Abstract
Hemolymphangioma is a rare, benign and non-invasive type of tumor. Only a few cases have been reported in the literature. In the present study, we report a case of hemolymphangioma growing on the left anterior chest wall of a 57-year-old woman. Physical and laboratory examinations were all normal. However, computed tomography (CT) revealed a mass. A CT-guided biopsy was performed, followed by a thoracoscopic resection and thoracotomy. The postoperative course of the patient was uneventful. Follow up of the patient is ongoing. The findings of this case report, however, showed the significance of complete excision versus minimally invasive surgery to reduce recurrence.
Keywords: hemolymphangioma, chest wall, tumor, surgery
Introduction
Hemolymphangioma is a rare, benign and non-invasive type of tumor. Hemolymphangiomas have been found in the pancreas, at the extremities, in the mediastinum, pericardium and on the tongue, as well as in the orbit, esophagus, retroperitoneally, adrenally, cervically, thoracically, hepatically and in the spleen (1-15). In addition, there are also reports of hemolymphangiomas in the skin, throat, stomach and scrotum in Chinese literature (16-18). However, there have not yet been any cases reported in the chest wall. In the present study, we report one case of hemolymphangioma in the chest wall treated in Nanfang Hospital (China).
Case report
A 57-year-old woman was admitted to the Department of Oncology, Nanfang Hospital, China, in March 2011, with a complaint of chest tightness and shortness of breath, which had persisted for more than a month, as well as a cough and a small amount of sputum, which had persisted for half a month. No abnormalities were found upon physical and laboratory examinations.
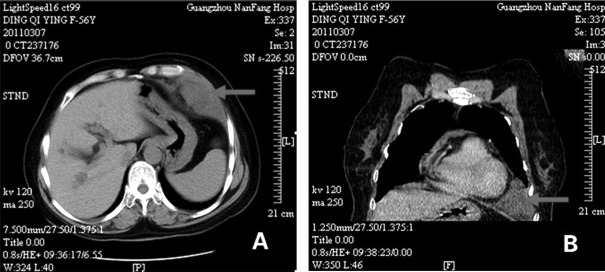
The serum tumor markers tissue polypeptide-specific antigen (TPS), carcinoembryonic antigen (CEA), cancer antigens (CA)125, 153 and 199, neuron-specific enolase (NSE), squamous cell carcinoma antigen (SCCA) and Cyfra21-1 were all within normal ranges. Lactate dehydrogenase (LDH): 226 units/l (normal range, 89-220 units/l), and alkaline phosphatase (ALP): 73 units/l (normal range, 35-160 units/l). Computed tomography (CT) scan revealed a 8.7x4.4-cm mass, with a spindle shape and low density in the left costophrenic angle area, closely adhered to the left anterior chest wall (Figure 1). No abnormal signs were found upon brain magnetic resonance imaging (MRI) examination, abdominal ultrosonography and bone electroconvulsive therapy (ECT). A CT-guided biopsy was performed and the pathological diagnosis was inflammatory fibrous and scar tissue.
Figure 1.
(A) Chest CT scan shows a spindle mass of 8.7x4.4 cm in the left costophrenic angle area, closely adhered to the left anterior chest wall, the precontrast CT value was 15 Hounsfield units. (B) Enhanced scan revealing that the mass is in mild enhancement and close to the pericardium. No significant damage in the surrounding bone is observed. CT, computed tomography.
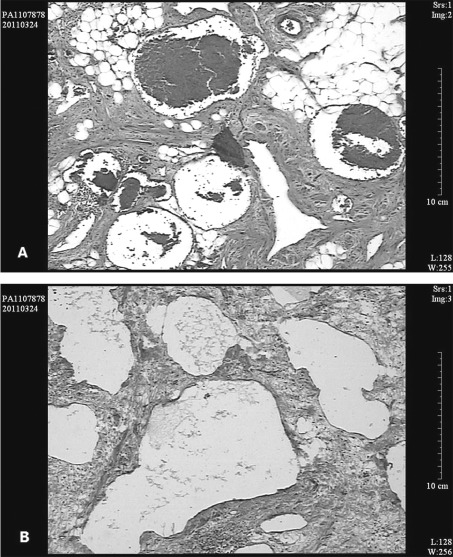
The patient underwent thoracoscopic resection of the tumor following the biopsy. During the surgery, a mass of 9x9x5 cm was found in the left anterior chest wall. The boundary of the mass was unclear. The tumor invaded into the left thoracic cavity and the mediastinum, and was adhered to the chest wall and the lung. Therefore, we abandoned the thoracoscopic surgery and instead performed a thoracotomy. The incision was extended to 20 cm and the tumor was excised following a complete separation. The surgical specimen was hard, gray-brown in color, irregular in shape, and its edge was clear, mostly enveloped. Of note, a diagnosis of hemolymphangioma was confirmed by pathological examination following removal of the mass (Figure 2). The postoperative course of the patient was uneventful and the patient was discharged 2 weeks following the surgery. During 3 months of follow-up, the patient experienced no complications or tumor recurrence detected by tumor markers and CT examination. At present, the patient is being followed up closely and carefully. Written consent for this case report was obtained from the patient.
Figure 2.
H&E staining of the tumor tissue shows round or irregular-shaped lumens of various sizes, covered by endothelium. (A) There are numerous erythrocytes in certain lumens, (B) while lymphatic fluid is shown in other lumens. The lumens are surrounded by adipose or interstitial fibrous tissues. The histological diagnosis is hemolymphangioma. H&E, hematoxylin and eosin.
Discussion
Hemolymphangioma is thought to originate from the mesenchymal tissue. It may be divided into primary and secondary lymphatic vascular tumors. The primary tumor is considered to be a congenital malformation of the lymphatic vascular system. The formation of this tumor may be explained by obstruction of the venolymphatic communication between dysembryoplastic vascular tissue and the systemic circulation. The secondary tumor is caused by poor lymph drainage and lymphatic damage resulting from surgery or trauma (19). According to Landing and Farber, those benign malformations are classified into four categories: capillary, cavernous, cystic (hygroma) and hemolymphangioma (combination of hemangioma and lymphangioma) (20).
In the present study, we report a case that belongs to hemolymphangioma. In general, hemolymphangiomas are large masses of varying sized cystic cavities with thin walls, having multiple thin septa and containing fluid similar to hemorrhagic fluid, and rarely of clear lymphatic nature. Microscopically, the tumor consists of abnormal lymphatic and blood vessels with polycystic spaces. These cysts have connective septa covered by endothelium (1). The tumor is possibly surrounded by adipose or interstitial fibrous tissues. The tumor may grow slowly, and can be found at birth or is diagnosed during childhood (2). The tumor size varies due to the anatomical location and relationship to the neighboring tissues.
The majority of small tumors remain asymptomatic for a long period of time. As the tumor develops, discomfort occurs, which is mainly caused by the occupied tumor. In the present case, the main complaints were chest tightness, shortness of breath, cough, a small amount of sputum and fullness behind the xiphoid, apparently, due to the large tumor on the chest wall. Our experience of this patient indicates that fine-needle aspiration biopsy may lead to misdiagnosis of the disease. Radical surgical resection is the main treatment for this disease. With tumor adhesion or invasion to the surrounding organs, the removal of adjacent organs needs to be considered (3). Findings of this case indicate that in the future minimally invasive surgery should be avoided. Complete excision provides the best results with a lower recurrence rate; however, careful follow-up is necessary. Other non-surgical treatments, including cryotherapy, laser therapy, radiotherapy and local injection of sclerotic agents, compared with surgical treatment, do not show superiority; therefore, surgical excision remains the first choice of treatment to reduce the recurrence (4).
Acknowledgments
We gratefully thank Professor Yang Yang (Department of Pathology and Arkansas Cancer Research Center, University of Arkansas, USA) and Professor Chuannong Zhou (The Chinese Academy of Medical Sciences) for revising the manuscript and providing excellent advice. Professor Kaican Cai is acknowledged for providing the surgical details. The project is supported by the National Natural Science Foundation of China (grant no. 81001212), China Postdoctoral Science Foundation (grant no. 20080431074), Foundation of Zhejiang Provincial Educational Committee (grant no. Y201019175) and the Zhejiang Provincial Health Bureau Foundation (Grant No. 2010KYB036).
References
- 1.Sun LF, Ye HL, Zhou QY. et al. A giant hemolymphangioma of the pancreas in a 20-year-old girl: a report of one case and review of the literature. World J Surg Oncol. 2009;7:31. doi: 10.1186/1477-7819-7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beninson J, Hurley JP. Hemolymphangioma in a neonate - a therapeutic problem - case history. Angiology. 1988;39:1043–1047. doi: 10.1177/000331978803901207. [DOI] [PubMed] [Google Scholar]
- 3.Toyoki Y, Hakamada K, Narumi S. et al. A case of invasive hemolymphangioma of the pancreas. World J Gastroenterol. 2008;14:2932–2934. doi: 10.3748/wjg.14.2932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kosmidis I, Vlachou M, Koutroufinis A, Filiopoulos K. Hemolymphangioma of the lower extremities in children: two case reports. J Orthop Surg Res. 2010;5:56. doi: 10.1186/1749-799X-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu RL, Li H. Giant cystic hemolymphangioma of the postmediastinum. Thorac Cancer. 2010;1:175–177. doi: 10.1111/j.1759-7714.2010.00030.x. [DOI] [PubMed] [Google Scholar]
- 6.Nataf P, Mestiri T, Martinde LE. et al. Pericardial hemolymphangioma. Apropos of a case. Arch Mal Coeur Vaiss. 1988;81:1137–1140. (In French) [PubMed] [Google Scholar]
- 7.Fimmanò A, Coppola BE, Cirillo C. Hemolymphangioma of the toungue: case report. Chirurgia. 2005;18:53–56. (In Italian) [Google Scholar]
- 8.Chanfi M. Hemolymphangioma of the orbit in a young girl: a clinical observation. J Fr Ophtalmol. 2004;27:1047–1049. doi: 10.1016/s0181-5512(04)96263-8. (In French) [DOI] [PubMed] [Google Scholar]
- 9.Canavese F, Cortese MG, Proietti L, Costantino S. Bulky-pedunculated hemolymphangioma of the esophagus: rare case in a two-years old girl. Eur J Pediatr Surg. 1996;6:170–172. doi: 10.1055/s-2008-1066499. [DOI] [PubMed] [Google Scholar]
- 10.Kanaitsuka T, Itani K, Shigeta H. et al. A case report of giant retroperitoneal hemolymphangioma. Nippon Naika Gakkai Zasshi. 1987;76:1595–1603. doi: 10.2169/naika.76.1595. (In Japanese) [DOI] [PubMed] [Google Scholar]
- 11.Gossot D, Decazes JM, Sarfati E, Dubost C. Cystic hemolymphangioma of the adrenal gland. J Chir (Paris) 1987;124:404–405. (In French) [PubMed] [Google Scholar]
- 12.Gaillard de Collogny L, Delage J. Cervical hemolymphangioma in a young patient. J Fr Otorhinolaryngol Audiophonol Chir Maxillofac. 1981;30:469–473. (In French) [PubMed] [Google Scholar]
- 13.Sztaba R, Vondrat W. Thoracic hemolymphangioma with chylothorax in a newborn infant. Ann Chir Infant. 1965;6:21–26. (In French) [PubMed] [Google Scholar]
- 14.Daudet M. Reflections apropos of a case of hepatic hemolymphangioma of the infant. Pediatrie. 1965;20:445–451. (In French) [PubMed] [Google Scholar]
- 15.Scaltriti F, Manenti A. Hemolymphangioma of the lower pole of the spleen (migrated into the pelvis minor). Chir Ital. 1967;19:543–554. (In Italian) [PubMed] [Google Scholar]
- 16.Zhou X, Chen MH, Luo Y, Huang Q, Lu Z. A case of generalized skin lymphatic venous malformation. J Pract Dermatol. 2009;2:120–122. (In Chinese) [Google Scholar]
- 17.Qi XM, Lv CL, Huang CL. Dumbbell-shaped hemolymphangioma of the throat: a case report. J Clin Otorhinolaryngol. 2005;3:111. (In Chinese) [Google Scholar]
- 18.Qi R. A giant hemolymphangioma in the lesser curvature of stomach. J Abdom Sur. 1996;2:78. [Google Scholar]
- 19.Lu YY, Zhan AL. Imaging diagnosis of CT and MRI on hemolymphangioma. Chinese J CT MRI. 2010;8:51–53. [Google Scholar]
- 20.Landing BH, Farber S, editors. Atlas of Tumor Pathology. Armed Forces Institute of Pathology; Washington DC: 1956. Tumors of the cardiovascular system; pp. 124–138. [Google Scholar]