Abstract
Background/Aims
Rebleeding after endoscopic therapy for non-variceal upper gastrointestinal hemorrhage (NGIH) is the most important predictive factor of mortality. We evaluated the risk factors of rebleeding in patients undergoing endoscopic therapy for the NGIH.
Methods
Between January 2003 and January 2007, 554 bleeding events in 487 patients who underwent endoscopic therapy for NGIH were retrospectively enrolled. We reviewed the clinicoendoscopical characteristics of patients with rebleeding and compared them with those of patients without rebleeding.
Results
The incidence of rebleeding was 21.7% (n=120). In the multivariate analysis, initial hemoglobin level ≤9 g/dL (p=0.002; odds ratio [OR], 2.433), inexperienced endoscopist with less than 2 years of experience in therapeutic endoscopy (p=0.001; OR, 2.418), the need for more 15 cc of epinephrine (p=0.001; OR, 2.570), injection therapy compared to thermal and injection therapy (p=0.001; OR, 2.840), and comorbidity with chronic renal disease (p=0.004; OR, 2.908) or liver cirrhosis (p=0.010; OR, 2.870) were risk factors for rebleeding following endoscopic therapy.
Conclusions
Together with patients with low hemoglobin level at presentation, chronic renal disease, liver cirrhosis, the need for more 15 cc of epinephrine, or therapy done by inexperienced endoscopist were risk factors for the development of rebleeding.
Keywords: Gastrointestinal hemorrhage, Risk factors, Endoscopy, Therapy
INTRODUCTION
Endoscopic therapies such as injections, clipping, and thermal ablation have been effective in achieving primary hemostasis in patients with non-variceal upper gastrointestinal hemorrhage (NGIH).1 Despite these advancements in therapeutic endoscopy, bleeding recurs in 15-20% of cases after successful endoscopic therapy for NGIH.2 Moreover, NGIH remains a common cause of hospitalization and rebleeding, which are the most important predictive factors of mortality, occurring in 3.1-7.0% of patients.3-5 Therefore, prevention and prediction of patients at risk of rebleeding, after initial endoscopic therapy, is essential for a successful outcome in patients with NGIH.
The presence of large ulcers (≥1 cm) with severe bleeding at presentation is well known to be predictive of rebleeding.4,6 Proton pump inhibitor (PPI) has been reported as an effective medication for recurrent bleeding after endoscopic therapy.7,8 In addition, advanced age, comorbidity, shock, rebleeding, and the need for surgery have been associated with an increase in mortality after endoscopic hemostasis.8,9 However, little is known about additional risk factors for rebleeding after endoscopic therapy, although scoring systems have been developed for the prediction of outcomes in patients with NGIH.10 Therefore, identification of the factors related to the development of rebleeding, after endoscopic therapy for NGIH, might improve patient management and outcome. The aim of this study was to evaluate the clinical outcome and potential predictive factors associated with rebleeding in patients undergoing endoscopic therapy for NGIH.
MATERIALS AND METHODS
Patients
Between January 2003 and January 2007, a total of 554 bleeding events in 487 patients (M:F=366:121; Age, 58.9±15.3) who underwent endoscopic therapy for NGIH were retrospectively enrolled. Patients that were not treated with endoscopic therapy or had Mallory-Weiss syndrome were excluded. The clinical and endoscopic characteristics of patients with rebleeding were reviewed and compared with patients who did not develop rebleeding. Patient characteristics and rebleeding related data were recorded for the following variables: gender, age, alcohol and smoking history, underlying disease (chronic renal failure, liver cirrhosis, hypertension without aspirin use, diabetes mellitus, aspirin or clopidogrel use, current use of coumadin, and others), past gastrointestinal bleeding history, endoscopic findings (cause and location of bleeding, size, and bleeding state), endoscopic therapies, endoscopists' experiences, clinical outcomes, and mortality. A written informed consent for therapy was obtained from each patient. The study was carried out in accordance with the Helsinki Declaration after the approval of Institutional Review Board of Wonju Christian Hospital.
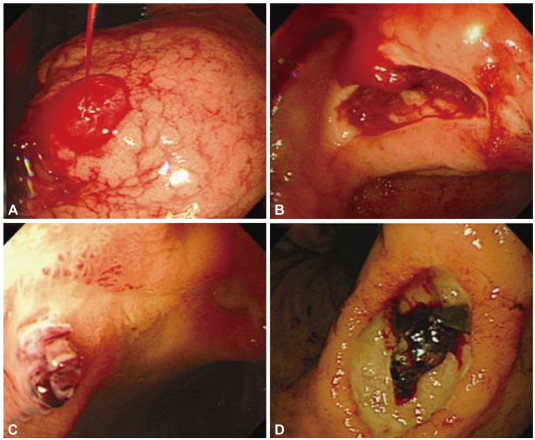
All patients were managed according to NIGH treatment protocol of the hospital. The patients' vital signs were assessed at 10 minutes interval before the endoscopy, and then every 2 hours for 24 hours after the endoscopy, and every 6 hours thereafter until the follow-up after the endoscopy. The hemoglobin level was checked at least once daily; a blood transfusion was given if the hemoglobin level decreased to lower than 9 g/dL. Rebleeding was defined by at least two of the followings: new-onset hematemesis or melena with blood pressure <100 mm Hg, decrease of more than 2 g/dL in hemoglobin level, endoscopic confirmation of bleeding, or pathologic lesion which required endoscopic therapy within 7 days after the initial therapy. Bleeding state was classified by Forrest classification (Fig. 1): active spurting bleeding (Ia), active oozing bleeding (Ib), vessel exposure (IIa), and red or black adherent clots (IIb).
Fig. 1.
Bleeding status. (A) Active pumping. (B) Active oozing. (C) Vessel exposure. (D) Red or black clot.
Endoscopic therapy
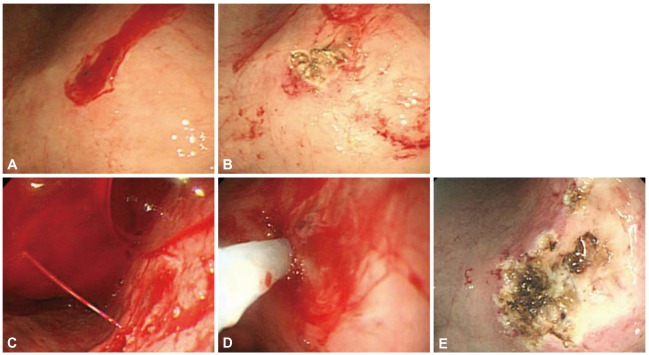
All feasible patients presented to the hospital with NGIH underwent endoscopy within 24 hours. The patients received intravenous PPIs to promote healing of the lesion before and after the endoscopic therapy. Levin tube insertion and irrigation with more than 3,000 cc of normal saline was provided before the initial endoscopy. Thirteen gastroenterologists, with more than 2 years of experience (>6,000 cases of endoscopy) of performing endoscopy, carried out the therapeutic endoscopy for NGIH during the study period. Therapies used for the initial NGIH were 1:10,000 epinephrine injection, GLUE (thrombin/fibrin, Greenplast; Green Cross, Yongin, Korea) injection, hemoclipping, and thermal ablation (monopolar or argon plasma coagulation [APC]). Patients were scheduled to have a follow-up endoscopy within 24 hours. If the general condition was not suitable for an endoscopy, the follow-up endoscopy was delayed. After evaluation of the follow-up endoscopy, further management was decided including: the appropriate meal time, follow-up endoscopic therapy, endoscopic biopsy, and Helicobacter pylori test. If active bleeding or vessel exposure was observed at the follow-up endoscopy, it was considered as a rebleeding and a second session of endoscopic therapy was planned (Fig. 2). If the bleeding continued after the endoscopic therapy, surgery or embolization therapy was performed. During fasting periods, 40 mg of intravenous pantoprazole sodium was injected, as a bolus, every 12 hours. And then, all patients were treated with oral PPI at a standard dose every morning during the next 6-8 weeks. Patients with positive rapid urea test results were provided with 7-day eradication therapy (10 mg or 20 mg of PPI+1 g of amoxicillin+500 mg of clarithromycin, b.i.d.). Patients underwent blood test, abdominal ultrasound, and a routine abdominal X-ray during the admission and on an outpatient basis after the procedure to assess bleeding, perforation, or other possible complications.
Fig. 2.
Serial endoscopic findings show rebleeding after the initial endoscopic therapy. (A) Initial endoscopic finding. (B) Post state of epinephrine injection+argon plasma coagulation. (C) Rebleeding occurred 2 days after the initial endoscopic treatment. (D) Second endoscopic therapy with epinephrine injection+argon plasma coagulation. (E) Post state of second endoscopic therapy.
Statistical analysis
An independent-samples t-test was used for comparison of continuous variables. Data were expressed as means and standard deviations. The correlation between rebleeding and risk variables was assessed by univariate analysis. In addition, multivariate logistic regression analysis was performed to identify factors related to rebleeding and mortality. Age, gender, and plausible risk factors (p<0.25) from the results of the univariate analysis were used in the multivariate analysis where appropriate. The enter method was performed to find the odds ratios; and the relationship of each variable in the multivariate analysis was analyzed. Data were analyzed with statistical software (SPSS version 13.0; SPSS Inc., Chicago, IL, USA). A p-value <0.05 was considered significant in all tests.
RESULTS
Patient characteristics and clinical outcomes of rebleeding
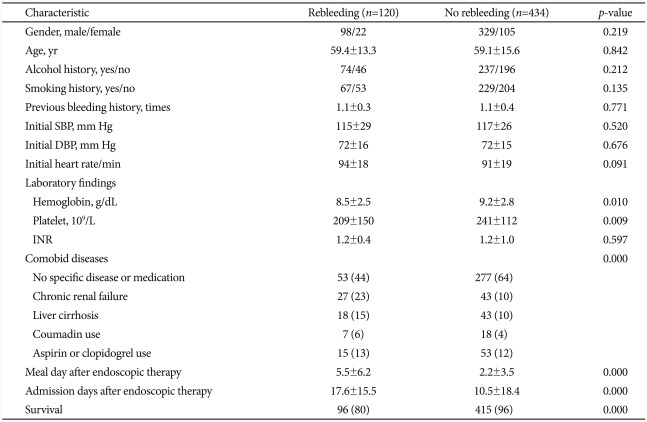
The mean age of the patients was 59.1 years (range, 13-93 years). Among a total of 554 patients, 120 (21.7%) patients were diagnosed as rebleeding after the endoscopic therapy. The causes of NGIH were gastric ulcer in 327 (59.1%), duodenal ulcer in 173 (31.2%), Dieulafoy lesion in 26 (4.7%), marginal ulcer in 16 (2.9%), and cancer bleeding in 12 (2.2%) patients. Comorbid diseases and medications used included chronic renal failure in 70 (12.6%), aspirin or clopidogrel use in 68 (12.3%), liver cirrhosis in 61 (11.0%), hypertension without aspirin therapy in 50 (9.0%), diabetes mellitus in 25 (4.5%), current use of coumadin in 25 (4.5%), diabetes mellitus and hypertension without aspirin therapy in 17 (3.1%), and others in 8 (1.4%) patients. The remaining (229 patients) had no underlying disease. The average hospital stay was 12 days (range, 1-210 days) after the endoscopic therapy. Twenty patients (3.6%) underwent surgery and 1 patient was treated with embolization because of continuous bleeding after therapy. Forty-four patients (7.9%) died after the endoscopic therapy (Table 1).
Table 1.
Clinical Characteristics of Patients
Values are presented as mean±SD or number (%); p-value for Pearson's χ2 test (2 by 2 and 2 by x) and the independent-samples t-test for comparison of continuous variables.
SD, standard deviation; SBP, systolic blood pressure; DBP, diastolic blood pressure; INR, international normalized ratio.
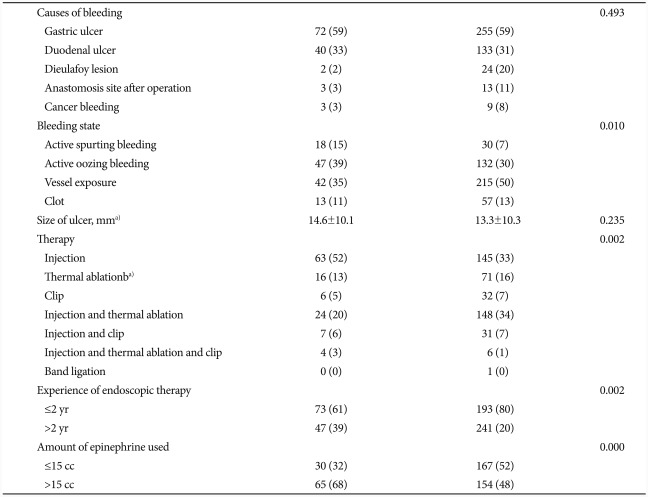
With regard to endoscopic characteristics (Table 2), the bleeding was characterized by vessel exposure in 257 (46.4%), active oozing in 179 (32.3%), active spurting bleeding in 48 (8.7%), and red and black clots in 70 (12.6%) patients. APC therapy (18.6%) was most commonly used as a single therapy. The mean amount of epinephrine used in therapy was 13.5 (12.8) cc. In the combination therapy, epinephrine and GLUE (Greenplast) injection therapy (22.4%) was the most common combination therapy in this study. The mean ulcer size was 13.6 (10.2) mm. The mean therapeutic experience of the endoscopist was 3.7 (3.0) years. In the gastric lesions, most common locations of bleeding were the body and lesser curvature.
Table 2.
Endoscopic Characteristics of Patients
Values are presented as mean±SD or number (%). p-value for Pearson's χ2 test (2 by x) and the independent-samples t-test for comparison of continuous variables.
a)Argon plasma coagulation or electrocoagulation.
Factors related to rebleeding
The univariate analysis showed no significant differences in gender, age, alcohol and smoking history, previous bleeding history, international normalized ratio, cause of bleeding, size of ulcer, and the number of biopsy in the rebleeding group compared to the group without rebleeding. However, lower initial hemoglobin level and platelet count (p=0.010 and p=0.009), comorbidity with chronic renal disease (p=0.000), degree of initial bleeding state (p=0.010), endoscopic treatment modality (p=0.002), experience of the endoscopist (p=0.002), and the need for large amount (>15 cc) of epinephrine during the therapy (p=0.000), were found to be positively related to rebleeding (Tables 1, 2).
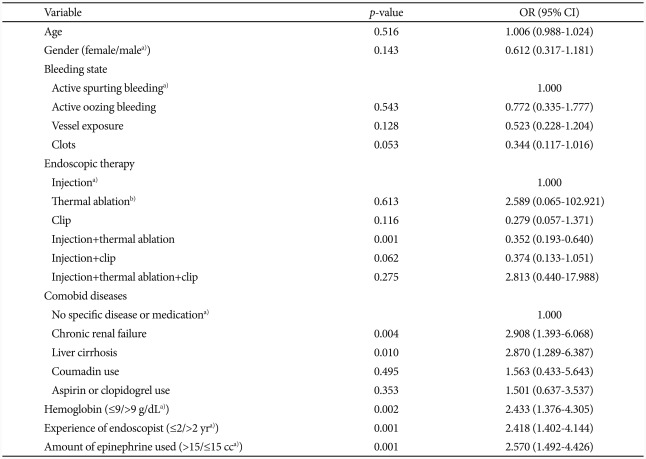
In the multivariate analysis, initial hemoglobin level ≤9 g/dL (p=0.002; odds ratio [OR], 2.433), unskillful endoscopist with less than 2 years of therapeutic endoscopy experience (p=0.001; OR, 2.418), the need for more 15 cc of epinephrine (p=0.001; OR, 2.570), injection therapy compared to thermal and injection therapy (p=0.001; OR, 2.840), and comorbidity with chronic renal disease (p=0.004; OR, 2.908) or liver cirrhosis (p=0.010; OR, 2.870) were risk factors of rebleeding following endoscopic therapy. Initial active spurting bleeding (p=0.021; OR, 5.208) and rebleeding (p=0.000; OR, 6.391) were significantly related to mortality (Table 3).
Table 3.
Multivariate Analysis of Factors for the Risk of Rebleeding
OR, odds ratio; CI, confidence interval.
a)Reference category; b)Argon plasma coagulation or electrocoagulation.
Factors related to mortality
The mortality rate of patients without comorbid disease (7.0%, n=23) was lower than that of patients with chronic renal disease (17.1%, n=12) or liver cirrhosis (11.5%, n=7). In the univariate analysis, the mortality rate was significantly higher in patients with advanced age, history of alcohol consumption, location of bleeding in the body, the presence of rebleeding or surgery, the need for large amounts of epinephrine, low blood pressure or platelet count at presentation, fast heart rate on presentation, active bleeding, and a longer hospitalization (p<0.05).
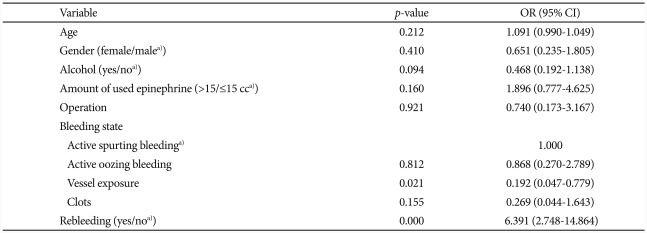
The multivariate analysis showed that initial active spurting bleeding (p=0.021; OR, 5.208) and rebleeding (p=0.000; OR, 6.391) were significantly related to the mortality following the endoscopic therapy (Table 4).
Table 4.
Multivariate Analysis of Factors for the Risk of Mortality
OR, odds ratio; CI, confidence interval.
a)Reference category.
DISCUSSION
In this study, the frequency of rebleeding after the initial endoscopic therapy was 22.1%, which is similar to prior reports.10-12 With regard to PPI use, prior studies suggested that PPI administration reduced the rebleeding rate to 4%; a rate lower than the finding of this study.5 The definition of rebleeding period (<7 days), selection of enrolled patients who received endoscopic hemostasis, and administration method of PPI might have affected the results of this study, because most prior studies used continuous infusion of high dose PPI with or without bolus injection. Also, several of these studies included patients whose ulcers did not require an endoscopic therapy or rebleeding lasted for a short period (<3 days).13-16 Treatment with continuous PPI infusion is thought to be associated with a better outcome by improving wound healing. However, prospective studies with gastric pH measurements during various administration methods of PPI are needed to further explain the underlying mechanism of better hemostasis.
Rebleeding after endoscopic hemostasis is associated with an increased risk of mortality, prolonged hospital stay, and increased medical expenses.3,9 In this study, endoscopic findings of active spurting bleeding and the presence of rebleeding was associated with poor prognosis. Chiu et al.4 reported that larger ulcers with stigmata and high American Society of Anesthesiologists (ASA) general score (grade III and IV) were important predictors of recurrent bleeding after a second endoscopy. However, we did not check the ASA general score in this study and the relation between ulcer size and rebleeding was not confirmed.
Comorbid disease with chronic renal failure and liver cirrhosis were major risk factors for rebleeding in this study. A recent study demonstrated that dialysis patients with end stage renal disease were more likely to experience rebleeding than patients who were not on dialysis after ulcer bleeding.17 Little has been known about the underlying mechanisms for high risks of bleeding, rebleeding, and mortality in patients with chronic renal failure. However, decreased bicarbonate secretion, abnormal coagulation system, or uremic platelet dysfunction could be related to high risk of rebleeding.17,18 Rebleeding also might be common in these patients, since most patients with renal disease and cirrhosis show advanced ASA status.19 In this study, 39% and 30% of patients with chronic renal failure and liver cirrhosis, respectively, experienced rebleeding after the first endoscopic treatment. A careful follow up with intensive monitoring is indicated, therefore, in these patients after the endoscopic therapy.
Other factors such as coumadin, aspirin, or clopidogrel use were not related to rebleeding. These findings are consistent with a recent report showing that anticoagulation use did not increase the risk of rebleeding.10 The suppression of gastroduodenal mucosal prostaglandin synthesis is associated with the mucosal damage caused by aspirin.20 Peters et al.21 suggested that the risk of bleeding increases with aspirin dose increase with or without clopidogrel. However, these studies did not report on the association between rebleeding and anticoagulation therapy. In this present study, anticoagulation therapy was not related to rebleeding which was similar to other prior reports.4 Immediate cessation of medication after the suspicion of bleeding might be associated with the negative correlation.
Consideration of procedure-related factors may be important to reduce the mortality rate due to bleeding during and/or after endoscopic therapy. At the time of therapy, inexperienced endoscopists and the need for large amounts of epinephrine were also definite risk factors for rebleeding in the current study. We found that 61% (73/120) of the patients with rebleeding had endoscopic therapy by an endoscopist with less than 2 years of therapeutic endoscopy experience. In addition, 30% (219) of bleeding cases, which could not be controlled by ≤15 cc of epinephrine injections, rebled within 7 days of the initial endoscopy in this study. These findings were unique in the current study. Therefore, more careful approaches under the expert supervision, short term follow-up endoscopy, and close and intensive monitoring are needed for patients who underwent endoscopic therapy in circumstances with these 2 risk conditions.
In the consensus recommendations for managing patients with NGIH, combination therapy was superior to single therapy.1,22 Thermal ablation such as APC or electrocoagulation with injection therapy significantly reduced rebleeding in this study (p<0.01), suggesting the intensive therapy using combination method by an expert is a primary determinant of better outcome in patients with NGIH.
Low hemoglobin level and active pumping bleeding at presentation were other risk factors of rebleeding. Active pumping means that seeding vessel is relatively large; and low hemoglobin level might be a result of massive arterial bleeding. As a result, these findings suggest that massive bleeding from a relatively large vessel was positively related to rebleeding after endoscopic therapy and consequent poor outcomes.
The limitations of this study include the retrospective study design and the use of different PPI doses and administration methods. Therefore, prospective studies using the same PPI administration are needed to properly identify the risk predictors for rebleeding in a larger number of patients. Currently, a lot of comparative studies reported the advantages of different PPIs, doses, treatment methods, therapy protocols, scoring systems, and costs. Therefore, new treatments for reducing rebleeding should be verified over time.
In conclusion, the results of this study showed that low hemoglobin level at presentation, chronic renal disease, liver cirrhosis, treatment with endoscopic injection therapy (>15 cc of epinephrine) or by inexperienced endoscopist were significantly related to the development of rebleeding after the endoscopic therapy. Moreover, since rebleeding is one of the risk factors of mortality, close follow up with intensive monitoring is indicated in these patients after endoscopic therapy.
Acknowledgments
This research was supported by Basic Science Research Program of the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (20110006074).
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Barkun A, Bardou M, Marshall JK Nonvariceal Upper GI Bleeding Consensus Conference Group. Consensus recommendations for managing patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2003;139:843–857. doi: 10.7326/0003-4819-139-10-200311180-00012. [DOI] [PubMed] [Google Scholar]
- 2.Laine L, Peterson WL. Bleeding peptic ulcer. N Engl J Med. 1994;331:717–727. doi: 10.1056/NEJM199409153311107. [DOI] [PubMed] [Google Scholar]
- 3.Müller T, Barkun AN, Martel M. Non-variceal upper GI bleeding in patients already hospitalized for another condition. Am J Gastroenterol. 2009;104:330–339. doi: 10.1038/ajg.2008.62. [DOI] [PubMed] [Google Scholar]
- 4.Chiu PW, Joeng HK, Choi CL, Kwong KH, Ng EK, Lam SH. Predictors of peptic ulcer rebleeding after scheduled second endoscopy: clinical or endoscopic factors? Endoscopy. 2006;38:726–729. doi: 10.1055/s-2006-925179. [DOI] [PubMed] [Google Scholar]
- 5.Lin HJ, Lo WC, Lee FY, Perng CL, Tseng GY. A prospective randomized comparative trial showing that omeprazole prevents rebleeding in patients with bleeding peptic ulcer after successful endoscopic therapy. Arch Intern Med. 1998;158:54–58. doi: 10.1001/archinte.158.1.54. [DOI] [PubMed] [Google Scholar]
- 6.Wong SK, Yu LM, Lau JY, et al. Prediction of therapeutic failure after adrenaline injection plus heater probe treatment in patients with bleeding peptic ulcer. Gut. 2002;50:322–325. doi: 10.1136/gut.50.3.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaviani MJ, Hashemi MR, Kazemifar AR, et al. Effect of oral omeprazole in reducing re-bleeding in bleeding peptic ulcers: a prospective, double-blind, randomized, clinical trial. Aliment Pharmacol Ther. 2003;17:211–216. doi: 10.1046/j.1365-2036.2003.01416.x. [DOI] [PubMed] [Google Scholar]
- 8.Chan FK, Ching JY, Hung LC, et al. Clopidogrel versus aspirin and esomeprazole to prevent recurrent ulcer bleeding. N Engl J Med. 2005;352:238–244. doi: 10.1056/NEJMoa042087. [DOI] [PubMed] [Google Scholar]
- 9.Chiu PW, Ng EK, Cheung FK, et al. Predicting mortality in patients with bleeding peptic ulcers after therapeutic endoscopy. Clin Gastroenterol Hepatol. 2009;7:311–316. doi: 10.1016/j.cgh.2008.08.044. [DOI] [PubMed] [Google Scholar]
- 10.Wolf AT, Wasan SK, Saltzman JR. Impact of anticoagulation on rebleeding following endoscopic therapy for nonvariceal upper gastrointestinal hemorrhage. Am J Gastroenterol. 2007;102:290–296. doi: 10.1111/j.1572-0241.2006.00969.x. [DOI] [PubMed] [Google Scholar]
- 11.Tajima A, Koizumi K, Suzuki K, et al. Proton pump inhibitors and recurrent bleeding in peptic ulcer disease. J Gastroenterol Hepatol. 2008;23(Suppl 2):S237–S241. doi: 10.1111/j.1440-1746.2008.05557.x. [DOI] [PubMed] [Google Scholar]
- 12.Andriulli A, Annese V, Caruso N, et al. Proton-pump inhibitors and outcome of endoscopic hemostasis in bleeding peptic ulcers: a series of meta-analyses. Am J Gastroenterol. 2005;100:207–219. doi: 10.1111/j.1572-0241.2005.40636.x. [DOI] [PubMed] [Google Scholar]
- 13.Lau JY, Sung JJ, Lee KK, et al. Effect of intravenous omeprazole on recurrent bleeding after endoscopic treatment of bleeding peptic ulcers. N Engl J Med. 2000;343:310–316. doi: 10.1056/NEJM200008033430501. [DOI] [PubMed] [Google Scholar]
- 14.Ng FH, Wong SY, Lam KF, et al. Gastrointestinal bleeding in patients receiving a combination of aspirin, clopidogrel, and enoxaparin in acute coronary syndrome. Am J Gastroenterol. 2008;103:865–871. doi: 10.1111/j.1572-0241.2007.01715.x. [DOI] [PubMed] [Google Scholar]
- 15.Marmo R, Koch M, Cipolletta L, et al. Predictive factors of mortality from nonvariceal upper gastrointestinal hemorrhage: a multicenter study. Am J Gastroenterol. 2008;103:1639–1647. doi: 10.1111/j.1572-0241.2008.01865.x. [DOI] [PubMed] [Google Scholar]
- 16.Sung JJ, Barkun A, Kuipers EJ, et al. Intravenous esomeprazole for prevention of recurrent peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2009;150:455–464. doi: 10.7326/0003-4819-150-7-200904070-00105. [DOI] [PubMed] [Google Scholar]
- 17.Cheung J, Yu A, LaBossiere J, Zhu Q, Fedorak RN. Peptic ulcer bleeding outcomes adversely affected by end-stage renal disease. Gastrointest Endosc. 2010;71:44–49. doi: 10.1016/j.gie.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 18.Dinoso VP, Jr, Murthy SN, Saris AL, et al. Gastric and pancreatic function in patients with end-stage renal disease. J Clin Gastroenterol. 1982;4:321–324. doi: 10.1097/00004836-198208000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Hu ML, Wu KL, Chiu KW, et al. Predictors of rebleeding after initial hemostasis with epinephrine injection in high-risk ulcers. World J Gastroenterol. 2010;16:5490–5495. doi: 10.3748/wjg.v16.i43.5490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vallurupalli NG, Goldhaber SZ. Gastrointestinal complications of dual antiplatelet therapy. Circulation. 2006;113:e655–e658. doi: 10.1161/CIRCULATIONAHA.105.590612. [DOI] [PubMed] [Google Scholar]
- 21.Peters RJ, Mehta SR, Fox KA, et al. Effects of aspirin dose when used alone or in combination with clopidogrel in patients with acute coronary syndromes: observations from the Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) study. Circulation. 2003;108:1682–1687. doi: 10.1161/01.CIR.0000091201.39590.CB. [DOI] [PubMed] [Google Scholar]
- 22.Barkun AN, Bardou M, Kuipers EJ, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010;152:101–113. doi: 10.7326/0003-4819-152-2-201001190-00009. [DOI] [PubMed] [Google Scholar]