Abstract
Background
Fatigue is a common and frequently observed complaint among older adults. However, knowledge about the nature and correlates of fatigue in old age is very limited. Objective: This study examined the relationship of functional indicators, psychological and situational factors and fatigue for 210 octogenarians and centenarians from the Georgia Centenarian Study.
Methods
Three indicators of functional capacity (self-rated health, instrumental activities of daily living, physical activities of daily living), two indicators of psychological well-being (positive and negative affect), two indicators of situational factors (social network and social support), and a multidimensional fatigue scale were used. Blocked multiple regression analyses were computed to examine significant factors related to fatigue. In addition, multi-group analysis in structural equation modeling was used to investigate residential differences (i.e., long-term care facilities vs. private homes) in the relationship between significant factors and fatigue.
Results
Blocked multiple regression analyses indicated that two indicators of functional capacity, self-rated health and instrumental activities of daily living, both positive and negative affect, and social support were significant predictors of fatigue among oldest-old adults. The multiple group analysis in structural equation modeling revealed a significant difference among oldest-old adults based on residential status.
Conclusion
The results suggest that we should not consider fatigue as merely an unpleasant physical symptom, but rather adopt a perspective that different factors such as psychosocial aspects can influence fatigue in advanced later life.
Key Words: Fatigue, Oldest-old adults, Georgia Centenarian Study
Introduction
Fatigue is defined as ‘a subjective state of overwhelming, sustained exhaustion and a decreased capacity for physical and mental work that is not relieved by rest’ [[1], p. 2]. Even though fatigue is common among older adults, especially older patients [2,3], fatigue has usually been identified as a universal symptom of disease and is frequently the first sign of some abnormal process [4]. Therefore, several studies on fatigue have focused on patients and their physical health problems such as cancer, bone marrow transplantation, chronic obstructive pulmonary disease or chemotherapy [5,6,7,8,9,10,11].
Fatigue has been characterized as the absence of energy from different perspectives from a physiological perspective [12,13], and most previous studies have been conducted in the context of physical functioning/disability, restricted activities, diseases, and pain with fatigue among older adults [14,15,16,17,18,19,20]. However, in order to obtain a comprehensive picture of fatigue, it is important to explore the influences of other factors such as social or psychological aspects explaining the association between tiredness and functional decline among the older population [20]. A few studies have examined emotional aspects of the relationship between fatigue and daily functioning among older women who had osteoarthritis, rheumatoid arthritis, and fibromyalgia [21]. Including psychological aspects of the relationship between functional ability and health may contribute to a more comprehensive understanding of fatigue [21] and affect, especially positive affect, as it appears to be a stronger predictor of health and functional ability [22]. Moreover, even though a number of studies have tried to identify psychosocial factors explaining fatigue [23,24,25], the relationship between social interaction/support and fatigue is not well understood, especially for older adults. Evidence of a significant relationship between social support or social interaction and fatigue has been found for healthy, younger adults [26,27]. For example, higher social support has been found to contribute to decreased levels of fatigue [26].
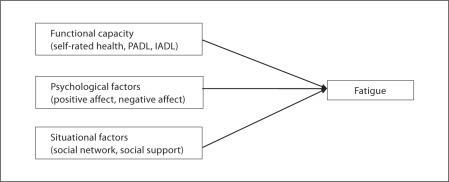
The middle-range theory of unpleasant symptoms [28] provides a theoretical perspective of a comprehensive picture of fatigue in association with multidimensional predictors such as social or psychological as well as physical aspects. The middle-range theory includes three major components: the symptoms, influencing factors that affect the symptoms, and the outcomes of the symptoms (e.g. performance). The concept of symptoms, the central aspect of this theory, refers to ‘the perceived indicators of change in normal functioning as experienced by individuals’ [[29], p. 242]. Consistent with prior research utilizing this theory which considered fatigue as a symptom [30,31,32,33], the current study will focus on fatigue as a symptom. An important contribution of the current study is the inclusion of multidimensional factors influencing fatigue. There are three different categories of influencing factors: functional capacity, psychological well-being, and situational context. Functional capacity refers to ‘anatomical/structural, physiological, genetic, and treatment-related variables’ [[34], p. 167]. Previous studies [33] defined activities of daily living as a manifestation of the ability to navigate one's day-to-day life, so the current study adhered to this definition. Psychological factors encompass ‘both affective and cognitive variables’ [[34], p. 168]. They indicate individuals' affective response to the symptom or levels of knowledge about the symptom that can impact the symptom experience [34]. Situational factors are defined as the individuals' social and physical environment [34]. For instance, individuals' background and accessibility to financial, emotional, or social support can influence symptoms [34]. Taken together, three influencing factors (i.e., functional capacity, psychological well-being, and situational context) in relationship to fatigue were the focus of this study (fig. 1).
Fig. 1.
Conceptual frame work: influencing factors and fatigue as a symptom. PADL = Physical activities of daily living; IADL = instrumental activities of daily living. Adapted from Chen et al. [30].
Even though fatigue is a commonly reported symptom among older adults and has been closely related to functional capacity [21,33], the influence of psychosocial factors is less known and few researchers have investigated an integrative assessment of the factors contributing to fatigue, especially among oldest-old adults. The proportion of oldest-old adults (those 85 years of age and older) is increasing rapidly and continuously in the US population as demonstrated by a 300% increase in those over 85 from 1960 to 2000 [28]. Several studies have investigated centenarians' functional abilities and various adaptational characteristics such as declining physical functioning, cognitive functioning, deterioration in housing, economic disadvantages, or nutritional risks [29,30,31,32]; however, these studies have not examined fatigue symptoms.
Potential factors attributed to the levels of fatigue among older adults have been identified as gender, residential settings and ethnicity. The gender difference of fatigue among older adults is still controversial. Two previous studies found there was no gender difference between men and women in musculoskeletal-related fatigue [35,36], but other studies suggested that women were less likely to feel tired compared to men especially in muscle fatigue [35,37,38,39]. Residential settings may be another factor to be considered as a significant predictor for fatigue. As people grow older, they are more likely to live in a care facility than a personal home [40]. The National Nursing Home Reports showed that less than 12% of older adults aged over 60 years live in care facilities, but the proportion is about 45% among those over 85 years of age and older [40]. As expected, nursing home/long-term care facility residents tend to have higher prevalence rates of chronic disease [41], and it may be assumed that this could lead to higher levels of fatigue. Furthermore, in terms of race/ethnic differences, previous studies found that race/ethnicity was associated with adverse symptoms which included fatigue [42]. Because of the evidence that gender, residential setting, and ethnicity may be related to fatigue, it is important to use these variables as covariates when assessing other predictors of fatigue.
Overall, our primary objective in the present study was to explore the relationship of fatigue with indicators of functional capacity (i.e., activities of daily living, self-rated health), psychological well-being (i.e., positive affect and negative affect), and situational factors (i.e., social networks and social support) in very late life using the middle-range theory of unpleasant symptoms. To pursue this objective, we examined data from the Georgia Centenarian Study (GCS, Phase III) [43]. Using these data, the following two research questions were addressed:
Are there significant associations of functional capacity, psychological well-being, and situation factors with fatigue among oldest-old adults?
Is there a difference in the relation between fatigue and functional capacity, psychological well-being, and situation factors among residents in long-term care facilities and those residing in private homes?
Methods
Participants
As discussed in our previous work [52], the sampling frame of the GCS (Phase III) [43], which provides data for this study, had two components. The first one was to identify the proportion of all residents of skilled nursing facilities and personal care homes in a 44-county area in northern Georgia. Based on Census proportions, the project identified residents of skilled nursing facilities and personal care homes as well as community-dwelling residents. The second recruiting strategy was to use the date-of-birth information in voter registration files. Based on these two components and five different characteristics (geographic, age, gender, race and type of residence), a sample of centenarians and octogenarians was drawn for this study [43].
This study included 210 community-dwelling and institutionalized octogenarians and centenarians who were cognitively intact (MMSE [44] score >17; average score 24.91). In this study, 66.2% of participants were centenarians and 73.8% were women. Over 70% of participants lived in a private home, apartment, or personal care facilities. The majority of the sample (82.9%) was White/Caucasian. Three quarters of respondents (76.2%) rated their health as good or excellent and almost 90% of participants reported knowing 5 or more people very well. In addition, over half of the sample (61.7%) received visits from people they knew. A summary of demographic characteristics is presented in table 1.
Table 1.
Summary of demographic characteristics
| Demographic characteristics | n | % |
|---|---|---|
| Age | ||
|
71 | 33.8 |
|
139 | 66.2 |
| Gender | ||
|
155 | 73.8 |
|
55 | 26.2 |
| Type of residence | ||
|
148 | 70.5 |
|
62 | 29.5 |
| Ethnicity | ||
|
174 | 82.9 |
|
36 | 17.1 |
| Subjective health | ||
|
7 | 3.4 |
|
42 | 20.4 |
|
114 | 55.3 |
|
43 | 20.9 |
| Number of people in social network | ||
|
7 | 3.4 |
|
14 | 6.8 |
|
184 | 89.8 |
| Frequency of visits | ||
|
16 | 7.8 |
|
12 | 5.8 |
|
51 | 24.8 |
|
127 | 61.7 |
Measures
Covariates. Gender, ethnicity and residential setting were used as covariates. Male was coded as ‘0’ and female was coded as ‘1’. Caucasian was coded as ‘1’ and African-American was coded as ‘0’. For the residential setting, there were two categories: private home (0) and long-term care facility residence (1).
Fatigue. Fatigue, as a symptom in this study, was assessed via the Multidimensional Fatigue Inventory (MFI) [45]. A multidimensional concept of fatigue was adopted given the belief that fatigue should be adequately associated in multi-causal models with other factors such as biomedical, psychosocial, or pathological factors [46]. The Multidimensional Fatigue Inventory consists of five sub-dimensions: general fatigue, physical fatigue, reduced activity, reduced motivation, and mental fatigue. Each sub-dimension has four indicators. General fatigue was assessed with items related to general tiredness (e.g., ‘I tire easily’, ‘I feel tired’), whereas physical fatigue was examined by items specifically associated with physical exhaustion and limitation (e.g., ‘physically, I feel I am in a bad condition’, ‘physically, I feel only able to do a little’). Reduced activity was comprised of questions such as ‘I think I do very little’, and ‘I get little done’. Reduced motivation was assessed including ‘I dread having to do things’, and ‘I don't feel like doing anything’. Lastly, mental fatigue was measured via items related to mental alertness (e.g., ‘My thoughts easily wander’, ‘It takes a lot of effort to concentrate on things’). All 20 items were scaled so that −1 = disagree, 0 = neutral, and 1 = agree, and the summary score of the 20 items was used in this study. Cronbach's α for multidimensional fatigue was 0.96. Scores ranged from −20 to 20, with higher scores indicating higher levels of fatigue.
Functional Factors. The self-care capacity (ADL) and self-rated health scales from the Duke Older Americans Resources and Services Procedures (OARS) [47] were used to assess daily functional ability. In terms of ADL, fourteen self-report items assessed the difficulty participants had with instrumental (e.g., shopping, cooking, and cleaning) and physical tasks (e.g., bathing or showering, dressing, eating, getting in and out of bed or a chair, walking, getting outside, and using the toilet). The functional assessment questionnaire of the Older Americans Resources and Services Procedures is highly reliable (r = 0.85) [47]. In our study, we used 10 of these 14 items after conducting a preliminary exploratory factor analysis. Cronbach's α for physical activity of daily living (PADL) and instrumental activity of daily living (IADL) was 0.85 and 0.83, respectively. The ranges for PADL and IADL were 0–10 and higher scores for instrumental and physical tasks indicated better functioning in each domain. Current subjective health was rated as excellent, good, fair, or poor, and was scaled so that 0 = poor to 3 = excellent.
Psychological Factors. Affect, an indicator of psychological well-being, was assessed with the Bradburn Affect Balance Scale [48]. The scale consists of two dimensions: positive affect and negative affect. Five positive affect items (α = 0.80) and five negative affect items (α = 0.80) were used in this study. Participants were asked to rate the following statements for positive affect: during the past 2 weeks, (1) did you ever feel pleased about having accomplished something?, (2) did you ever feel proud because someone complimented you on something you had done?, (3) did you ever feel particularly excited or interested in something?, (4) did you ever feel that things were going your way?, and (5) did you ever feel on top of the world? For negative affect, the following questions were asked: (1) did you ever feel depressed and very unhappy?, (2) did you ever feel vaguely uneasy?, (3) did you ever feel bored?, (4) did you ever feel so restless that you couldn't sit long in a chair?, and (5) did you ever feel very lonely or remote from other people? Ratings were used with a four-point Likert scale: 1 = not at all, 2 = once, 3 = several times, 4 = often. Higher scores for positive affect indicated higher levels of positive affect, whereas higher scores for negative affect indicated higher levels of negative affect.
Situational Factors. The Duke Older Americans Resources and Services Procedures [47] was used to gauge situational factors. Participants assessed the number of people within their social network (‘how many people do you know well enough to visit within your home or in their homes?’) and the frequency of visits as social support (‘how many times during the past week did you spend some time with someone who does not live with you; that is you went to see them or they came to visit you, or you went out to do things together?’). The 2 questions were used separately as single items. Higher scores indicated higher levels of social networks and social support as situational factors.
Analysis Plan
Data were analyzed using the SPSS statistical package (version 19.0). Bivariate correlations including means (M) and standard deviations (SD) were used to examine relationships among levels of fatigue, self-rated health, instrumental activities of daily living, physical activities of daily living, positive and negative affect, social network and social support (table 2). Blocked multiple regression models were computed to identify significant and independent predictors of fatigue as a symptom. In addition, multiple group analysis in structural equation modeling was used to investigate the possibility of residential differences using Mplus[49].
Table 2.
Correlation matrix for variables
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Covariate | |||||||||||
|
1 | ||||||||||
|
–0.04 | 1 | |||||||||
|
0.12 | 0.16* | 1 | ||||||||
| Functional capacity | |||||||||||
|
–0.13 | 0.05 | –0.06 | 1 | |||||||
|
–0.24** | 0.07 | –0.24** | 0.32** | 1 | ||||||
|
–0.13 | 0.05 | –0.34** | 0.29** | 0.64** | 1 | |||||
| Psychological factors | |||||||||||
|
–0.02 | 0.03 | –0.17* | 0.29** | 0.18** | 0.23** | 1 | ||||
|
0.10 | –0.02 | 0.01 | –0.18 | 0.03 | –0.04 | –0.21** | 1 | |||
| Situational factors | |||||||||||
|
–0.08 | –0.08 | –0.11 | 0.07 | 0.11 | 0.03 | 0.17** | –0.08 | 1 | ||
|
0.11 | –0.03 | –0.30** | 0.22** | 0.27** | 0.36** | 0.22** | –0.03 | 0.24** | 1 | |
|
0.02 | 0.03 | 0.21** | –0.38** | –0.38** | –0.34** | –0.40** | 0.29** | –0.14* | –0.26** | 1 |
| Means | 0.74 | 0.83 | 0.30 | 1.94 | 6.91 | 8.40 | 11.22 | 6.55 | 2.86 | 2.40 | –3.16 |
| SD | 0.44 | 0.38 | 0.46 | 0.74 | 2.83 | 2.14 | 3.37 | 2.28 | 0.43 | 0.91 | 6.34 |
ADL = Activities of daily living.
p < 0.05;
p < 0.01.
Results
Significant Predictors of Fatigue among Oldest-Old Adults
Using three different categories of variables and covariates, we computed blocked multiple regression analyses to investigate fatigue among oldest-old adults. The results are summarized in table 3. Four different models were computed. The first model included potentially influential demographic characteristics: gender, ethnicity, and residential setting. The second model included functional capacity (i.e., self-rated health, instrumental activities of daily living, and physical activities of daily living). The third model included demographic variables and psychological factors (i.e., positive and negative affect). Lastly, demographic variables and situational factors (i.e., social network and social support) were included in model 4. Three different blocked multiple regression analyses (models 2–4) were used to assess whether each model was a significant improvement over model 1.
Table 3.
Blocked regression models for fatigue
| Variables | Model 1 (n = 208) |
Model 2 (n = 204) |
Model 3 (n = 207) |
Model 4 (n = 204) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | B | SE | β | B | SE | β | B | SE | β | |
| Gender (female = 1) | –0.12 | 1.10 | –0.01 | –1.48 | 0.90 | –0.10 | –0.39 | 0.91 | –0.03 | 0.28 | 1.00 | 0.02 |
| Ethnicity (White = 1) | –0.12 | 1.16 | –0.01 | 0.76 | 1.03 | 0.05 | 0.27 | 1.06 | 0.02 | –0.12 | 1.15 | –0.01 |
| Residence (long-term care = 1) | 3.31 | 0.96 | 0.24** | 1.66 | 0.93 | 0.12+ | 2.44 | 0.90 | 0.18** | 2.26 | 1.01 | 0.16* |
| Self-rated health | –2.79 | 0.56 | –0.33*** | |||||||||
| Instrumental ADL | –0.65 | 0.18 | –0.29*** | |||||||||
| Physical ADL | –0.04 | 0.24 | –0.01 | |||||||||
| Positive affect | –0.60 | 0.12 | –0.32*** | |||||||||
| Negative affect | 0.60 | 0.18 | 0.22** | |||||||||
| Social network | –1.10 | 1.03 | –0.08 | |||||||||
| Social support | –1.48 | 0.52 | –0.21** | |||||||||
| FΔ | 4.03** | 22.43*** | 22.16*** | 5.88** | ||||||||
| R2 | 0.06 | 0.30 | 0.23 | 0.11 | ||||||||
| Adjusted R2 | 0.04 | 0.28 | 0.21 | 0.09 | ||||||||
ADL = Activities of daily living.
† p < 0.10;
p < 0.05;
p < 0.01;
p < 0.001.
Results from model 1 suggest that residence (β = 0.24, p < 0.01) was a significant predictor of fatigue. Long-term care facility residents were more likely to report higher levels of fatigue than private home residents. Adding functional capacity significantly improved the model, FΔ (3, 197) = 22.43, p < 0.001. Self-rated health (β = −0.33, p < 0.001) and instrumental activities of daily living (β = −0.29, p < 0.001) were significant predictors of fatigue in model 2. Those who rated their health as better and needed less help for their activities such as shopping, cooking, and cleaning from others felt less tired than those who rated their health worse and needed more help from others. Including psychological factors in model 3 significantly improved the model compared to model 1, FΔ (2, 201) = 22.16, p < 0.001. Positive affect (β = −0.32, p < 0.001) and negative affect (β = 0.22, p < 0.01) had significant influences on fatigue. Those who reported higher levels of positive affect and lower levels of negative affect also reported lower levels of fatigue. Finally, including situational factors (model 4) demonstrated another significant improvement, FΔ (2, 198) = 5.88, p < 0.01, over model 1. Those who spent more time with acquaintances had lower levels of fatigue.
Residential Differences in Fatigue
Given the significance of residential setting on fatigue in models 1–4 (table 3), the second issue that we addressed was whether the significant predictors for fatigue were consistent for long-term care facility residents and private home residents. To address this question, regression analysis was conducted simultaneously for long-term care facility residents and private home residents with the multiple-group option in Mplus[49]. Thus, we were able to compare the path coefficients that were derived for the two different residential settings.
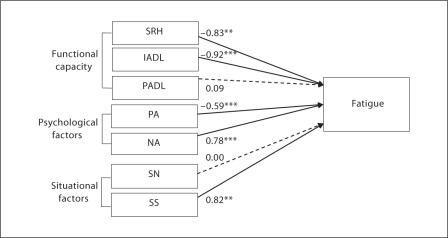
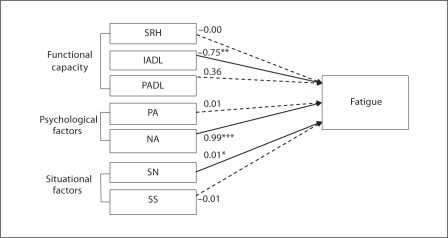
To test this question, the fit of two models were compared. The first model assumed that the causal paths from predictors in table 3 to fatigue were the same for long-term care facility residents and private home residents. The alternative model allowed the causal paths from the variables to fatigue to vary for two different residential settings. Freeing these paths significantly altered the fit of the model. The χ2 difference test indicated that there was a significant difference, χ2 (7, n = 210) = 31.73, p < 0.001. The differences in the 2 different models are shown in figures 2 and 3.
Fig. 2.
The relationships among fatigue, functional capacity (self-rated health, instrumental activities of daily living, physical activities of daily living), psychological factors (positive affect, negative affect), and situational factors (social network, social support) among private home residents. Note: Path coefficients are standardized parameter estimates and significant paths are displayed by solid lines. Nonsignificant paths are displayed by broken lines. SRH = Self-rated health; PADL = physical activities of daily living; IADL = instrumental activities of daily living; PA = positive affect; NA = negative affect; SN = social network; SS = social support. ** p < 0.01; *** p < 0.001.
Fig. 3.
The relationships among fatigue, functional capacity (self-rated health, instrumental activities of daily living, physical activities of daily living), psychological factors (positive affect, negative affect), and situational factors (social network, social support) among long-term care residents. Note: Path coefficients are standardized parameter estimates and significant paths are displayed by solid lines. Nonsignificant paths are displayed by broken lines. SRH = Self-rated health; PADL = physical activities of daily living; IADL = instrumental activities of daily living; PA = positive affect; NA = negative affect; SN = social network; SS = social support. * p < 0.05; ** p < 0.01; *** p < 0.001.
Based on the alternative model (the model which freed the causal paths), self-rated health (β = −0.83, p < 0.01), instrumental activities of daily living (β = −0.92, p < 0.001), positive affect (β = −0.59, p < 0.001), negative affect (β = 0.78, p < 0.001), and social support (β = 0.82, p < 0.01) were significant predictors of levels of fatigue among private home residents (fig. 2). Among older adults who did not reside in a long-term care facility, those persons who rated their health as worse needed more help from others for instrumental activities of daily living, had lower levels of positive affect, higher levels of negative affect, and had more visits of acquaintances, felt more fatigued. In contrast, predictors of fatigue among long-term care facility residents were different. Instrumental activities of daily living (β = −0.75, p < 0.01), negative affect (β = 0.99, p < 0.001), and social networks (β = 0.01, p < 0.05) were significantly associated with levels of fatigue (fig. 3). Among long-term care facility residents, persons reporting high functioning with instrumental activities of daily living, higher levels of negative affect, and more people within their social network also reported increased levels of fatigue.
Discussion
Fatigue is a common symptom in older adults. Fatigue is usually related to specific diseases such as cancer, chronic obstructive pulmonary disease, or chemotherapy [5,6,7,8,9,10,11]; however, idiopathic (non-disease related) fatigue is also reported by older adults. Physical functioning, psychological status or social interaction with others might influence unexplained fatigue of older adults, especially among oldest-old adults. The purpose of this study therefore was to explore significant predictors of fatigue for centenarians and octogenarians of the Georgia Centenarian Study with the middle-range theory of unpleasant symptoms.
Four sets (i.e., covariates, functional capacity, psychological well-being, and situational factors) of blocked multiple regressions were computed to examine significant factors related to fatigue. First, blocked multiple regressions showed expected results. Self-rated health and instrumental activities of daily living, two indicators of functional capacity, were important for fatigue among oldest-old adults. Participants who rated their health as poor and needed less help from others for activities such as shopping, cooking, and cleaning felt higher levels of fatigue. This finding is consistent with previous results suggesting that there is a significant relationship between physical health, self-rated health, and fatigue [50], and that fatigue is a significant determinant limiting activity for community-dwelling adults [15]. In addition, the data further reveal the importance of psychological aspects, especially positive and negative affect, for fatigue. This is consistent with findings reported by Zautra et al. [21] which also indicate a significant relationship between affect, both positive and negative affect, and fatigue. It is intriguing that there was a significant effect of affect on fatigue. Most studies on fatigue among older adults focus on fatigue as a physical symptom and emphasized relationships with physical aspects such as chronic diseases, health, or physical functioning [17,18,19,20]. This result suggests that we should have a holistic understanding for fatigue as it relates to other factors. Specifically, the current findings revealed a significant relationship between fatigue and social support which is a situational factor (i.e., social network and social support). Previous studies [26,27,51] focused on only healthy and young-old adults. This finding extends previous research noting that social support had a significant effect on fatigue for oldest-old adults.
Multiple group analysis in SEM indicated the importance of residential differences in understanding fatigue among oldest-old adults. A noteworthy finding of this study was the detection of residential differences (i.e., long-term care facility vs. more private setting) for the relationships among functional, psychological, situational factors and fatigue. Self-rated health, instrumental activities of daily living, both positive and negative affect, and social support were significant predictors of fatigue among private home residents. This suggests that most of the indicators of three factors (functional, psychological, and situational factors) were important predictors of fatigue symptomatology for private home residents. Surprisingly, we found that there was a significant relationship between social network and fatigue among oldest-old adults who lived in apartments, personal care, or private homes. In other words, it might be more tiring to have more people to interact with in very later life. While interactions with acquaintances may improve quality of life, fatigue may be an unwanted consequence among the oldest-old population.
In terms of long-term care facility residents, instrumental activities of daily living and negative affect were strong predictors of fatigue. Even though participants lived in long-term care facilities, those who had better functioning of activities such as shopping, cooking, and cleaning, and had lower levels of negative affect had lower levels of fatigue. Situational factors also played a different role for this subsample. Social support was a strong significant factor for private home residents but not for long-term care facility residents. Whereas social support had a significant influence on fatigue (β = 0.82, p < 0.01) among private home residents, it was not as strong as social networks in predicting fatigue (β = 0.01, p < 0.05) among long-term care facility residents. One possible explanation that the two social factors differed by residential setting is that social support given in long-term care facilities is not systematically associated with fatigue as it is primarily considered to be formal support. In essence, long-term care facility residents can typically count on a certain amount of support. This is another important finding of this study suggesting the inclusion of situational factors for fatigue with oldest-old participants. Most studies that investigated the influences of social support or social networks on fatigue included only younger and healthy participants [26,27].
Another significant aspect of this study is the focus on advanced old age. Even though fatigue is typically approached as poor energy utilization from a physiological perspective, more attention should be paid to fatigue as both an unexplained/idiopathic symptom and multidimensional concept among older adults. Therefore, focusing on fatigue, as a multidimensional aspect, in advanced old age and its influence on the relationship among functional, psychological, and social aspects could be helpful to develop more sophisticated interventions that consider distinct disease-related and psychosocial influences in advanced old age [21].
When interpreting the present results, limitations of this study should be considered. First, it cannot be assumed that the observed relationship among affect, fatigue and physical functioning is causal because of the cross-sectional research design. Second, the participants of this study were recruited from only one geographic region of the United States. Individuals from other parts of United States or other countries might demonstrate different patterns in the relationship among fatigue, functional capacity, psychological well-being, and situational factors. Future research on fatigue and other significant predictors should assess changes over time and should include representative participants.
Although fatigue is a common symptom among the older population, most studies have considered fatigue as a physical symptom or sign for physical disease. Beyond physical mechanism, a psychosocial approach to fatigue is largely unknown. This study suggests that practitioners and caregivers for oldest-old adults should address symptoms of fatigue with early management of symptoms and by providing support that enhances quality of life at the end of life. In sum, the present study demonstrates that there is a significant role of functional, psychological, and social aspects on fatigue. The results suggest that we should consider fatigue not just an unpleasant and physical symptom, but a critical symptom related to various factors such as psychosocial factors in very later life.
Acknowledgements
The Georgia Centenarian Study (Leonard W. Poon, PI) was funded by 1P01-AG17553 from the National Institute on Aging, a collaboration among the University of Georgia, Tulane University Health Sciences Center, Boston University, University of Kentucky, Emory University, Duke University, Wayne State University, Iowa State University, Temple University, and University of Michigan. Authors acknowledge the valuable recruitment and data acquisition effort of M. Burgess, K. Grier, E. Jackson, E. McCarthy, K. Shaw, L. Strong and S. Reynolds, data acquisition team manager; S. Anderson, E. Cassidy, M. Janke, and J. Savla, data management; M. Poon for project fiscal management.
References
- 1.Poluri A, Mores J, Cook DB, Findley TW, Cristian A. Fatigue in the elderly population. Phys Med Rehabil Clin N Am. 2005;16:91–108. doi: 10.1016/j.pmr.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 2.Gialamas A, Beilby JJ, Pratt NL, Henning R, Marley JE, Roddick JF. Investigating tiredness in Australian general practice. Do pathology tests help in diagnosis? Aust Fam Physician. 2003;32:663–666. [PubMed] [Google Scholar]
- 3.Murtagh J. Fatigue – a general diagnostic approach. Aust Fam Physician. 2003;32:873–876. [PubMed] [Google Scholar]
- 4.Ferrell BR, Grand M, Funk B, Ly J. ‘Bone tired’: the experience of fatigue and its impact on quality of life. Oncol Nurs Forum. 1996;23:1539–1547. [Google Scholar]
- 5.Blesch KS, Paice JA, Wichkham R, Harte N, Schnoor DK, Purl S, Rehwalt M, Kopp PL, Mason S, Coveny SB, McHale M, Cahill M. Correlates of fatigue in people with breast or lung cancer. Oncol Nurs Forum. 1991;18:81–87. [PubMed] [Google Scholar]
- 6.Cimprich B. Attentional fatigue following breast surgery. Res Nurs Health. 1992;15:199–207. doi: 10.1002/nur.4770150306. [DOI] [PubMed] [Google Scholar]
- 7.Grant M, Ferrell BR, Schmidt GM, Fonbuena P, Niland JC, Forman SF. Measurement of quality of life in bone marrow transplant survivors. Qual Life Res. 1992;1:375–384. doi: 10.1007/BF00704432. [DOI] [PubMed] [Google Scholar]
- 8.Nail L, Jones L, Greene D, Schipper D, Jensen R. Use and perceived efficacy of self-care activities in patients receiving chemotherapy. Oncol Nurs Forum. 1991;18:883–887. [PubMed] [Google Scholar]
- 9.Rhode VA, Watson PM, Hanson BM. Patients descriptions of the influence of tiredness and weakness on self-care abilities. Cancer Nurs. 1988;11:186–194. [PubMed] [Google Scholar]
- 10.Rhoten D. Fatigue and postsurgical patient. In: Norris C, editor. Concept Clarification in Nursing. Rockville: Aspen; 1982. pp. 277–300. [Google Scholar]
- 11.Walke LM, Byers AL, Tinetti ME, Dubin JA, McCorkle R, Fried TR. Range and severity of symptoms over time among alder adults with COPD and HF. Arch Intern Med. 2007;167:2503–2508. doi: 10.1001/archinte.167.22.2503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alexander NB, Raffet GE, Horne FM, Eldadah BA, Ferrucci L, Nayfield S, Studenski S. Bedside-to-bench conference: research agenda for idiopathic fatigue and aging. J Am Geriatr Soc. 2010;58:967–975. doi: 10.1111/j.1532-5415.2010.02811.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilson MM, Morley JE. Invited review: Aging and energy balance. J Appl Physiol. 2003;95:1728–1736. doi: 10.1152/japplphysiol.00313.2003. [DOI] [PubMed] [Google Scholar]
- 14.Martin P, Long MV, Poon LW. Age changes and differences in personality traits and states of the old and very old. J Gerontol B Psychol Sci Soc Sci. 2002;57B:P144–P152. doi: 10.1093/geronb/57.2.p144. [DOI] [PubMed] [Google Scholar]
- 15.Gill TM, Desai MM, Gahbauer EA, Holford TR, Williams CS. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Ann Intern Med. 2001;135:313–321. doi: 10.7326/0003-4819-135-5-200109040-00007. [DOI] [PubMed] [Google Scholar]
- 16.Dean G, Ferrell BR. The meaning of cancer pain. Semin Oncol Nurs. 1995;11:17–21. doi: 10.1016/s0749-2081(95)80038-7. [DOI] [PubMed] [Google Scholar]
- 17.Avlund K, Damsgaard MT, Sakari-Rantala R, Laukkanen P, Schroll M. Tiredness in daily activities among non-disabled old people as determinant of onset of disability. J Clin Epidemiol. 2002;55:965–973. doi: 10.1016/s0895-4356(02)00463-8. [DOI] [PubMed] [Google Scholar]
- 18.Avlund K, Pedersen AN, Schroll M. Functional decline from age 80 to 85: influence of preceding changes in tiredness in daily activities. Psychosom Med. 2003;65:771–777. doi: 10.1097/01.psy.0000082640.61645.bf. [DOI] [PubMed] [Google Scholar]
- 19.Avlund K, Sakari-Rantala R, Rantanen T, Pedersen AN, Frandin K, Schroll M. Tiredness and onset of walking limitations in older adults. J Am Geriatr Soc. 2004;52:1963–1965. doi: 10.1111/j.1532-5415.2004.52529_2.x. [DOI] [PubMed] [Google Scholar]
- 20.National Institute on Aging (NIA) Unexplained fatigue in the elderly: an exploratory workshop sponsored by the National Institute on Aging. Unpublished workshop summary2007
- 21.Zautra AJ, Fasman R, Parish BP, Davis MC. Daily fatigue in women with osteoarthritis, rheumatoid arthritis, and fibromyalgia. Pain. 2007;128:128–135. doi: 10.1016/j.pain.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 22.Benyamini Y, Ilder EL, Leventhal H, Leventhal EA. Positive affect and function as influences on self-assessment of health. J Gerontol B Psychol Sci Soc Sci. 2000;55:P107–P116. doi: 10.1093/geronb/55.2.p107. [DOI] [PubMed] [Google Scholar]
- 23.Nakao M, Fricchione G, Zuttermeister PC, Myers P, Barsky AJ, Benson H. Effects of gender and marital status on somatic symptoms of patients attending a mind/body medicine clinic. Behav Med. 2001;26:159–168. doi: 10.1080/08964280109595763. [DOI] [PubMed] [Google Scholar]
- 24.Mansuso CA, Rincon M, Sayles W, Paget SA. Psychosocial variables and fatigue: a longitudinal study comparing individuals with rheumatoid arthritis and healthy controls. J Rheumatol. 2006;33:1496–1502. [PubMed] [Google Scholar]
- 25.Stewart D, Abbey S, Meana M, Boydell KM. What makes women tired: a community sample. J Womens Health. 1988;7:69–76. doi: 10.1089/jwh.1998.7.69. [DOI] [PubMed] [Google Scholar]
- 26.Aaronson LS, Pallikkathayil L, Crighton F. Qualitative investigation of fatigue among healthy working women. West J Nurs Res. 2003;25:419–433. doi: 10.1177/0193945903025004007. [DOI] [PubMed] [Google Scholar]
- 27.Dzurec LC. Relationship as an inherent component in healthy women's fatigue. West J Nurs Res. 2002;24:441–453. doi: 10.1177/01945902024004010. [DOI] [PubMed] [Google Scholar]
- 28.Lenz ER, Pugh LC, Miligan RA, Gift AG, Suppe F. The middle-range theory of unpleasant symptoms: an update. ANS Adv Nurs Sci. 1997;19:14–27. doi: 10.1097/00012272-199703000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Rhodes VA, Watson PM. Symptom distress – the concept: past and present. Semin Oncol Nurs. 1987;3:242–247. doi: 10.1016/s0749-2081(87)80014-1. [DOI] [PubMed] [Google Scholar]
- 30.Chen LH, Li CY, Shieh SM, Y WH, Chiou AF. Predictors of fatigue in patients with heart failure. J Clin Nurs. 2010;19:1588–1596. doi: 10.1111/j.1365-2702.2010.03218.x. [DOI] [PubMed] [Google Scholar]
- 31.Francoeur RB. The relationship cancer symptom clusters to depressive affect in the initial phase of palliative radiation. J Pain Symptom Manage. 2005;29:130–155. doi: 10.1016/j.jpainsymman.2004.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sarna L, Evangelista D, Tashkin G, Padilla CH, Brecht ML, et al. Impact of respiratory symptoms and pulmonary function on quality of life of long-term survivor of non-small cell lung cancer. Chest. 2004;125:439–445. doi: 10.1378/chest.125.2.439. [DOI] [PubMed] [Google Scholar]
- 33.Wilmonth MC, Colemena EA, Smith SC, Davis C. Fatigue, weight gain and altered sexuality in patients with breast cancer: exploration of a symptom cluster. Oncol Nurs Forum. 2004;31:1069–1075. doi: 10.1188/04.ONF.1069-1075. [DOI] [PubMed] [Google Scholar]
- 34.Lenz ER, Pugh LC. The theory of unpleasant symptoms. In: Smith MJ, Liehr P, editors. Middle Range Theory for Nursing. New York: Springer; 2007. pp. 159–182. [Google Scholar]
- 35.Hunter SK, Critchlow A, Enoka RM. Influence of aging on sex differences in muscle fatigability. J Appl Physiol. 2004;97:1723–1732. doi: 10.1152/japplphysiol.00460.2004. [DOI] [PubMed] [Google Scholar]
- 36.Melzer I, Benjuya N, Kaplanski J. Age related changes in muscle strength and fatigue. Isokinet Exerc Sci. 2000;8:73–83. [Google Scholar]
- 37.Hunter SK, Enoka RM. Sex differences in the fatigability of arm muscles depends on absolute force during isometric contractions. J Appl Physiol. 2001;91:2686–2694. doi: 10.1152/jappl.2001.91.6.2686. [DOI] [PubMed] [Google Scholar]
- 38.Kent-Braun JA, Ng AV, Doyle JW, Towse TF. Human skeletal muscle responses vary with age and gender during fatigue due to incremental isometric exercise. J Appl Physiol. 2002;93:1813–1823. doi: 10.1152/japplphysiol.00091.2002. [DOI] [PubMed] [Google Scholar]
- 39.Miller AEJ, Macdougall JD, Tarnopolsky MA, Sale DG. Gender differences in strength and muscle-fiber characteristics. Eur J Appl Physiol O. 1993;66:254–262. doi: 10.1007/BF00235103. [DOI] [PubMed] [Google Scholar]
- 40.Jones AL, Dwyer LL, Bercovitz AR, Strahan GW. The National Nursing Home Survey: 2004 overview. Vital Health Stat. 2009;167:1–155. [PubMed] [Google Scholar]
- 41.Shah SM, Carey IM, Harris T, DeWilde S, Hubbard R, Lewis S, Cook DG. Identifying the clinical characteristics of older people living in care homes using a novel approach in a primary care database. Age Ageing. 2010;39:617–623. doi: 10.1093/ageing/afq086. [DOI] [PubMed] [Google Scholar]
- 42.Tammemagi CM, Neslund-Dudas C, Simoff M, Kvale P. Lung carcinoma symptoms – an independent predictor of survival and an important mediator of African-American disparity in survival. Cancer. 2004;101:1655–1663. doi: 10.1002/cncr.20547. [DOI] [PubMed] [Google Scholar]
- 43.Poon LW, Jazwinski SM, Green RC, Woodard JL, Martin P, Rodgers WL, Johnson MA, Hausman D, Arnold J, Davey A, Batzer MA, Markesbery WR, Gearing M, Siegler IC, Reynolds S, Dai J. Methodological considerations in studying centenarians: lessons learned from the Georgia Centenarian Studies. In: Poon LW, Perls TT, editors. Annual Review of Gerontology and Geriatrics. New York: Springer; 2007. pp. 231–264. [PMC free article] [PubMed] [Google Scholar]
- 44.Folstein MF, Folstein SE, McHugh PR. ‘Minimental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 45.Smets EM, Garssen B, Bonke B, De Haes JC. The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res. 1995;39:315–325. doi: 10.1016/0022-3999(94)00125-o. [DOI] [PubMed] [Google Scholar]
- 46.Bensing JM, Hulsman RL, Schreurs KMG. Gender differences in fatigue: biopsychosocial factors relating to fatigue in men and women. Medical Care. 1999;37:1078–1083. doi: 10.1097/00005650-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 47.Fillenbaum GG. Multidimensional Functional Assessment of Older Adults: The Duke Older Americans Resources and Services Procedures. Hillsdale: Erlbaum; 1988. [Google Scholar]
- 48.Bradburn N. The Structure of Psychological Well-Being. Chicago: Aldine; 1969. [Google Scholar]
- 49.Muthén LK, Muthén BO. Mplus User's Guide. ed 5. Los Angeles: Muthén & Muthén; 1998. [Google Scholar]
- 50.Adams KB. Depressive symptoms, depletion, or developmental change? Withdrawal, apathy, and lack of vigor in the Geriatric Depression Scale. Gerontologist. 2001;41:768–777. doi: 10.1093/geront/41.6.768. [DOI] [PubMed] [Google Scholar]
- 51.Kwag KH, Martin P, Russell D, Franke W, Kohut M. The impact of perceived stress, social support, and home-based physical activity on mental health among older adults. Int J Aging Hum Dev. 2011;72:137–154. doi: 10.2190/AG.72.2.c. [DOI] [PubMed] [Google Scholar]
- 52.Cho J, Martin P, MacDonald M, Margrett J, Poon LW.The relationship between health and psychological well-being among oldest-old adults. J Aging Res DOI: 10.4061/2011/605041. [DOI] [PMC free article] [PubMed]