Abstract
There is currently no standardized therapy available for metastatic breast cancer in patients with aromatase inhibitor (AI)-resistant breast cancer. We conducted a prospective study to examine the efficacy and safety of high-dose toremifene (TOR) treatment for the first-line treatment of metastatic breast cancer following AI adjuvant therapy. A multicenter phase II study was designed (Registry no.: UMIN000000489). Inclusion criteria comprised hormone-responsive postmenopausal women who had received adjuvant AI postoperatively for >1 year and had relapsed during the treatment or within 12 months of completion of adjuvant therapy. Treatment comprised oral intake of 120 mg TOR once a day. The primary endpoint was objective response rate (ORR). The secondary endpoints were evaluations of clinical benefit (CB), progression-free survival (PFS) and toxicity. A total of 13 patients were enrolled. ORR was 7.7% (1/13) [95% CI, 0.2–36.0%]. In total, 7 patients (53.8%) had stable disease (SD), 5 of whom were long SD, and 5 patients (38.5%) experienced progressive disease (PD). The CB rate was 46.2% (6/13) [95% CI, 19.2–74.9%]. The median time to PFS was 5.9 months. No serious adverse events were observed. Patients with HER2-positive disease exhibited marginally poorer PFS (p=0.08). Patients with PD had a relatively short duration of AI treatment in contrast to responders, who had a longer period of AI treatment (p=0.02). High-dose TOR as a first-line treatment following AI adjuvant therapy was effective and well tolerated. A longer duration of adjuvant AI therapy and negative HER2 overexpression may, with further studies, be beneficial as positive predictive factors for the effectiveness of TOR treatment.
Keywords: breast cancer, aromatase inhibitor resistant, toremifene
Introduction
Aromatase inhibitors (AI) are standard agents in adjuvant hormone therapy for postmenopausal breast cancer patients (1–3). Since 2005, the American Society of Clinical Oncology Technology Assessment has recommended initial AI or AI administered after treatment with tamoxifen for postmenopausal breast cancer (4). However, as yet no standardized therapy is available for metastatic breast cancer in patients with AI-resistant breast cancer (5–9). Thus, the development of non-cross-resistant endocrine agents is crucial, particularly since AI has increasingly been used in the adjuvant setting.
Toremifene (TOR) is a selective estrogen receptor (ER) modulators (SERM). The efficacy in the adjuvant setting has been equivalent to tamoxifen (TAM) (10–13). The standard dose of TOR is 40 mg administered orally once a day. Moreover, high-dose TOR of 120 mg once a day has been approved in Japan. High-dose TOR has the property of competing with estrogen at the ER site, as well as suppressing insulin-like growth factor I-dependent growth (14) and angiogenesis (15). High-dose TOR is effective in TAM-resistant breast cancer and has been used for secondary endocrine therapy (16). We therefore conducted a prospective, multicenter phase II study of high-dose TOR in the first-line treatment of metastatic breast cancer following aromatase inhibitor adjuvant therapy.
Patients and methods
Study design and ethics
This was an open-label multicenter phase II study conducted at 8 centers in Japan (International Clinical Trials Registry No.: UMIN000000489). This study was conducted in accordance with the Declaration of Helsinki and Japanese Ethical Guideline of Clinical Research. The protocol was reviewed and approved by the institutional review board of each participating institution. Written informed consent was obtained from the patients prior to the study.
Eligibility
Patients were included if they met the following eligibility criteria: women who had undergone surgery for histologically confirmed primary invasive breast cancer that was positive for estrogen receptor (ER) and progesterone receptor (PgR), or both; had received adjuvant AI postoperatively for >1 year including switching after TAM and relapse during the treatment or within 12 months of completion of adjuvant therapy; for postmenopausal women, menopause in this study was defined as: age >60 years, age >45 years with amenorrhea for ≥2 years without hysterectomy or bilateral ovariectomy; measurable disease by Response Evaluation Criteria in Solid Tumors; no prior therapy for metastatic disease; Eastern Cooperative Oncology Group performance status of 0–1; life expectancy of >12 weeks; and adequate organ function at the time of enrollment. Pre- or postoperative chemotherapy was allowed. Patients were excluded if they had any of the following conditions: invasive cancer in other organs for which treatment was not completed within 5 years; brain metastasis; bilateral breast cancer; male breast cancer; severe drug allergy; uncontrollable complications; and psychological disease.
Treatment
Patients were treated with 120 mg toremifene (Fareston®, Nippon Kayaku Co., Ltd, Tokyo, Japan) once a day orally. Treatment was administered until tumor progression or unacceptable adverse events occurred.
Clinical response assessment
Radiological evaluation was scheduled at least every 3 months using computed tomography or magnetic resonance imaging. Clinical response was evaluated according to the Response Evaluation Criteria in Solid Tumors (RECIST) guidelines (17). Efficacy was judged by the clinicians at each facility.
Toxicity assessment
The severity of adverse events (AEs) was evaluated using the National Cancer Institute Common Toxicity Criteria (NCI-CTC) version 3.0. Patients were monitored for clinical and laboratory toxic effects at least every 12 weeks. Drug-related AEs were monitored during the study period.
Endpoints and statistical analysis
The primary endpoint was objective response rate (ORR). The secondary endpoints were clinical benefit (CB) rate, progression-free survival (PFS) and toxicity. A complete response (CR) was defined as the complete disappearance of the measurable lesions; a partial response (PR) as a decrease by 30% or more in the sum of the longest diameters (LDs) of measurable lesions; progressive disease (PD) as an increase of 20% or more in the sum of the LDs of measurable lesions; and long-lasting stable disease (long SD) as stable disease (SD) in the size of measurable lesions for 24 weeks or longer. ORR was defined as the sum of the frequencies of CR and PR, and the CB rate as the sum of the frequencies of CR, PR, and long SD. For analysis of primary efficacy, we expected that approximately 20% of the patients would achieve clinical response, and the acceptable lower limit of response rate was estimated to be 5%. The necessary number of patients was calculated to be 40 under the conditions of the one-sided test (α=0.05, β=0.10). All treated patients were analyzed for safety. The case records were reviewed carefully and judged by the Clinical Trial Office, Nagoya University, Japan.
Statistical analysis
Statistical analysis was performed using SAS software, version 9.1.3, Service Pack 4 (SAS Institute Japan, Ltd.). Survival rates were calculated by the Kaplan-Meier method, and statistical significance was evaluated using the log-rank test. The relationship between response and duration of AI was assessed by using Spearman’s rank correlation coefficient. P<0.05 was considered to be statistically significant.
Results
Patient characteristics
A total of 13 patients were enrolled from 8 centers between January 2006 and August 2010. The patient characteristics are shown in Table I. All patients had received postoperative adjuvant AI for >1 year and relapsed during the treatment. They had no prior therapy for metastasis. The mean age was 63.6 years (range 52–75). A total of 8 patients (61.5%) had undergone chemotherapy. Of these, 5 patients (38.5%) were administered an anthracycline-containing regimen and taxane, respectively, 2 patients (15.4%) had only an anthracycline-containing regimen, and 1 patient (7.7%) was treated with an anthracycline-containing regimen, taxane and trastuzumab, respectively. With regard to adjuvant AI, 12 patients (92.3%) had received anastrozole (Arimidex®, AstraZenaca KK, Osaka, Japan) and 1 patient (7.7%) had received exemestane (Aromacin®, Pfizer Japan Inc., Tokyo, Japan). A total of 12 patients (92.3%) had received AI as initial hormone therapy, and 1 patient (7.7%) switched hormone therapy after TAM. The mean duration of AI therapy prior to recurrence was 33.2 months (range 14–52).
Table I.
Baseline characteristics of patients (n=13).
| Characteristic | Patients |
|---|---|
| Median age, years (range) | 63.6 (52–75) |
| Primary stage | |
| I | 2 |
| II | 2 |
| III | 9 |
| Hormone receptor | |
| ER (+) and PgR (+) | 3 |
| ER (+) and PgR (−) | 10 |
| ER (−) and PgR (+) | 0 |
| ER (−) and PgR (−) | 0 |
| HER2 overexpression | |
| 0 | 6 |
| 1 | 4 |
| 2 | 0 |
| 3 | 3 |
| Disease sites | |
| Lymph nodes, soft tissue | 7 |
| Chest wall | 1 |
| Lung | 2 |
| Liver | 3 |
| Duration of AI for adjuvant therapy (years) | |
| <1 | 0 |
| 1–2 | 3 |
| 2–3 | 5 |
| 3–4 | 3 |
| 4–5 | 2 |
| <5 | 0 |
Clinical response and safety profiles of the 13 patients were used for this analysis. This study was prematurely terminated due to low accrual recruitment as a result of the paucity of cases with only first-line treatment of patients with metastatic breast cancer resistant to the adjuvant aromatase inhibitor.
Clinical responses
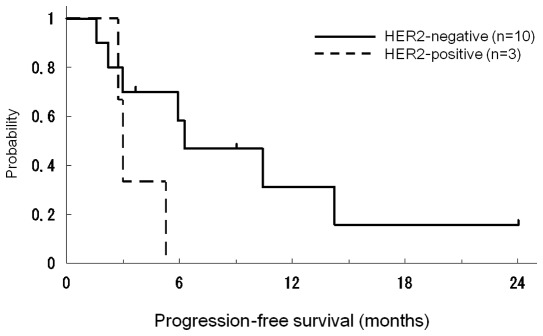
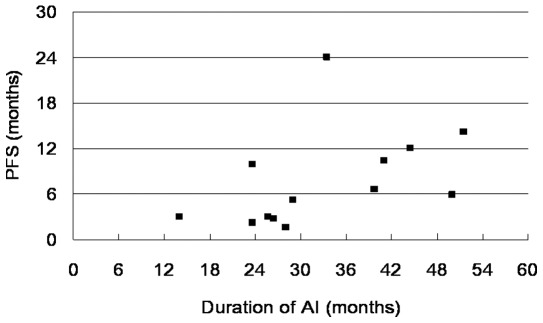
Patients were evaluable for assessment of response. ORR was 7.7% (1/13) [95% CI, 0.2–36.0%] with 0% CR and 7.7% PR. A total of 7 patients (53.8%) had SD, 5 of whom were long SD, and 5 patients (38.5%) experienced progressive disease (PD). The CB rate was 46.2% (6/13) [95% CI, 19.2–74.9%]. The patient characteristics according to the responses are shown in Tables II and III. The responders were HER2-negative. Median times in PFS curves according to HER2 status are shown in Fig. 1. The median time to PFS was 5.9 months (range 1.7–24.0). Patients with HER2-positive disease had marginally poorer PFS (p=0.08). The clinical responses according to the duration of AI are shown in Fig. 2. Patients with PD exhibited a relatively short duration of AI treatment compared with the responders, who had a longer period of AI treatment (p=0.02).
Table II.
Patients responding to high-dose toremifene therapy.
| Age | Response | ER/PgR | HER2 | Duration of AI (months) | Disease sites | Time to progression (months) |
|---|---|---|---|---|---|---|
| 74 | Long SD | +/− | 0 | 33.5 | Chest wall | 24.0 |
| 58 | PR | +/− | 0 | 41.0 | Liver | 10.4 |
| 75 | Long SD | +/− | 0 | 51.5 | Lung | 14.2 |
| 52 | Long SD | +/− | 0 | 23.7 | Liver | 9.9 |
| 65 | Long SD | +/− | 0 | 44.5 | Lymph node | 9.0 |
| 66 | Long SD | +/− | 1 | 39.8 | Lung | 6.7 |
SD, stable disease; PR, partial response.
Table III.
Patients not responding to high-dose toremifene therapy.
| Age | Initial response | ER/PgR | HER2 | Duration of AI (months) | Disease sites |
|---|---|---|---|---|---|
| 68 | PD | +/+ | 3 | 26.5 | Lymph nodes |
| 65 | PD | +/− | 1 | 14.0 | Lymph nodes |
| 55 | PD | +/− | 1 | 23.7 | Liver |
| 52 | PD | +/− | 3 | 25.7 | Lymph nodes |
| 75 | PD | +/+ | 1 | 28.0 | Lymph nodes |
SD, stable disease; PD, partial disease.
Figure 1.
Progression-free survival (PFS) curve in 13 patients treated with toremifene 120 mg once daily. The median time to PFS was 5.9 months (range 1.7–24.0). Responders were HER2-negative. Patients with HER2-positive disease had marginally poorer PFS (p=0.08; log-rank test).
Figure 2.
Progression-free survival (PFS) and the duration of AI. Patients with PD had a relatively short duration of AI treatment compared with responders, who had a longer period of AI treatment (p=0.02; Spearman’s rank correlation coefficient test).
Safety and tolerability
Adverse events were evaluated in 13 patients, and are shown in Table IV. No serious adverse events were observed. Patients received >80% of planned treatment with TOR 120 mg. No patients required premature discontinuation. In 1 case, hepatic dysfunction of Grade 3 was observed, but was cured without interruption. No cases of thromboembolism were reported.
Table IV.
Adverse events (n=13)a.
| Events | n | Grade (n) |
|---|---|---|
| AST, sGOT | 3 | 3 (1), 1 (2) |
| ALT, sGPT | 3 | 3 (1), 1 (2) |
| Hypertriglyceridemia | 2 | 3 (1), 1 (1) |
| Alkaline phosphatase | 1 | 1 (1) |
| GGT (γGTP) | 1 | 1 (1) |
| Hypercholesteremia | 1 | 1 (1) |
| Leukocytes | 1 | 1 (1) |
| Anorexia | 1 | 1 (1) |
| Creatinine | 1 | 1 (1) |
| Hypocalcemia | 1 | 1 (1) |
CTCAE v. 3.0.
Discussion
Despite improvements in adjuvant endocrine therapy, numerous patients harboring hormone-responsive tumors relapse and require endocrine therapy in advanced disease. Although AIs are standard agents for adjuvant hormone therapy for postmenopausal breast cancer patients, treatment options are required for metastatic breast cancer in patients with AI-resistant metastatic breast cancer. In the most up-to-date guidelines, AI therapy has been recommended at a certain point during adjuvant treatment as up-front therapy or in sequential treatment following tamoxifen (18). However, no randomized data are available to date regarding the efficacy of estrogens or SERMs among patients failing treatment with an AI. Thus, more data regarding clinical efficacy and toxicity are required to support endocrine therapy as a reasonable choice in this setting (9).
Our phase II study, albeit of a limited number of patients, indicates that high-dose toremifene is effective and safe as a first-line treatment for patients with adjuvant AI-resistant metastatic breast cancer. In published studies regarding AI-resistant metastatic breast cancer, ORR and CB of TAM treatment after anastrozole failure (n=95) were 7.4 and 56.8%, respectively (5). ORR and CB of exemestane regarding non-steroidal AI failure (n=105) were 4.8 and 20.0%, respectively (6). ORR and CB of fulvestrant, an ER antagonist, after treatment with a third-generation AI (n=77) were 14.3 and 35%, respectively (7). Another study group revealed that the CB of fulvestrant after AI treatment was 30%, and indicated that any prior response to an AI did not appear to offer predictive benefit with fulvestrant (8).
The efficacy of high-dose TOR following AI failure has been evaluated in only a small number of clinical studies. In a larger retrospective study in which the efficacy of 120 mg TOR was analyzed with AI-failure cases (n=80), ORR and CB were 15 and 45%, respectively (19). In cases where tamoxifen preceded AI, high-dose TOR was effective for tamoxifen-resistant breast cancer (20–22). The majority of the patients in that study as well as ours tolerated the side effects and experienced a more favorable quality of life during treatment.
In our limited number of patients, high-dose TOR was ineffective on HER2-positive patients or those who had undergone a relatively short period of AI treatment. Recently, trastuzumab plus anastrozole exhibited improved outcomes for patients with HER2/hormone receptor-co-positive metastatic breast cancer compared with anastrozole alone (23). In the case of HER2/hormone receptor-co-positive patients, use of a hormone receptor blockade alone may not suffice for inhibition of cancer growth. Endocrine resistance while receiving AIs may be due to enhanced signal transduction pathways, such as HER2 and ras/raf/mitogen-activated protein kinase (24). Further investigation using a larger cohort is required for a more precise predictive biomarker analysis.
In conclusion, high-dose TOR is effective for AI-resistant metastatic breast cancer with favorable toxicity, and may be considered as a treatment option. This is the first report on the efficacy of high-dose TOR therapy for metastatic breast cancer in patients with AI-resistant metastatic breast cancer. A phase III study is required to determine the most favorable treatment following AI failure.
Acknowledgements
This study was presented in part at the primary therapy of early breast cancer 12th International Conference, St. Gallen, Switzerland, 16–19, March 2011.
Abbreviations
- AI
aromatase inhibitors
- TAM
tamoxifen
- TOR
toremifene
- SERM
selective estrogen receptor modulators
References
- 1.Baum M, Budzar AU, Cuzick J, Forbes J, Houghton JH, Klijn JG, Sahmoud T. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early breast cancer: first results of the ATAC randomised trial. Lancet. 2002;359:2131–2139. doi: 10.1016/s0140-6736(02)09088-8. [DOI] [PubMed] [Google Scholar]
- 2.Howell A, Cuzick J, Baum M, Buzdar A, Dowsett M, Forbes JF, Hoctin-Boes G, Houghton J, Locker GY, Tobias JS. Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet. 2005;365:60–62. doi: 10.1016/S0140-6736(04)17666-6. [DOI] [PubMed] [Google Scholar]
- 3.Thurlimann B, Keshaviah A, Coates AS, Mouridsen H, Mauriac L, Forbes JF, Paridaens R, Castiglione-Gertsch M, Gelber RD, Rabaglio M, et al. A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med. 2005;353:2747–2757. doi: 10.1056/NEJMoa052258. [DOI] [PubMed] [Google Scholar]
- 4.Winer EP, Hudis C, Burstein HJ, Wolff AC, Pritchard KI, Ingle JN, Chlebowski RT, Gelber R, Edge SB, Gralow J, et al. American Society of Clinical Oncology technology assessment on the use of aromatase inhibitors as adjuvant therapy for postmenopausal women with hormone receptor-positive breast cancer: status report 2004. J Clin Oncol. 2005;23:619–629. doi: 10.1200/JCO.2005.09.121. [DOI] [PubMed] [Google Scholar]
- 5.Thurlimann B, Robertson JF, Nabholtz JM, Buzdar A, Bonneterre J. Efficacy of tamoxifen following anastrozole (‘Arimidex’) compared with anastrozole following tamoxifen as first-line treatment for advanced breast cancer in postmenopausal women. Eur J Cancer. 2003;39:2310–2317. doi: 10.1016/s0959-8049(03)00602-6. [DOI] [PubMed] [Google Scholar]
- 6.Lonning PE, Bajetta E, Murray R, Tubiana-Hulin M, Eisenberg PD, Mickiewicz E, Celio L, Pitt P, Mita M, Aaronson NK, et al. Activity of exemestane in metastatic breast cancer after failure of nonsteroidal aromatase inhibitors: a phase II trial. J Clin Oncol. 2000;18:2234–2244. doi: 10.1200/JCO.2000.18.11.2234. [DOI] [PubMed] [Google Scholar]
- 7.Ingle JN, Suman VJ, Rowland KM, Mirchandani D, Bernath AM, Camoriano JK, Fishkin PA, Nikcevich DA, Perez EA. Fulvestrant in women with advanced breast cancer after progression on prior aromatase inhibitor therapy: North Central Cancer Treatment Group Trial N0032. J Clin Oncol. 2006;24:1052–1056. doi: 10.1200/JCO.2005.04.1053. [DOI] [PubMed] [Google Scholar]
- 8.Perey L, Paridaens R, Hawle H, Zaman K, Nole F, Wildiers H, Fiche M, Dietrich D, Clement P, Koberle D, et al. Clinical benefit of fulvestrant in postmenopausal women with advanced breast cancer and primary or acquired resistance to aromatase inhibitors: final results of phase II Swiss Group for Clinical Cancer Research Trial (SAKK 21/00) Ann Oncol. 2007;18:64–69. doi: 10.1093/annonc/mdl341. [DOI] [PubMed] [Google Scholar]
- 9.Lonning PE. Additive endocrine therapy for advanced breast cancer – back to the future. Acta Oncol. 2009;48:1092–1101. doi: 10.3109/02841860903117816. [DOI] [PubMed] [Google Scholar]
- 10.Lewis JD, Chagpar AB, Shaughnessy EA, Nurko J, McMasters K, Edwards MJ. Excellent outcomes with adjuvant toremifene or tamoxifen in early stage breast cancer. Cancer. 2010;116:2307–2315. doi: 10.1002/cncr.24940. [DOI] [PubMed] [Google Scholar]
- 11.Pyrhonen S, Ellmen J, Vuorinen J, Gershanovich M, Tominaga T, Kaufmann M, Hayes DF. Meta-analysis of trials comparing toremifene with tamoxifen and factors predicting outcome of antiestrogen therapy in postmenopausal women with breast cancer. Breast Cancer Res Treat. 1999;56:133–143. doi: 10.1023/a:1006250213357. [DOI] [PubMed] [Google Scholar]
- 12.Gams R. Phase III trials of toremifene vs tamoxifen. Oncology (Williston Park) 1997;11:23–28. [PubMed] [Google Scholar]
- 13.Holli K, Valavaara R, Blanco G, Kataja V, Hietanen P, Flander M, Pukkala E, Joensuu H. Safety and efficacy results of a randomized trial comparing adjuvant toremifene and tamoxifen in postmenopausal patients with node-positive breast cancer. Finnish Breast Cancer Group. J Clin Oncol. 2000;18:3487–3494. doi: 10.1200/JCO.2000.18.20.3487. [DOI] [PubMed] [Google Scholar]
- 14.Iino Y, Takai Y, Ando T, Sugamata N, Maemura M, Takeo T, Ohwada S, Morishita Y. Effect of toremifene on the growth, hormone receptors and insulin-like growth factor-1 of hormone-dependent MCF-7 tumors in athymic mice. Cancer Chemother Pharmacol. 1993;32:353–358. doi: 10.1007/BF00735918. [DOI] [PubMed] [Google Scholar]
- 15.Ruohola JK, Valve EM, Karkkainen MJ, Joukov V, Alitalo K, Harkonen PL. Vascular endothelial growth factors are differentially regulated by steroid hormones and antiestrogens in breast cancer cells. Mol Cell Endocrinol. 1999;149:29–40. doi: 10.1016/s0303-7207(99)00003-9. [DOI] [PubMed] [Google Scholar]
- 16.Stenbygaard LE, Herrstedt J, Thomsen JF, Svendsen KR, Engelholm SA, Dombernowsky P. Toremifene and tamoxifen in advanced breast cancer – a double-blind cross-over trial. Breast Cancer Res Treat. 1993;25:57–63. doi: 10.1007/BF00662401. [DOI] [PubMed] [Google Scholar]
- 17.Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–216. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 18.Burstein HJ, Prestrud AA, Seidenfeld J, Anderson H, Buchholz TA, Davidson NE, Gelmon KE, Giordano SH, Hudis CA, Malin J, et al. American Society of Clinical Oncology clinical practice guideline: update on adjuvant endocrine therapy for women with hormone receptor-positive breast cancer. J Clin Oncol. 2010;28:3784–3796. doi: 10.1200/JCO.2009.26.3756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yamamoto Y, Masuda N, Ohtake T, Yamashita H, Saji S, Kimijima I, Kasahara Y, Ishikawa T, Sawaki M, Hozumi Y, Iwase H. Clinical usefulness of high-dose toremifene in patients relapsed on treatment with an aromatase inhibitor. Breast Cancer. 2010;17:254–260. doi: 10.1007/s12282-009-0148-2. [DOI] [PubMed] [Google Scholar]
- 20.Jonsson PE, Malmberg M, Bergljung L, Ingvar C, Ericsson M, Ryden S, Nilsson I, Terje IJ. Phase II study of high dose toremifene in advanced breast cancer progressing during tamoxifene treatment. Anticancer Res. 1991;11:873–875. [PubMed] [Google Scholar]
- 21.Vogel CL, Shemano I, Schoenfelder J, Gams RA, Green MR. Multicenter phase II efficacy trial of toremifene in tamoxifen-refractory patients with advanced breast cancer. J Clin Oncol. 1993;11:345–350. doi: 10.1200/JCO.1993.11.2.345. [DOI] [PubMed] [Google Scholar]
- 22.Pyrhonen S, Valavaara R, Vuorinen J, Hajba A. High dose toremifene in advanced breast cancer resistant to or relapsed during tamoxifen treatment. Breast Cancer Res Treat. 1994;29:223–228. doi: 10.1007/BF00666475. [DOI] [PubMed] [Google Scholar]
- 23.Kaufman B, Mackey JR, Clemens MR, Bapsy PP, Vaid A, Wardley A, Tjulandin S, Jahn M, Lehle M, Feyereislova A, et al. Trastuzumab plus anastrozole versus anastrozole alone for the treatment of postmenopausal women with human epidermal growth factor receptor 2-positive, hormone receptor-positive metastatic breast cancer: results from the randomized phase III TAnDEM study. J Clin Oncol. 2009;27:5529–5537. doi: 10.1200/JCO.2008.20.6847. [DOI] [PubMed] [Google Scholar]
- 24.Kato S, Endoh H, Masuhiro Y, Kitamoto T, Uchiyama S, Sasaki H, Masushige S, Gotoh Y, Nishida E, Kawashima H, et al. Activation of the estrogen receptor through phosphorylation by mitogen-activated protein kinase. Science. 1995;270:1491–1494. doi: 10.1126/science.270.5241.1491. [DOI] [PubMed] [Google Scholar]