The speed effect sizes (ES) ranged from 0.26 (sensorimotor) to 0.55 (Abstraction and mental flexibility). Two domains also showed improvement in accuracy (Abstraction and mental flexibility) and attention. Significant beneficial effects in the efficiency scores were noted for abstraction and mental flexibility as well as face memory (Cohen's d=0.24). In the SZ/ TAU group, there was significant decline in emotion identification (efficiency). On the other hand, there was significant improvement in spatial memory (speed). Other domains did not show statistically significant changes in the SZ/YT or the TAU groups.
YT in other diagnostic groups
The effect sizes for the changes in CNB scores among the other diagnostic groups are shown Figure 2 and in the Supplementary Table 1 (p values uncorrected for multiple comparisons). In the BP1 group, speed, accuracy and efficiency improved for abstraction and mental flexibility, and face memory. Accuracy and efficiency improved in the attention, working memory, and spatial memory domains. Speed, but not accuracy or efficiency improved significantly in the emotion identification test. There were significant improvements in the MDD group with regard to accuracy indices for attention, face memory and spatial memory. There was also significant improvement in speed indices for the abstraction and mental flexibility, spatial ability and emotion domains. Unlike the SZ group, where the improvements were most marked with regard to speed, the cardiac outpatient group showed improvement in accuracy for the following domains: attention (ES = 0.35), face memory (0.615), spatial memory (0.35) and spatial ability (0.28). There was no significant change with regard to abstraction and mental flexibility and emotion domains. Efficiency also improved in the attention (0.34) and face memory (0.595) domains.
Discussion
Improvement occurred in certain cognitive domains following relatively brief YT. Significant improvement was noted in indices of speed as well as accuracy for these domains, with attendant improvement in efficiency. The changes varied across diagnostic groups and provide grounds for therapeutic optimism. The magnitude of the changes also varied across domains, suggesting some specificity for the adjunctive treatment. For example, indices of speed were more likely to improve than accuracy with YT in the SZ group. In the YT groups, significant differences were observed in relation to attention immediately after completion of the yoga regimen as well as at the two month point. The improvement was more prominent among the men than the women. There was also variation in the degree of improvement across diagnostic groups. The BP1, MDD and cardiac groups improved predominantly with regard to accuracy following YT, though improvements in speed were also noted for some indices. Overall, the number of domains that improved significantly with YT is higher than would be expected by chance alone. In contrast, only three variables improved in the SZ TAU group, with significant deterioration in another variable. The cognitive domains that were evaluated are rooted in complex neural pathways and are correlated. YT also includes several components and is inherently difficult to evaluate through therapeutic trials. Additionally, the relatively small sample and the non-randomized design make it premature to speculate on the primary effects of YT. For the same reasons, it is not possible to identify the specific components of the adjunctive treatment that were beneficial. For example, the benefit may have accrued from a placebo effect, due to physical exercise or through interactions with meditations.
Yoga includes a set of spiritual and physical practices that have been evolving over several millennia. It may be viewed as a mind-body approach that has components centering on meditation, breathing, and activity or postures. While the precise components of YT that contribute to cognitive improvement cannot be identified at present, repeated contact with empathic therapists over a three week period must be considered as a contributory factor. Further research is required to clarify whether the temporal changes can be attributed to YT acting in isolation or in conjunction with medications. Practice effects may also have played a role, as some beneficial effects were observed even in the TAU groups. However, significant improvement was more often observed in the YT groups than in the TAU groups.
The sample comprised outpatients at a publicly funded facility. A wide spectrum of individuals was thus represented. Our YT participants comprised cooperative urban dwellers who were likely more educated than individuals who reside in rural regions of India. Therefore, our results may not be generalizable to Indian persons who live in rural areas or less educated individuals. We have also highlighted clinical differences between the SX/YT and the SZ/TAU groups that may impact the different patterns of improvement noted in these groups (Table 2). Due to the non-randomized design, there may be other unidentified confounding variables that may also explain these patterns. The results may also not be generalizable at present, because the YT protocol required adherence to a strict attendance routine that necessarily led to ascertainment bias for the YT group. We made within group (over time) comparisons for each participant, as well as between group (SZ/YT vs. TAU) comparisons for the YT and TAU SZ groups. Both sets of comparisons show significant improvement in the YT group for specific cognitive domains. While care was taken to ensure that YT was provided in a uniform manner, it was adjunctive in nature. Pharmacotherapy or other forms of therapy administered concurrently to the patients were not regulated; neither did the treating clinicians specifically inquire about yoga participation. In addition, we did not assess changes in clinical status, such as symptom scores. Therefore, it is uncertain whether the cognitive variables improved in tandem with symptom scores or were independent. The study design did not include placebo groups. Indeed, it would be difficult to design suitable comparable ‘placebo’ groups for YT. Though double blind evaluations would be difficult for studies of YT, the automated nature of the CNB itself reduces observer bias. The duration between the initial and the follow up cognitive assessments differed in the YT/SZ and the TAU/SZ groups. However, comparison of these groups at identical time points continued to indicate significantly greater improvement in the YT group. Finally, the non-random assignation of YT in the SZ group introduces bias that may influence the results. Additional, randomized studies are needed.
In conclusion, our pilot study suggests that cognitive impairment in psychotic disorders may improve with adjunctive treatment. Adjunctive YT improves performance in different domains of cognitive function across psychiatric disorders. The physiological basis for the observed changes is unknown. It may be related to correction of autonomic dysfunction reported among patients with schizophrenia (37). Mentally ill persons could benefit from simple economical yoga exercises if these are incorporated in their treatment regimens. This cognitive improvement may help them in their rehabilitation and adjustment in society.
Supplementary Material
Acknowledgments
We thank our study participants, clinical recruiters and data specialists of our research groups. Constructive comments from two peer reviewers are acknowledged with gratitude. We thank Ms Sue Clifton for editorial advice and Mr. Pramod Thomas for statistical inputs. This work was supported in part by grants from the Central Council for Research in Yoga and Naturopathy, AYUSH, MoHFW, India (12-1/CCRYN/2005-2006/Res.P-III), and NIH (MH56242, MH66263, MH 63480, and Indo-US Project Agreement # N-443-645).
Footnotes
Conflicts of interest: None.
References
- 1.Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology. 1998;12:426–45. doi: 10.1037//0894-4105.12.3.426. [DOI] [PubMed] [Google Scholar]
- 2.Marazziti D, Consoli G, Picchetti M, Carlini M, Faravelli L. Cognitive impairment in major depression. Eur J Pharmacol. 626:83–6. doi: 10.1016/j.ejphar.2009.08.046. [DOI] [PubMed] [Google Scholar]
- 3.Goldberg JF, Chengappa KN. Identifying and treating cognitive impairment in bipolar disorder. Bipolar Disord. 2009;11(2):123–37. doi: 10.1111/j.1399-5618.2009.00716.x. [DOI] [PubMed] [Google Scholar]
- 4.Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–30. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- 5.Penn DL, Spaulding W, Reed D, Sullivan M, Mueser KT, Hope DA. Cognition and social functioning in schizophrenia. Psychiatry. 1997;60:281–91. doi: 10.1080/00332747.1997.11024806. [DOI] [PubMed] [Google Scholar]
- 6.Green MF. Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J Clin Psychiatry. 2006;67:e12. [PubMed] [Google Scholar]
- 7.McGurk SR, Mueser KT. Cognitive functioning and employment in severe mental illness. J Nerv Ment Dis. 2003;191:789–98. doi: 10.1097/01.nmd.0000100921.31489.5a. [DOI] [PubMed] [Google Scholar]
- 8.Bourgeois M, Swendsen J, Young F, Amador X, Pini S, Cassano GB, Lindenmayer JP, Hsu C, Alphs L, Meltzer HY. Awareness of disorder and suicide risk in the treatment of schizophrenia: results of the international suicide prevention trial. Am J Psychiatry. 2004;161:1494–6. doi: 10.1176/appi.ajp.161.8.1494. [DOI] [PubMed] [Google Scholar]
- 9.Rund BR, Borg NE. Cognitive deficits and cognitive training in schizophrenic patients: a review. Acta Psychiatr Scand. 1999;100:85–95. doi: 10.1111/j.1600-0447.1999.tb10829.x. [DOI] [PubMed] [Google Scholar]
- 10.Wykes T, Reeder C, Landau S, Everitt B, Knapp M, Patel A, Romeo R. Cognitive remediation therapy in schizophrenia: randomised controlled trial. Br J Psychiatry. 2007;190:421–7. doi: 10.1192/bjp.bp.106.026575. [DOI] [PubMed] [Google Scholar]
- 11.Hodge MA, Siciliano D, Withey P, Moss B, Moore G, Judd G, Shores EA, Harris A. A Randomized Controlled Trial of Cognitive Remediation in Schizophrenia. Schizophr Bull. 2008;36:419–27. doi: 10.1093/schbul/sbn102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McGurk SR, Twamley EW, Sitzer DI, McHugo GJ, Mueser KT. A meta-analysis of cognitive remediation in schizophrenia. Am J Psychiatry. 2007;164:1791–802. doi: 10.1176/appi.ajp.2007.07060906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.SAMHSA. Results from the 2006 National Survey on Drug Use and Health:National Findings. Substance Abuse and Mental Health Services Administration; 2006. [Google Scholar]
- 14.Raju PS, Prasad KV, Venkata RY, Murthy KJ, Reddy MV. Influence of intensive yoga training on physiological changes in 6 adult women: a case report. J Altern Complement Med. 1997;3:291–5. doi: 10.1089/acm.1997.3.291. [DOI] [PubMed] [Google Scholar]
- 15.Sageman S. Breaking through the despair: spiritually oriented group therapy as a means of healing women with severe mental illness. J Am Acad Psychoanal Dyn Psychiatry. 2004;32:125–41. doi: 10.1521/jaap.32.1.125.28329. [DOI] [PubMed] [Google Scholar]
- 16.Chattha R, Nagarathna R, Padmalatha V, Nagendra HR. Effect of yoga on cognitive functions in climacteric syndrome: a randomised control study. Bjog. 2008;115:991–1000. doi: 10.1111/j.1471-0528.2008.01749.x. [DOI] [PubMed] [Google Scholar]
- 17.Uma K, Nagendra HR, Nagarathna R, Vaidehi S, Seethalakshmi R. The integrated approach of yoga: a therapeutic tool for mentally retarded children: a one-year controlled study. J Ment Defic Res. 1989;33(Pt 5):415–21. doi: 10.1111/j.1365-2788.1989.tb01496.x. [DOI] [PubMed] [Google Scholar]
- 18.Vani PR, Nagarathna R, Nagendra HR, Telles S. Progressive increase in critical flicker fusion frequency following yoga training. Indian J Physiol Pharmacol. 1997;41:71–4. [PubMed] [Google Scholar]
- 19.Manjunath NK, Telles S. Improved performance in the Tower of London test following yoga. Indian J Physiol Pharmacol. 2001;45:351–4. [PubMed] [Google Scholar]
- 20.Subramanya P, Telles S. Effect of two yoga-based relaxation techniques on memory scores and state anxiety. BioPsychoSocial Medicine. 2009;3(8) doi: 10.1186/1751-0759-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown DP, Forte M, Dysart M. Visual sensitivity and mindfulness meditation. Perceptual Motor Skills. 1984;58:775–777. doi: 10.2466/pms.1984.58.3.775. [DOI] [PubMed] [Google Scholar]
- 22.Duraiswamy G, Thirthalli J, Nagendra HR, Gangadhar BN. Yoga therapy as an add-on treatment in the management of patients with schizophrenia--a randomized controlled trial. Acta Psychiatr Scand. 2007;116:226–32. doi: 10.1111/j.1600-0447.2007.01032.x. [DOI] [PubMed] [Google Scholar]
- 23.Behere RV, Arasappa R, Jagannathan A, et al. Effect of yoga therapy on facial emotion recognition deficits, symptoms and functioning in patients with schizophrenia. Acta Psychiatr Scand. 2011;123:147–53. doi: 10.1111/j.1600-0447.2010.01605.x. [DOI] [PubMed] [Google Scholar]
- 24.Selvamurthy W, Nayar H, Joseph S. Physiological effects of yogic practice. NIMHANS Journal. 1983;1:71–80. [Google Scholar]
- 25.Wallace RK, Benson H, Wilson AF. A wakeful hypometabolic physiologic state. Am J Physiol. 1971;221:795–9. doi: 10.1152/ajplegacy.1971.221.3.795. [DOI] [PubMed] [Google Scholar]
- 26.Joseph S, Sridharan K, Patil SK, et al. Study of some physiological and biochemical parameters in subjects undergoing yogic training. Indian J Med Res. 1981;74:120–4. [PubMed] [Google Scholar]
- 27.Steptoe A, Kearsley N, Walters N. Cardiovascular activity during mental stress following vigorous exercise in sportsmen and inactive men. Psychophysiology. 1993;30:245–52. doi: 10.1111/j.1469-8986.1993.tb03350.x. [DOI] [PubMed] [Google Scholar]
- 28.Nurnberger JI, Jr, Blehar MC, Kaufmann CA, et al. Diagnostic interview for genetic studies. Rationale, unique features, and training. NIMH Genetics Initiative. Arch Gen Psychiatry. 1994;51:849–59. doi: 10.1001/archpsyc.1994.03950110009002. discussion 863-4. [DOI] [PubMed] [Google Scholar]
- 29.Deshpande SN, Mathur MN, Das SK, Bhatia T, Sharma S, Nimgaonkar VL. A Hindi version of the Diagnostic Interview for Genetic Studies. Schizophr Bull. 1998;24:489–93. doi: 10.1093/oxfordjournals.schbul.a033343. [DOI] [PubMed] [Google Scholar]
- 30.Maxwell E Family Interview for Genetic Studies (FIGS) Intramural Research Program – Clinical Neurogenetics Branch. Rockville: National Institute of Mental Health; 1992. [Google Scholar]
- 31.Gur RC, Ragland JD, Moberg PJ, et al. Computerized neurocognitive scanning: II. The profile of schizophrenia. Neuropsychopharmacology. 2001;25:777–88. doi: 10.1016/S0893-133X(01)00279-2. [DOI] [PubMed] [Google Scholar]
- 32.Sachs G, Steger-Wuchse D, Kryspin-Exner I, Gur RC, Katschnig H. Facial recognition deficits and cognition in schizophrenia. Schizophr Res. 2004;68:27–35. doi: 10.1016/S0920-9964(03)00131-2. [DOI] [PubMed] [Google Scholar]
- 33.Gur RE, Nimgaonkar VL, Almasy L, et al. Neurocognitive endophenotypes in a multiplex multigenerational family study of schizophrenia. Am J Psychiatry. 2007;164:813–9. doi: 10.1176/ajp.2007.164.5.813. [DOI] [PubMed] [Google Scholar]
- 34.Avila R, Bottino CM, Carvalho IA, Santos CB, Seral C, Miotto EC. Neuropsychological rehabilitation of memory deficits and activities of daily living in patients with Alzheimer's disease: a pilot study. Braz J Med Biol Res. 2004;37:1721–9. doi: 10.1590/s0100-879x2004001100018. [DOI] [PubMed] [Google Scholar]
- 35.Cohen J. Statistical Power Analysis for the Behavioral Scences. NJ: Erlbaum, Hillsdale; 1976. [Google Scholar]
- 36.Hochberg A sharper Bonferroni procedure for multiple tests of significance. Biometrika. 1988;75(4):800–802. [Google Scholar]
- 37.Nielsen BM, Mehlsen J, Behnke K. Altered balance in the autonomic nervous system in schizophrenic patients. Clin Physiol. 1988;8:193–9. doi: 10.1111/j.1475-097x.1988.tb00208.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.