Abstract
Bronchopulmonary dysplasia (BPD), a chronic lung disease of infancy, is characterized by arrested alveolar development. Pulmonary angiogenesis, mediated by the vascular endothelial growth factor (VEGF) pathway, is essential for alveolarization. However, the transcriptional regulators mediating pulmonary angiogenesis remain unknown. We previously demonstrated that NF-κB, a transcription factor traditionally associated with inflammation, plays a unique protective role in the neonatal lung. Therefore, we hypothesized that constitutive NF-κB activity is essential for postnatal lung development. Blocking NF-κB activity in 6-day-old neonatal mice induced the alveolar simplification similar to that observed in BPD and significantly reduced pulmonary capillary density. Studies to determine the mechanism responsible for this effect identified greater constitutive NF-κB in neonatal lung and in primary pulmonary endothelial cells (PEC) compared with adult. Moreover, inhibiting constitutive NF-κB activity in the neonatal PEC with either pharmacological inhibitors or RNA interference blocked PEC survival, decreased proliferation, and impaired in vitro angiogenesis. Finally, by chromatin immunoprecipitation, NF-κB was found to be a direct regulator of the angiogenic mediator, VEGF-receptor-2, in the neonatal pulmonary vasculature. Taken together, our data identify an entirely novel role for NF-κB in promoting physiological angiogenesis and alveolarization in the developing lung. Our data suggest that disruption of NF-κB signaling may contribute to the pathogenesis of BPD and that enhancement of NF-κB may represent a viable therapeutic strategy to promote lung growth and regeneration in pulmonary diseases marked by impaired angiogenesis.
Keywords: bronchopulmonary dysplasia, endothelial cells, vascular endothelial growth factor receptor-2
the formation of the alveoli by secondary septation allows for the 20-fold increase in surface area of the lung, necessary for effective air breathing existence (15). Bronchopulmonary dysplasia (BPD), a chronic lung disease that affects premature infants (67), results from disrupted secondary septation, leading to larger and fewer alveoli, thereby reducing gas exchange surface area (27). Infants with BPD require significant respiratory support early in life and have an increased risk for developing lung diseases in the future, such as asthma, pulmonary hypertension, and emphysema (17, 25, 74). Physiological angiogenesis is essential for postnatal lung development, and compromised pulmonary angiogenesis impairs alveolarization, leading to BPD. Moreover, signaling via the vascular endothelial growth factor (VEGF) signaling pathway appears to specifically drive postnatal angiogenesis and alveolarization. VEGF expression is decreased in the lungs of infants dying from BPD (9) and in a neonatal rat model of BPD induced by hyperoxia (70). Inhibiting VEGF receptor-2 (VEGFR2) in neonatal rats causes rarefaction of pulmonary vessels and impairs alveolar formation (34), whereas enhancement of VEGF signaling rescues the alveolar disruption induced by hyperoxia. Blocking postnatal angiogenesis impairs alveolarization in animal models (40), and decreased pulmonary capillary density is observed in patients dying from BPD (9). However, although the connection between angiogenesis and postnatal lung development is clear, the transcriptional regulators mediating postnatal pulmonary angiogenesis are not known.
During development, the NF-κB family of transcription factors plays a key role in cell survival, lymphocyte differentiation, and innate immunity (23, 73). The NF-κB family is comprised of five subunits, each able to homo- or heterodimerize with each other and associate with alternate transcription factors, thereby enabling regulation of genes in a tissue- and context-specific manner (32). NF-κB dimers remain inactive in the cytoplasm of cells in association with an inhibitory protein, IκB. Activation of NF-κB by the IκB kinases, IKK-α and -β, in response to cytokines, growth factors, or bacterial products results in the phosphorylation and subsequent degradation of IκBs (52). The removal of IκB allows active NF-κB complexes to translocate into the nucleus and regulate diverse downstream targets that regulate inflammation, cell adhesion, and cell survival. Clinical and experimental evidence has implicated NF-κB-mediated gene regulation in the pathogenesis of a number of pulmonary diseases including acute lung injury, asthma, and cystic fibrosis (14, 20, 24, 69). In the vasculature, increased NF-κB activity plays a key pathogenic role in a number of diseases marked by inflammation and abnormal proliferation, including aneurysm formation (4, 5), pulmonary hypertension (51, 63), and atherosclerosis (21). However, although extensive data links increased NF-κB to pulmonary and vascular pathology, a physiological role for NF-κB in pulmonary vascular development has not been previously described.
In contrast to its well-described pathological role in the adult, our previous work identified a uniquely protective role for NF-κB in the neonate (2). Although both neonatal and adult mice activated NF-κB in the lung after exposure to systemic lipopolysaccharide (LPS), the lungs of the neonatal mice were significantly less inflamed than the adult lungs. Furthermore, whereas blocking NF-κB in LPS-treated adult mice decreases lung inflammation (11, 35), we found that blocking NF-κB in the LPS-treated neonatal mice paradoxically increased inflammation. This observation motivated the hypothesis that perhaps NF-κB plays an essential role in the developing lung.
In this study, we demonstrate that pharmacological blockade of NF-κB in neonatal mice reduces pulmonary capillary density and induces the alveolar simplification pathognomonic for BPD. We identify a high level of constitutive NF-κB activity in the neonatal pulmonary endothelium compared with the adult pulmonary endothelium. Furthermore, blocking NF-κB increases apoptosis, decreases proliferation, and impairs angiogenesis, suggesting that this constitutive NF-κB activity is critical for neonatal pulmonary endothelial cell (PEC) homeostasis. Finally, as a putative mechanism accounting for these effects, we demonstrate that NF-κB directly regulates the expression of the proangiogenic molecule, VEGFR2, in the developing pulmonary vasculature.
MATERIALS AND METHODS
Animal model.
Neonatal (6 day) C57BL/6 mice were injected intraperitoneally (i.p.) with either vehicle (DMSO in PBS + 20% Tween-80) or 10 mg/kg of BAY 11–7082 (EMD Chemicals, Gibbstown, NJ). For each litter, half of the pups were given vehicle, and half of the pups treated with BAY. At 24 h and 7 days after treatment, the animals were killed and lungs were fixed at 25 cm H2O pressure with 10% formalin and paraffin embedded for histology. Similar experiments were performed in adult mice (aged 8–12 wk) treated with vehicle or BAY, with formalin fixation at 24 h and 7 days. Frozen sections of control neonatal and adult mice and in neonatal mice 24 h after vehicle or BAY treatment were obtained by first inflating the lungs with a 1:1 ratio of PBS and optimal cutting temperature compound (OCT)-embedding medium (Sakura Finetek, Torrance, CA) at a pressure of 35 cm H2O pressure (due to the high viscosity), then immersed in OCT, and snap frozen before cryosectioning. Additional neonatal lungs were snap frozen at 8 and 24 h for RNA and protein isolation. All animal procedures were approved by the Institutional Animal Care and Use Committee (IACUC) at Stanford University.
Morphometry.
Morphometric analysis was performed on neonatal and adult lung sections after formalin fixation (described above). For each animal, the entire lung was sectioned serially, and multiple areas of the lung were evaluated by performing measurements on three randomly chosen sections that were at least 250 μm apart in distance. Brightfield images of hematoxylin and eosin (H&E)-stained lung tissue were acquired using a Leica DM5500 upright microscope and a Micropublisher 5MPixel, color digital camera, using HC Plan Apo 25-mm objectives at ×10 and ×20 magnification (Leica Microsystems, Buffalo Grove, IL). Radial alveolar counts were determined in a minimum of 30 perpendicular lines per animal (19) derived from three lung sections per animal and averaged to give a single value per mouse. The mean linear intercept was determined using the method described by Knudsen et al. (37) on five randomly chosen ×20 images per section, with the total values derived from three sections averaged into a single value per mouse (37). For each experiment, 5–8 animals per group were used.
CD31 immunohistochemistry.
Formalin-fixed lung sections were incubated with primary antibody for platelet endothelial cell adhesion molecule (PECAM)-1 (Dianova, Hamburg, Germany), and formalin-fixed lung tissue was incubated with a biotinylated primary antibody against PCNA (Invitrogen, Carlsbad, CA) overnight at 4°C. Slides were then incubated with the appropriate biotinylated secondary antibody, followed by Vectastain ABC reagent (Vector Laboratories, Burlingame, CA), and color was developed with diaminobenzidine peroxidase substrate per the manufacturer's protocol (31). The CD-31 immunoreactive (endothelial) area relative to air-exchanging parenchymal area was determined in 15 nonoverlapping, random fields, derived from three lung sections that were at least 250 μm apart in distance, using a point-counting method in which a computer-derived 7,575-point lattice grid was superimposed on the images, and the number of points falling on CD-31-positive tissue was divided by the number of points falling on parenchymal tissue. The values were then averaged to derive a single value of vascular density for each animal.
Immunofluorescent staining of lung tissue.
Neonatal and adult lung tissue was collected after either cryo-preservation or formalin fixation as described above. Fixed tissue sections were deparaffinized and rehydrated. A basic antigen retrieval solution (R&D Systems, Minneapolis, MN) has been applied for 30 min at 95°C (tissues have been cooled down for 30 min at room temperature). Both fixed or frozen tissue sections were submitted to a 30-min treatment with a 1× PBS/0.25% Triton-X 100 solution, after which they were rinsed in PBS for 5 min twice. To quench the autofluorescence generated by aldehyde residues, fixed tissue sections were incubated for 20 min in a 100 mM glycine solution (pH 7.5), followed by treatment with 0.5% Pontamine Sky Blue 5BX (Sigma, St. Louis, MO). Lipofuscein autofluorescence was reduced in frozen sections by treatment with 10 mM CuSO4 for 15 min (65). After the quenching of the autofluorescence, both frozen and fixed tissue sections were incubated for 40 min in nondiluted Sea Block Blocking Solution (Thermo Scientific, Waltham, MA), rinsed in PBS, and then incubated in nondiluted Fc Receptor Blocker solution (Innovex Biosciences, Richmond, CA) for 30 min. After being rinsed in PBS, tissue sections were then incubated overnight at 4°C with either of the following primary antibodies: VEGFR2 (1:250; Cell Signaling, Danvers, MA), PCNA (1:150; Abcam, Cambridge, MA), active caspase-3 (1:200; Cell Signaling), NF-κB-p65 (1:200; Santa Cruz Biotechnology, Santa Cruz, CA); the endothelial cells were then labeled by incubation with antibodies against CD31 (1:200 for frozen tissue; BD Pharmingen, San Diego, CA; or 1:200 for fixed tissue; Dianova ). After being probed with the primary antibody, sections were washed in PBS for 3 × 10 min and then incubated with the suitable fluorochrome-labeled secondary antibodies: goat anti-rabbit Alexa Fluor 488, goat anti-rat Alexa Fluor 647, and goat anti-rabbit Alexa Fluor 568 (1:200; Invitrogen/Molecular Probes). Chromatin was counterstained with 10 mg/ml Hoechst reagent (Sigma-Aldrich) diluted in H2O (1:10,000). Specimens were examined by confocal microscopy using an Olympus FV-1000 laser scanning confocal microscope (HeNe/Ar). The acquisition parameters for the photomultiplier included a detector gain of 1, amplifier offset 1%, and the high voltage values for each spectral line of 450 for blue and 650 for green or red. Images were captured sequentially for each spectral line and corrected using Kalman filtered algorithm. Images were obtained with either ×40 or ×60 oil immersion objectives, using a zoom factor of 1 or 2. Confocal aperture was 80 μm, acquisition mode was slow (4–8 pixel/s), and xy-frame size was 2,048 × 2,048 pixels. The interval values on the Look Up Table were 0–4,045 for the blue spectral line, 150–1,500 for the red spectral line, and 50–750 for the green spectral line. The laser power applied on the samples was 5% for the blue laser, 15% for the red laser, and 25% for the far-red laser. Confocal micrograms were processed using Fluoview software (Olympus). Each selected frame is a representative image obtained from serial confocal Z-sections (where the Z-interval between 2 sections was 0.2 μm) within a stack of 20 sections.
Isolation of PEC.
PEC were isolated from neonatal and adult mouse lungs after digestion of whole lung tissue with collagenase IA (0.5 mg/ml) for 30 min at 37°C, and incubation of cell homogenate for 15 min was done at room temperature with anti-CD31-coated magnetic beads (Dynabeads, Invitrogen) (29), followed by magnet separation per the manufacturer's protocol. PEC were then cultured in endothelial growth media (EGM) containing 5% FBS (Microvascular EBM-2; Lonza, Basel, Switzerland) at 37°C in 5% CO2. Cells from passages 1-3 were used for all experiments (29).
Characterization of PEC by flow cytometry.
Neonatal PEC (passage 1 or 2) were detached by using TrypLE-Express solution (Invitrogen) and characterized by immunolabeling using the following antibodies: anti-mouse cell membrane markers: CD45 (BD Pharmingen), CD102-FITC (BD Pharmingen), and Flk-1/VEGFR2-PE (BD Pharmingen). Cells were incubated with specific antibodies for 45 min, after which cells were analyzed by using a LSRII flow cytometer (BD Pharmingen). Raw data were processed by FACSDiva 6.1 software (BD Pharmingen). The number of the counted events was 30,000. Gating for cell debris was applied as well as compensation factors for the Ab-tandem tests or autofluorescence. Results obtained for fixed cells were compared with preliminary data obtained on live cell tests, and they did not differ significantly.
Immunocytochemistry.
PEC treated with and without BAY were grown for 24 h on glass chamber slides (BD Biosciences, San Diego, CA), fixed with 90% cold ethanol for 15 min, and air-dried (10 min). Fixed cells were rehydrated with PBS for 30 min at room temperature and then treated with buffer containing 0.1% sodium citrate, 0.1% Triton-X 100, for 10 min. Cell samples were incubated with primary antibodies against PECAM (Beckton Dickinson, Franklin Lakes, NJ), p65 (Santa Cruz Biotechnology), active caspase-3 (Abcam), or PCNA (Abcam) overnight at 4°C. After being washed in PBS, the cells were incubated for 45 min at room temperature with goat-anti rat FITC- and anti-rabbit TRITC-labeled secondary antibodies (Invitrogen/Molecular Probes), washed three times, and incubated with Hoechst reagent chromatin staining (1 μg/ml) (Sigma-Aldrich). Fluorescent images were captured and quantified using a Leica DM5500B Upright Microscope and Photometrics CoolSNAP HQ2 CCD camera, using HC Plan Apo 25-mm objectives at ×40 magnification, and Methamorph Image analysis software (Molecular Devices, Sunnyvale, CA). Green signals were captured at a wavelength of 488 nm, red signals at 568 nm, and blue signals at 340 nm.
EMSA.
Nuclear extracts were obtained from the PEC using the NE-PER kit (Pierce, Rockford, IL), and protein concentration was determined by the Bradford method. A total of 10 mg of protein was used for binding reactions using γ−32P-labeled oligonucleotides containing the κB consensus sequence (Promega, Madison, WI) in a binding buffer containing 500 ng of salmon sperm DNA, 0.01 U of poly(dI-dC), and 0.5 mM DTT (EMD Chemicals) as described previously (2). Supershift experiments were conducted with the addition of 2 ml of anti-p65, p50, p52, cRel, and RelB antibodies (Santa Cruz Biotechnology) to the nuclear extracts 30 min before the addition of the radiolabeled probe. Nuclear extracts were incubated with the radiolabeled κB probe at room temperature for 30 min and electrophoresed on 6% polyacrylamide gels. To distinguish nonspecific binding of the nuclear proteins, competition reactions were performed by adding 100-fold excess nonradiolabeled κB probe (2).
Proliferation assays.
Proliferation of neonatal and adult PEC (P2) was determined by performing bromodeoxyuridine (BrdU) incorporation assays. Six thousand PEC were plated into each well of a 96-well plate and synchronized by incubation in starvation media (0.2% FBS) for 16 h, allowing for 70% confluence at the start of the experiment. The starvation media was then removed and replaced with EGM in addition to BrdU. The incorporation of BrdU was measured by ELISA at 2, 6, 12, and 24 h after serum stimulation with media per the manufacturer's protocol (Roche Diagnostics, Mannheim, Germany).
For the studies determining the effect of BAY on PEC proliferation, 6,000 PEC were plated in each well (96-well plate) and allowed to attach in EGM for 24 h. The cells were starved for 12 h before the beginning of the experiment (media with 0.2% serum). After starvation, the media was replaced with starvation media containing vehicle control (DMSO, 1:40,000) or BAY (2.5 μM), in the presence or absence of recombinant mouse VEGF-A (50 ng/ml) (R&D Systems), and the cells were counted at 48 h using a hemocytometer (31).
Apoptosis assays.
For comparisons between neonatal and adult PEC, 10,000 PEC were plated into each well of a 96-well plate and allowed to attach for 24 h in complete EGM. At time 0, EGM was replaced with starvation media and the amount of cleaved caspase-3 and -7 was measured using a GloMax 96-well plate luminometer and the Caspase Glo-3/7 reagent (Promega) at 2–24 h. For apoptosis assays performed on neonatal cells treated with vehicle or BAY, 10,000 PEC were plated in each well and allowed to attach for 16 h in EGM. After 16 h, EGM was replaced with starvation media containing either vehicle (DMSO, 1:20,000 or 1:40,000) or BAY (2.5 or 5.0 μM), and the amount of cleaved caspase-3 and -7 was measured using a GloMax 96-well plate luminometer and the Caspase Glo-3/7 reagent (Promega) at 2–24 h.
In vitro angiogenesis assay.
PEC were pretreated for 4 h in starvation media containing either vehicle (DMSO) or BAY (2.5 μM). Cells in starvation media containing either DMSO or BAY were plated into 24-well dishes coated with Reduced Growth Factor Basement Membrane Extract (Trevigen, Gaithersburg, MD) in the presence or absence of VEGF-A (50 ng/ml). Additional experiments were performed on PEC 40 h after transfection with siRNA against IKK-α or IKK-β. For all experiments, representative images of tube networks were obtained at 4 h, and the total tube length per ×4 field was quantified in a blinded fashion using Bioquant Image Analysis software (R&M Biometrics, Nashville, TN).
RNA interference.
PEC were transfected using either IKK-α or IKK-β On-Target Plus SMART pool siRNA or nontargeting siRNA as a control (Dharmacon; Thermo Fisher Scientific, Lafayette, CO) and Lipofectamine 2000 (Invitrogen) for 6 h. RNA was isolated at 36 h using the RNeasy kit (Qiagen, Valencia, CA) for qPCR, and whole cell protein lysate was extracted at 42 h for Western immunoblot. Additional siRNA-treated cells were used at 40 h posttransfection for in vitro angiogenesis assays as described above.
Quantitative RT-PCR.
Total RNA was isolated from PEC and whole mouse lung using the RNeasy kit (Qiagen). RNA (2 μg) was reverse-transcribed using Superscript III (Invitrogen), and qPCR was performed using TaqMan primers (Applied Biosystems, Carlsbad, CA) as described previously (2). Quantification of target gene expression was performed after normalizing to the expression of Hsp90ab1, identified by a PCR array (SABiosciences, Qiagen) as the most stable housekeeping gene for our experimental groups.
Western immunoblot.
Cytoplasmic and nuclear protein was extracted from frozen lung tissue and PEC using the NE-PER kit (Pierce). Whole cell lysates were obtained from PEC using a lysis buffer containing 10 mM Tris·HCl and 1% SDS, heated to 100°C. Protein lysates were quantified using the Bradford method and then subjected to SDS-PAGE. Membranes were incubated with primary antibodies to detect VEGFR2 (Santa Cruz Biotechnology), IKK-α, and IKK-β (Cell Signaling) and the appropriate horseradish peroxidase-conjugated secondary antibody, followed by detection with enhanced chemiluminescence reagents (GE Life Sciences, Piscataway, NJ) (2).
Chromatin immunoprecipitation.
For PEC, vehicle- (DMSO) and BAY-treated endothelial cells were formaldehyde cross-linked for 4 h, and the chromatin was sheared using an enzymatic method per the manufacturer's protocol (Active Motif, Carlsbad, CA). For tissue, neonatal (6 day) C57BL/6 mice were injected i.p. with either vehicle (DMSO in PBS + 20% Tween-80) or 10 mg/kg of BAY 11–7,082 (Calbiochem, La Jolla, CA). At 24 h, the animals were killed, and lungs were fixed with 4% formalin for 10 min. For both cells and tissue, chromatin was immunoprecipitated using an antibody against p65 or mouse IgG (Santa Cruz Biotechnology), and the ChIP-IT Enzymatic Express Kit (Active Motif). PCR for VEGFR2 was performed using the following primers: 5-ggaaacccaaacctggtatccagtg-3 (forward); and 5-aaagagagcgccggctacac-3 (reverse), based on the published sequence (51a), and yielding a 111-bp predicted product.
Statistics.
All data are presented as means ± SE. Statistical differences between two groups were determined by Student's t-test and between more than two groups by one-way ANOVA, followed by Neumann-Keuls Multiple-Comparison post hoc analysis. A P value of ≤ 0.05 was considered statistically significant.
RESULTS
Inhibiting NF-κB impairs pulmonary angiogenesis and arrests alveolar development.
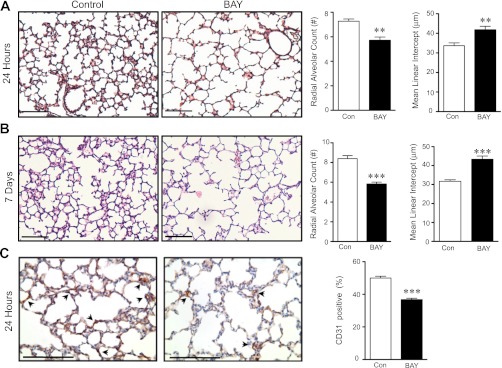
At term, the murine lung is in the saccular stage of development, similar to that of a premature infant, and begins alveolarization only postnatally, thus serving as a valuable model for investigating the mechanisms regulating alveolar development. To determine whether NF-κB activity is required for postnatal lung development, we treated neonatal mice with a selective and irreversible pharmacological inhibitor of IKK-α and -β, BAY 11–7082 (BAY) (54). We choose this strategy because the presence of five NF-κB subunits and multiple distinct mechanisms of activation suggest a functional redundancy that may be impervious to a strategy that targets only one component of the pathway. We first show that blocking NF-κB with BAY arrests alveolar development in neonatal mice (Fig. 1A), as indicated by decreased radial alveolar counts (RAC) (7.7 ± 0.24 vs. 6.2 ± 0.21) and increased mean linear intercepts (MLI) (33.7 ± 1.4 vs. 41.8 ± 1.8 μm) in BAY-treated animals compared with controls (Fig. 1A). In contrast, BAY treatment did not affect either the RAC (9.7 ± 0.17 vs. 10.3 ± 0.5, P = NS) or MLI (29.4 ± 1.7 vs. 28.3 ± 1.7, P = NS) in adult mice (BAY vs. vehicle treated).
Fig. 1.
Blocking NF-κB in the neonatal lung disrupts postnatal alveolar development and angiogenesis. A: representative images of hematoxylin and eosin (H&E)-stained lung sections obtained from neonatal mice, 24 h after administration of vehicle or the NF-κB inhibitor, BAY, with morphometric analysis to determine the radial alveolar count (**P = 0.003) and mean linear intercept (**P = 0.008). Data are expressed as means ± SE. B: representative images of H&E-stained lung sections obtained from neonatal mice, 7 days after administration of vehicle or the NF-κB inhibitor, BAY, with morphometric analysis to determine the radial alveolar count (***P = 0.0004) and mean linear intercept (***P = 0.0008). Data are expressed as means ± SE. C: representative images of lung sections, 24 h after administration of vehicle or BAY, immunostained to detect the endothelial-specific marker, CD31 (brown). Quantification of vascular density using a point-counting method expressed as the percentage of CD-31-positive points divided by total parenchymal points, with data expressed as means ± SE and ***P < 0.0001 (n = 5–8 mice per group). Scale bar for all images = 100 μm.
This developmental difference was further highlighted by experiments performed to evaluate the long-term effect of BAY on alveolarization. Administration of a single injection of BAY to the neonatal mice resulted in a 60% mortality by 7 days. Examination of the lungs of surviving neonates at 7 days demonstrated a persistent and profound arrest in alveolarization (Fig. 1B), suggesting that inhibition of NF-κB during this critical window in alveolar development has long-standing consequences on lung growth. In contrast, there was no associated mortality observed in adult animals treated with the same strategy. Furthermore, even at this later time point, there was an absence of differences in either RAC (9.6 ± 0.25 vs. 9.4 ± 0.14, P = NS) or MLI (27 ± 0.32 vs. 28.8 ± 1.2, P = NS) in BAY vs. vehicle-treated adult mice.
Development of the alveolar capillary network by angiogenesis is essential for the process of alveolarization, and disruption of angiogenesis causes enlargement of the airspaces, similar to that seen in infants with BPD (40, 70). Therefore, we next evaluated whether BAY treatment impaired pulmonary capillary development in the neonatal mouse lung. We immunostained lung sections from control and BAY-treated mice with an antibody against CD31 and found that inhibiting NF-κB with BAY significantly reduced pulmonary capillary density by 24 h, even when accounting for the overall reduction in lung tissue in this group (Fig. 1C).
NF-κB is constitutively active in the developing pulmonary vascular endothelium.
NF-κB subunits are ubiquitously expressed (3, 30, 59) but typically remain inactive in the cytoplasm and translocate to the nucleus only after stimulation. Although BAY treatment could potentially block NF-κB activity in multiple cell types within the lung, we hypothesized that effects on the endothelium would be critically important for alveolarization. The focus on endothelial cells was based on the observations that 1) BAY treatment significantly reduced pulmonary capillary density and 2) loss of IKK-β in EC has been shown to impair EC survival, migration, and neovascularization after ischemia (6).
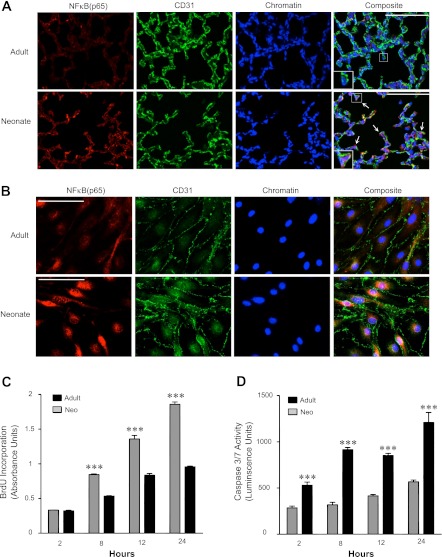
To test whether NF-κB was constitutively active in the neonatal pulmonary endothelium, we first immunostained frozen sections of lung tissue obtained from the neonatal and adult mice under control conditions to detect the nuclear presence of the NF-κB subunit, p65, and the endothelial-specific marker, CD31. Examination by confocal microscopy demonstrated that, in the adult lung, p65 was expressed diffusely throughout the lung, but its localization was primarily cytoplasmic (Fig. 2A, top). Specific examination of the EC demonstrated that, under control conditions, p65 was rarely found in the nucleus (Fig. 2A, top, inset), suggesting minimal constitutive NF-κB activity in the mature lung. In contrast, numerous cells within the neonatal lung contained p65 in the nucleus, including many EC (Fig. 2A, bottom, inset).
Fig. 2.
NF-κB is constitutively active in the developing pulmonary vascular endothelium. A: representative confocal immunofluorescent images from frozen sections of adult and neonatal lung tissue immunostained to detect the NF-κB subunit, p65 (red), and CD31 (green). The presence of nuclear (active NF-κB) is visualized by a pink signal. In the composite panels a single endothelial cell (EC) is magnified and shown in the insets. Arrows indicate examples of CD31-positive cells with p65 in the nucleus. Scale bar = 100 μm. B: representative confocal fluorescent images of adult (top) and neonatal (bottom) pulmonary endothelial cells (PEC) demonstrating localization of the NF-κB subunit, p65 (red) in CD31-labeled (green) ECs. Few p65-positive nuclei were observed in adult PEC, compared with multiple positive nuclei in the neonatal PEC. Scale bar = 50 μm. C: in vitro bromodeoxyuridine (BrdU) incorporation assays performed in adult (solid bars) and neonatal (shaded bars) PEC, 2–24 h after stimulation with endothelial growth media (EGM) containing 5% FBS and EC growth factors (n = 8, with ***P < 0.0001 vs. adult values at that same time point). D: in vitro luminescent caspase-3/7 activity assays performed in neonatal and adult PEC, 2–24 h after serum withdrawal (n = 6, with ***P < 0.001 vs. adult PEC at that same time point).
We then confirmed this difference in the amount of NF-κB active in neonatal and adult pulmonary endothelium by isolating primary PEC from the lungs of neonatal and adult mice. The PEC were first characterized by flow cytometry and found to be exclusively CD45- and >95% CD102+ (data not shown). Furthermore, by immunostaining, >95% of the cells stained positively for CD31. We then immunostained the adult PEC for p65 and demonstrated primarily cytoplasmic staining and little nuclear staining (Fig. 2B, top), consistent with previous reports of minimal NF-κB activity in the pulmonary endothelium under unstimulated conditions (77). In contrast, the majority of neonatal PEC displayed prominent nuclear p65 immunoreactivity (Fig. 2B, bottom), with a greater than threefold increase in p65-positive nuclei in the neonatal vs. adult PEC (54 ± 5.4 vs. 16.3 ± 1.7, P = 0.0002).
NF-κB is a key regulator of cell survival and proliferation. Increased constitutive activity in cancer cells has been associated with an antiapoptotic and proproliferative phenotype (10, 45, 55). Therefore, we next explored whether basal survival and proliferation differed in the adult compared with neonatal PEC. By assessing BrdU incorporation in response to serum stimulation, the neonatal PEC were found to proliferate faster than the adult PEC (Fig. 2C). In addition, the neonatal PEC were also more resistant than the adult PEC to apoptosis in response to serum deprivation (Fig. 2D).
BAY 11–7082 effectively decreases NF-κB activity in vitro and in vivo.
We then performed experiments to elucidate how blocking NF-κB activity in the neonatal lung impairs alveolarization. We first confirmed that BAY treatment effectively blocks constitutive NF-κB activity in the neonatal lung and PEC. We immunostained lung sections from vehicle- and BAY-treated mice at 24 h and found by confocal microscopy that BAY markedly reduced the amount of p65 nuclear signal (Fig. 3A). Similar results were obtained in vitro in the neonatal PEC, where increasing doses of BAY resulted in qualitative decrease in nuclear staining along with a concomitant increase in p65 cytoplasmic staining (Fig. 3B).
Fig. 3.
BAY treatment effectively decreases active NF-κB in vitro and in vivo. A: representative composite immunofluorescent images from frozen section of lungs obtained from vehicle- and BAY-treated neonatal mice at 24 h, to detect p65 (red), CD31 (green), or chromatin (blue). Scale bar = 100 μm. B: representative composite confocal fluorescent images demonstrating p65 localization (red) in CD31-labeled (green) neonatal PEC 8 h after exposure to either DMSO or BAY (2.5 or 5 μM). Scale bar = 100 μm. C: EMSA using radiolabeled oligonucleotides containing the NF-κB consensus sequence and nuclear extracts obtained from neonatal PEC 4 h after incubation with either vehicle control (DMSO) or BAY (2.5 or 5 μM). D: EMSA with supershift analysis using antibodies against the 5 NF-κB family members and nuclear extracts from neonatal PEC under control conditions, incubated with radiolabeled κB oligo nucleotides (lane 1) Specificity of the band was confirmed by the disappearance of the band with the addition of 100-fold excess of cold oligonucleotide (lane 2). Supershift analysis of the NF-κB complex present in control PEC was then performed (lanes 3–7), with the shift produced by the addition of p65 antibodies (lane 3) labeled as S1, and that produced by p50 antibodies (lane 4) labeled S2. Lanes 5–7 contained supershift reactions using antibodies against p52, cRel, and RelB, respectively.
By EMSA, we identified a single NF-κB complex that was active in the neonatal PEC under control conditions (Fig. 3C, lanes 1–3) and found that this complex was decreased in a dose-dependent manner by incubation with BAY (Fig. 3C, lanes 4–8). Interestingly, the neonatal PEC demonstrated an exquisite sensitivity to BAY. Doses of BAY below those required to block NF-κB in other cells (41, 48) were extremely effective in the neonatal PEC, with 2.5 μM decreasing binding by ∼50% and 5 μM decreasing binding by more than 70%. We then performed supershift experiments using antibodies against each of the five known NF-κB family subunits. The addition of antibodies against either p65 or p50 resulted in an upward shift of the complex (Fig. 3D, lanes 3 and 4), whereas antibodies against p52, cRel, and RelB had no effect on complex binding (Fig. 3D, lanes 5–7). This indicates that the NF-κB dimer constitutively active in the neonatal PEC is a heterodimer comprised of p65 and p50.
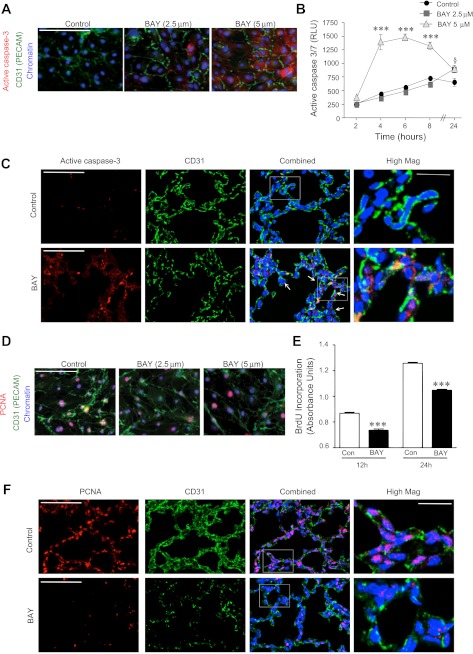
Blocking NF-κB increases apoptosis and decreases proliferation of neonatal PEC.
The prominent nuclear presence of NF-κB in the developing endothelium and the high sensitivity to BAY suggested an essential role for constitutive NF-κB in immature PEC homeostasis. Thus we next performed functional assays on the neonatal PEC in the presence and absence of NF-κB blockade. We first evaluated the effect of blocking NF-κB on PEC survival by immunofluorescent staining and found that BAY treatment induced a qualitative, dose-dependent increase in active caspase-3 immunostaining (Fig. 4A). These results were then confirmed using a quantitative assay to measure caspase-3 and -7 activity. We found that treatment with 5 μM of BAY rapidly induced PEC apoptosis, beginning at 4 h and continuing through 8 h (Fig. 4B), after which time the signal decreased due to death of the cells. However, treatment with a lower dose of BAY (2.5 μM) increased PEC apoptosis only slightly at 24 h. Immunostaining lung tissue from vehicle- and BAY-treated neonatal mice at 8 h to detect active caspase-3 followed by confocal microscopy demonstrated a small amount of basal apoptosis in the neonatal murine lung under control conditions; however, very few of these cells were CD31 positive. BAY treatment markedly increased active caspase-3 immunoreactivity in the lung, including numerous cells that were active caspase-3-and CD31-double positive (Fig. 4C, arrows).
Fig. 4.
Blocking NF-κB increases apoptosis and decreases proliferation in neonatal PEC in vitro and in vivo. A: representative composite fluorescent images of active caspase-3 staining (red) in CD31-labeled (green) neonatal PEC, 8 h after exposure to vehicle (DMSO) or BAY (2.5 or 5 μM). Scale bar = 100 μm. B: in vitro luminescent apoptosis assay to quantify active caspase-3/7 in relative luminescent units (RLU), 2 to 24 h after incubation with vehicle control (DMSO) or BAY (2.5 or 5 μM). Data are means ± SE with n = 4–5 per group. ***P < 0.001 for 5 μM vs. control at 4, 6, and 8 h and vs. 5 μM at 2 h, and §P < 0.05 for 2.5 μM at 24 h vs. 2 h. C: representative confocal fluorescent images from formalin-fixed lung tissue obtained from vehicle- and BAY-treated neonates after 8 h and immunostained to detect active caspase-3 (red), and CD31 (green). Arrows indicate examples of CD31-positive cells with active caspase-3 in the cytoplasm. Scale bar = 100 μm. Insets: selected fields at higher magnification, with scale bar = 25 μm. Arrows identify cells that are both active caspase-3 and CD31 positive. D: representative composite fluorescent images of PEC immunostained to detect PCNA (red) and CD31 (green), 8 h after exposure to vehicle (DMSO) or BAY (2.5 or 5 μM). Scale bar = 100 μm. E: BrdU incorporation assays to measure the proliferation of control and BAY (2.5 μM)-treated PEC after stimulation with EGM containing 5% FBS at 12 and 24 h. Data are means ± SE with n = 8 per group. ***P < 0.001 vs. control at same time point. F: representative confocal fluorescent images from formalin-fixed lung tissue obtained from vehicle- and BAY-treated neonates after 8 h and immunostained to detect PCNA (red) and CD31 (green). Scale bar = 100 μm. Insets: selected fields at higher magnification, with scale bar = 25 μm.
We also determined the effect of NF-κB inhibition on PEC proliferation. The majority of immature PEC nuclei were positive for PCNA under control conditions, and the number of positive nuclei decreased with increasing concentrations of BAY (Fig. 4D). We confirmed and quantified this effect on proliferation by performing a BrdU incorporation assay. To limit the confounding effects of cell death, these experiments were performed using the 2.5 μM dose of BAY. Treatment with this lower dose of BAY attenuated the proliferative response induced by serum stimulation at 12 and 24 h (Fig. 4E). A similar role for NF-κB in modulating proliferation in the whole lung was demonstrated by immunostaining lung sections from vehicle- and BAY-treated mice at 8 h to detect PCNA. Under control conditions, there was a large number of PCNA-positive cells evident by confocal microscopy (Fig. 4F, top). Blocking constitutive NF-κB activity with BAY reduced the amount of proliferating cells in the neonatal lung, including a qualitative decrease in the number of PCNA-positive EC (Fig. 4F, bottom). Taken together, these data demonstrate that constitutive NF-κB activity in the neonatal PEC is necessary for both survival and proliferation.
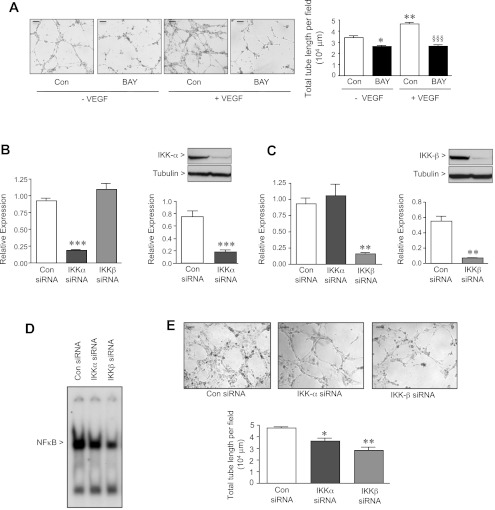
Blocking NF-κB impairs angiogenesis in vitro.
To characterize the role of NF-κB in modulating angiogenesis in the immature PEC, we next pretreated cells with either vehicle or BAY before performing in vitro angiogenesis assays. Control PEC rapidly formed thin capillary tubes on reduced growth factor basement membrane extract, even in the absence of VEGF (Fig. 5A). In contrast, 4-h pretreatment with BAY markedly attenuated PEC tube and network formation. Furthermore, although the addition of VEGF significantly enhanced tube formation in control cells, it had no effect in the BAY-treated PEC, demonstrating that blocking NF-κB disrupts angiogenesis in vitro and that this effect cannot be rescued by VEGF.
Fig. 5.
Blocking NF-κB in neonatal PEC impairs angiogenesis in vitro. A: in vitro tube formation assays performed with vehicle control (DMSO)- and BAY (2.5 μM)-treated PEC without and with vascular endothelial growth factor (VEGF) (50 ng/ml). PEC suspensions were plated on reduced growth factor matrix, and, after 4 h of incubation, representative images were obtained using a Leica DMI3000B Inverted Microscope, at ×4 magnification, and Spot imaging software, and the extent of capillary tube formation was evaluated by measuring the total tube length per field. Data are expressed as means ± SE with n = 3–5 per group. *P < 0.05 and **P < 0.001 vs. control-VEGF, and §§§P < 0.001 vs. control + VEGF. Scale bar = 100 μm for all images. qRT-PCR and Western immunoblot to detect either IKK-α (B) or IKK-β (C) in PEC 36 h after transfection with either control, IKK-α, or IKK-β siRNA. Data are expressed as means ± SE with n = 3 per group. **P < 0.01 and ***P < 0.001 vs. control siRNA. D: representative EMSA using radiolabeled oligonucleotides containing the NF-κB consensus sequence and nuclear extracts obtained from neonatal PEC 36 h after siRNA transfection with nontargeting control, IKK-α, or IKK-β siRNA. E: in vitro angiogenesis assays using PEC 40 h after siRNA transfection in the presence of VEGF (50 ng/ml). Representative images were obtained using a Leica DMI3000B Inverted Microscope, at ×4 magnification, and Spot imaging software. Total tube length per field was quantified after 4 h of incubation, with data expressed as means ± SE with n = 3 per group. *P < 0.05 and **P < 0.01 vs. control siRNA. Scale bar = 100 μm for all images.
Although increased NF-κB activity has been linked to the pathological angiogenesis observed in cancer, the distinct roles that IKK-α and -β play in modulating this effect are not clear. IKK-α is increased in the vasculature of lung adenocarcinomas, and overexpression of IKK-α enhances in vitro angiogenesis in human umbilical vein EC. However, overexpression of IKK-β does not induce this effect (22). This is in contrast to a very recent report demonstrating that EC-specific loss of IKK-β impairs neovascularization after ischemia (6).
Therefore, to evaluate the relative proangiogenic contribution of IKK-α vs. IKK-β in the immature PEC, we disrupted IKK signaling in a subunit-specific manner using RNA interference. Transfection of the PEC with siRNA targeting IKK-α markedly decreased IKK-α gene and protein expression without affecting the levels of IKK-β (Fig. 5B). Converse results were obtained after transfection with siRNA targeting IKK-β (Fig. 5C). Despite marked reductions in gene and protein expression, siRNA against IKK-α only mildly decreased NF-κB complex binding in the PEC, whereas siRNA against IKK-β decreased NF-κB binding to a greater degree (Fig. 5D). However, even modest decreases in NF-κB binding produced by either IKK-α or IKK-β siRNA impaired in vitro angiogenesis (Fig. 5E). This observation provides evidence that both kinases are required for NF-κB to optimally mediate angiogenesis in the neonatal PEC.
NF-κB regulates the expression of VEGFR2 in the developing lung.
To identify the mechanism by which NF-κB promotes angiogenesis in the PEC, we chose to focus on the capacity of NF-κB to regulate the VEGF pathway, as VEGF-mediated signaling is essential for postnatal lung angiogenesis (40). The rationale for this focus includes our observation that exogenous VEGF was unable to rescue the PEC from the effects of BAY. Furthermore, the murine VEGFR2 promoter contains a putative κB binding site, and the induction of VEGFR2 expression by hypoxia-induced mitogenic factor is thought to be NF-κB dependent (60, 71). Thus we evaluated the gene and protein expression of VEGFR2 in the neonatal PEC and found that BAY induced a dose-dependent decrease in VEGFR2 mRNA (Fig. 6A) and protein (Fig. 6B), demonstrating that inhibiting NF-κB downregulates VEGFR2 expression. In addition, in vivo treatment of neonatal mice with BAY significantly reduced both VEGFR2 mRNA (Fig. 6C) and protein (Fig. 6D) in the whole lung. Furthermore, by using chromatin immunoprecipitation followed by PCR using primers flanking the κB binding site within the mouse VEGFR2 promoter, we found that p65 was bound to the VEGFR2 promoter in the neonatal PEC under control conditions (Fig. 6E, lane 2). Using the same strategy, we demonstrated that BAY completely abolished occupancy of p65 from the VEGF promoter (Fig. 6E, lane 5). Similar results were obtained by performing chromatin immunoprecipitation in whole lung tissue, where p65 was also found to bind the VEGFR2 promoter in vehicle-treated mice and a reduction of p65 binding was demonstrated after 24 h of BAY treatment. Finally, we performed immunostaining to detect VEGFR2 in frozen lung tissue obtained from neonatal vehicle- and BAY-treated mice at 24 h. Confocal images under high magnification were obtained to specifically evaluate the colocalization of VEGFR2 with the EC-specific marker, CD31. In neonatal control mice, there were a few isolated cells expressing VEGFR2 in the absence of CD31, consistent with reports of epithelial cells also expressing VEGFR2 (1). However, the vast majority of VEGFR2 was expressed by EC (as evidenced by the predominantly yellow/orange signal on the composite image produced by the colocalization of VEGFR2 with CD31), including by many EC located at the tips of the secondary crests (Fig. 6G, top, arrow). BAY treatment markedly reduced VEGFR2 immunoreactivity, resulting in minimal colocalization of the two membrane proteins, including an absence of VEGFR2 expressed by the EC located at the septal tips (Fig. 6G, bottom, arrows). Taken together, these data demonstrate that NF-κB directly regulates VEGFR2 expression in the neonatal pulmonary endothelium.
Fig. 6.
NF-κB regulates the expression of VEGF receptor 2 (VEGFR2) in the developing lung. qRT-PCR (A) and Western immunoblot (B) performed on neonatal PEC to detect VEGFR2 mRNA and protein from PEC treated with vehicle or BAY (2.5 or 5 μM) for 16 h with data expressed as means ± SE with n = 3 per group. **P < 0.01 and ***P < 0.001 vs. control. qRT-PCR (C) performed on whole lung, 8 h after either vehicle or BAY to detect VEGFR2 mRNA expression, and Western immunoblot (D) of extracts from whole lung at 16 h to determine VEGFR2 protein (n = 4–5 mice per group). *P < 0.01 vs. control. E: representative chromatin immunoprecipitation on neonatal PEC treated for 4 h with vehicle (DMSO) or BAY (5 μM), using either anti-p65 antibody or isotype control IgG immunoprecipitation followed by PCR using primers to detect the expected 111-bp VEGFR2 gene product. F: representative chromatin immunoprecipitation on whole lung tissue obtained from vehicle-or BAY-treated neonatal mice after 24 h, using either anti-p65 antibody or isotype control IgG immunoprecipitation followed by PCR using primers to detect the expected 111-bp VEGFR2 gene product. G: representative confocal immunofluorescent images taken at ×60-oil magnification of frozen sections obtained from vehicle- and BAY-treated neonatal mice at 24 h, to detect VEGFR2 (red), CD31 (green), or chromatin (blue), with colocalization of the 2 membrane proteins visualized as yellow/orange signal. Arrows indicate examples of CD-31-positive EC located at the tips of septal crests. Scale bar = 50 μm.
DISCUSSION
In summary, the present report identifies a novel and developmentally regulated role for the transcription factor NF-κB, classically considered a proinflammatory transcription factor, in the neonatal lung. We demonstrate that in vivo blockade of NF-κB produces alveolar simplification and loss of distal pulmonary vessels in neonatal mice comparable to that observed in premature infants with BPD. Under basal conditions, there is a high amount of constitutive NF-κB activity present in EC isolated from the developing lung, and this basal activity is essential for neonatal PEC survival, proliferation, and in vitro angiogenesis. Furthermore, this report is the first to demonstrate that NF-κB regulates VEGFR2 in the developing lung, a key mediator of EC homeostasis and known regulator of angiogenesis.
Our observation that high levels of basal NF-κB activity are present in immature PEC is particularly interesting given that constitutive NF-κB activity is normally restricted to hematopoietic cells (64). In mature PEC, as is the case in other cell types, basal NF-κB activity is minimal, induced only after stimulation with cytokines, bacterial products, and reactive oxygen species (57, 58). That constitutive NF-κB plays a critical, yet a previously undescribed role in postnatal vascular development is not surprising given that p65 deletion in mice results in early embryonic lethality (8). In addition, although it is known that widespread gene expression of NF-κB subunits occurs early in embryonic development, the kinetics of NF-κB activation during organogenesis are not well characterized. The mechanism underlying the higher constitutive activity in immature vs. mature PEC remains unclear but may involve autocrine secretion of growth factors able to persistently activate NF-κB in the neonatal cells or posttranslational modifications allowing for more persistent nuclear retention of p65.
We go on to demonstrate that constitutive NF-κB in the developing pulmonary endothelium is required for EC proliferation and survival and promotes angiogenesis in vitro and in vivo. NF-κB is a key regulator of cell proliferation and survival. NF-κB increases the expression of numerous antiapoptotic genes (13, 53), and constitutive NF-κB activity is associated with the antiapoptotic, proproliferative phenotype observed in neoplastic cells (45, 55). Furthermore, inhibition of NF-κB restores the sensitivity to apoptosis, suppresses proliferation of cancer cells (45, 55), and has therefore been proposed as a possible adjuvant to traditional chemotherapeutic strategies (16, 50). Taken together with our data, this suggests that constitutive activity of NF-κB may confer a developmentally specific, proproliferative, antiapoptotic phenotype to the neonatal PEC that is necessary for angiogenesis.
In this study, we focused on constitutive NF-κB activity in the pulmonary endothelium as a key component of the mechanism accounting for alveolar simplification. However, it is possible that NF-κB activity in other cell types within the lung also contributes to alveolarization. Expression of the p65 subunit has been shown to be increased in the neonatal lung at postnatal day 2 and decreased in the adult lung; however, the cell-specific pattern of expression has not been characterized (42). In the same study, Londhe et al. (42) demonstrated that targeted overexpression of p65 in the alveolar type II cells increases alveolar type II cell number by decreasing apoptosis. However, that study did not entail morphometric analysis of the lung, thereby precluding definitive conclusions relative to an effect on lung maturation. Future studies involving the creation of murine models with tissue-specific and conditional deletions of the various NF-κB pathway components will be necessary to clarify the cell-specific roles of NF-κB activity in the developing lung.
This physiological, proangiogenic role for NF-κB during development stands in contradistinction to its pathological role described in the angiogenesis observed in inflammatory diseases and cancer. A number of NF-κB-regulated inflammatory cytokines are potent angiogenic stimulators (43, 56). Macrophages recruited to areas of injury or associated with tumors also possess angiogenic activity due to their ability to secrete many of these same cytokines in an NF-κB-dependent manner (49, 66). Increased NF-κB activity has been documented in the vasculature of colorectal and lung carcinoma (22, 62), and strategies to inhibit NF-κB are effective in decreasing tumor angiogenesis. Furthermore, the antiangiogenic effects of the anti-inflammatory compound, thalidomide, have been attributed to its ability to inhibit NF-κB (36). These data begin to delineate the mechanism whereby chronic inflammation induces or exacerbates cancer (28). However, evidence demonstrating that constitutive NF-κB promotes physiological angiogenesis in the absence of inflammation has not been previously described.
Evidence that NF-κB is critical for lung angiogenesis and development is of particular significance, given that, exclusive of embryonic development, NF-κB plays primarily a pathological role in the lung (75). NF-κB has been implicated in the pathogenesis of inflammatory lung diseases including asthma and the acute respiratory distress syndrome (12, 20, 46, 75). However, how NF-κB modulates inflammation in the developing lung and in diseases of disrupted alveolarization such as BPD is not clear. Although much of the early scientific literature highlights the proinflammatory function for NF-κB, recent experimental evidence has shown that the NF-κB can also serve to suppress inflammation (26, 38, 39). Furthermore, there is some evidence to suggest that this anti-inflammatory role may be particularly prominent in the neonate. For example, in contrast to studies demonstrating that NF-κB blockade improves endotoxin induced lung injury in adult mice (18), we have shown that inhibiting NF-κB in neonatal mice exposed to LPS paradoxically increases lung inflammation (2). Similarly, NF-κB protects the neonatal lung against hyperoxic lung injury, as mice lacking the NF-κB subunit p50 are more sensitive to hyperoxic lung injury (76). This suggests the existence of distinct pathways that allow NF-κB to play either protective or pathological roles. The extent to which these pathways are developmentally regulated or whether the differential downstream gene regulation involves the activation of unique combinations of NF-κB dimers or epigenetic mechanisms remain unknown.
In contradistinction to the inducible activation of NF-κB that occurs in response to inflammation, we demonstrate an essential role for constitutive NF-κB signaling in promoting angiogenesis in the developing lung. Enhancement of NF-κB is also associated with the pathological angiogenesis observed in carcinoma of the mature lung (22). Considered in concert, these reports support the evolving paradigm that developmentally regulated pathways are often recapitulated in pathological states such as neoplasia (68). Furthermore, it is possible that these same pathways could be reinvoked in an attempt to augment angiogenesis in the setting of adult diseases characterized by airspace loss and rarefaction of small vessels, such as emphysema (72).
The present paradigm may possess significant clinical implications. If, as our data suggest, NF-κB plays an essential role in postnatal lung development, then therapies that decrease NF-κB activation may compromise alveolar development. Glucocorticoids, potent inhibitors of NF-κB activation (7), accelerate the development of the surfactant system in the saccular lung but inhibit secondary septation during later lung development (44, 61). Therefore, suppression of constitutive NF-κB activity may be one mechanism whereby glucocorticoids compromise alveolarization at a specific time point during development. In addition, pharmacological inhibitors of NF-κB have been developed and are currently being studied as possible adjuvants to standard chemotherapeutics (16). Given that alveolarization continues into early childhood (33, 47), our data suggest that use of such strategies in young patients could be detrimental to long-term lung function.
Taken together, our data have palpable clinical and biological relevance. This study is the first to identify NF-κB as an essential transcriptional regulator of secondary septation and angiogenesis in the developing lung. We speculate that disruption of NF-κB signaling may contribute to the pathogenesis of BPD. Moreover, NF-κB may represent a previously unaddressed therapeutic target as strategies to enhance NF-κB may be effective in promoting lung growth and regeneration in pulmonary diseases marked by impaired angiogenesis.
GRANTS
This work was supported by NIH grants 1P30HL101315-01 (D. Cornfield and C. Alvira), R01 HL60784 (D. Cornfield), and R01 HL70628 (D. Cornfield), the American Heart Association FTF Award 0875001N (C. Alvira), and postdoctoral fellowships from the Sigrid Juselius Foundation, Instrumentarium Foundation, Finnish Foundation for Cardiovascular Research, Finnish Cultural Foundation, Finnish Foundation for Pediatric Research, and the Academy of Finland (T.-P. Alastalo).
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the authors.
AUTHOR CONTRIBUTIONS
Author contributions: C.I., T.-P.A., Y.H., C.C., E.S.A., S.-C.L., and C.M.A. performed experiments; C.I., T.-P.A., Y.H., C.C., E.S.A., S.-C.L., and C.M.A. analyzed data; C.I., T.-P.A., Y.H., D.N.C., and C.M.A. interpreted results of experiments; C.I., T.-P.A., Y.H., D.N.C., and C.M.A. edited and revised manuscript; C.I., T.-P.A., Y.H., C.C., E.S.A., S.-C.L., D.N.C., and C.M.A. approved final version of manuscript; C.M.A. conception and design of research; C.M.A. prepared figures; C.M.A. drafted manuscript.
REFERENCES
- 1. Ahlbrecht K, Schmitz J, Seay U, Schwarz C, Mittnacht-Kraus R, Gaumann A, Haberberger RV, Herold S, Breier G, Grimminger F, Seeger W, Voswinckel R. Spatiotemporal expression of flk-1 in pulmonary epithelial cells during lung development. Am J Respir Cell Mol Biol 39: 163–170, 2008 [DOI] [PubMed] [Google Scholar]
- 2. Alvira CM, Abate A, Yang G, Dennery PA, Rabinovitch M. Nuclear factor-kappaB activation in neonatal mouse lung protects against lipopolysaccharide-induced inflammation. Am J Respir Crit Care Med 175: 805–815, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Anrather J, Csizmadia V, Brostjan C, Soares MP, Bach FH, Winkler H. Inhibition of bovine endothelial cell activation in vitro by regulated expression of a transdominant inhibitor of NF-kappa B. J Clin Invest 99: 763–772, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Aoki T, Kataoka H, Ishibashi R, Nozaki K, Morishita R, Hashimoto N. Reduced collagen biosynthesis is the hallmark of cerebral aneurysm: contribution of interleukin-1beta and nuclear factor-kappaB. Arterioscler Thromb Vasc Biol 29: 1080–1086, 2009 [DOI] [PubMed] [Google Scholar]
- 5. Aoki T, Kataoka H, Shimamura M, Nakagami H, Wakayama K, Moriwaki T, Ishibashi R, Nozaki K, Morishita R, Hashimoto N. NF-kappaB is a key mediator of cerebral aneurysm formation. Circulation 116: 2830–2840, 2007 [DOI] [PubMed] [Google Scholar]
- 6. Ashida N, Senbanerjee S, Kodama S, Foo SY, Coggins M, Spencer JA, Zamiri P, Shen D, Li L, Sciuto T, Dvorak A, Gerszten RE, Lin CP, Karin M, Rosenzweig A. IKKbeta regulates essential functions of the vascular endothelium through kinase-dependent and -independent pathways. Nat Commun 2: 318, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Auphan N, DiDonato JA, Rosette C, Helmberg A, Karin M. Immunosuppression by glucocorticoids: inhibition of NF-kappa B activity through induction of I kappa B synthesis. Science 270: 286–290, 1995 [DOI] [PubMed] [Google Scholar]
- 8. Beg AA, Sha WC, Bronson RT, Ghosh S, Baltimore D. Embryonic lethality and liver degeneration in mice lacking the RelA component of NF-kappa B. Nature 376: 167–170, 1995 [DOI] [PubMed] [Google Scholar]
- 9. Bhatt AJ, Pryhuber GS, Huyck H, Watkins RH, Metlay LA, Maniscalco WM. Disrupted pulmonary vasculature and decreased vascular endothelial growth factor, Flt-1, and TIE-2 in human infants dying with bronchopulmonary dysplasia. Am J Respir Crit Care Med 164: 1971–1980, 2001 [DOI] [PubMed] [Google Scholar]
- 10. Biswas DK, Shi Q, Baily S, Strickland I, Ghosh S, Pardee AB, Iglehart JD. NF-kappa B activation in human breast cancer specimens and its role in cell proliferation and apoptosis. Proc Natl Acad Sci USA 101: 10137–10142, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Blackwell TS, Blackwell TR, Holden EP, Christman BW, Christman JW. In vivo antioxidant treatment suppresses nuclear factor-kappa B activation and neutrophilic lung inflammation. J Immunol 157: 1630–1637, 1996 [PubMed] [Google Scholar]
- 12. Blackwell TS, Yull FE, Chen CL, Venkatakrishnan A, Blackwell TR, Hicks DJ, Lancaster LH, Christman JW, Kerr LD. Use of genetically altered mice to investigate the role of nuclear factor-kappa B activation and cytokine gene expression in sepsis-induced ARDS. Chest 116: 73S–74S, 1999 [DOI] [PubMed] [Google Scholar]
- 13. Brouard S, Berberat PO, Tobiasch E, Seldon MP, Bach FH, Soares MP. Heme oxygenase-1-derived carbon monoxide requires the activation of transcription factor NF-kappa B to protect endothelial cells from tumor necrosis factor-alpha-mediated apoptosis. J Biol Chem 277: 17950–17961, 2002 [DOI] [PubMed] [Google Scholar]
- 14. Brouillard F, Bouthier M, Leclerc T, Clement A, Baudouin-Legros M, Edelman A. NF-kappa B mediates up-regulation of CFTR gene expression in Calu-3 cells by interleukin-1beta. J Biol Chem 276: 9486–9491, 2001 [DOI] [PubMed] [Google Scholar]
- 15. Burri PH. Structural aspects of postnatal lung development— alveolar formation and growth. Biol Neonate 89: 313–322, 2006 [DOI] [PubMed] [Google Scholar]
- 16. Calzado MA, Bacher S, Schmitz ML. NF-kappaB inhibitors for the treatment of inflammatory diseases and cancer. Curr Med Chem 14: 367–376, 2007 [DOI] [PubMed] [Google Scholar]
- 17. Carpenter TC, Stenmark KR. Predisposition of infants with chronic lung disease to respiratory syncytial virus-induced respiratory failure: a vascular hypothesis. Pediatr Infect Dis J 23: S33–S40, 2004 [DOI] [PubMed] [Google Scholar]
- 18. Cheng DS, Han W, Chen SM, Sherrill TP, Chont M, Park GY, Sheller JR, Polosukhin VV, Christman JW, Yull FE, Blackwell TS. Airway epithelium controls lung inflammation and injury through the NF-kappa B pathway. J Immunol 178: 6504–6513, 2007 [DOI] [PubMed] [Google Scholar]
- 19. Cooney TP, Thurlbeck WM. The radial alveolar count method of Emery and Mithal: a reappraisal 1–postnatal lung growth. Thorax 37: 572–579, 1982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Das J, Chen CH, Yang L, Cohn L, Ray P, Ray A. A critical role for NF-kappa B in GATA3 expression and TH2 differentiation in allergic airway inflammation. Nat Immunol 2: 45–50, 2001 [DOI] [PubMed] [Google Scholar]
- 21. De Martin R, Hoeth M, Hofer-Warbinek R, Schmid JA. The transcription factor NF-kappa B and the regulation of vascular cell function. Arterioscler Thromb Vasc Biol 20: E83–E88, 2000 [DOI] [PubMed] [Google Scholar]
- 22. DeBusk LM, Massion PP, Lin PC. IkappaB kinase-alpha regulates endothelial cell motility and tumor angiogenesis. Cancer Res 68: 10223–10228, 2008 [DOI] [PubMed] [Google Scholar]
- 23. Doi TS, Takahashi T, Taguchi O, Azuma T, Obata Y. NF-kappa B RelA-deficient lymphocytes: normal development of T cells and B cells, impaired production of IgA and IgG1 and reduced proliferative responses. J Exp Med 185: 953–961, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Everhart MB, Han W, Sherrill TP, Arutiunov M, Polosukhin VV, Burke JR, Sadikot RT, Christman JW, Yull FE, Blackwell TS. Duration and intensity of NF-kappaB activity determine the severity of endotoxin-induced acute lung injury. J Immunol 176: 4995–5005, 2006 [DOI] [PubMed] [Google Scholar]
- 25. Fawke J, Lum S, Kirkby J, Hennessy E, Marlow N, Rowell V, Thomas S, Stocks J. Lung function and respiratory symptoms at 11 years in extremely preterm children: The EPICure Study. Am J Respir Crit Care Med 182: 237–245, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fong CH, Bebien M, Didierlaurent A, Nebauer R, Hussell T, Broide D, Karin M, Lawrence T. An anti-inflammatory role for IKKbeta through the inhibition of “classical” macrophage activation. J Exp Med 205: 1269–1276, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Galambos C, Demello DE. Regulation of alveologenesis: clinical implications of impaired growth. Pathology 40: 124–140, 2008 [DOI] [PubMed] [Google Scholar]
- 28. Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell 140: 883–899, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Guignabert C, Alvira CM, Alastalo TP, Sawada H, Hansmann G, Zhao M, Wang L, El-Bizri N, Rabinovitch M. Tie2-mediated loss of peroxisome proliferator-activated receptor-γ in mice causes PDGF-receptor-β-dependant pulmonary arterial muscularization. Am J Physiol Lung Cell Mol Physiol 297: L1082–L1090, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hall JL, Wang X, Van A, Zhao Y, Gibbons GH. Overexpression of Ref-1 inhibits hypoxia and tumor necrosis factor-induced endothelial cell apoptosis through nuclear factor-kappaB-independent and -dependent pathways. Circ Res 88: 1247–1253, 2001 [DOI] [PubMed] [Google Scholar]
- 31. Hansmann G, de Jesus Perez VA, Alastalo TP, Alvira CM, Guignabert C, Bekker JM, Schellong S, Urashima T, Wang L, Morrell NW, Rabinovitch M. An antiproliferative BMP-2/PPARgamma/apoE axis in human and murine SMCs and its role in pulmonary hypertension. J Clin Invest 118: 1846–1857, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hayden MS, Ghosh S. Shared principles in NF-kappaB signaling. Cell 132: 344–362, 2008 [DOI] [PubMed] [Google Scholar]
- 33. Hyde DM, Blozis SA, Avdalovic MV, Putney LF, Dettorre R, Quesenberry NJ, Singh P, Tyler NK. Alveoli increase in number but not size from birth to adulthood in rhesus monkeys. Am J Physiol Lung Cell Mol Physiol 293: L570–L579, 2007 [DOI] [PubMed] [Google Scholar]
- 34. Jakkula M, Le Cras TD, Gebb S, Hirth KP, Tuder RM, Voelkel NF, Abman SH. Inhibition of angiogenesis decreases alveolarization in the developing rat lung. Am J Physiol Lung Cell Mol Physiol 279: L600–L607, 2000 [DOI] [PubMed] [Google Scholar]
- 35. Kang JL, Lee HW, Lee HS, Pack IS, Chong Y, Castranova V, Koh Y. Genistein prevents nuclear factor-kappa B activation and acute lung injury induced by lipopolysaccharide. Am J Respir Crit Care Med 164: 2206–2212, 2001 [DOI] [PubMed] [Google Scholar]
- 36. Keifer JA, Guttridge DC, Ashburner BP, Baldwin AS., Jr Inhibition of NF-kappa B activity by thalidomide through suppression of IkappaB kinase activity. J Biol Chem 276: 22382–22387, 2001 [DOI] [PubMed] [Google Scholar]
- 37. Knudsen L, Weibel ER, Gundersen HJ, Weinstein FV, Ochs M. Assessment of air space size characteristics by intercept (chord) measurement: an accurate and efficient stereological approach. J Appl Physiol 108: 412–421, 2010 [DOI] [PubMed] [Google Scholar]
- 38. Lawrence T, Bebien M, Liu GY, Nizet V, Karin M. IKKalpha limits macrophage NF-kappaB activation and contributes to the resolution of inflammation. Nature 434: 1138–1143, 2005 [DOI] [PubMed] [Google Scholar]
- 39. Lawrence T, Gilroy DW, Colville-Nash PR, Willoughby DA. Possible new role for NF-kappaB in the resolution of inflammation. Nat Med 7: 1291–1297, 2001 [DOI] [PubMed] [Google Scholar]
- 40. Le Cras TD, Markham NE, Tuder RM, Voelkel NF, Abman SH. Treatment of newborn rats with a VEGF receptor inhibitor causes pulmonary hypertension and abnormal lung structure. Am J Physiol Lung Cell Mol Physiol 283: L555–L562, 2002 [DOI] [PubMed] [Google Scholar]
- 41. Lee H, Lin CI, Liao JJ, Lee YW, Yang HY, Lee CY, Hsu HY, Wu HL. Lysophospholipids increase ICAM-1 expression in HUVEC through a Gi- and NF-κB-dependent mechanism. Am J Physiol Cell Physiol 287: C1657–C1666, 2004 [DOI] [PubMed] [Google Scholar]
- 42. Londhe VA, Nguyen HT, Jeng JM, Li X, Li C, Tiozzo C, Zhu N, Minoo P. NF-κB induces lung maturation during mouse lung morphogenesis. Dev Dyn 237: 328–338, 2008 [DOI] [PubMed] [Google Scholar]
- 43. Martin D, Galisteo R, Gutkind JS. CXCL8/IL8 stimulates vascular endothelial growth factor (VEGF) expression and the autocrine activation of VEGFR2 in endothelial cells by activating NFkappaB through the CBM (Carma3/Bcl10/Malt1) complex. J Biol Chem 284: 6038–6042, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Massaro D, Teich N, Maxwell S, Massaro GD, Whitney P. Postnatal development of alveoli. Regulation and evidence for a critical period in rats. J Clin Invest 76: 1297–1305, 1985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Mayo MW, Denlinger CE, Broad RM, Yeung F, Reilly ET, Shi Y, Jones DR. Ineffectiveness of histone deacetylase inhibitors to induce apoptosis involves the transcriptional activation of NF-kappa B through the Akt pathway. J Biol Chem 278: 18980–18989, 2003 [DOI] [PubMed] [Google Scholar]
- 46. Moine P, McIntyre R, Schwartz MD, Kaneko D, Shenkar R, Le Tulzo Y, Moore EE, Abraham E. NF-kappaB regulatory mechanisms in alveolar macrophages from patients with acute respiratory distress syndrome. Shock 13: 85–91, 2000 [DOI] [PubMed] [Google Scholar]
- 47. Mund SI, Stampanoni M, Schittny JC. Developmental alveolarization of the mouse lung. Dev Dyn 237: 2108–2116, 2008 [DOI] [PubMed] [Google Scholar]
- 48. Nakakuki T, Ito M, Iwasaki H, Kureishi Y, Okamoto R, Moriki N, Kongo M, Kato S, Yamada N, Isaka N, Nakano T. Rho/Rho-kinase pathway contributes to C-reactive protein-induced plasminogen activator inhibitor-1 expression in endothelial cells. Arterioscler Thromb Vasc Biol 25: 2088–2093, 2005 [DOI] [PubMed] [Google Scholar]
- 49. Ono M. Molecular links between tumor angiogenesis and inflammation: inflammatory stimuli of macrophages and cancer cells as targets for therapeutic strategy. Cancer Sci 99: 1501–1506, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Orlowski RZ, Stinchcombe TE, Mitchell BS, Shea TC, Baldwin AS, Stahl S, Adams J, Esseltine DL, Elliott PJ, Pien CS, Guerciolini R, Anderson JK, Depcik-Smith ND, Bhagat R, Lehman MJ, Novick SC, O'Connor OA, Soignet SL. Phase I trial of the proteasome inhibitor PS-341 in patients with refractory hematologic malignancies. J Clin Oncol 20: 4420–4427, 2002 [DOI] [PubMed] [Google Scholar]
- 51. Ortiz LA, Champion HC, Lasky JA, Gambelli F, Gozal E, Hoyle GW, Beasley MB, Hyman AL, Friedman M, Kadowitz PJ. Enalapril protects mice from pulmonary hypertension by inhibiting TNF-mediated activation of NF-κB and AP-1. Am J Physiol Lung Cell Mol Physiol 282: L1209–L1221, 2002 [DOI] [PubMed] [Google Scholar]
- 51a. Patterson C, Perrella MA, Hsieh CM, Yoshizumi M, Lee M, Haber E. Cloning and functional analysis of the promoter for KDR/flk-1, a receptor for vascular endothelial growth factor. J Biol Chem 270: 23111–23118, 1995 [DOI] [PubMed] [Google Scholar]
- 52. Perkins ND. Integrating cell-signalling pathways with NF-kappaB and IKK function. Nat Rev Mol Cell Biol 8: 49–62, 2007 [DOI] [PubMed] [Google Scholar]
- 53. Pham LV, Tamayo AT, Yoshimura LC, Lo P, Ford RJ. Inhibition of constitutive NF-kappa B activation in mantle cell lymphoma B cells leads to induction of cell cycle arrest and apoptosis. J Immunol 171: 88–95, 2003 [DOI] [PubMed] [Google Scholar]
- 54. Pierce JW, Schoenleber R, Jesmok G, Best J, Moore SA, Collins T, Gerritsen ME. Novel inhibitors of cytokine-induced IkappaBalpha phosphorylation and endothelial cell adhesion molecule expression show anti-inflammatory effects in vivo. J Biol Chem 272: 21096–21103, 1997 [DOI] [PubMed] [Google Scholar]
- 55. Portis T, Harding JC, Ratner L. The contribution of NF-kappa B activity to spontaneous proliferation and resistance to apoptosis in human T-cell leukemia virus type 1 Tax-induced tumors. Blood 98: 1200–1208, 2001 [DOI] [PubMed] [Google Scholar]
- 56. Raghuwanshi SK, Nasser MW, Chen X, Strieter RM, Richardson RM. Depletion of beta-arrestin-2 promotes tumor growth and angiogenesis in a murine model of lung cancer. J Immunol 180: 5699–5706, 2008 [DOI] [PubMed] [Google Scholar]
- 57. Rahman A, Kefer J, Bando M, Niles WD, Malik AB. E-selectin expression in human endothelial cells by TNF-α-induced oxidant generation and NF-κB activation. Am J Physiol Lung Cell Mol Physiol 275: L533–L544, 1998 [DOI] [PubMed] [Google Scholar]
- 58. Read MA, Cordle SR, Veach RA, Carlisle CD, Hawiger J. Cell-free pool of CD14 mediates activation of transcription factor NF-kappa B by lipopolysaccharide in human endothelial cells. Proc Natl Acad Sci USA 90: 9887–9891, 1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Read MA, Whitley MZ, Williams AJ, Collins T. NF-kappa B and I kappa B alpha: an inducible regulatory system in endothelial activation. J Exp Med 179: 503–512, 1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ronicke V, Risau W, Breier G. Characterization of the endothelium-specific murine vascular endothelial growth factor receptor-2 (Flk-1) promoter. Circ Res 79: 277–285, 1996 [DOI] [PubMed] [Google Scholar]
- 61. Sahebjami H, Domino M. Effects of postnatal dexamethasone treatment on development of alveoli in adult rats. Exp Lung Res 15: 961–973, 1989 [DOI] [PubMed] [Google Scholar]
- 62. Sakamoto K, Maeda S, Hikiba Y, Nakagawa H, Hayakawa Y, Shibata W, Yanai A, Ogura K, Omata M. Constitutive NF-kappaB activation in colorectal carcinoma plays a key role in angiogenesis, promoting tumor growth. Clin Cancer Res 15: 2248–2258, 2009 [DOI] [PubMed] [Google Scholar]
- 63. Sawada H, Mitani Y, Maruyama J, Jiang BH, Ikeyama Y, Dida FA, Yamamoto H, Imanaka-Yoshida K, Shimpo H, Mizoguchi A, Maruyama K, Komada Y. A nuclear factor-kappaB inhibitor pyrrolidine dithiocarbamate ameliorates pulmonary hypertension in rats. Chest 132: 1265–1274, 2007 [DOI] [PubMed] [Google Scholar]
- 64. Schmidt-Ullrich R, Memet S, Lilienbaum A, Feuillard J, Raphael M, Israel A. NF-kappaB activity in transgenic mice: developmental regulation and tissue specificity. Development 122: 2117–2128, 1996 [DOI] [PubMed] [Google Scholar]
- 65. Schnell SA, Staines WA, Wessendorf MW. Reduction of lipofuscin-like autofluorescence in fluorescently labeled tissue. J Histochem Cytochem 47: 719–730, 1999 [DOI] [PubMed] [Google Scholar]
- 66. Seo KH, Ko HM, Choi JH, Jung HH, Chun YH, Choi IW, Lee HK, Im SY. Essential role for platelet-activating factor-induced NF-kappaB activation in macrophage-derived angiogenesis. Eur J Immunol 34: 2129–2137, 2004 [DOI] [PubMed] [Google Scholar]
- 67. Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, Hale EC, Newman NS, Schibler K, Carlo WA, Kennedy KA, Poindexter BB, Finer NN, Ehrenkranz RA, Duara S, Sanchez PJ, O'Shea TM, Goldberg RN, Van Meurs KP, Faix RG, Phelps DL, Frantz ID, 3rd, Watterberg KL, Saha S, Das A, Higgins RD. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 126: 443–456, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Strizzi L, Hardy KM, Seftor EA, Costa FF, Kirschmann DA, Seftor RE, Postovit LM, Hendrix MJ. Development and cancer: at the crossroads of Nodal and Notch signaling. Cancer Res 69: 8526–8527, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Tabary O, Boncoeur E, de Martin R, Pepperkok R, Clement A, Schultz C, Jacquot J. Calcium-dependent regulation of NF-(kappa)B activation in cystic fibrosis airway epithelial cells. Cell Signal 18: 652–660, 2006 [DOI] [PubMed] [Google Scholar]
- 70. Thébaud B, Ladha F, Michelakis ED, Sawicka M, Thurston G, Eaton F, Hashimoto K, Harry G, Haromy A, Korbutt G, Archer SL. Vascular endothelial growth factor gene therapy increases survival, promotes lung angiogenesis, and prevents alveolar damage in hyperoxia-induced lung injury: evidence that angiogenesis participates in alveolarization. Circulation 112: 2477–2486, 2005 [DOI] [PubMed] [Google Scholar]
- 71. Tong Q, Zheng L, Lin L, Li B, Wang D, Huang C, Matuschak GM, Li D. Participation of the PI-3K/Akt-NF-kappa B signaling pathways in hypoxia-induced mitogenic factor-stimulated Flk-1 expression in endothelial cells. Respir Res 7: 101, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Voelkel NF, Douglas IS, Nicolls M. Angiogenesis in chronic lung disease. Chest 131: 874–879, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Weih F, Carrasco D, Durham SK, Barton DS, Rizzo CA, Ryseck RP, Lira SA, Bravo R. Multiorgan inflammation and hematopoietic abnormalities in mice with a targeted disruption of RelB, a member of the NF-kappa B/Rel family. Cell 80: 331–340, 1995 [DOI] [PubMed] [Google Scholar]
- 74. Wong PM, Lees AN, Louw J, Lee FY, French N, Gain K, Murray CP, Wilson A, Chambers DC. Emphysema in young adult survivors of moderate-to-severe bronchopulmonary dysplasia. Eur Respir J 32: 321–328, 2008 [DOI] [PubMed] [Google Scholar]
- 75. Wright JG, Christman JW. The role of nuclear factor kappa B in the pathogenesis of pulmonary diseases: implications for therapy. Am J Respir Med 2: 211–219, 2003 [DOI] [PubMed] [Google Scholar]
- 76. Yang G, Abate A, George AG, Weng YH, Dennery PA. Maturational differences in lung NF-kappaB activation and their role in tolerance to hyperoxia. J Clin Invest 114: 669–678, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Zulueta JJ, Sawhney R, Kayyali U, Fogel M, Donaldson C, Huang H, Lanzillo JJ, Hassoun PM. Modulation of inducible nitric oxide synthase by hypoxia in pulmonary artery endothelial cells. Am J Respir Cell Mol Biol 26: 22–30, 2002 [DOI] [PubMed] [Google Scholar]