Abstract
Back ground and Purpose:
Hamstring injury is a common occurrence in sport and there has been limited success in reducing this rate of recurrence to date.
Description of Topic with Related Evidence:
High speed running requires eccentric strength when the hamstring muscles are in a lengthened state. The lengthened state occurs when the hip is in flexion and the lower leg moves into extension, thus lengthening the two joint hamstring muscle over both articulations upon which they act. There is evidence to suggest that athletes who have sustained a hamstring strain lack strength when the muscle is utilized during performance in a lengthened state.
Purpose:
To examine the risk factors contributing to such a high recurrence rate and propose a unique rehabilitation strategy addressing these factors in order to decrease the rate of reinjury.
Discussion/Relation to Clinical Practice:
Failing to increase an athlete's eccentric strength in a lengthened position after a hamstring injury may predispose an athlete to subsequent reinjury. Incorporating lengthened state eccentric training may help reduce the rate of reinjury.
Level of Evidence:
Level 5
Keywords: Hamstring strain, lengthened state eccentrics
BACKGROUND AND PURPOSE
Hamstring strains are one of the most frequently occurring injuries in sport. They can be challenging and frustrating to treat because of the high recurrence rate. Hamstring strains account for 12–16% of all injuries in athletes1–5 with a reinjury rate reported as high as 22–34%.5–7 Furthermore, recurrent hamstring strains have been shown to result in significantly more time lost than first time hamstring strains.1 In order to decrease this rate we must first examine the potential risk factors for injury and then address them accordingly. While there is a myriad of studies focusing on risk factors for hamstring strains, there is a paucity of high-level evidence with regards to the identification of these risk factors as well as rehabilitation with an emphasis on reducing the risk of reinjury.8 The purpose of this clinical commentary is to examine the risk factors contributing to such a high recurrence rate and propose a unique rehabilitation strategy addressing these factors in order to decrease the rate of reinjury.
RISK FACTORS FOR HAMSTRING STRAINS
Several risk factors for hamstring strains have been proposed in the literature, including: decreased flexibility,9–10 strength deficits,11 muscle fatigue,12 poor core stability,13 lack of proper warm-up,14 poor lumbar posture,15 and a prior hamstring injury.16,17 Previous hamstring injury appears to be the most consistent risk factor for restraining the hamstring. Engebretsen et al17 examined over 500 amateur soccer players prospectively and among all the risk factors examined, previous acute hamstring strain was the strongest risk factor for recurrent strain. In fact, a previous hamstring strain has been shown to increase the risk of a recurrence two to six times.16–18
MECHANISM OF INJURY
Hamstring strains can occur during a variety of athletic maneuvers and situations, resulting in several distinct types of injuries, each with a unique mechanism. The first occurs during a stretching of the muscle at extreme joint positions, such as in a Rockette style high kick.19–20 These injuries generally occur to the proximal free tendon of the semimembranosus tendon and appear to be less severe initially but ultimately require a longer recovery time than hamstrings strained by other mechanisms.21 The second mechanism of hamstring strain occurs during high speed running.1,22 There remains some debate in the literature as to which phase of the sprinting cycle in which hamstring strains occur: the early stance phase or the late swing phase. Proponents of hamstring injury during early stance phase of sprinting suggest it is during this phase in which the muscle absorbs the most force as a result of high ground reaction forces.23 In vivo studies of the Achilles tendon in sprinting24 and patella tendon in jumping25 and hopping26 show that the forces are much higher in the concentric stance phase as opposed to the eccentric swing phase and this may apply to the hamstrings as well. There is also evidence to suggest hamstrings may be susceptible to injury in the late swing phase. Previous studies demonstrate that the hamstrings are under a large amount of stress in the terminal swing phase as the hamstrings eccentrically contract to absorb the kinetic energy and slow the lower limb.27 In a biomechanical study Schache et al28 found that peak musculotendonous strain occurred during terminal swing phase of the sprinting cycle, suggesting that this period may pose the greatest risk for injury. They went on to recommend a rehabilitation program focusing on eccentric loading at longer muscle lengths.
To assess whether a reduction in force production at longer muscle lengths exists in athletes who have sustained a hamstring strain, Brockett et al29 examined the angle torque curves of previously injured subjects and compared them with the subjects' uninvolved leg as well as those of uninjured control subjects. The authors showed that the peak hamstring torque occurred at a significantly shorter muscle length in the previously injured hamstring when compared to controls, indicating what may be termed a shift in the length-tension curve. It is possible that when an athlete sustains a hamstring strain they potentially return to play with weakness at longer muscle lengths possibly predisposing them for a second hamstring strain during the eccentric terminal sprinting movement.
It has been well established in the literature that eccentric training is effective in the prevention of hamstring strains.1,30–33 The authors feel that the eccentric training should be done not just in the seated position from 90 degrees to full knee extension, but should include training in the lengthened state. We hypothesize that training in the lengthened state may help shift the curve to acquire the necessary eccentric strength at the end of the range of motion to avoid susceptibility to further injury. The absence of rehabilitation focusing on lengthened state eccentric training may explain the disproportionally high rate of recurrence. Therefore, it is the belief of the authors that complete rehabilitation of a strained hamstring should include lengthened state eccentric training in order to minimize exposure to further muscle strain. Unfortunately, despite the best prevention programs hamstring strain injuries still occur.
POST INJURY REHABILITATION
Table 1 outlines rehabilitation guidelines for a hamstring strain, with emphasis on lengthened state eccentric training in the latter stages. It is important to consider that these are general guidelines and a rehabilitation program should be custom tailored to address the specific deficits discovered in each athlete during the examination process.
Table 1.
Normalization of Strength/length Curve Protocol.
| Phase 1 |
| Goals |
| 1. Protect healing tissue |
| 2. Minimize atrophy and strength loss |
| 3. Prevent motion loss |
| Protection |
| Avoid excessive active or passive lengthening of the hamstrings |
| Avoid antalgic gait pattern |
| Ice |
| 2–3 times daily |
| Therapeutic exercise (performed daily) |
| 1. Stationary bike |
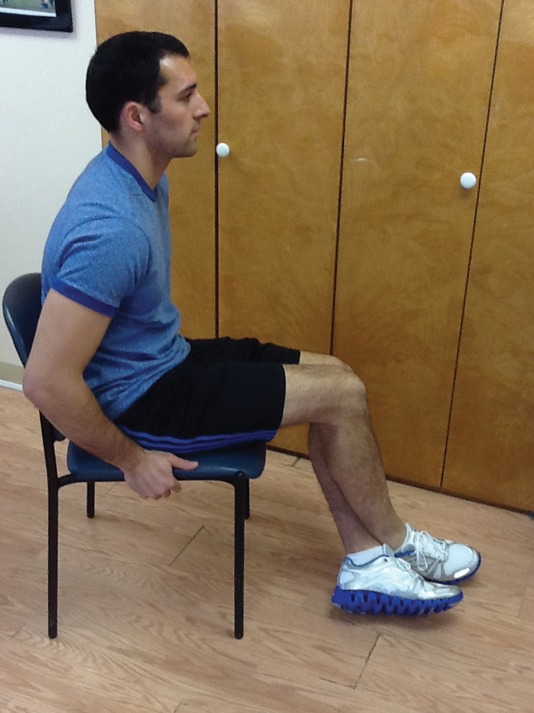
| 2. Sub maximal Isometric at 3 angles (90°, 60°, 30°) (Figure 1) |
| 3. Single leg balance |
| 4. Balance Board |
| 5. Soft tissue mobilization (STM)/Instrument assisted (IASTM) |
| 6. Pulsed Ultrasound (duty cycle 50%, 1 MHz, 1.2 W/cm2) |
| 7. Progressive hip strengthening |
| 8. Painfree isotonic knee flexion |
| 9. Active sciatic nerve flossing |
| 10. Ice with sensory electrical stimulation (e.g. Conventional TENS) |
| Criteria for progression to next phase |
| 1. Normal walking stride without pain |
| 2. Pain-free isometric contraction against submaximal (50%-75%) resistance during prone knee flexion (90°) manual strength test |
| Phase 2 |
| Goals |
| 1. Regain pain-free hamstring strength, progressing through full range |
| 2. Develop neuromuscular control of trunk and pelvis with progressive increase in movement speed preparing for functional movements |
| Protection |
| Avoid end-range lengthening of hamstrings if painful |
| Ice |
| Post-exercise, 10–15 min |
| Therapeutic exercise (performed 5–7 d/wk) |
| 1. Stationary bike |
| 2. Treadmill at moderate to high intensity (progressive increasing intervals), pain-free speed anc stride |
| 3. Isokinetic eccentrics in non-lengthened state |
| 4. Single-limb balance windmill touches without weight |
| 5. Single leg stance with perturbation (eg ball toss, reaches) |
| 6. Supine hamstring curls on swiss ball |
| 7. STM/IASTM |
| 8. Nordic hamstring exercise (Figure 3) |
| 9. Shuttle jumps |
| 10. Prone leg drops |
| 11. Lateral and retro bandwalks |
| 12. Sciatic nerve tensioning |
| Criteria for progression to next phase |
| 1. Full strength (5/5) without pain during prone knee flexion (90°) manual strength test |
| 2. Pain-free forward and backward jog, moderate intensity |
| 3. Strength deficit less than 20% compared against uninjured limb |
| 4. Pain free max eccentric in a non-lengthened state |
| Phase 3 |
| Goals |
| 1. Symptom-free (eg, pain and tightness) during all activities |
| 2. Normal concentric and eccentric hamstring strength through full range of motion and speeds |
| 3. Improve neuromuscular control of trunk and pelvis |
| 4. Integrate postural control into sport-specific movements |
| Protection |
| Train within symptom free intensity |
| Ice |
| Postexercise, 10–15 min, as needed |
| Therapeutic exercise (performed 4–5 d/wk) |
| 1. Treadmill moderate to high intensity as tolerated |
| 2. Hamstring dynamic stretching |
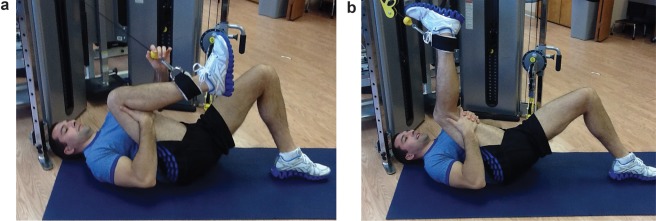
| 3. Isokinetic eccentric training at end ROM (in hyperflexion, see figures 4, 5a, 5b) |
| 4. STM/IASTM |
| 5. Plyometric jump training |
| 6. 5–10 yard accelerations/decelerations |
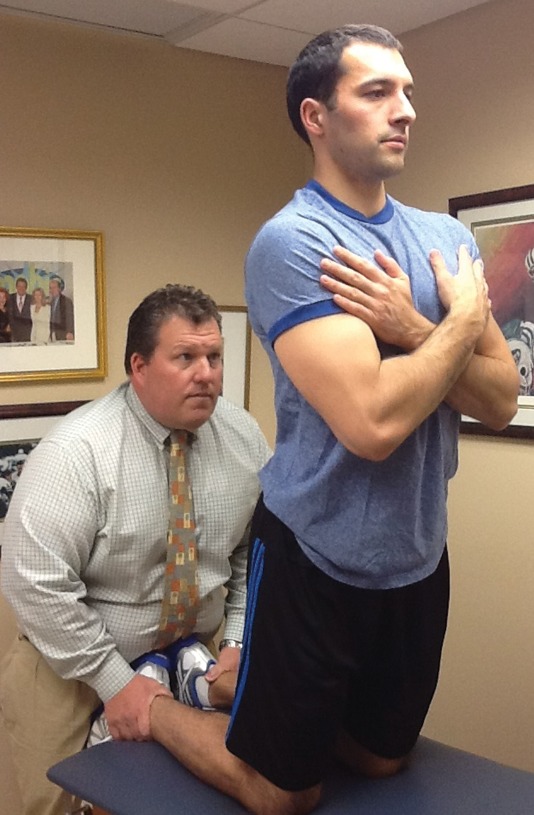
| 7. Single-limb balance windmill touches with weight on unstable surface (Figure 2) |
| 9. Sport-specific drills that incorporate postural control and progressive speed |
| Criteria for return to sport |
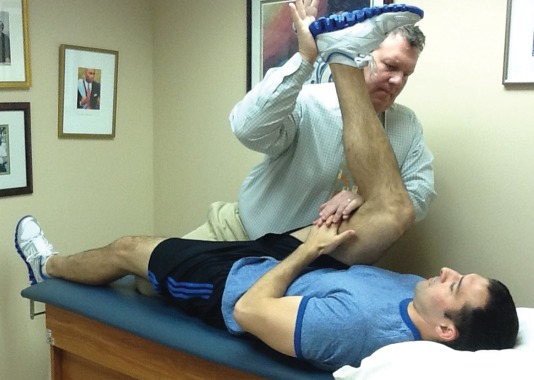
| 1. Full strength without pain in the lengthened state testing position (Figure 7) |
| 2. Bilateral symmetry in knee flexion angle of peak torque |
| 2. Full range of motion without pain |
| 3. Replication of sport specific movements at competition speed without symptoms |
In the acute stage of hamstring rehabilitation the treatment should focus on protecting the injury and minimizing range of motion and strength loss. Modalities such as ice, pulsed ultrasound, and laser are commonly utilized at this time. The athlete may begin pain free submaximal isometric strengthening at multiple angles (Figure 1) beginning at 48 hrs to allow the scar between fractured muscle fibers34 to achieve sufficient strength to avoid extensive separation of fiber stumps. These should be completed as a set of isometric knee flexion contraction at 30, 60, and 90 degrees of knee flexion by placing the injured limb on top of the into contralateral limb and contracting the strained hamstring. The hamstring should not be stretched into a painful range at this time but available hip and knee ROM should be maintained. Motion is also good for aligning fibers and increasing the strength of the lateral adhesion of fibers which protects the injured fibers from stump separation.35 The goals of this stage are to normalize gait and to obtain knee flexion strength at greater than 50% of uninjured length upon manual muscle testing at 90 degrees of knee flexion. Once these milestones are met the athlete may begin the next phase.
Figure 1.
Isometric knee flexion in the seated position. Note that this would be performed at multiple angles.
The goals of the second phase are to progressively regain strength throughout the range of motion and improve neuromuscular control of the hips and pelvis in preparation for sports specific movements. End range lengthening should be avoided if painful in this stage. The athlete may begin to strengthen both concentrically and eccentrically at this time. Eccentric training can be achieved using an isokinetic dynamometer if available and performing exercises such as the straight leg deadlift, single leg windmills (Figure 2), and Nordic hamstring exercise (Figure 3). To complete an eccentric single leg windmill the patient stands with the uninjured leg on a chair or fixed surface and reaches down in a diagonal plane while keeping stance leg straight and maintaining lumbar lordosis. The Nordic hamstring exercise is performed by having the clinician hold the patient's feet while in tall kneeling. The patient slowly falls forward while maintaining neutral hip posture until he or she can't control descent any longer and then pushes back into starting position with upper extremities. At the completion of this phase the athlete should have full strength upon manual muscle testing (5/5) or be within 20% of the uninjured leg in the zero to 90 degree range when measured with a hand held or isokinetic dynamometer in order to progress to the next phase. The athlete should also be able to jog both forward and backward without pain at a moderate speed at this point.
Figure 2.
Single leg eccentric hamstring windmills, which can be performed without (early) weights and progressed to use of hand-held weights or kettlebells, as shown.
Figure 3.
Nordic hamstring exercise.
In the third and final phase the focus of the rehabilitation is on functional movements and eccentric strengthening in the lengthened state. Plyometric and sports specific training may be initiated as well as advanced balance exercise. Lengthened state eccentric training may be done using an isokinetic dynamometer. Using a setup previously described in the literature,36,37 the Biodex may be modified so patient is in hip flexion and then passively extends and flexes the knee into the end range of motion (Figure 4). The patient resists the passive motion as the knee is extended. It is imperative the hip is positioned in flexion as the knee extends to ensure the hamstring is truly at a lengthened state. Alternative lengthened state eccentric training may also be achieved without a dynamometer by keeping the involved thigh on the subject's chest while resisting an outside force via elastic resistance Thera-Band, cable column, (Figure 5) or manual resistance. This exercise may be performed by having the patient lay supine pulling knee snugly into chest while hooked up to cable column or elastic resistance (Figure 5a). The patient then uses his or her arms to pull the knee into flexion and then slowly eccentrically resists the cable or elastic band as it pulls the knee into extension (Figure 5b). At the completion of this stage the athlete should have full strength throughout the range of motion and should be able to confidently perform all sport related tasks without limitation.
Figure 4.
Lengthened state eccentric training on the Biodex™.
Figure 5a,b.
Lengthened state eccentric training on cable column.
RETURN TO PLAY CRITERIA
Often athletes demonstrate full strength and ROM as assessed manually and with dynamometry in the clinic after completion of their rehabilitation, yet the recurrence rate remains disproportionately high. There is little evidence suggesting a valid functional test to determine return to play status after hamstring strain, which may mean rehabilitation professionals are returning athletes to competition before they have regained full strength in the lengthened hamstring position. In this regard Askling et al38 recently described a dynamic straight leg raise flexibility test, termed the H-test (Figure 6), to identify residual functional impairments that would preclude return to play. To perform the H-test, hamstring flexibility was calculated using data collected using an electrogoniometer during active ballistic hip flexion and conventional passive slow hip-flexion while in a supine position. A VAS-scale (0–100) was used to estimate experience of insecurity during active tests. Patients with hamstring injuries who were thought to be ready to return to sports based on standard clinical assessment demonstrated deficits in dynamic flexibility with the H-test despite having normal passive flexibility. The subjects also reported subjective insecurity while performing the test. Range of motion was assessed with an electrogoniometer which may not be widely available. Therefore the authors of this paper have performed the test using a non-retractable measuring tape and using simple trigonometry to calculate the angle during dynamic testing (Figure 6). Future research is required to establish the validity and clinical utility of this test in larger populations of patients.
Figure 6.
Dynamic hamstring flexibility test (H-test).
As an alternative or compliment to the H-test the authors have developed and are currently testing the validity of a manual muscle test to examine hamstring weakness in the lengthened state. Since the hamstring muscle group is a two joint muscle, crossing both the hip and knee joint, both hip flexion and knee extension must be incorporated when testing the hamstring at its true functional length. To conduct this manual muscle test the athlete lays supine and holds pulls one thigh into hip flexion holding it snugly against the chest. The contralateral limb remains flat on the table. The clinician then passively extends the knee until met with soft tissue resistance (i.e. putting a stretch on the hamstring). The clinician backs off by allowing the knee to flex 10 degrees from maximal stretch (Figure 7). From this position the clinician conducts the break test of the hamstring, and grades it using the tradition 0–5 scale established by Kendall or objectively by using a handheld dynamometer.
Figure 7.
Lengthened state manual muscle hamstring test.
CONCLUSION
Hamstring injuries have long been the bane of athletes' participation in sport among those who engage in sprinting and explosive movements, primarily because of both the high occurrence and recurrence rates. These injuries appear to create subsequent weakness at the muscle's lengthened state, predisposing the athlete to further injury. Lengthened state eccentric training may increase the end range strength resulting in fewer reinjuries and therefore should be incorporated in the rehabilitation process. Further research is needed to determine the effect of lengthened state eccentric training on incidence of hamstring strain reinjury.
REFERENCES
- 1.Brooks JH, Fuller CW, Kemp SP, et al. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. Am J Sports Med 2006; 34: 1297–1306 [DOI] [PubMed] [Google Scholar]
- 2.Woods C, Hawkins RD, Maltby S, et al. The Football Association Medical Research Programme: an audit of injuries in professional football – analysis of hamstring injuries. Br J Sports Med 2004; 38: 36–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ekstrand J, Hagglund M, Walden M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med 2011; 39: 1226–32 [DOI] [PubMed] [Google Scholar]
- 4.Elliot MC, Zarins B, Powell JW, et al. Hamstring strains in professional football players: a 10 year review. Am J Sports Med 2011; 39: 1621–8 [DOI] [PubMed] [Google Scholar]
- 5.Orchard J, Sweard H. Epidemiology of injuries in the Australian Football League, seasons 1997–2000. Br J Sports Med 2002; 36: 39–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malliaropoulos N, Isinkaye T, Tsitas K, et al. Reinjury after acute posterior thigh muscle injuries in elite track and field athletes. Am J Sports Med 2011; 39: 304–10 [DOI] [PubMed] [Google Scholar]
- 7.Marcus C, Elliott CW, Zarins B, et al. Hamstring Muscle Strains in Professional Football Players: 10 Year review. Am J Sports Med 2011; 39:843–850 [DOI] [PubMed] [Google Scholar]
- 8.Mendiguchia J, Alentorn-Geli E, Brughelli M. Hamstring strain injuries: are we headed in the right direction? Br J Sports Med 2012; 42: 81–86 [DOI] [PubMed] [Google Scholar]
- 9.Fousekis K, Tsepis E, Poulmedis P. Intrinsic risk factors of non-contact quadriceps and hamstring strains in soccer: a prospective study of 100 professional players. Br J Sports Med 2011; 45:709–14 [DOI] [PubMed] [Google Scholar]
- 10.Watsford ML, Murphy AJ, McLachlan KA, et al. A Prospective Study of the Relationship Between Lower Body Stiffness and Hamstring Injury in Professional Australian Rules Footballers. Am J Sports Med 2010: 2058–64 [DOI] [PubMed] [Google Scholar]
- 11.Orchard J, Marsden J, Lord S, et al. Preseason Hamstring Muscle Weakness Associated with Hamstring Muscle Injury in Australian Footballers. Am J Sports Med 1997; 25: 81–85 [DOI] [PubMed] [Google Scholar]
- 12.Small K, McNaughton LR, Greig M, et al. Soccer fatigue, sprinting, and hamstring injury risk. Int J Sports Med 2009; 8:587. [DOI] [PubMed] [Google Scholar]
- 13.Sherry MA, Best TM. A comparison of 2 rehabilitation progras in the treatment of acute hamstring strains. J Orthop Sports Phys Ther 2004; 34:116–25 [DOI] [PubMed] [Google Scholar]
- 14.Worrell TW. Factors associated with Hamstring injuries. An approach to treatment and preventative measures. Sports Med 1994; 17: 338–45 [DOI] [PubMed] [Google Scholar]
- 15.Hennessey L, Watson AW. Flexibility and posture assessment in relation to hamstring injury. Br J Sports Med 1993; 27:243–246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Engebretsen AH, Myklebust G, Holme I, et al. Intrinsic risk factors for hamstring injuries among male soccer players: A prospective cohort study. Am J Sports Med 2010; 2010: 1147–53 [DOI] [PubMed] [Google Scholar]
- 17.Hagglund M, Walden M, Ekstrom J. Previous injury as a risk factor for injury in elite football: A sporspective study over two consecutive seasons. Br J Sports Med 2006; 40: 767–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gabbe BJ, Bennell KL, Finch CF, et al. Predictors of hamstring injury at the elite level of Australian Football. Scan J Med Sci Sports 2006; 16:7–13 [DOI] [PubMed] [Google Scholar]
- 19.Askling CM, Tengvar M, Saartok T, et al. Acute first time hamstring strains during slow speed stretching: a clinical, magnetic resonance imaging, and recovery characteristics. Am J Sports Med 2007; 35: 1716–24 [DOI] [PubMed] [Google Scholar]
- 20.Askling CM, Tengvar M, Saartok T, et al. Proximal hamstring strains of stretching type in different sports: injury situations, clinical and magnetic resonance imaging characteristics, and return to sport. Am J Sports Med 2008; 36: 1799–804 [DOI] [PubMed] [Google Scholar]
- 21.Askling CM, Saartok T, Thortensson, et al. Type of acute hamstring strain affects flexibility, strength, and time to return to pre-injury level. Br J Sports Med 2006; 40: 40–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heidercheit BC, Sherry MA, Silder A, et al. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. J Orthop Sports Phys Ther 2010; 40: 67–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Orchard JW. Hamstrings are most susceptible to injury during the early stance phase of sprinting. Br J Sports Med 2012; 46: 88–89 [DOI] [PubMed] [Google Scholar]
- 24.Komi PV. Relevance of in vivo force measurements to human biomechanics. J Biomechanics 1990; 23(Suppl 1):23–34 [DOI] [PubMed] [Google Scholar]
- 25.Finni T, Komi PV, Lepola V. In vivo human triceps surae and quadriceps femoris muscle function in a squat jump and countermovement jump. Eur J Appl Physiol 2000; 83:416–26 [DOI] [PubMed] [Google Scholar]
- 26.Finni T, Komi PV, Lepola V. In vivo muscle mechanics during locomotion depend on movement amplitude and contraction intensity. Eur J Appl Physiol 2001; 85:272–8 [DOI] [PubMed] [Google Scholar]
- 27.Chumanov ES, Scache AG, Heidersheit BC, et al. Hamstrings are most susceptible to injury during the late swing phase of sprinting. Br J Sports Med 2011; 46:90. [DOI] [PubMed] [Google Scholar]
- 28.Schache AG, Dorn TW, Blanch PD, et al. Mechanics of the human hamstring muscle during sprinting. Med Sci Sports Exerc 2012; 44: 647–58 [DOI] [PubMed] [Google Scholar]
- 29.Brockett CL, Morgan DL, Proske U. Predicting hamstring strain injury in elite athletes. Med Sci Sports Exerc 2004; 36: 379–87 [DOI] [PubMed] [Google Scholar]
- 30.Arason A, Andersen TE, Holme I, et al. Prevention of hamstring strains in elite soccer: an intervention study. Scand J Med Sci 2008; 18:40–48 [DOI] [PubMed] [Google Scholar]
- 31.Askling C, Karlsson J, Thorstensson A. A hamstring injury occurence in elite soccer players after preseason training with eccentric overload. Scand J Med Sci 2003; 13: 244–50 [DOI] [PubMed] [Google Scholar]
- 32.Gabbe BL, Branson R, Bennel KL. A pilot randomised controlled trial of eccentric exercise to prevent hamstring injuries in community-level Australian football. J Sci Med Sport 2006; 9: 103–09 [DOI] [PubMed] [Google Scholar]
- 33.Petersen J, Thorborg K, Bachmann M, et al. Preventive Effect of Eccentric Training on Acute Hamstring Injuries in Men's Soccer: A cluster-Randomized Controlled Trial. Am J Sports Med 2011; 39: 2296–2303 [DOI] [PubMed] [Google Scholar]
- 34.Jarvinen AH, Jarvinen TLN, Kaariainen M, et al. Muscle injuries biology and treatment. Am J Sports Med 2005; 33: 745–64 [DOI] [PubMed] [Google Scholar]
- 35.Kaariainen M, Liljamo T, Pelto-Huikko M, et al. REgulation of alpha-7 integrin by mechanical stress during skeletal muscle regeneration. Neuromuscular Disord 2001; 11: 360–69 [DOI] [PubMed] [Google Scholar]
- 36.McHugh MP, Nesse M. Effect of strength loss and pain after eccentric exercise. Med Sci Sports Exerc 2008; 40: 566–73 [DOI] [PubMed] [Google Scholar]
- 37.Herda TJ, Cramer JT, Ryan ED, et al. Acute effects of static versus dynamic stretching on isometric peak torque, electromyography, and mechanomyography of the biceps femoris muscle. J Strength Cond Res 2008; 22: 809–17 [DOI] [PubMed] [Google Scholar]
- 38.Askling CM, Nilsson J, Thorstensson A. A new hamstring test to compliment the common clinical examination before return to sport after injury. Knee Surg Sports Traumatol Arthrosc 2010; 18: 1798–803 [DOI] [PubMed] [Google Scholar]