Abstract
Estrogen receptor α36 (ERα36) is believed to mediate membrane-initiated effects of estrogen signaling, and promote cell growth and resistance to tamoxifen treatment. However, few studies are available regarding ERα36 expression in gastric cancer. In the present study, we evaluated the expression of ERα36, as well as estrogen receptor α66 (ERα66), in gastric cancer and its correlation with clinicopathological parameters. Real-time polymerase chain reaction (PCR) was applied to detect the expression of ERα66 and ERα36 mRNA in 45 pairs of samples of gastric cancer tissues and matched normal tissues. The ΔΔCT method was used to evaluate the relative quantity of target mRNA expression. Among the 45 pairs of samples of gastric cancer tissues and matched normal tissues adjacent to the tumor, the ERα36 mRNA levels in normal tissues were significantly higher than those observed in gastric cancer tissues (p=0.040). Additionally, the expression of ERα66 mRNA levels between gastric cancer tissues and matched normal tissues had no statistically significant difference. We confirmed that ERα36 mRNA was expressed in the four gastric cancer cell lines, and ERα66 mRNA was expressed in two of the four gastric cancer cell lines. According to the tissue and cell findings, it was suggested that the expression level of ERα36 is greater than that of ERα66 in gastric cancer. In conclusion, the expression of ERα66 and ERα36 in gastric cancer tissues and cells was confirmed in this study. A decreased expression of ERα36 mRNA in gastric cancer tissues may be one of the factors affecting tumorigenesis in gastric cancer patients.
Keywords: gastric cancer, estrogen receptor α36, estrogen receptor α66, variation, polymerase chain reaction
Introduction
Findings of recent studies have shown that there is a possible correlation of estrogen with the biological activity of gastric cancer cells (1), and that the expression of estrogen receptor α66 (ERα66) may correlate with poorer prognosis among patients with gastric cancer (2).
ERα36, a novel variant of the full-length 66 kDa ERα66, has one of the most crucial roles in cell growth and differentiation in various types of cancer (3). This variant differs from ERα66 by lacking the transcriptional activation domains (AF-1 and AF-2), but retains the partial dimerization and ligand-binding domains and DNA-binding domain.
ERα36 enhances oncogenesis, and promotes cell growth and survival during endocrine therapy in breast cancer (4). The expression of ERα36 was subsequently detected in breast (5), colorectal (6) and endometrial cancer (7). Furthermore, unlike ERα66, which is often detected in the cell nucleus, ERα36 is located in the cytoplasm and plasma membrane. As a result, ERα36 mediates the membrane-initiated effects of estrogen signaling cascades and stimulates cell growth (3,8). These features make ERα36 an attractive target for antibody-based therapy.
The expression of ERα66 has been detected in gastric cancer cell lines as well as in normal and cancer tissues. However, the physiological role of ERα66’s possible involvement in the etiology of gastric cancer remains to be clarified. Recently, it was reported that the effect of tamoxifen treatment in ERα66-positive breast tumors could be prevented by ERα36. A similar event may occur in other types of cancer, including gastric cancer. Therefore, understanding the existence and expression status of ERα36 may have significant implications in the prognosis and treatment of gastric cancer.
Although ERα36 has been extensively studied in other types of cancer, no investigation has been conducted in gastric cancer. We hypothesize that ERα66 and its splicing variant ERα36 may play a role in the oncogenesis of gastric cancer. The present study was undertaken to examine the expression of ERα36 and ERα66 in gastric cancer tissues by using a validated specific and sensitive real-time quantitative PCR assay. In this study, we examined tissue from 45 cases of gastric cancer to observe the potential difference of ERα66 and ERα36 expression in gastric cancer tissues and their matched normal tissues, and to assess the correlation between ERα66 and ERα36 expression and clinicopathological characteristics in gastric cancer patients.
Materials and methods
Case selection
Specimens were obtained from 45 patients who underwent curative resection of gastric cancer at the Department of Surgical Oncology of the Sir Run Run Shaw Hospital, Zhejiang University College of Medicine, China, between July 2007 and November 2009. Informed consent was obtained from all patients, and the study was conducted according to the guidelines of the Hospital Ethics Committee. The patients comprised 26 males and 19 females, aged 35–81 years (mean 60.0). The correlation between the expression of ERα36 and ERα66 and clinicopathological parameters including age, gender, differentiation state, location and pTNM pathological classification according to the International Union against Cancer (UICC) (9) were evaluated. The clinicopathological characteristics of the 45 cases are shown in Table I.
Table I.
Clinicopathological characteristics of 45 patients with gastric cancer.
| Clinicopathological characteristics | Case (n) |
|---|---|
| Age | |
| ≤60 | 25 |
| >60 | 20 |
| Gender | |
| Male | 26 |
| Female | 19 |
| Histological type | |
| Differentiated | 22 |
| Undifferentiated | 23 |
| Location | |
| Upper or whole | 15 |
| Middle or lower | 30 |
| Tumor size (cm) | |
| ≤5.5 | 24 |
| >5.5 | 21 |
| Outside of serosal | |
| Yes | 5 |
| No | 40 |
| Node stage | |
| N0-1 | 21 |
| N2-3 | 24 |
Cell culture
Four gastric cancer cell lines, AGS, MKN-45, NCL-N87 and SGC-7901, were maintained in Roswell Park Memorial Institute (RPMI)-1640 medium supplemented with 10% heat-inactivated fetal calf serum, 100 U/ml penicillin G and 100 mg/ml streptomycin.
RNA extraction and cDNA synthesis
Total RNA was extracted from freshly frozen gastric tissues using the TRIzol reagent (Invitrogen Life Technologies, Carlsbad, CA, USA). Total RNA was reverse-transcribed into single-strand complementary DNA (cDNA) using Moloney-murine leukemia (M-MLV) reverse transcriptase (Promega, Madison, WI, USA). Briefly, the RNA was denatured by heating for 5 min at 70°C, cooled on ice, and then used for reverse transcription (2 μg of total RNA, 25 U of RNAse inhibitor, 0.5 mM each of dNTPs, 1.5 μM reverse primer and 200 U of M-MLV reverse transcriptase in a total volume of 25 μl). For reverse transcription, tubes were incubated at 42°C for 60 min, followed by rapid cooling.
Real-time quantitative PCR
Real-time RT-PCR analyses were performed with the ABI Prism 7500 sequence detection system (Applied Biosystems, Foster City, CA, USA). Reaction mixture (25 μl) containing 2 μl of cDNA template, 1 μl each of sense and anti-sense primers and 1X SYBR-Green Universal PCR Mix was amplified as follows: denaturation at 95°C for 10 min and 40 cycles at 95°C for 30 sec, 60°C for 30 sec and 72°C for 40 sec. Real-time quantitative PCR was performed in triplicate for each sample and a mean value of glyceraldehyde 3-phosphate dehydrogenase (GAPDH) was used to calculate mRNA levels. Quantitative analysis was performed using the comparative CT method (10,11). The ERα66 and ERα36 mRNA copy numbers in normal and tumor tissues were normalized to mRNA copy numbers of the housekeeping gene, GAPDH to give a value of ΔCT. This final value was to determine changes in the expression of ERα66 and ERα36 in each sample. The primer sequences for ERα66 were: forward 5′-AAGAAAGAACAACATCAGCAGTAAAGCT-3′; and reverse 5′-GGGCTATGGCTTGGTTAAACAT-3′. The primer sequences for ERα36 were: forward, 5′-CCAAGAATG TTCAACCACAACCT-3′; and reverse 5′-GCACGGTTCATT AACATCTTTCTG-3′. The primers for GAPDH were obtained as previously described (12). Fluorescent data were converted i) into RQ measurements, which represent relative expression, ii )automatically by the SDS system software and iii) exported to Microsoft Excel. Thermal dissociation plots were examined for biphasic melting curves, indicative of whether primer dimers or other non-specific products may be contributing to the amplification signal.
Statistical analysis
Statistical analysis was conducted using the statistical program SPSS 15.0 for Windows (SPSS, Chicago, IL, USA). Pre-treatment characteristics were analyzed using the two-tailed χ2 test. The two-tailed t-test was used to evaluate the correlation between ERα36 expression and the clinicopathological parameters.
Results
Real-time quantitative PCR of the expression of ERα36 and ERα66 in gastric cancer cells
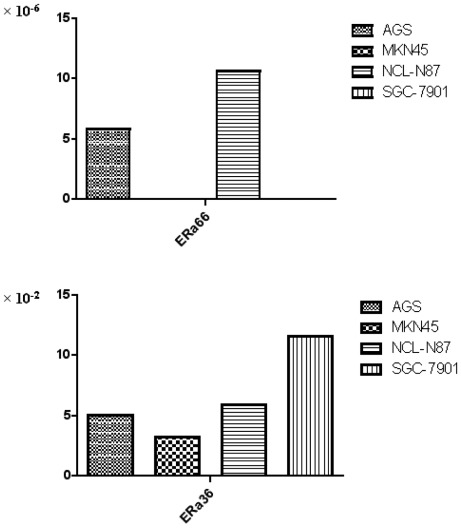
To evaluate mRNA expression of ERα66 and ERα36 in cancer cells, we detected four gastric cancer cell lines. As shown in Fig. 1, ERα66 mRNA was detected in two cell lines, AGS and NCI-N87. By contrast, ERα36 mRNA was detected in the four cell lines. Consistent with the clinical data, the expression of ERα36 mRNA was more predominant than the ERα66 mRNA expression.
Figure 1.
ERα66 and ERα36 mRNA expression level in gastric cancer cells (AGS, MKN45, NCL-N87, SGC-7901).
Expression of ERα36 and ERα66 mRNA in gastric cancer tissues by real-time PCR
Among the 45 pairs of samples of gastric cancer tissues and matched normal tissues adjacent to the tumor, the level of ERα66 of the former was similar to that of the latter, and no significant associations were found between ERα66 mRNA expression in gastric cancer tissues and normal tissues (p=0.135).
As shown in Table II, of the 45 samples of gastric cancer tissues and matched normal tissues adjacent to the tumor, expression of ERα36 was detected in the total samples. In normal tissues, the ERα36 mRNA levels ranged from 0.029 to 157.696 with a median of 2.016. In gastric cancer tissues, the ERα36 mRNA levels ranged from 0.004 to 39.233 with a median of 0.237. The ERα36 mRNA levels in normal tissues were significantly higher than those observed in gastric cancer tissues (p=0.040). Moreover, we found that the expression of ERα36 mRNA was higher than that of ERα66 mRNA in gastric cancer tissues and their matched normal tissues.
Table II.
Relative quantity of ERα36 mRNA and ERα66 mRNA in gastric cancer tissues and matched normal tissues.
| Tumor tissue | Normal tissues | P-value | |
|---|---|---|---|
| Relative ERα36 expression | 1.73±5.85 | 10.54±2.70 | 0.040 |
| Relative ERα66 expression | (7.87±15.66)×10−3 | (4.30±6.98)× 10−3 | 0.135 |
Correlation between ERα36 and clinicopathological parameters
According to the median expression level of ERα36, the 45 cases of gastric cancer were divided into two groups, the high ERα36 expression group (ERα36 expression level >0.237) and the low ERα36 expression group (ERα36 expression level ≤0.237). The mean number of metastasis lymph nodes in the high ERα36 group was lower than that in the low ERα36 expression group (11.4 vs. 7.3), but the differences among them were not statistically significant (p=0.150) (Table III). Moreover, tumor size varied between the high ERα36 expression group versus the low ERα36 expression group (6.4cm vs. 5.2 cm), but the difference was also not statistically significant (p=0.099) (Table III).
Table III.
Correlation between the expression of ERα36 mRNA and the number of metastasis lymph nodes, tumor size.
| ERα36 expression level ≤0.237 | ERα36 expression level >0.237 | P-value | |
|---|---|---|---|
| Number of metastasis lymph nodes | 11.4±11.3 | 7.3±7.1 | 0.150 |
| Tumor size | 6.4±2.4 | 5.2±2.6 | 0.100 |
Discussion
In the present study, we found the relative quantity of ERα36 mRNA and ERα66 mRNA in 45 samples of gastric cancer tissues as determined by real-time PCR. ERα36 mRNA was expressed more predominantly than ERα66 mRNA in gastric cancer and normal tissues adjacent to the tumor.
Recent studies have shown conflicting results of ERα expression in gastric cancer (13,14). Moreover, when using the immunohistochemical method, the expression of ERα gastric cancer tissues showed marked variability (0–62.5%) among a number of studies (15–17). These data suggested that a more reliable and sensitive method was required to evaluate the ERα expression in gastric cancer tissues, particularly those with low expression levels. In the current study, real-time quantitative PCR was used to compare the expression of ERα66 and its splice variant ERα36 mRNA in 45 cases of gastric cancer and their matched normal tissues, which allows the detection of ERα expression in stomach tissues at a low level. In our study, the expression of another ERα66 splice variant, ERα46 mRNA, was also detected; however, it was found in neither the gastric cancer cells nor the gastric cancer tissues.
Estrogen not only modulates cell proliferation in classic estrogen-sensitive tissues, but also in other tissues such as the lungs (18), colon (19) and stomach (15,16). An epidemiological study showed that tamoxifen, an anti-estrogen agent, may increase the incidence of gastric cancer, which suggested that estrogen may be involved in the pathogenesis of gastric cancer (20). However, few studies have reported the expression of ERα66 and its variant forms in gastric cancer.
In the present study, we determined not only ERα66, but also, for the first time, its splicing variant ERα36 mRNA in gastric cancer samples and their matched normal tissues by real-time quantitative PCR assay. Furthermore, we correlated these findings with the clinicopathological parameters of the gastric cancer samples.
The expression levels of ERα66, between gastric cancer tissues and normal tissues did not exhibit a significant difference, and the expression level was extremely low. ERα36 had a differential expression level between normal and cancer tissues, suggesting that ERα36 plays a more significant role in stomach tumorigenesis, and the decrease in this variant was significantly correlated with increased tumor size. This result suggests that ERα36 is involved in gastric cancer proliferation.
Recently, it was reported that aromatase expression in gastric cancer cells, and cancer cells in the presence of testosterone, produced estradiol in a short incubation period, suggesting estrogen is also localized in human gastric cancer tissues (21). However, a randomized, controlled study of adjuvant tamoxifen therapy in gastric cancer found that estrogen receptor α expression is an independent prognostic factor. By contrast, tamoxifen had no effect on overall survival in gastric cancer patients; furthermore, treatment with tamoxifen significantly decreased the survival time of patients with estrogen receptor α-positive tumors (22).
It is notable that breast cancer patients with ERα66 expression-positive tumors that also express high levels of ERα36 are less likely to benefit from tamoxifen treatment (4). In our study, ERα36 mRNA was expressed more predominantly than ERα66 mRNA in gastric cancer tissues, which may be one of the factors impacting on the function of tamoxifen treatment in gastric cancer patients.
The human ERα36 is known to mediate membrane-initiated estrogen and antiestrogen signaling, such as the mitogen-activated protein kinase (MAPK) signaling pathway, which may provide an explanation for the antiestrogen resistance observed in breast cancer patients. Similar results may present in gastric cancer patients. Furthermore, elucidation of the roles of the estrogen receptor and its variant in gastric cancer may contribute to diagnosis and treatment.
References
- 1.Freedman ND, Ahn J, Hou L, et al. Polymorphisms in estrogen- and androgen-metabolizing genes and the risk of gastric cancer. Carcinogenesis. 2009;30:71–77. doi: 10.1093/carcin/bgn258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu CY, Guo JL, Jiang ZN, et al. Prognostic role of estrogen receptor alpha and estrogen receptor beta in gastric cancer. Ann Surg Oncol. 2010;17:2503–2509. doi: 10.1245/s10434-010-1031-2. [DOI] [PubMed] [Google Scholar]
- 3.Wang Z, Zhang X, Shen P, et al. Identification, cloning, and expression of human estrogen receptor-alpha36, a novel variant of human estrogen receptor-alpha66. Biochem Biophys Res Commun. 2005;336:1023–1027. doi: 10.1016/j.bbrc.2005.08.226. [DOI] [PubMed] [Google Scholar]
- 4.Shi L, Dong B, Li Z, et al. Expression of ER-{alpha}36, a novel variant of estrogen receptor {alpha}, and resistance to tamoxifen treatment in breast cancer. J Clin Oncol. 2009;20:3423–3429. doi: 10.1200/JCO.2008.17.2254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee LM, Cao J, Deng H, et al. ER-alpha36, a novel variant of ER-alpha, is expressed in ER-positive and -negative human breast carcinomas. Anticancer Res. 2008;28:479–483. [PMC free article] [PubMed] [Google Scholar]
- 6.Jiang H, Teng R, Wang Q, et al. Transcriptional analysis of estrogen receptor alpha variant mRNAs in colorectal cancers and their matched normal colorectal tissues. J Steroid Biochem Mol Biol. 2008;112:20–24. doi: 10.1016/j.jsbmb.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 7.Lin SL, Yan LY, Liang XW, et al. A novel variant of ER-alpha, ER-alpha36 mediates testosterone-stimulated ERK and Akt activation in endometrial cancer Hec1A cells. Reprod Biol Endocrinol. 2009;24:102. doi: 10.1186/1477-7827-7-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Z, Zhang X, Shen P, et al. A variant of estrogen receptor-{alpha}, hER-{alpha}36: transduction of estrogen- and antiestrogen-dependent membrane-initiated mitogenic signaling. Proc Natl Acad Sci USA. 2006;103:9063–9068. doi: 10.1073/pnas.0603339103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sobin LH, Wittekind C. UICC: TNM Classification of Malignant Tumours. 5. London: Wiley; 1997. [Google Scholar]
- 10.Schmittgen TD, Livak KJ. Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc. 2008;3:1101–1108. doi: 10.1038/nprot.2008.73. [DOI] [PubMed] [Google Scholar]
- 11.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T) Method Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 12.Jiang HP, Teng RY, Wang Q, et al. Estrogen receptor alpha variant ERalpha46 mediates growth inhibition and apoptosis of human HT-29 colon adenocarcinoma cells in the presence of 17beta-oestradiol. Chin Med J (Engl) 2008;121:1025–1031. [PubMed] [Google Scholar]
- 13.Chandanos E, Rubio CA, Lindblad M, et al. Endogenous estrogen exposure in relation to distribution of histological type and estrogen receptors in gastric adenocarcinoma. Gastric Cancer. 2008;11:168–174. doi: 10.1007/s10120-008-0475-6. [DOI] [PubMed] [Google Scholar]
- 14.Kameda C, Nakamura M, Tanaka H, et al. Oestrogen receptor-alpha contributes to the regulation of the hedgehog signalling pathway in ERalpha-positive gastric cancer. Br J Cancer. 2010;16:738–747. doi: 10.1038/sj.bjc.6605517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhao XH, Gu SZ, Liu SX, et al. Expression of estrogen receptor and estrogen receptor messenger RNA in gastric carcinoma tissues. World J Gastroenterol. 2003;9:665–669. doi: 10.3748/wjg.v9.i4.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang M, Pan JY, Song GR, et al. Altered expression of estrogen receptor alpha and beta in advanced gastric adenocarcinoma: correlation with prothymosin alpha and clinicopathological parameters. Eur J Surg Oncol. 2007;33:195–201. doi: 10.1016/j.ejso.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 17.Oshima CT, Wonraht DR, Catarino RM, Mattos D, Forones NM. Estrogen and progesterone receptors in gastric and colorectal cancer. Hepatogastroenterology. 1999;46:3155–3158. [PubMed] [Google Scholar]
- 18.Raso MG, Behrens C, Herynk MH, et al. Immunohistochemical expression of estrogen and progesterone receptors identifies a subset of NSCLCs and correlates with EGFR mutation. Clin Cancer Res. 2009;15:5359–5368. doi: 10.1158/1078-0432.CCR-09-0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nüssler NC, Reinbacher K, Shanny N, et al. Sex-specific differences in the expression levels of estrogen receptor subtypes in colorectal cancer. Gend Med. 2008;5:209–217. doi: 10.1016/j.genm.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 20.Chandanos E, Lindblad M, Rubio CA, et al. Tamoxifen exposure in relation to gastric adenocarcinoma development. Eur J Cancer. 2008;44:1007–1014. doi: 10.1016/j.ejca.2008.02.049. [DOI] [PubMed] [Google Scholar]
- 21.Izawa M, Inoue M, Osaki M, et al. Cytochrome P450 aromatase gene (CYP19) expression in gastric cancer. Gastric Cancer. 2008;11:103–110. doi: 10.1007/s10120-008-0463-x. [DOI] [PubMed] [Google Scholar]
- 22.Harrison JD, Morris DL, Ellis IO, Jones JA, Jackson I. The effect of tamoxifen and estrogen receptor status on survival in gastric carcinoma. Cancer. 1989;64:1007–1010. doi: 10.1002/1097-0142(19890901)64:5<1007::aid-cncr2820640506>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]