Abstract
Background and Purpose:
Athletes reporting chest pain are challenging to diagnose and equally challenging to treat. The majority of chest pain is musculoskeletal in origin, yet differentiating these from other more serious conditions should be the initial primary focus. The ability to reproduce the patient's symptoms aids in the differential diagnostic process. The purpose of this case report is to illustrate the use of dry needling (DN) to aid in the diagnosis and treatment of focal chest wall pain.
Case Descriptions:
A 22 year-old male military athlete with anterior chest pain, refractory to traditional physical therapy, was evaluated and treated with dry needling.
Outcomes:
Favorable results were achieved as demonstrated by clinically meaningful improvements in the Patient Specific Functional Scale, the Global Rating of Change score, and his physical performance which allowed this athlete to return to competition and military training.
Conclusion:
Dry needling in the hands of properly trained providers may aid in diagnosis and treatment of focal chest wall syndromes.
Level of Evidence:
Therapy, Level 4
Keywords: chest pain, costochondritis, dry needling, military athlete, physical therapy
INTRODUCTION
Athletes who seek care for a primary complaint of focal chest pain in the direct-access sports physical therapy setting present unique challenges. When faced with any new patient consultation, especially a patient reporting “chest pain”, the physical therapist must determine whether the patient is appropriate for physical therapy or if he or she requires immediate medical referral.1,2 Visceral or somatic origins of chest pain include the heart, lungs, pleura, liver, and stomach.3 While the cause of chest pain is often musculoskeletal in origin and 80% of all chest pain seen in primary care is benign,4 differentiating between cardiac-related, visceral, and musculoskeletal chest pain conditions is essential for formulating an accurate diagnosis and developing an appropriate course of action.
Once the patient is determined to have pain of musculoskeletal origin, physical therapy is an appropriate setting for definitive care.5,6,7 The challenge for the physical therapist then becomes conducting a focused physical examination and designing an effective treatment plan. When an athlete reports a history of direct trauma, such as a contact injury to the chest from an opponent's elbow, the evaluation and treatment can be straightforward. In patients who present with an insidious onset of chest wall pain and an unremarkable history, the list of differential diagnoses can be extensive (Table 1).4,8–11 While a myriad of contributing factors must be considered when evaluating focal chest pain, the highest percentages of musculoskeletal-related chest pain have been reported to originate from either costochondritis,12 segmental dysfunction of the cervicothoracic spine,13 or local muscular tenderness.14
Table 1.
Potential causes of chest pain in athletes.
| Musculoskeletal | Cardiac | Respiratory | Gastrointestinal |
|---|---|---|---|
| Sternocostal joint sprain | Myocardial infarction | Asthma | Gastroesophageal reflux disease |
| Intercostal muscle strain | Pericarditis | Exercise induced asthma | Esophagitis |
| Rib contusion | Myocarditis | Lower respiratory infection | Hiatus hernia |
| Referred pain from the thoracic | Aortic dissection | Pneumothorax | Peptic ulcer |
| spine | Pleuritis | Cholecystitis | |
| Stress fracture (rib, manubrium, or sternum) | Pulmonary embolus | Pancreatitis Oesophgeal motility disorders |
|
| Chondral cartilage injury (fracture) | |||
| Rib tip syndrome | |||
| Costochondritis | |||
| Tietze's syndrome | |||
| Osteoarthritis (sternoclavicular, manubriosternal, or costovertebral) |
One suggested contributor to focal chest wall pain that may cause both local muscular tenderness and/or referred symptoms is local neuromuscular dysfunction and the presence of so-called muscle trigger points (MTrPs).15 MTrPs are described as localized hyperirritable areas in skeletal muscle associated with hypersensitive palpable taut bands,15 which have been reported in the literature as either “active” or “latent”.16 Active MTrPs are suggested to spontaneously contribute to local or referred symptoms without manual stimulation and may alter muscle activation and joint range of motion (ROM).16 Latent MTrPs may also alter muscle activation patterns and affect range-of-motion without contributing to pain referral unless manually stimulated.16,17 Variability between patients and muscle structure or type may contribute to poor reliability in detecting focal contractile changes such as those suggested to be MTrPs.18 Despite concerns regarding reliability and accuracy of localizing and identifying MTrPs, their treatment is frequently included in the plan of care for numerous musculoskeletal conditions, including pain in the chest wall.19,20 Various techniques and modalities have been described in the literature that may be used to treat MTrPs, including stretching, soft tissue mobilization, dry needling (DN), and injection therapy.21–23 The purpose of this case report is to illustrate the use of DN to aid in the diagnosis and treatment of focal chest wall pain.
CASE DESCRIPTION: INITIAL EVALUATION AND TREATMENT (PROVIDER #1):
The subject was a 22 year-old right upper extremity dominant male who presented to a direct-access sports physical therapy clinic with a primary complaint of left-sided anterior chest pain for one month duration. While symptoms had been gradually worsening over the past month, the patient reported he experienced a “severe” bout of pain shortly following pushups two days prior. The patient attributed his pain to increased physical training in preparation for the Sandhurst Competition, an international military academy competition consisting of high-intensity endurance and obstacle negotiating challenges.24 Resting pain was reported at 3/10 which increased to 7/10 on a numeric pain rating scale (NPRS) with push-ups, bench press, or similar resistance activities. He denied history of any serious cardiopulmonary conditions or direct trauma to the upper extremity, chest, neck, or upper back.
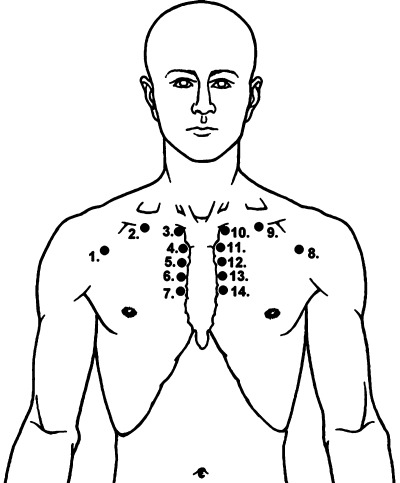
Physical examination revealed a well-appearing, muscularly developed and otherwise healthy male in no apparent distress. Observation revealed no bruising, swelling, or deformities. Cervical, thoracic, and bilateral upper extremity active range of motion were pain free and within normal limits. Gross manual muscle testing of the upper extremities was 5/5 and equal bilaterally, with minor anterior chest wall discomfort reported during resisted left shoulder flexion, abduction, and internal rotation. Bilateral pectoralis minor tightness was demonstrated when examined in supine,25 left greater than right. Pain was reproduced with palpation to the anteromedial aspect of the left ribs 2–4 as well as the left side of the sternum and corresponding costochondral joint (Figure 1, points 11–13).
Figure 1.
Potential points of tenderness on the anterior chest wall. Point 8 represents the left pectoralis major point at the anterior axillary line approximately 3 cm caudal to the clavicle. Point 11 represents the area corresponding to the costochondral region of the 2nd rib. (Reprinted from Medical Clinics of North America, 94(2), Stochkendahl MJ, Christensen HW, Chest Pain in Focal Musculoskeletal Disorders, 259–273, 2010 with permission from Elsevier).
Based on the initial history and evaluation, including reproduction of symptoms with palpation of the anterior rib and costochondral area, the therapist concluded that the patient's condition was musculoskeletal in nature and was primarily due to overuse. Consistent with the patient history and presentation of localized sharp pain at the costal cartilages, a working diagnosis of “costochondritis” was made, which is often the term used for conditions characterized by pain and local tenderness without focal swelling in the costochondral region.4,8,10 The treatment plan included home exercises consisting of pectoralis stretching and thoracic active range of motion exercises with an additional recommendation to avoid aggravating activities.11
FOLLOW-UP VISITS AND CARE (PROVIDER #1):
Following two weeks of the home exercise program and rest, the patient reported resting pain had resolved (0/10), and pain with resisted activity was unknown since he had avoided aggravating activities as instructed. Compared to the initial evaluation, there were no significant changes on physical examination although subjectively less pain was reported with palpation of the anterior chest wall. The patient was advised to continue the current exercises and to gradually increase activity as tolerated.
Two weeks later, the patient reported his symptoms had returned as he increased his activity (NPRS at rest 3/10, NPRS with activity 7/10). Upon more thorough cervicothoracic spine examination conducted during this visit, the therapist determined there to be painfree hypomobility throughout the upper thoracic spine from T1-T7.26,27 The hypomobile segments were immediately treated with supine thoracic regional manipulation and a cervicothoracic junction distraction manipulation.28 Grade I & II mobilizations of the costochondral joints were performed as described by Greenman,28 at the anterior aspect of ribs 2–5 with the therapist's thumb and thenar eminence at the superior aspect of the rib shaft.11 An additional two weeks later, the patient stated his symptoms were unchanged. The treating provider considered DN as a potential treatment option; however, he had not received training/certification to safely administer this intervention. He consulted with a colleague who did have the appropriate training who suggested a trial of needling may stimulate a healing response. The patient agreed to obtain a second opinion and to consider the DN treatment.
INITIAL EVALUATION AND TREATMENT (PROVIDER #2)
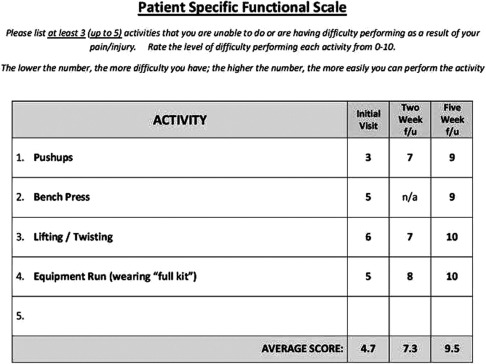
At the time of this evaluation, the patient reported that his chest pain was overall unchanged compared to 3 months prior – although symptoms had improved for a couple weeks with rest but returned with activity. Current reported pain was 4/10 (resting) and 7/10 (with resistive activity) on the NPRS. During this visit, the patient was asked to complete a Patient Specific Functional Scale (PSFS), rating the difficulty level of several “important” activities on which he indicated “push-ups” to be his most difficult activity (Figure 2). There are no specific outcomes measures reported in the literature for assessment of chest wall syndromes, however the PSFS has been reported to be a valid, reliable, and responsive outcome measure for patients with neck pain, back pain, and upper quarter complaints.29–31 He further stated that prior to onset of his current pain he was able to perform over fifty push-ups during his most recent physical fitness assessment (Army Physical Fitness Test, 2-minute push-up event).
Figure 2.
Patient Specific Functional Scale. The patient self-selected four activities that were difficult to perform due to his symptoms. For example, activity number 4 “Equipment Run (wearing full kit)” involves running in boots with full military gear.
The majority of physical examination findings (ROM, strength, etc.) coincided with those described previously. Examination of the cervicothoracic region, including soft tissue, transverse processes, and rib angles26 was unremarkable. During palpation, this provider determined the greatest discomfort corresponded to the area of the costochondral joint at the level of the second rib (Figure 1, point 11). Several focal symptomatic areas of local muscular tenderness, consistent with the description of MTrPs, were also located in the left pectoralis major and pectoralis minor muscles using flat and pincer-type palpation (Figure 1, points 8, 9).15,22
Following this history and physical examination, DN was discussed with the patient as a potential treatment option, including a thorough discussion of precautions and risks associated with needling in the thoracic region. After written informed-consent was obtained, dry needling was performed over the second rib32 at the costochondral joint and along the soft tissues superficial and corresponding to the second rib. During the dry needling of the costochondral joint and soft tissue, the patient reported reproduction of his symptoms. A reproduction in symptoms served to add diagnostic value by confirming that the patient's symptoms were musculoskeletal in origin. The needle was pistoned repeatedly (manipulated up and down without withdrawing the needle) targeting the areas of symptom reproduction and the patient consistently reported reproduction of his symptoms, although no local twitch responses were recognized (Figure 3, top). While DN was potentially indicated to the pectoralis muscles at this time, the therapist elected to assess the patient's response to direct needle stimulation of the costochondral structures prior to adding a second treatment location. The patient did not report any significant changes in symptoms immediately following therapy. He was advised to perform shoulder active range of motion with gentle unilateral pectoralis muscle stretching33–35 as a home exercise program, and to avoid aggravating activities.
Figure 3.
Locations used for dry needling technique: costohondral region of 2nd rib (top), and pectoralis major muscle (bottom).
Based on the history and evaluation, including reproduction of symptoms with palpation and needling of the costochondral area, the second therapist concurred with the original clinician that the patient's condition was musculoskeletal in nature; however, the diagnosis was generalized to “chest wall syndrome”. It has been suggested that musculoskeletal pain localized to the chest wall is best termed “chest wall syndrome”, as the morphological and physiological basis is elusive and the exact nature is challenging to ascertain.9
TREATMENT AND FOLLOW-UP VISITS (PROVIDER #2)
Two days later the patient returned for re-evaluation and treatment. He reported his overall pain level was unchanged (4/10 at rest) although he stated that his symptoms seemed to be more focal. During this visit, in addition to DN the second rib costochondral region, DN was also directed to the palpable tender bands of soft tissue in his left pectoralis muscle region (Figure 3, bottom). Local twitch responses were elicited, and the patient again reported reproduction of his focal chest wall symptoms, with needling at both locations. Immediately following needling therapy the patient reported feeling “looser” in his chest muscles and the previously palpable bands of soft tissue were no longer symptomatic. No additional exercises were prescribed at that time.
Three days later, the patient subjectively reported feeling “50% better” overall, rated his pain as 2/10, and he was able to demonstrate five pain free push-ups at that time. During this visit the patient agreed to defer further needling treatment to assess the duration of symptom improvement from the previous treatment. He stated that he intended to resume training as tolerated for the Sandhurst Competition with his teammates and was encouraged to continue pectoralis muscle stretching.
An additional week later, the patient reported pain at rest was 0/10 and pain with activity was 2/10 (localized to the pectoral muscles). The patient further stated he performed a cumulative total of 100 repetitions of push-ups throughout the previous weekend (two days prior) with minimal discomfort. Additionally, his PSFS was improved from baseline (Figure 2). He was treated with DN to the left pectoralis major muscle, in the area of reported symptoms during activity, with local twitch responses elicited during therapy. Additionally, he was provided a closed-chain upper extremity exercise program to help prepare him more completely for his upcoming endurance and obstacle course event consisting of a push-up progression program, upper extremity box drills, and plyometrics.
OUTCOME
At one month following the initial dry needling treatment the patient reported that he had been pain free at rest and with activity for greater than a week, and he successfully completed the Sandhurst Challenge without significant symptoms. His composite PSFS score, which was initially reported at 4.7, had improved to 9.5 (Figure 2). The minimum important difference (MID) in the overall PSFS for patients with upper extremity conditions is 1.2 points.30 Each individual PSFS score improved between 4 (bench press) to 6 (pushups) points (Figure 2). The minimum detectable change in single activities on the PSFS is 3 points. In addition, this patient's Global Rating of Change (GROC) was scored at +6. The GROC used in this case was a 15-point scale in which patients assess their impression of their global clinical change from the time they began treatment, ranging from “A very great deal worse” to “A very great deal better”. The GROC is considered a valuable tool to assess self-perceived change in patient's symptoms, with greater than 5 point change considered clinically meaningful.36,37
At a follow-up visit 3 months later, the patient continued to report significant improvement in symptoms with intermittent minor discomfort during strenuous exercise activities. He reported overall that he has continued to feel over 90% improved and rated his GROC at +6. He reported he was able to complete several advanced military physical training courses that required strenuous repetitive use of the upper extremities. He stated that he was able to perform 50 repetitions of push-ups before onset of discomfort, was able to perform the same number of pushups as before initial onset of his problem and estimated having performed several hundred push-ups during the previous month.
DISCUSSION
This case report illustrates the use of dry needling targeting the costochondral region and pectoral musculature to aid in the diagnosis and treatment of focal chest wall pain. Because traditional physical therapy management did not yield significant changes in the patient's symptoms, this patient was referred to a physical therapist with advanced training in DN.38 During the evaluation, DN to the costochondral joint and focal soft tissue tenderness consistent with the description of MTrPs in the pectoralis musculature reproduced this patient's familiar chest wall symptoms. This information served to confirm the current symptoms were most likely musculoskeletal in nature. Despite this being a challenging area to manage which is often recalcitrant to other therapies, after 4 treatment sessions of DN directed to the costochondral joints and pectoralis musculature over a 1 month period of time, this patient achieved substantial improvements in pain and function. Although case studies such as this illustrate a potential response to treatment and favorable outcomes, they do not provide sufficient information to determine a cause and effect relationship.
Musculoskeletal chest wall pain has traditionally been a difficult area to evaluate and treat. Injection therapy with local anesthetics or corticosteroids has been previously described as a treatment method for costochondral-related chest wall pain.4 Since results of previous research studies have indicated DN may be as effective as injection therapy for various conditions,39,40 a trial of DN was deemed appropriate for this case and was performed to potentially stimulate a healing response. Following the first two treatments of DN, the subject was able to resume training and following two additional treatment sessions he was able to successfully participate in the physically demanding Sandhurst Challenge.
Needling has been reported in the literature as an effective adjunct to treatment for numerous musculoskeletal conditions.41–47 Furthermore, in some cases, needling may aid in the diagnostic process by reproducing the patient's symptoms.22 DN is a potentially valuable technique when used to differentiate between symptoms originating in muscle tissue from other structures. The ability to reproduce the patient's symptoms, such as described in the current case, has great value aiding in the differential diagnostic process. If DN elicits a local twitch response in conjunction with the patients familiar pain the cause is likely to be, at least partly, of muscular origin.22,48,49
Several conceptual models explaining the mechanism of action of DN have been described in the literature, including the radiculopathy model, the MTrP model, and the spinal segmental sensitization model.41 Clinicians practicing based on the trigger point model target specific locations in muscle tissue thought to be MTrPs, although the reliability and accuracy of detecting these focal muscle lesions lacks strong support in the literature.18 Patient expectations and the placebo effect can provide significant results, and there is limited evidence to determine if needling has an effect beyond placebo.50 In this case the patient failed to improve with traditional therapies and therefore the authors elected to use a functional treatment approach, focusing on patient-specific responses in function following DN intervention. Favorable changes were demonstrated after localizing therapy with DN to the costochondral joint and local areas of tenderness associated with the patient's primary complaint.
The ability to elicit a local twitch response (LTR) is proposed to confirm that the needle has affected an MTrP. Hong and colleagues stated that outcomes are significantly better when a LTR is elicited during needling.39 The authors' experience has been that patients frequently feel little or no discomfort during insertion of the needle, and depending on the target tissue, typically only respond with discomfort following several millimeters to centimeters of depth of needle advancement has been achieved. The depth of needle insertion prior to patient feedback leads us to believe we are truly affecting the target tissue and not simply the superficial or subcutaneous sensory tissue, since the depth of needle insertion has exceeded that of the superficial soft tissue. Although not reported elsewhere, non-contractile tissue such as are described in the current case, may also benefit from needling therapies. Further research is required to determine responsiveness to needling various musculoskeletal structures such as ligaments, tendons, and entheses.
It should be emphasized that only properly trained providers with an extensive knowledge of human anatomy should perform DN. Physical therapists have been recognized as neuromusculoskeletal clinical experts6,7,51 with extensive training in anatomy, physiology, palpation, and manual therapies. Several DN training programs are available in the United States for clinicians whose state practice act allows needling,46 typically the thoracic region is not covered in introductory and beginning level courses.38,52
Because DN is an invasive procedure, great caution needs to be heeded when DN is performed in the vicinity of vital internal organs. Risks associated with needling the thoracic region include pneumothorax, cardiac trauma, and infection.53 Needling is safe, however, when performed by properly trained health professionals who use the proper safety precautions.46,50,53 The risk of iatrogenic pneumothorax from dry needling in the thoracic region is likely similar to that of other needling therapies such as acupuncture, which has an estimated incidence of less than 1/10,000.53 Handwashing and thorough cleaning of the area to be treated are basic steps employed to reduce the risk of infection. Universal precautions, such as wearing gloves, should be standard practice for all clinicians performing invasive procedures in which they may come into contact with bodily fluids. To the authors' knowledge, no adverse events have been reported when following the appropriate procedures and precautions and there are no cases of pneumothorax, cardiac trauma, or infection from dry needling by physical therapists reported in the literature.
While DN is an accepted treatment technique by therapists in many countries, relatively few physical therapists in the United States have received training and certification in DN.22 In 2009, the Executive Committee of the American Academy of Orthopaedic Manual Physical Therapists issued a position statement that dry needling falls within the scope of physical therapy practice.54 Recently, the American Physical Therapy Association published an educational resource paper regarding physical therapists use of DN.55 As with any modality or rehabilitation technique, research is needed to determine the most effective parameters in which DN should be implemented.
CONCLUSION
Although the majority of focal chest wall pain is attributed to musculoskeletal dysfunction, effective treatment strategies remain elusive. The substantial change in function and symptoms illustrated in this case study suggests that dry needling in the hands of a qualified provider with advanced training may aid in treatment for patients with focal chest wall pain of musculoskeletal origin. While this treatment modality has great potential for aiding as an adjunct to management in musculoskeletal conditions, future research is needed to evaluate the effectiveness of dry needling to determine what conditions would most likely benefit from needling techniques. Additionally, research is needed to determine best practices regarding duration and frequency of this treatment modality.
REFERENCES
- 1.Childs JD, Whitman JM. Advancing physical therapy practice: the accountable practitioner. J Orthop Sports Phys Ther. 2005;35(10):624–627 [DOI] [PubMed] [Google Scholar]
- 2.Davenport TE, Kulig K, Resnik C. Diagnosing pathology to decide the appropriateness of physical therapy: what's our role? J Orthop Sports Phys Ther. 2006;36(1):1–2 [DOI] [PubMed] [Google Scholar]
- 3.Gerwin RD. Myofascial and Visceral Pain Syndromes: Visceral-Somatic Pain Representations. Journal of Musculoskeletal Pain. 2002;10(1–2):165–175 [Google Scholar]
- 4.Stochkendahl MJ, Christensen HW. Chest pain in focal musculoskeletal disorders. Med Clin North Am. 2010;94(2):259–273 [DOI] [PubMed] [Google Scholar]
- 5.Cohen SP, Kapoor SG, Anderson-Barnes VC, et al. Noncardiac chest pain during war. Clin J Pain. 2010;27(1):19–26 [DOI] [PubMed] [Google Scholar]
- 6.Childs JD, Whitman JM, Sizer PS, Pugia ML, Flynn TW, Delitto A. A description of physical therapists' knowledge in managing musculoskeletal conditions. BMC Musculoskelet Disord. 2005;6:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deyle GD. Direct access physical therapy and diagnostic responsibility: the risk-to-benefit ratio. J Orthop Sports Phys Ther. 2006;36(9):632–634 [DOI] [PubMed] [Google Scholar]
- 8.Sik EC, Batt ME, Heslop LM. Atypical chest pain in athletes. Curr Sports Med Rep. 2009;8(2):52–58 [DOI] [PubMed] [Google Scholar]
- 9.Bosner S, Becker A, Hani MA, et al. Chest wall syndrome in primary care patients with chest pain: presentation, associated features and diagnosis. Fam Pract. 2010;27(4):363–369 [DOI] [PubMed] [Google Scholar]
- 10.Gregory PL, Biswas AC, Batt ME. Musculoskeletal problems of the chest wall in athletes. Sports Med. 2002;32(4):235–250 [DOI] [PubMed] [Google Scholar]
- 11.Brukner PD, Khan K, Singer K. Thoracic and Chest Pain: Costochondritis. Clinical Sports Medicine. 3rd ed.North Ryde: McGraw-Hill Australia; 2009 [Google Scholar]
- 12.How J, Volz G, Doe S, Heycock C, Hamilton J, Kelly C. The causes of musculoskeletal chest pain in patients admitted to hospital with suspected myocardial infarction. Eur J Intern Med. 2005;16(6):432–436 [DOI] [PubMed] [Google Scholar]
- 13.Christensen HW, Vach W, Gichangi A, Manniche C, Haghfelt T, Hoilund-Carlsen PF. Cervicothoracic angina identified by case history and palpation findings in patients with stable angina pectoris. J Manipulative Physiol Ther. 2005;28(5):303–311 [DOI] [PubMed] [Google Scholar]
- 14.Verdon F, Herzig L, Burnand B, et al. Chest pain in daily practice: occurrence, causes and management. Swiss Med Wkly. 2008;138(23–24):340–347 [DOI] [PubMed] [Google Scholar]
- 15.Simons D, Travell J, Simons L. Travell & Simons' Myofascial Pain and Dysfunction: The Trigger Point Manual. Vol 1 2nd ed.Baltimore, MD: Lippincott Williams & Wilkins; 1999 [Google Scholar]
- 16.Bennett R. Myofascial pain syndromes and their evaluation. Best Pract Res Clin Rheumatol. 2007;21(3):427–445 [DOI] [PubMed] [Google Scholar]
- 17.Lucas KR, Polus BI, Rich PA. Latent myofascial trigger points: their effects on muscle activation and movement efficiency. Journal of Bodywork and Movement Therapies. 2004;8(3):160–166 [Google Scholar]
- 18.Lucas N, Macaskill P, Irwig L, Moran R, Bogduk N. Reliability of physical examination for diagnosis of myofascial trigger points: a systematic review of the literature. Clin J Pain. 2009;25(1):80–89 [DOI] [PubMed] [Google Scholar]
- 19.Lawson GE, Hung LY, Ko GD, Laframboise MA. A case of pseudo-angina pectoris from a pectoralis minor trigger point caused by cross-country skiing. J Chiropr Med. 2011;10(3):173–178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gerwin RD, Shannon S, Hong CZ, Hubbard D, Gevirtz R. Interrater reliability in myofascial trigger point examination. Pain. 1997;69(1–2):65–73 [DOI] [PubMed] [Google Scholar]
- 21.Kamanli A, Kaya A, Ardicoglu O, et al. Comparison of lidocaine injection, botulinum toxin injection, and dry needling to trigger points in myofascial pain syndrome. Rheumatology International. 2005;25(8):604–611 [DOI] [PubMed] [Google Scholar]
- 22.Dommerholt J, Huijbregts P. Myofascial trigger points: pathophysiology and evidence-informed diagnosis and management. Sudbury, MA: Jones and Bartlett; 2011 [Google Scholar]
- 23.De las Penas CF, Sohrbeck Campo M, Fernandez Carnero J, Miangolarra Page JC. Manual therapies in myofascial trigger point treatment: a systematic review. Journal of Bodywork and Movement Therapies. 2005;9(1):27–34 [Google Scholar]
- 24.USMA Sandhurst Competition Manual. Available at: http://www.usma.edu/dmi/sandhurst_manual.htm Accessed September 30, 2011
- 25.Sahrmann S. Diagnosis and treatment of movement impairment syndromes. London: Mosby; 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Flynn TW, Cleland JA, Whitman JM. Users' Guide to the Musculoskeletal Examination: Fundamentals for the Evidence-Based Clinician. Buckner, KY: Evidence in Motion; 2008 [Google Scholar]
- 27.Maitland GD. Vertebral Manipulation. 5th ed.Boston: Butterworth-Heinemann; 1986 [Google Scholar]
- 28.Greenman PE. Principles of Manual Medicine. 3rd ed.Philadelphia, PA: Lippincott Williams & Wilkins; 2003 [Google Scholar]
- 29.Cleland JA, Fritz JM, Whitman JM, Palmer JA. The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine (Phila Pa 1976). 2006;31(5):598–602 [DOI] [PubMed] [Google Scholar]
- 30.Hefford C, Abbott JH, Arnold R, Baxter GD. The patient-specific functional scale: validity, reliability, and responsiveness in patients with upper extremity musculoskeletal problems. J Orthop Sports Phys Ther. 2012;42(2):56–65 [DOI] [PubMed] [Google Scholar]
- 31.Sterling M, Brentnall D. Patient Specific Functional Scale. Aust J Physiother. 2007;53(1):65. [DOI] [PubMed] [Google Scholar]
- 32.Zylstra E. Advanced Trigger Point Dry Needling (Level II): Applications for Pain Management and Sports Injuries (Training Manual). Brighton, CO: Kinetacore; 2011 [Google Scholar]
- 33.Borstad JD, Ludewig PM. Comparison of three stretches for the pectoralis minor muscle. J Shoulder Elbow Surg. 2006;15(3):324–330 [DOI] [PubMed] [Google Scholar]
- 34.McClure P, Greenberg E, Kareha S. Evaluation and management of scapular dysfunction. Sports Med Arthrosc. 2012;20(1):39–48 [DOI] [PubMed] [Google Scholar]
- 35.Muraki T, Aoki M, Izumi T, Fujii M, Hidaka E, Miyamoto S. Lengthening of the pectoralis minor muscle during passive shoulder motions and stretching techniques: a cadaveric biomechanical study. Phys Ther. 2009;89(4):333–341 [DOI] [PubMed] [Google Scholar]
- 36.Kamper S. Global Rating of Change scales. Aust J Physiother. 2009;55(4):289. [DOI] [PubMed] [Google Scholar]
- 37.Kamper SJ, Maher CG, Mackay G. Global rating of change scales: a review of strengths and weaknesses and considerations for design. J Man Manip Ther. 2009;17(3):163–170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kinetacore IMT-TDN Advanced Training: Advanced Trigger Point Dry Needling. Kinetacore. Available at: http://www.kinetacore.com Accessed June 15, 2011 [Google Scholar]
- 39.Hong CZ. Lidocaine injection versus dry needling to myofascial trigger point. The importance of the local twitch response. Am J Phys Med Rehabil. 1994;73(4):256–263 [DOI] [PubMed] [Google Scholar]
- 40.Brukner PD, Khan K, Granter R. Treatments Used for Musculoskeletal Conditions: More Choices and More Evidence. Clinical Sports Medicine. 3rd ed.North Ryde: McGraw-Hill Australia; 2009 [Google Scholar]
- 41.Dommerholt J, Bron C, Franssen J. Myofascial trigger points: an evidence-informed review. Journal of Manual & Manipulative Therapy (Journal of Manual & Manipulative Therapy). 2006;14(4):203–221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fernandez-Carnero J, La Touche R, Ortega-Santiago R, et al. Short-term effects of dry needling of active myofascial trigger points in the masseter muscle in patients with temporomandibular disorders. J Orofac Pain. 2010;24(1):106–112 [PubMed] [Google Scholar]
- 43.Furlan AD, van Tulder M, Cherkin D, et al. Acupuncture and dry-needling for low back pain: an updated systematic review within the framework of the cochrane collaboration. Spine. 2005;30(8):944–963 [DOI] [PubMed] [Google Scholar]
- 44.Ga H, Choi JH, Park CH, et al. Dry needling of trigger points with and without paraspinal needling in myofascial pain syndromes in elderly patients. Journal of Alternative & Complementary Medicine. 2007;13(6):617–624 [DOI] [PubMed] [Google Scholar]
- 45.Hsieh YL, Kao MJ, Kuan TS, et al. Dry needling to a key myofascial trigger point may reduce the irritability of satellite MTrPs. American Journal of Physical Medicine & Rehabilitation. 2007;86(5):397–403 [DOI] [PubMed] [Google Scholar]
- 46.Kalichman L, Vulfsons S. Dry needling in the management of musculoskeletal pain. J Am Board Fam Med. 2010;23(5):640–646 [DOI] [PubMed] [Google Scholar]
- 47.Osborne NJ, Gatt IT, Osborne NJ, Gatt IT. Management of shoulder injuries using dry needling in elite volleyball players. Acupuncture in Medicine. 2010;28(1):42–45 [DOI] [PubMed] [Google Scholar]
- 48.Escobar PL, Ballesteros J. Teres minor. Source of symptoms resembling ulnar neuropathy or C8 radiculopathy. Am J Phys Med Rehabil. 1988;67(3):120–122 [DOI] [PubMed] [Google Scholar]
- 49.Facco E, Ceccherelli F. Myofascial pain mimicking radicular syndromes. Acta Neurochir Suppl. 2005;92:147–150 [DOI] [PubMed] [Google Scholar]
- 50.Rickards LD. Therapeutic needling in osteopathic practice: An evidence-informed perspective. International Journal of Osteopathic Medicine. 2009;12(1):2–13 [Google Scholar]
- 51.Murphy BP, Greathouse D, Matsui I. Primary care physical therapy practice models. J Orthop Sports Phys Ther. 2005;35(11):699–707 [DOI] [PubMed] [Google Scholar]
- 52.Myopain Intramuscular Manual Therapy Program. Myopain Seminars. Available at: http://www.myopainseminars.com Accessed June 15, 2011 [Google Scholar]
- 53.McCutcheon L, Yelland M. Iatrogenic pneumothorax: safety concerns when using acupuncture or dry needling in the thoracic region. Physical Therapy Reviews. 2011;16(2):126–132 [Google Scholar]
- 54.AAOMPT Position Statements: Dry Needling. Available at: http://www.aaompt.org/about/statements.cfm Accessed June 15, 2011
- 55.APTA Physical Therapists & the Performance of Dry Needling: An Educational Resource Paper. Available at: http://www.apta.org/StateIssues/DryNeedling/ResourcePaper Accessed April 23, 2012