Abstract
Bleeding or open wounds of the integumentary system occur frequently in athletics. Integumentary wounds vary from minor scrapes, blisters, and small punctures to more serious lacerations and arterial wounds that could threaten the life of the athlete. The Sports physical therapist (PT) must realize that integumentary wounds and subsequent bleeding can occur in many sports, and assessment and care of such trauma is an essential skill. The purpose of this “On the Sidelines” clinical commentary is to review types of integumentary wounds that may occur in sport and their acute management.
Level of Evidence:
5
Keywords: Athletes, bleeding, integument, wounds
INTRODUCTION
Bleeding or open wounds of the integumentary system occur frequently in athletics.1,2 Integumentary wounds range from minor scrapes, blisters, and small punctures to more serious lacerations and arterial wounds that could threaten the life of the athlete. The Sports physical therapist (PT) must realize that integumentary wounds and subsequent bleeding can occur in many sports, and assessment and care of such trauma is an essential skill. For example, the skin can be injured by an object travelling at speed (i.e. baseball that is thrown at a high speed, or a shot-put that is thrown at a low speed) or during sports that are classified as high speed collision, due to contact with other athletes, stationary objects, or secondary to an athlete falling or sliding. The sports physical therapist must be prepared to manage any integumentary wound that is encountered on the sideline, using the principles of universal precautions,2 with thought given to infection control and subsequent wound healing. Prompt and appropriate management of skin lesions and bleeding conditions can decrease the risk of infection, and facilitate safe and expeditious return to sporting events.3 The purpose of this clinical commentary is to review types of integumentary wounds that may occur in sport and their acute management.
CLASSIFICATION OF WOUNDS
Arterial wounds
Arterial wounds may be sustained due to lacerations and punctures, and most typically occur due to major trauma. Arterial bleeding, described as pulsatile bleeding, is characterized by blood “spurting” from the body rhythmically by the beating heart.1 The blood produced by this type of an injury appears bright red, and this situation should be considered a medical emergency.1,2 The Sports PT should immediately activate the local emergency care system and should be prepared to take whatever steps are necessary to bring this type of bleeding under control. Arterial bleeding is very difficult to control due to the pressure of the beating heart which pushes blood into the arterial system.1 Management of acute arterial wounds, which will be discussed later, is extremely time sensitive and requires thorough knowledge of circulatory anatomy.
Venous Wounds
Bleeding of venous origin may also occur due to lacerations and punctures, but unlike the arterial wound, is due to injury of venous structures in the region of the injury. (Figure 1) Venous blood appears dark red and flows at a steady rate.1 (Figure 2) Venous bleeding is much easier to control than arterial bleeding, but can be life threatening in serious situations. Serious situations involving venous bleeding occur when large veins are injured and blood loss is severe.
Figure 1.
Example of a superficial laceration on the leg of an athlete, produced by contact with a spiked track shoe.
Figure 2.
Example of a puncture wound on the palm of an athlete.
Capillary Wounds
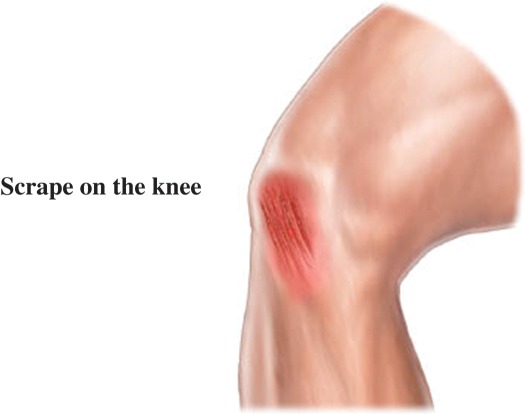
The most common form of bleeding associated with participation in athletics is capillary bleeding which occurs secondary to an abrasion.1,2,3 (Figure 3) Capillary bleeding is by far the most common skin wound and source of bleeding experienced by the Sports PT. An abrasion most commonly involves the epidermal layer of skin, but in more severe cases may include the removal of the epidermal layer and progression of the wound into the underlying dermal layer.1,3 Abrasions occur due to friction or scrape which can occur due to the collision of two players or the collision of a player with an object or surface such as a fence, goalpost, gym floor, or playing field.2 The injury occurs as force or friction being applied to the soft tissue exceeds the elasticity of the soft tissue, resulting in the superficial layer of skin being removed. This type of bleeding is also commonly referred to as “a strawberry”, “road rash”, “floor or mat burn”, names used to describe the mechanism of injury. (Figure 4) Regardless of the mechanism of injury, the outcome is essentially the same, interruption of the integumentary system, damage to the small capillaries, which creates of an open wound from which blood is lost. This injury results in slow or persistent seeping of blood, sustained over a larger surface area of tissue than the area associated with a puncture wound or abrasion. The size of the wound and the loss of blood are directly proportional to the area of epidermis and dermis that is affected. A bleeding capillary wound is much more painful than arterial or venous wound due to the exposure of multiple small nerve endings.
Figure 3.
Graphic representation of an abrasion on the knee, as would be sustained by a fall to the knee on turf or cement.
Figure 4.

Abrasion on the right hip of a 17 year old male soccer player, caused by friction of turf surface during a slide tackle.
WOUND MANAGEMENT
Universal Precautions and Preparedness
When bleeding does occur in athletics, the primary concern of the Sports PT should be self-protection and the prevention of disease transmission.1,3,4 In a study conducted by Jessee et al 4.1% of athletic trainer contacts with high school athletes involved potentially infectious bodily fluids, while the incidence of exposure to these fluids was 12.9% of athlete contacts.4 They concluded that universal precautions and personal protective equipment should be used in the athletic setting as a matter of course for protection of the health provider and the athlete. The authors of this clinical commentary were unable to find additional incidence data in other levels of sport, but believe that there are a number of steps that should be taken by the Sports PT to protect themselves in all situations. Personal protective equipment, such as latex or rubber gloves afford protection when controlling bleeding, performing bandaging, and when handling soiled or bloody bandages or instruments. Latex or rubber gloves should be readily available to the Sports PT at all times during the athletic competition, preferably in the pocket of the Sports PT to be accessible at a moment's notice. Should the Sports PT not have gloves readily available and the athlete suffers an injury resulting in bleeding, time is lost while the Sports PT looks through the sideline kit to locate gloves. This could result in blood loss and loss of precious time in the management of bleeding in the case of severe wounds. In addition to latex or rubber gloves, sterile gauze four by fours (4 X 4) should also be readily available to assist in covering the wound and achieving hemostasis.
Arterial Bleeding
Hemostasis is the goal of treatment of all bleeding wounds.5 No matter the wound type or etiology, hemostasis is the initial step in providing care to a bleeding athlete. In the most severe example, arterial bleeding should initially be treated by placing direct pressure over the site of the wound with a gloved hand and sterile gauze 4 X 4 if available.1,6 Any other type of cloth may be used in this emergency situation if no sterile dressings are available to assist in the application of direct pressure. If this technique is sufficient to control the bleeding, the wound should be covered with sterile gauze dressing and a bandage which will continue to apply pressure to the wound. Should the wound resume bleeding, additional direct pressure to the wound with the application of additional dressings and bandages should commence to decrease the loss of blood from the site of the wound. For extremity wounds, elevation above the level of the heart will assist with controlling bleeding. Should these bleeding control techniques fail to control bleeding, pressure over the “pressure point” of the extremity should be utilized.6 These “pressure points” are located in the upper extremities at the brachial artery located between the biceps and triceps on the inner aspect of the upper arm and for the lower extremities, pressure should be applied to the femoral artery in the femoral triangle. The femoral triangle in the lower extremity is located and the anterior proximal aspect of the hip joint. If the bleeding is unable to be stopped, the final and most extreme measure to control arterial bleeding is the application of a tourniquet. The tourniquet should be applied proximal to the area of the wound.6 There are many commercial tourniquets available today, however a tourniquet can be fabricated from something as simple as a strip of cloth, a leather or cloth belt, or a piece of rope and a stick of wood or some similar stiff object (used for tightening the rope). It is important to realize the application of a tourniquet is an absolute last resort in the control of arterial bleeding, and it should not be loosened or removed except by trained medical professionals in a controlled environment such as an emergency room or surgery suite. Advanced medical care providers (i.e. EMS personnel) must be notified of the presence of a tourniquet and assurances must be taken that emergency room personnel are aware of the fact that a tourniquet has been placed on the athlete. This is accomplished by informing advanced medical care providers of the presence of a tourniquet or marking with some type of marker change a “T” on the athlete's forehead. This will also serve to inform the hospital personnel that there is a tourniquet in place on the athlete. The tourniquet should never be left in place for an extended period of time secondary to the possibility of tissue necrosis and subsequent loss of limb.6 Thankfully, very few arterial wounds occur in sport.
Venous Bleeding
Control of serious venous blood loss begins with application of direct pressure with a latex gloved hand and sterile gauze, as previously described. The application of a pressure bandage should be considered with the application of sterile gauze directly over the wound followed by the application of a rolled bandage with sufficient pressure to effectively control bleeding.6 The injured extremity should then be elevated above the level of the heart to utilize gravity to slow the bleeding. If these techniques do not stop the flow of blood, the Sports PT should consider the use of previously described pressure points located at the brachial artery on the medial aspect of the upper arm or the femoral triangle located on the anterior aspect of the hip.
Lacerations
During the assessment of the athlete who has sustained a laceration, the Sports PT must initially be concerned with bleeding control and secondarily concerned with disposition of the athlete. The sports PT must decide if use of surgical tape such as Steri-Strips™ (3M, St. Paul, MN) (Figure 5) is sufficient to approximate the edges and maintain closure of the wound or if referral of the athlete to a local hospital or physician's office is necessary to have the wound stitched or stapled closed. When evaluating the wound following injury, once the bleeding is brought under control, the decision as to whether or not to refer the athlete for further care is based on the size and status of the laceration. If the wound “gaps open” or the edges of the wound do not approximate and stick together, the athlete should be referred for further care. (Figure 6) It is the responsibility of the Sports PT to clean the wound as much as possible without inducing additional bleeding. Ideally, lacerations should be sutured or stapled closed within 8 hours of occurrence.2 Staples are best used for scalp lesions where cosmesis is less critical.2
Figure 5.
Example of a deep laceration with exposed subcutaneous tissue.
Figure 6.
Example of the use of Steri-strips™ (3M, St. Paul, MN) for closure of a laceration.
Another method of wound closure that may be selected by the Sports PT is the use of Dermabond® (Ethicon, Somerville, NJ) to seal the wound. Dermabond® a type of medical adhesive that is utilized extensively in surgery to close surgical incisions, and has been shown to provide good cosmetic results and minimal discomfort, but also allows an athlete to return quickly to competition.2 The Sports PT should follow local protocol to determine if the use of Dermabond® is within allowable protocol for their use. Dermabond® must be applied to dry skin that has achieved hemostasis.2 If the use of Dermabond® is acceptable, the Sports PT must carefully cleanse the wound prior to the application of Dermabond® to the edges of the wound. Should Dermabond® be used for wound closure and the wound not be free of bacteria, a serious infection could develop due the closed environment in which bacteria may grow.
Capillary bleeding
Abrasion type wounds should be washed with soap and water or a non-cytotoxic cleansing agent. Contaminated abrasions may need to be irrigated under pressure in order to remove foreign particles or debris in the wound bed. Cleansing is important not only to remove contaminants in order to prevent infection, but also to prevent permanent discoloration of the skin known as tattooing.5 After cleansing, capillary bleeding is controlled through the application of direct pressure with a latex gloved hand and sterile dressing. This type of bleeding is typically not difficult to control with direct pressure. Usually, other methods such as pressure dressings, pressure points, extremity elevation, and application of a tourniquet are not necessary. When hemostasis is achieved, the wound is covered with an application of a topical ointment that contains antibiotics and a local anesthetic. Use of a topical antibiotic is important to prevent wound contamination that may occur due to environmental exposure from surfaces or other athletes. Maintain caution to make certain that the athlete is not allergic to the topical medication. If there are any questions as to the proper utilization of topical antibiotics, check regarding local protocol prior to administering the medication. The Sports PT must also be aware of additional soft tissue damage and subsequent pain that may occur with capillary bleeding. Application of ice and pressure along with elevation of the injured extremity would be appropriate in the management of soft tissue bruising that may occur in this type of injury.
Healthy wound healing environment
Finally, regardless of the etiology, the wound must be dressed with an appropriate dressing that allows for a moist healing environment which has been proven to be optimal for epidermal migration.5 Optimally, a transparent or semi-permeable film or hydrocolloid is used that provides an anti-microbial barrier while allowing oxygen access to the wound, thus expediting healing.3 It is especially important that a moist environment be maintained in the healing process of abrasions, as when they dry out and are allowed to scab they are frequently re-injured by scab removal during sport participation.1,2,3
CONCLUSION
In conclusion, the Sports PT may assume the responsibility of management of a number of types of open wounds when providing care on the sidelines of athletic events. The Sports PT must take seriously the use of universal precautions and utilize personal protective equipment, primarily rubber or latex gloves. Sterile dressings and roller bandages should be close by and readily available to hold dressings in place and to apply direct pressure to the wound. Wounds should initially be managed by direct pressure, followed by elevation, pressure dressing and pressure bandage. Should these methods fail to control the bleeding, the Sports PT must consider pressure point application or in extreme cases, the use of a tourniquet. In any case, the Sports PT must be ready to provide appropriate acute wound care and subsequent cleansing and treatment of integumentary lesions.
REFERENCES
- 1.Prentice WE. Principles of Athletic Training: A Competency-based Approach (14th ed). New York, New York: McGraw-Hill, 2010 [Google Scholar]
- 2.Foster DT, Rowedder LJ, Reese SK. Management of sport-induced skin wounds. J Athl Train. 1995;30(2):135–140 [PMC free article] [PubMed] [Google Scholar]
- 3.Honsik KA, Romeo MW, Hawley CJ, Romeo SJ, Romeo JP. Sideline skin and wound care for acute injuries. Curr Sports Med Report. 2007;6(3):147–154 [DOI] [PubMed] [Google Scholar]
- 4.Jessee KB, Middlemas DA, Mulder DK, Rehberg RS. Exposure of athletic trainers to potentially infectious bodily fluids in the high school setting. J Athl Train. 1997;32(4):b320–322 [PMC free article] [PubMed] [Google Scholar]
- 5.Irion GL. Comprehensive Wound Management. Throrfare, NJ: Slack, Inc., 2002 [Google Scholar]
- 6.American Red Cross Emergency Medical Response. Staywell Health and Safety Solutions, Yardley, PA; 2011 [Google Scholar]