Abstract
Purpose of the study
Problem-solving therapy (PST) has been found effective when delivered to informal caregivers of patients with various conditions. In hospice, however, its translation to practice is impeded by the increased resources needed for its delivery. The study purpose was to compare the effectiveness of a PST intervention delivered face-to-face with one delivered via videophone to hospice primary caregivers.
Design and methods
The study design was a randomized noninferiority trial with two groups, Group 1 in which caregivers received PST face-to-face, and Group 2 in which caregivers received PST via videophone. Family hospice caregivers were recruited from two urban hospice agencies and received the PST intervention (in three visits for Group 1 or three video-calls in Group 2) in an approximate period of 20 days after hospice admission. Standard caregiver demographic data were collected. Psychometric instruments administered to caregivers at baseline and at study completion included the CQLI-R (Caregiver Quality of Life Index–Revised), the STAI (State-Trait Anxiety Inventory), and the PSI (Problem-Solving Inventory).
Results
One hundred twenty-six caregivers were recruited in the study; 77 were randomly assigned to Group 1 and 49 to Group 2. PST delivered via video was not inferior to face-to-face delivery. The observed changes in scores were similar for each group. Caregiver quality of life improved and state anxiety decreased under both conditions.
Conclusions
The delivery of PST via videophone was not inferior to face-to-face. Audiovisual feedback captured by technology may be sufficient, providing a solution to the geographic barriers that often inhibit the delivery of these types of interventions to older adults in hospice.
Introduction
Hospice services aim to provide comfort and dignity to patients at the end of life as well as provide support to their caregivers. Of the 1.56 million patients who received hospice care last year in the United States, 83% were age 65 or older,1 making this a particularly salient concern for older adults and their caregivers.
In hospice care spouses, family members, or others who take care of a patient with a terminal illness play an essential role. Although they are often referred to as informal caregivers, they are the primary caregivers and face immediate challenges when they accept that role and responsibility for their loved one, performing nursing tasks and dealing with emotional problems while also witnessing their loved one's dying process.2
Given the extent of responsibilities, informal caregivers are at a higher risk for deteriorating physical health, depression, financial challenges, and premature death than demographically similar noncaregivers.3,4 Such health and psychological risks are compounded as caregivers tend to sacrifice their own health needs as they struggle with caregiving challenges.5 Caregiving stress can have a significant impact, as mortality risk is found to be significantly higher in elderly caregivers who are experiencing distress compared with those who are providing care but do not feel stressed.6 Even though the challenges and needs of hospice informal caregivers are well documented, there are very few interventions designed specifically for this population.7
One cognitive-behavioral intervention that can assist with coping and problem-solving for informal caregivers in hospice is problem-solving therapy (PST). PST is defined as “the self-directed cognitive-behavioral process by which a person attempts to identify or discover effective or adaptive solutions for specific problems encountered in everyday living.”8 This process highlights various potentially effective solutions for a given problem and facilitates the selection of the most effective solution.9 A problem is defined as any present or anticipated life situation or task that requires a timely response for adaptive functioning, even though “no effective response is immediately apparent or available to the person due to the presence of one or more obstacles.”9 D'Zurilla and Nezu8 developed the relational/problem-solving conceptual framework that defines stress as a function of the reciprocal relations among stressful life events, emotional stress responses, and problem solving/coping. The actual PST approach is summarized by the acronym ADAPT, which includes the following steps: A=Attitude (adopt a positive, optimistic attitude); D=Define (define the problem by obtaining facts, identifying obstacles, and specifying realistic goals); A=Alternatives (generate alternatives for overcoming the identified obstacles and achieving goals); P=Predict (predict positive and negative consequences of each alternative and select the one with the highest probability of success); T=Try Out (implement the solution in real life and monitor its effects).8
PST has been found effective when delivered to informal caregivers of patients with various conditions including physical or cognitive impairment,10 dementia,11 and traumatic brain injury.12 Specifically in hospice, a coping skills nursing intervention labeled COPE based on PST principles was developed and tested, and was found to have the potential to improve quality of life for caregivers of hospice cancer patients.13 In a previous pilot study, we found that PST impacts caregiver quality of life, problem-solving ability, and caregiver anxiety.14
However, one of the barriers to adoption of PST in hospice practice pertains to the increased resources it requires, particularly the number of increased visits by clinicians and associated travel costs. The need for additional resources partially explains the review results by Northouse and colleagues15 that demonstrate very few, if any, evidence-based caregiver interventions have been translated to or implemented in practice settings. In their meta-analysis the investigators concluded that there is a need for the exploration of technology as a cost-effective mode of intervention delivery.15
Hospice agencies aim to improve the quality of their services in spite of limited resources; innovative technology-based tools can provide efficient ways to bridge geographic distance and expand services provided to families. Telehealth tools, such as videophones that allow for audiovisual feedback during psychoeducational interventions and bridge geographic distance, have shown promise in supporting hospice caregivers.16 Traditional audio-only communication (e.g., the telephone) prevents nonverbal interaction and can cause communication difficulties.17 Unable to capture nonverbal behaviors, telephone communication is not a promising candidate as a delivery mechanism for psychosocial assessments and interventions such as PST. Videophone technology, on the other hand, has been shown to capture critical, nonverbal communication necessary for assessment and is therefore a logical choice as an alternative delivery method for cognitive-behavioral interventions.18 To date, published work has not reported whether the use of a video platform can facilitate or impede the delivery of a cognitive-behavioral intervention. If the video platform is as effective as the face-to-face delivery, it may introduce new cost-effective approaches for hospice agencies to deliver additional support to caregivers in both urban and rural areas.
The purpose of this study was to compare the effectiveness of a PST intervention delivered face –to-face with one delivered via videophone to hospice informal caregivers. We hypothesized that caregivers in the video-based group would report similar (not inferior) levels of post-intervention quality of life, problem-solving ability, and anxiety as compared with caregivers in the face-to-face group.
Design and Methods
The study design was a randomized noninferiority trial with two groups (Group 1 in which caregivers received PST face-to-face, and Group 2 in which caregivers received PST via videophone). Informal caregivers whose loved one was receiving home hospice care from our participating hospice agencies were enrolled in the study. These agencies are located in an urban setting in the Pacific Northwest, and were both Medicare and Medicaid certified. Total home admissions per year were 2619 for Hospice Agency A, and 1325 for Hospice Agency B, with an average daily census of 510 and 189, respectively, and with average length of stay of 65.2 days for Agency A and 59 for Agency B.
Caregivers referred to the study met the following criteria: (1) enrolled as a family/informal caregiver of a hospice patient; (2) 18 years or older; (3) at least sixth-grade education; (4) no or only mild cognitive impairment (assessed using the Short Portable Mental Status Questionnaire;19 individuals with a score <7 were excluded); and (5) without functional hearing loss or with a hearing aid that allows the participant to conduct telephone conversations as assessed by the research staff (by questioning and observing the caregiver). Additionally, caregivers needed to have access to a standard telephone line at home.
The hospice admissions staff presented the research opportunity to caregivers upon admission, asking if they would agree to be contacted by the research staff to hear more about the study. The admissions staff forwarded contact information for willing caregivers. The interventionist called and scheduled the initial visit where the project was discussed, informed consent was obtained, and demographic data were collected. A systematic review of PST for adults reveals that most studies use registered nurses and social workers as interventionists.20 For our study, interventionists were registered nurses and social workers (M.S.W.) (with hospice experience) who underwent training in PST for a total of 25 hours.
The interventionist then opened a numbered sealed envelope, prepared in advance, containing group assignment. We pursued simple (nonrestricted) randomization to preserve complete unpredictability of each intervention assignment. This randomization minimizes bias but can yield disparate sample sizes in the groups by chance alone.
Caregivers were asked to review and prioritize common caregiver concerns using a problem checklist identifying up to three problems they wanted to work on, including any problems or concerns that they identified that may not have been part of the list. Before departing, the interventionist tentatively scheduled the first face-to-face or videophone session (depending on group assignment) with the caregiver. Based on the experience of a small pilot study14 a total of three intervention visits/video-calls were made with a suggested timeline between days 5 and 18 of the hospice admission. This timeline was calculated based on average length of stay for our participating hospice agencies and also nationally, as well as on the PST recommendations. Each intervention visit or video-call lasted approximately 45 minutes. If the caregiver was assigned to the video group (Group 2), the interventionist installed the videophone at the initial visit.
The videophone was the Beamer Videophone (Vialta, Inc., CA) which operates over regular telephone lines. This model was found during our preliminary work to be user-friendly for adult users over the age of 65 years. The Beamer Videophone plugs into a regular telephone and does not interfere with its use. Only if both parties have a videophone and both parties consent to a video-call (by pressing the video button) is a video-call possible.
The agenda for the first intervention visit for caregivers, regardless of modality (face-to-face or videophone), included an explanation of the purpose of the visit/call, and confirmation of the three specific problems that the caregiver had selected from the initial visit concern list. Caregivers' Problem-Solving Inventory (PSI) scores (based on a survey described below) and subscales indicated their problem-solving style (positive problem orientation, negative problem orientation, rational problem-solving, impulsivity/carelessness, and avoidance) and allowed the interventionist to customize the delivery of the intervention. During the first visit, the interventionist also worked on steps one and two of the ADAPT model of the PST, namely “Attitude” and “Defining the Problem and Setting Realistic Goals.” For the first step the focus is on realistic optimism, that is, acceptance that problems are a normal part of life. This step focuses on promoting visualizing successful problem-solving, healthy thinking rules, positive self-talk, and using emotions adaptively. Problems identified by the caregiver were used as examples for exercises and to brainstorm about applying different approaches. The second step of defining the problem focuses on enabling caregivers to seek available facts, describe facts in a clear language, separate facts from assumptions, set realistic goals, and identify obstacles to overcome.
During the second intervention visit (suggested timeline: 11 to 13 days after hospice admission) the interventionist covered steps three and four of the ADAPT model. Step three encourages caregivers in being creative and generating alternative solutions. Step four focuses on predicting the consequences and developing a solution plan. This step involves evaluating alternatives and choosing the one that is most likely to effectively solve the identified problem.
The third visit (suggested timeline: 16 to 18 days after hospice admission) focused on step five, namely trying out the solution plan and determining if it works. The general goal is to systematically evaluate the solution that caregivers implemented as a result of the previous steps to determine if it was effective in solving (or improving) the identified problem.
Finally, all caregivers received a face-to-face exit interview a few days after the last intervention visit. Caregivers were interviewed about their perceptions of the problem-solving intervention and potential benefits or concerns associated with the video delivery (Group 2). During exit interview visits to the caregivers in Group 2 the interventionist removed the videophone. Caregivers in both groups received a $50 gift card as a token of appreciation for their participation. If the patient died before all three intervention visits were completed, the intervention was either stopped due to the patient's death or continued if the caregiver explicitly stated that they wished to continue (as an addition to the standard bereavement services of the hospice agency).
Treatment fidelity
To ensure treatment fidelity to the PST intervention, we used a training and treatment fidelity manual. The guide detailed the training of research staff (two interventionists), the nature of each of the three intervention visits, and the protocol for administering each of the evaluative instruments. All face-to-face visits (for subjects in intervention Group 1) and all video-calls (for subjects in intervention Group 2) were audio-recorded by the research staff, and a randomly chosen sample of 10% of all recordings was studied to ensure the integrity of the intervention protocol. Recordings were independently rated by two members of the research team (GD, DPO) for overall adherence to the protocol and inclusion of all required elements, as well as to confirm that no contamination took place (e.g., a case where the interventionist provided specific advice for a problem without allowing the caregiver to review and select an option). Our intervention monitoring tools were refined based on recommendations by Radziewicz and coworkers21 to help assure fidelity in individualized intervention studies.
Measures
Standard demographic data were collected from caregivers during the initial visit, including age, gender, ethnicity, race, education level, marital status, occupation, and diagnosis of patient.
The following psychometric instruments were administered at the initial and last visits:
Caregiver Quality of Life Index–Revised (CQLI-R)
The CQLI-R includes four dimensions: emotional, social, financial, and physical.22 This four-item instrument was designed specifically for hospice caregivers, and its reliability and validity have been established.22 Our research team has revised the CQLI instrument for use in oral interviews using 0 and 10 for each of the four anchors in place of the visual analog scale and validated with hospice caregivers.23
The State-Trait Anxiety Inventory (STAI)
The STAI is a self-report assessment instrument that includes separate measures of state and trait anxiety. The present study specifically investigated state anxiety, defined as a "transitory emotional state or condition of the human organism that is characterized by subjective, consciously perceived feelings of tension and apprehension, and heightened autonomic nervous system activity.”24
Problem-Solving Inventory (PSI)
The PSI is a 35-item Likert-type inventory that assesses problem-solving appraisal, or an individual's perceptions of their problem-solving behavior and attitudes.25 Five subscales measure problem-solving style (positive, rational, negative, impulsive, and avoidant problem-solving attitudes).
Statistical analysis
Linear mixed modeling was used to estimate the intervention effect: the average change in a measure before and after the intervention. In a linear mixed model all participants contribute to estimating of the intervention effect—even if they are missing follow-up measures. Linear mixed models and analysis of covariance (ANCOVA) were both used to estimate differences in treatment effects. ANCOVA is a complete case analysis, excluding all participants with missing data. To test for noninferiority of videophone delivery, we first established a minimally significant clinical effect. These were defined a priori as a 10% adverse change in a given measure. Furthermore, we assumed inferiority (video is clinically significantly less effective than face-to-face) and if the 90% confidence interval (CI) for the difference between video and face-to-face did not contain the minimally significant effect, we rejected the null hypothesis and accepted the video intervention as noninferior to the face-to-face intervention at the 95% confidence level.
Results
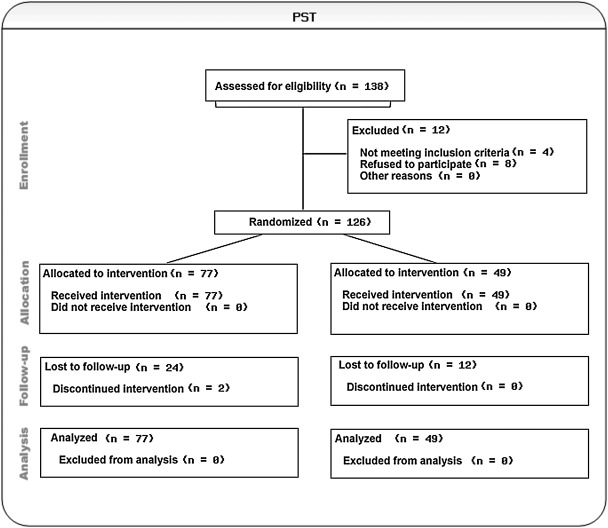
A total of 138 caregivers referred to our research team by the participating hospice agencies were contacted by phone to assess their eligibility and interest in the study. Eight caregivers chose not to participate citing lack of time or interest and/or anticipated travel responsibilities, and four caregivers were not eligible to participate (one was a paid/professional caregiver rather than an informal one, and for three the patient had died prior to being contacted). The remaining 126 caregivers were recruited in the study following a block randomization approach; 77 were randomly assigned to the face-to-face group (Group 1) and 49 to the video group (Group 2). Each caregiver was the primary caregiver of a patient (we did not recruit more than one caregiver of the same patient). Of all 126 caregivers, 89 caregivers (71%) completed the full study protocol, whereas 38 caregivers did not complete all intervention steps (36 participated until their patient died before study completion and 2 voluntarily withdrew). Figure 1 illustrates subject enrollment and study flow.
FIG. 1.
Flow diagram of subject enrollment and participation.
In terms of caregivers' education, the majority had some college education or higher. In terms of ethnic and racial representation, the vast majority were non-Hispanic Caucasian. Table 1 lists subjects' demographic characteristics. Fifty-nine caregivers were adult children of a hospice patients, 38 were taking care of a spouse/partner, 4 of a sibling, and 4 of a grandparent, whereas 5 were parents of an adult hospice patient and 16 identified their relationship to the patient as “other.” Sixty-eight caregivers resided with the patients, and in the remaining 58 cases, the patients resided elsewhere (such as a group home or nursing home). At baseline, no significant differences were observed between groups in terms of their age and sex or baseline assessments (see Table 2).
Table 1.
Subject Characteristics
| |
Total |
Face-to-face |
Video |
|---|---|---|---|
| N | 126 | 77 | 49 |
| Education | |||
| High school | 17 | 10 | 7 |
| Some college | 39 | 22 | 17 |
| College degree | 50 | 31 | 19 |
| Professional diploma | 4 | 1 | 3 |
| Master's degree | 12 | 7 | 5 |
| Doctorate degree | 4 | 2 | 2 |
| Race | |||
| African American | 6 | 4 | 2 |
| Asian American | 7 | 3 | 4 |
| Native Hawaian/Pacific Islander | 2 | 0 | 2 |
| American Indian | 1 | 1 | 0 |
| Caucasian | 110 | 69 | 41 |
| Ethnicity | |||
| Hispanic | 3 | 2 | 1 |
| Non-Hispanic | 123 | 75 | 48 |
Table 2.
Baseline Mean Values and Comparison between Groups
| Face-to-face | Video | P value | |
|---|---|---|---|
| % Female | 71.4 | 79.6 | 0.31 |
| Age | 59.5 | 59.7 | 0.94 |
| CQLI-R total | 28.6 | 29.0 | 0.71 |
| STAI total score | 40.0 | 40.3 | 0.87 |
| PSI-Positive | 19.5 | 18.9 | 0.27 |
| PSI-Rational | 18.7 | 18.5 | 0.75 |
| PSI-Negative | 11.8 | 11.7 | 0.95 |
| PSI-Impulsive | 11.8 | 11.2 | 0.25 |
| PSI-Avoidant | 12.2 | 11.4 | 0.21 |
CQLI-R, Caregiver Quality of Life Index–Revised; PSI, Problem-Solving Inventory; STAI, State-Trait Anxiety Inventory.
As hypothesized, problem-solving therapy delivered via video was not inferior to face-to-face delivery. The observed changes in scores were similar for each group and in the expected direction of the scale. Caregiver quality of life improved and state anxiety decreased under both conditions (see Table 3 for aggregate estimates of the effects of the intervention).
Table 3.
Aggregate Estimates of the Intervention Effects (Both Groups)
| Outcome | Post–Prea | P value |
|---|---|---|
| CQLI-R total | 0.7 (−0.17, 1.57) | 0.1902 |
| STAI total score | −5.82(−7.38, −4.26) | <0.0001 |
| PSI-Positive | 1.19 (0.66, 1.73) | 0.0004 |
| PSI-Rational | 0.7 (0.05, 1.35) | 0.0781 |
| PSI-Negative | −1.14 (−1.74, −0.54) | 0.0024 |
| PSI-Impulsive | −0.35 (−0.84, 0.14) | 0.2449 |
| PSI-Avoidant | −1.05 (−1.6, −0.49) | 0.0026 |
Difference adjusted for age and sex.
CQLI-R, Caregiver Quality of Life Index–Revised; PSI, Problem-Solving Inventory; STAI, State-Trait Anxiety Inventory.
State anxiety was the mostly affected by the intervention. Additionally, the positive, rational, negative, and avoidant subscales of the PSI were all more significant than caregiver quality of life. Both group analyses were similar to aggregate analysis of intervention effects. The intervention effect on the rational PSI subscale did not appear in the face-to-face group (see Table 4).
Table 4.
Intervention Impact by Group
| |
Face-to-face |
Video |
||
|---|---|---|---|---|
| Outcome | Post–Prea | P value | Post–Prea | P value |
| CQLI-R total | 0.86 (−0.18, 1.91) | 0.1803 | 0.26 (−1.23, 1.74) | 0.7755 |
| STAI total score | −4.4 (−6.38, −2.43) | 0.0006 | −7.71 (−10.13, −5.3) | <0.0001 |
| PSI-Positive | 0.7 (0.06, 1.34) | 0.0784 | 1.91 (1, 2.81) | 0.0015 |
| PSI-Rational | 0.21 (−0.64, 1.06) | 0.6872 | 1.41 (0.42, 2.39) | 0.0249 |
| PSI-Negative | −1.18 (−1.84, −0.52) | 0.005 | −1.09 (−2.25, 0.07) | 0.1317 |
| PSI-Impulsive | −0.36 (−1.03, 0.3) | 0.3716 | −0.2 (−0.92, 0.52) | 0.6539 |
| PSI-Avoidant | −0.85 (−1.47, −0.22) | 0.0298 | −1.33 (−2.36, −0.31) | 0.0399 |
Difference adjusted for age and sex.
CQLI-R, Caregiver Quality of Life Index–Revised; PSI, Problem-Solving Inventory; STAI, State-Trait Anxiety Inventory.
No significant differences in the effect of the intervention were observed for any of the outcomes except state anxiety (see Table 5a). In Table 5a only participants with both baseline and follow-up measures contribute to the estimation of the effect. For Table 5b all participants are included in the linear mixed model and thus contribute directly or indirectly to the estimated differences in the intervention effects. For CQLI-R and STAI, the video intervention was not inferior to the face-to-face intervention (see Table 5b). A population average CQLI-R score for participants in the video intervention group is no more than 2.21 points lower than the average score among caregivers receiving the face-to-face intervention at the 95% confidence level. Similarly, the true mean STAI score for participants receiving the video-based intervention is no more than 0.43 points higher than among those receiving the intervention face-to-face at the 95% confidence level (see Table 5b).
Table 5a.
ANCOVA Analysis
| Outcome | Video–Face-to-face (95% CI) | P value |
|---|---|---|
| CQLI-R total | −0.54 (−2.47, 1.39) | 0.58 |
| STAI total score | −2.94 (−5.68, −0.2) | 0.04 |
| PSI-Positive | 0.8 (−0.31, 1.91) | 0.16 |
| PSI-Rational | 1.15 (−0.33, 2.62) | 0.13 |
| PSI-Negative | 0.14 (−1.1, 1.38) | 0.83 |
| PSI-Impulsive | −0.2 (−1.38, 0.99) | 0.75 |
| PSI-Avoidant | −0.88 (−2.09, 0.33) | 0.16 |
Differences between video and face-to-face intervention groups adjusted for baseline scores (only participants with both baseline and follow-up measures contribute to the estimation of the effect).
ANCOVA, analysis of covariance; CQLI-R, Caregiver Quality of Life Index–Revised; PSI, Problem-Solving Inventory; STAI, State-Trait Anxiety Inventory.
Table 5b.
Linear Mixed Model Results
| Outcome | Video–Face-to-face | 90% CI | Minimum significant clinical effect | Reject null hypothesis of inferiority? |
|---|---|---|---|---|
| CQLI-R total | −0.52 | (minus;2.21, 1.18) | −4 | Yes |
| STAI total score | −3.28 | (minus;6.14, −0.43) | +6 | Yes |
| PSI-Positive | 0.91 | (minus;0.06, 1.88) | −2 | Yes |
| PSI-Rational | 1.2 | (minus;0.01, 2.41) | −2 | Yes |
| PSI-Negative | −0.04 | (minus;1.18, 1.09) | +2 | Yes |
| PSI-Impulsive | −0.22 | (minus;1.13, 0.7) | +2 | Yes |
| PSI-Avoidant | −0.92 | (minus;1.97, 0.13) | +2 | Yes |
Differences between video and face-to-face intervention adjusted for age and gender. The 90% confidence intervals (CIs) establish noninferiority at the 95% confidence level (all participants are included in the linear mixed model and thus contribute directly or indirectly to the estimated differences in the intervention effects).
CQLI-R, Caregiver Quality of Life Index–Revised; PSI, Problem-Solving Inventory; STAI, State-Trait Anxiety Inventory.
Discussion
The delivery of PST via videophone was not inferior to face-to-face delivery. Nonverbal communication essential to the delivery of a cognitive-behavioral intervention was not inhibited by the use of technology. The modality findings of this study suggest that audiovisual feedback captured by technology is sufficient, providing a solution to the geographic barriers that often inhibit the delivery of these types of interventions. Although this study was conducted in a hospice setting, it provides evidence for relative effectiveness in other health care settings.
This study also found that the intervention delivered in both modalities is associated with improvement in caregiver quality of life and problem-solving ability and reduction of anxiety. Therefore, it holds promise as an intervention that may support caregivers during their hospice experience and enable them to cope with the physical and emotional challenges of caregiving. As the video platform is found to be as effective as the face-to face-delivery, this study provides evidence for the further development of technologically enhanced, cost-effective services to support caregivers.
Subject recruitment for palliative care research is challenging due to several factors, including short length of stay, complicated inclusion criteria, and perceived study burden.26,27 Once we established the mechanisms to obtain and screen referrals in this trial, recruitment was successful as 91% of all referred caregivers who were contacted by the interventionist enrolled in the study. We minimized perceived study burden and used only caregiver measures that were found in previous studies to be affected by coping skills or problem-solving interventions, and limited to obtaining essential information. The timeline of the intervention for both groups was designed based on the average length of stay of the participating agencies. The inclusion criteria for this study were intentionally broad to include the largest possible number of caregivers. This study allowed us to test and finalize the PST intervention manual and fidelity protocol, which can facilitate the translation of the intervention in practice. As in many palliative care studies our attrition rate was significant as only 73% of enrolled caregivers completed all phases of the study (with most caregivers completing only portions of the intervention primarily due to the death of the patient).
There are limitations associated with the use of an equivalence or noninferiority trial design that does not incorporate a traditional control group. Without a control group, time effects potentially confound this study's estimates of the effects of intervention. For instance, state anxiety was assessed at time of enrollment in hospice and might be expected to be lower at follow-up even without the intervention. Thus, related to the implicit lack of measures of internal validity (in contrast to superiority trials), we can only estimate the relative difference between the two deliveries of the interventions, rendering external validation necessary to provide evidence for efficacy of either version of the intervention. Validation requires a protocol that is loyal to the one used to show a significant difference between one of the interventions and a control group. In our case, we adopted the study protocol, primary variables, manual, instruments, eligibility criteria, conditions, and frequency of intervention used in other studies of PST and our pilot work with the PST delivery in hospice. However, there is a need for a larger controlled trial testing the intervention delivered via both modalities (face-to-face and video) against a control population (where the same pre-post assessment occurs without the delivery of the PST intervention).
Reliance on regular telephone lines for the operation of the videophones was a potential limitation, given the recent trend toward abandoning landline telephones in US households.28 We chose to use analog videophones that operate over regular phone lines because the majority of the U.S. population continues to have landlines, and the necessary infrastructure to support Internet or cellular phones has substantial geographic variation in addition to higher implementation and operation costs. The use of analog videophones reduces the intervention cost, which could be important in adoption decisions by hospice agencies. However, recent technological advances and the diffusion of the Internet introduce new opportunities for the delivery of the PST intervention using Internet-based videoconferencing solutions that can be low cost and would not require training if caregivers already have access to such resources.
Additionally, two large hospice agencies within one urban setting were used for recruitment. Obviously a multi-site design that combines urban and rural settings would have strengthened our study and increased the generalizability of our findings. Finally, the lack of racial diversity in our sample is a limitation. It is well documented that hospice care is underutilized by minorities and the vast majority of hospice clients are Caucasian. This was also reflected in our sample size, with only 13% of all subjects being non-Caucasian (which is in accordance with the national hospice statistics, which estimate that only 19% of hospice patients in 2009 in the US were non-Caucasian.1
Our study highlighted the potential of low-cost innovative tools to enhance hospice and palliative care for families. Although not designed to test the efficacy of the intervention, findings demonstrate the potential of this problem-solving intervention for hospice caregivers. After completing the intervention, caregivers in both groups reported lower levels of anxiety, higher levels of quality of life, and improved problem-solving skills. Further research testing the efficacy in a randomized controlled trial is an important next step.
Acknowledgments
This project was funded in part by the National Institutes of Health (NIH) National Institute of Nursing Research Grant Nr. R21 NR010744-01 (A Technology Enhanced Nursing Intervention for Hospice Caregivers, Demiris PI).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.National Hospice and Palliative Care Organization (NHPCO) (2010) Facts, Figures on Hospice Care. 2010. www.nhpco.org/files/public/Statistics_Research/Hospice_Facts_Figures_Oct-2010.pdf. [Nov 1;2011 ]. www.nhpco.org/files/public/Statistics_Research/Hospice_Facts_Figures_Oct-2010.pdf
- 2.Pinquart M. Sorensen S. Differences between caregivers and noncaregivers in psychological health: A meta-analysis. Psychol Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- 3.Dean M. A law that would care for carers. Lancet. 1995;345:1101. doi: 10.1016/s0140-6736(95)90827-7. [DOI] [PubMed] [Google Scholar]
- 4.Sherwood PR. Given CW. Given B. von Eye A. Caregiver burden and depressive symptoms: Analysis of common outcomes in caregivers of elderly patients. J Aging Health. 2005;17:125–147. doi: 10.1177/0898264304274179. [DOI] [PubMed] [Google Scholar]
- 5.Schultz R. Newsom J. Mittelmark M. Burton L. Hirsch C. Jackson S. Health Effects of Caregiving: the Caregiver Health Effects Study. An ancillary study of the Cardiovascular Health Effects Study. Ann Behav Med. 1997;19:110–116. doi: 10.1007/BF02883327. [DOI] [PubMed] [Google Scholar]
- 6.Schulz R. Beach SR. Caregiving as a risk factor for mortality. The Caregiver Health Effects Study. JAMA. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 7.Harding R. Higginson IJ. What is the best way to help caregivers in cancer palliative care? A systematic literature review of interventions and their effectiveness. Palliat Med. 2003;17:63–74. doi: 10.1191/0269216303pm667oa. [DOI] [PubMed] [Google Scholar]
- 8.D'Zurilla TJ. Nezu AM. Problem Solving Therapy. A Positive Approach to Clinical Intervention. 3rd. New York: Springer Publishing Company; 2007. [Google Scholar]
- 9.D'Zurilla TJ. Goldfried MR. Problem solving and behavior modification. J Abnorm Psychol. 1971;78:107–126. doi: 10.1037/h0031360. [DOI] [PubMed] [Google Scholar]
- 10.Gallagher-Thompson D. Lovett S. Rose J. McKibbin C. Coon D. Futterman A. Thompson LW. Impact of psychoeducational interventions on distressed caregivers. J Clin Geropsychology. 2000;6:91–110. [Google Scholar]
- 11.Roberts J. Browne G. Milne C. Spooner L. Gafni A. Drummon-Youn M. LeGris J. Watt S. LeClair K. Beaumont L. Roberts J. Problem solving counseling for caregivers of the cognitively impaired: Effective for whom? Nurs Res. 1999;48:162–172. doi: 10.1097/00006199-199905000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Wade SL. Wolfe C. Brown TM. Pestian JP. Putting the pieces together: Preliminary efficacy of a web-based family intervention for children with TBI. J Pediatr Psychol. 2005;30:437–442. doi: 10.1093/jpepsy/jsi067. [DOI] [PubMed] [Google Scholar]
- 13.McMillan SC. Small BJ. Weitzner M. Schonwetter R. Tittle M. Moody L. Haley WE. Impact of coping skills intervention with family caregivers of hospice patients with cancer: A randomized clinical trial. Cancer. 2006;106:214–222. doi: 10.1002/cncr.21567. [DOI] [PubMed] [Google Scholar]
- 14.Demiris G. Parker Oliver D. Washington K. Thomas Fruehling L. Haggarty-Robbins D. Doorenbos A. Wechkin H. Berry D. a problem solving intervention for hospice caregivers: A pilot study. J Palliat Med. 2010;13:1005–1011. doi: 10.1089/jpm.2010.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Northouse LL. Katapodi MC. Song L. Zhnag L. Wood DW. Interventions with family caregivers of cancer patients. Meta-analysis of randomized trials. CA Cancer J Clin. 2010;60:317–339. doi: 10.3322/caac.20081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parker Oliver D. Demiris G. Comparing face-to-face and telehealth-mediated delivery of a psychoeducational intervention: A case comparison study in hospice. Telemed J e-Health. 2010;16:751–753. doi: 10.1089/tmj.2010.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wadhwa A. Lingard L. A qualitative study examining tensions in interdoctor telephone consultations. Med Educ. 2006;40:759–767. doi: 10.1111/j.1365-2929.2006.02534.x. [DOI] [PubMed] [Google Scholar]
- 18.Demiris G. Parker Oliver DR. Courtney K. A study of the suitability of videophones for psychometric assessment. Behav Inf Technol. 2006;25:233–237. [Google Scholar]
- 19.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 20.Gellis ZD. Kenaley B. Problem solving therapy for depression in adults: A Systematic review. Res Soc Work Pract. 2008;18:117–131. [Google Scholar]
- 21.Radziewicz R. Rose JH. Bowman K. Berila RA. O'Toole E. Given B. Establishing treatment fidelity in a coping and communication support telephone intervention for aging patients with advanced cancer and their family caregivers. Cancer Nurs. 2009;32:193–202. doi: 10.1097/NCC.0b013e31819b5abe. [DOI] [PubMed] [Google Scholar]
- 22.McMillan SC. Mahon M. The impact of hospice services on the quality of life of primary caregivers. Oncol Nurs Forum. 1994;21:1189–1195. [PubMed] [Google Scholar]
- 23.Courtney KL. Demiris G. Parker Oliver D. Porock D. Conversion of the CQLI to an interview instrument. Eur J Cancer Care. 2005;14:463–464. doi: 10.1111/j.1365-2354.2005.00612.x. [DOI] [PubMed] [Google Scholar]
- 24.Spielberger CD. Gorsuch RL. Lushene RE. Manual for the State-Trait Anxiety Inventory (Self Evaluation Questionaire) Palo Alto, CA: Consulting Psychologist Press; [Google Scholar]
- 25.Heppner PP. Petersen CH. The development and implications of a personal problem solving inventory. J Counsel Psychol. 1982;29:66–75. [Google Scholar]
- 26.McMillan SC. Weitzner MA. Methodologic issues in collecting data from debilitated patients with cancer near the end of life. Oncol Nurs Forum. 2003;30:123–129. doi: 10.1188/03.ONF.123-129. [DOI] [PubMed] [Google Scholar]
- 27.Ransom S. Azzarello LM. McMillan SC. Methodological issues in the recruitment of cancer pain patients and their caregivers. Res Nurs Health. 2006;29:190–198. doi: 10.1002/nur.20129. [DOI] [PubMed] [Google Scholar]
- 28.Pew Research Center. The Cell Phone Challenge to Polling. 2010. http://pewresearch.org/reports/?ReportID=22. [Nov 1;2011 ]. http://pewresearch.org/reports/?ReportID=22