Abstract
Background
Postnatal depression has received considerable research and clinical attention; however, anxiety and stress in postpartum women have been relatively neglected.
Objective
The aim of this study was to determine the prevalence of depression, anxiety, and stress during the postpartum period of women using the Depression Anxiety Stress Scales, and to examine the associated correlates of these conditions.
Design
This was a cross-sectional study conducted from January 2010 to May 2011.
Setting
Primary health care centers of the State of Qatar Supreme Council of Health.
Subjects
A representative sample of 2091 women who attended primary health care centers was surveyed. From this sample, 1659 women (79.3%) consented to participate in the study.
Methods
The study was based on a face-to-face interview using a designed questionnaire covering sociodemographic characteristics, family history, medical history, the obstetric variables of patients, and stressful life events. Depression, anxiety, and stress were measured using the Depression Anxiety Stress Scales.
Results
In the study sample, the prevalence of depression, anxiety, and stress was 18.6%, 13.1%, and 8.7%, respectively. Young mothers and those with higher education (above secondary level) were more depressed (35.7% and 67.5%, respectively), anxious (34.9% and 68.3%, respectively), and under stress (29.7% and 62.1%, respectively) in their postpartum period. Postpartum working women were more stressed (60.7%) and anxious (51.8%), while housewives were more depressed (51.6%). Nearly half of the depressed mothers reported experiencing more than one stressful life event in their postpartum period, such as low income (41.9%; P = 0.05) or unplanned pregnancy (60.4%; P < 0.001). Unplanned pregnancy (OR = 1.9; P < 0.001) was the major significant correlate for postpartum depression, while a lack of family support (OR = 1.9; P < 0.001) was the major significant correlate for postpartum anxiety. For stress, being an older mother aged from 40 to 45 years of age (OR = 2.0; P = 0.04) and having dissatisfaction in married life (OR = 1.9; P = 0.006) were the significant correlates.
Conclusion
The study found clearly defined groups of women at risk for postpartum depression, anxiety, and stress. There was a marked association between stressful life events and postpartum depression, anxiety, and stress disorders.
Keywords: prevalence, obstetric risks, Qatar, depression, postpartum
Introduction
The postpartum period represents one of the most important life stages in which the accurate detection and treatment of psychological distress is required. The transition to new motherhood has been associated with emotional distress in up to 30% of women. 1 It involves changes in relationships between couples and within families, and is commonly a cause of additional financial stress, even among households with relatively high incomes. The impact of stressful life events and social health issues on maternal psychological morbidity such as depression, anxiety, and stress has been identified in several studies.2,3 It is widely acknowledged that symptoms of depression and anxiety co-occur and that this comorbidity may be an indicator of the severity of psychological distress.4
O’Hara and Swain5 pointed to the importance of distinguishing between depression and anxiety in postnatal periods in order to provide appropriate treatments that specifically target the symptoms and etiology of anxiety. It was suggested that anxiety may be a precursor to depression as a result of altered physiological pathways, or from the consequences of failing to manage stress.6 Stress is a distinct negative emotional state that involves chronic arousal and impaired functions7 A study by Glasheen et al8 of maternal postnatal psychological distress suggests that exposure is related to adverse psychological problems in children.
Maternity care in Qatar has improved remarkably in the last decade. The main goal of the Maternal and Child Health Section of the Primary Health Care department is to improve the health of mothers and children within the primary care setting through the provision of quality health care. They make sure that mothers and children enjoy the highest standard of physical, mental, and social well-being. Infant mortality, neonatal mortality, and postneonatal mortality rates have declined considerably compared to previous years, and the rates are much lower than the global target value set by the World Health Organization. No maternal deaths have been encountered annually. Despite these improvements, however, significant deficits in the provision of basic maternity services remain. Poor understanding, a lack of health education, and poor health behavior advice have been noted. There is a dearth of studies related to pregnancy, childbirth, and the postpartum experiences of women from Middle Eastern countries. The impact of mental health problems is one of the main causes of morbidity in our societies. It is important to identify the symptoms of each negative affective state in the postpartum period, in order to identify women who might be distressed. The Depression Anxiety Stress Scale (DASS)9 has been found to be a reliable instrument for distinguishing between the symptoms of depression, anxiety, and stress in both nonclinical and clinical samples. In the present study, the 21-item DASS (DASS-21) was selected to identify these three negative emotional states as separate phenomena. Using this instrument, the study aimed to determine the prevalence of depression, anxiety, and stress in postpartum women, and to examine the associated factors of these psychiatric disorders.
Subjects and methods
This was a cross-sectional study that included Arab women within 6 months of the postnatal period who attended primary health care centers. In order to support primary health care, 22 health centers were established covering all of the districts of Qatar. Every health center provides primary health care services to the people in the surrounding catchment areas. Antenatal programs in health centers take care of pregnant women until they reach 28 weeks of pregnancy. All deliveries take place in hospitals and women receive postpartum care and well-baby care in health centers after being discharged from the hospital.
The data were collected through a validated questionnaire with the help of qualified nurses. The recruited nurses are Arab nationals who speak and write the English and Arabic languages well. They were aware of Arabic culture and thus were able to engage with and gain the trust of the study participants if the participants were not open to discussing their problems and answering the questions. Data collection took place from January 2010 to May 2011. The sample size was determined on an a priori presumption that the prevalence rate of postpartum depression in Qatar would be more or less similar to rates found in other countries in the eastern Mediterranean, where the reported prevalence of postpartum depression is 20%, with a 95% confidence interval for a 2.5% margin of error; a sample size of 2091 subjects was required for this study. Of the 22 primary health care centers available, we randomly selected ten. Of these, eight were located in urban and two in semiurban areas of Qatar. Finally, one out of every two subjects was selected systematically using a sampling procedure. Each participant was provided with brief information about the study and was assured of strict confidentiality. A total of 2091 Arab mothers were approached; 1659 mothers agreed to participate in the study, for a response rate of 79.3%. Qualified nurses were trained to interview the patients and complete the questionnaires. The survey instrument was initially tested for validation through face-to-face interviews with 100 patients who visited the health centers. The study excluded mothers whose postnatal period was longer than 6 months and who refused to give consent to take part in the study.
The questionnaire consisted of four parts. The first part collected the patients’ sociodemographic details, the second part collected the patients’ medical and family history, the third part collected obstetric variables, and the fourth part was the diagnostic screening questionnaire. The DASS-21 questionnaire is a quantitative measure of distress on the basis of three subscales of depression, anxiety, and stress.9,10 The DASS-21 is a brief, 21-item version of the full DASS, which originally consisted of 42 items. Each of the three DASS-21 scales contains seven items representing the dimensions of depression, anxiety, and stress. The DASS consists of three self-report scales that have been designed to measure the negative emotional scales of depression, anxiety, and stress. Each question has three subscales ranging from 0 to 3; the rating scale is as follows: (a) 0 for “did not apply to me at all,” (b) 1 for “applied to me to some degree, or some of the time,” (c) 2 for “applied to me to a considerable degree, or a good part of the time,” and (d) 3 for “applied to me very much, or most of the time.” Scores for the DASS-21 subscales of depression, anxiety, and stress were derived by totaling the scores for each subscale and multiplying by two. A score of DASS ≥ 10 was used to distinguish women suffering from depression, a score of DASS ≥ 8 for anxiety disorders, and a score of DASS ≥ 15 for stress.
The study was approved by the Institutional Review Board of the Hamad Medical Corporation’s Research Ethics Committee (HMC-MRC), as well as by the equivalent Weill Cornell Medical College body (WCMC-Q). Data were analyzed using SPSS software (version 19; SPSS Inc, Chicago, IL). Student’s t-tests were used to ascertain the significance of differences between mean values of two continuous variables. A chi-square analysis was performed to test for differences in proportions of categorical variables between two or more groups. A multivariate logistic regression analysis, using the forward inclusion and backward deletion method, was used to assess the relationship between dependent and independent variables and to adjust for potential confounders, and to order the importance of risk factors (determinants) for postpartum depression, anxiety, and stress. All statistical tests were two-sided and P < 0.05 was considered statistically significant.
Results
Table 1 shows the sociodemographic characteristics of the studied postpartum women according to nationality. Of those studied, almost half were Qataris (45.9%), 40.3% were young women aged below 30 years old, 41.8% had a university degree, 53.6% were working women, and 47% had low monthly income (<QR10,000). There were statistically significant differences observed between both nationalities in terms of their sociodemographic characteristics, age groups (P < 0.001), education levels (P = 0.003), occupations (P < 0.001), and monthly household income (P = 0.002).
Table 1.
Sociodemographic characteristics of the postpartum women according to their nationality (N = 1659)
| Total N = 1659 |
Qatari (N = 762) n (%) |
Other Arab (N = 897) n (%) |
P§ value | |
|---|---|---|---|---|
| Age (mean ± SD) | 31.8 ± 5.9 | 32.4 ± 6.5 | 0.05 | |
| Maternal age (years) | ||||
| <30 | 669 (40.3) | 299 (39.2) | 370 (41.2) | <0.001 |
| 30–34 | 430 (25.9) | 209 (27.4) | 221 (24.6) | |
| 35–39 | 352 (21.2) | 196 (25.7) | 156 (17.4) | |
| 40–45 | 208 (12.5) | 58 (7.6) | 150 (16.7) | |
| Education level | ||||
| Illiterate | 110 (6.6) | 44 (5.8) | 66 (7.4) | <0.001 |
| Primary | 159 (9.6) | 95 (12.5) | 64 (7.1) | |
| Intermediate | 202 (12.2) | 65 (8.5) | 137 (15.3) | |
| Secondary | 495 (29.8) | 259 (34) | 236 (26.3) | |
| University | 693 (41.8) | 299 (39.2) | 394 (43.9) | |
| Occupation | ||||
| Housewife | 769 (46.4) | 300 (39.4) | 469 (52.3) | <0.001 |
| Working | 890 (53.6) | 462 (60.6) | 428 (47.7) | |
| Household income (QR) | ||||
| <10,000 | 779 (47.0) | 322 (42.3) | 457 (50.9) | 0.002 |
| 10,000–20,000 | 707 (42.6) | 354 (46.5) | 353 (39.4) | |
| >20,000 | 173 (10.4) | 86 (11.3) | 87 (9.7) | |
| Parental consanguinity | ||||
| Yes | 638 (38.5) | 310 (40.7) | 328 (36.6) | 0.086 |
| No | 1021 (61.5) | 452 (59.3) | 569 (63.4) | |
| Baby’s sex | ||||
| Male | 843 (50.8) | 387 (50.8) | 456 (50.8) | 0.984 |
| Female | 816 (49.1) | 375 (49.2) | 441 (49.2) | |
| No of people living in the home (mean ± SD) | 6.2 ± 3.1 | 6.2 ± 3.1 | 6.0 ± 2.8 | 0.306 |
| No of people living in the home | ||||
| <5 | 502 (30.3) | 225 (29.5) | 277 (30.9) | 0.543 |
| ≥5 | 1157 (69.7) | 537 (70.5) | 620 (69.1) | |
Note:
Two-sided P-value based on chi-square or the Student’s t-test.
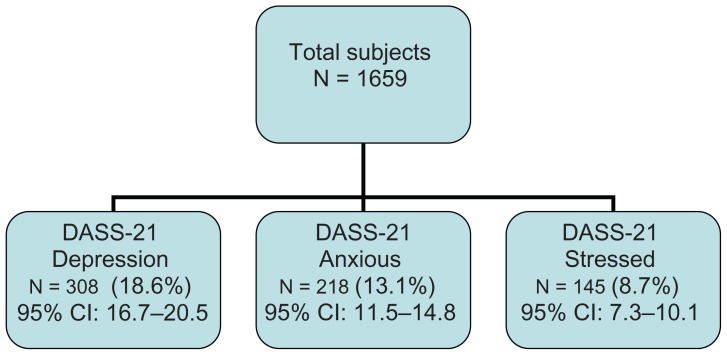
Table 2 reveals the association of depression, anxiety, and stress with socio-demographic characteristics in postpartum women. Depression (18.6%) was more prevalent among postpartum women than anxiety (13.1%) and stress (8.7%). Figure 1 shows the prevalence of depression, anxiety, and stress using the DASS-21 instrument, along with their 95% confidence interval. Postpartum women aged under 30 years were mostly affected by depressive (35.7%) and anxiety (34.9%) disorders, while stress (29.7%) was more frequent among women aged 30 to 34 years. Depression (67.5%), anxiety (68.3%), and stress (62.1%) were more frequent among postpartum women with higher education (above secondary level). Working women were more under stress (60.7%), while housewives were more depressed (51.6%) and anxious (48.2%) in their postpartum period. A significant difference was observed between depressed and nondepressed women in their occupation (P = 0.040). No significant difference was found in the sociodemographic characteristics of postpartum women with and without anxiety, while there was significant association in their age (P = 0.01) and educational level (P = 0.009) with stress.
Table 2.
Association of depression, anxiety, and stress with sociodemographic characteristic in postpartum women (n = 1659)
| Variables | Depression | P value | Anxiety | P value | Stress | P value | |||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Yes DASS ≥ 10 (n = 308) n (%) |
No DASS < 10 (n = 1351) n (%) |
Yes DASS ≥ 8 (n = 218) n (%) |
No DASS < 8 (n = 1441) n (%) |
Yes DASS ≥ 15 (n = 145) n (%) |
No DASS < 15 (n = 1514) n (%) |
||||
| Age (mean ± SD) | 32.6 ± 6.0 | 31.98 ± 6.2 | 0.114 | 32.5 ± 5.7 | 32.0 ± 6.3 | 0.348 | 33.6 ± 5.9 | 31.9 ± 6.2 | 0.002 |
| Maternal age (years) | |||||||||
| <30 | 110 (35.7) | 559 (41.4) | 0.144 | 76 (34.9) | 593 (41.2) | 0.232 | 40 (27.6) | 629 (41.5) | 0.011 |
| 30–34 | 92 (29.9) | 338 (25.0) | 58 (26.6) | 372 (25.8) | 43 (29.7) | 387 (25.6) | |||
| 35–39 | 62 (20.1) | 290 (21.5) | 56 (25.7) | 296 (20.5) | 38 (26.2) | 314 (20.7) | |||
| 40–45 | 44 (14.3) | 164 (12.1) | 28 (12.8) | 180 (12.5) | 24 (16.6) | 184 (12.2) | |||
| Education level | |||||||||
| <Secondary level | 100 (32.5) | 373 (27.6) | 0.088 | 69 (31.7) | 404 (28.0) | 0.270 | 55 (37.9) | 418 (27.6) | 0.009 |
| ≥Secondary level | 208 (67.5) | 978 (72.4) | 149 (68.3) | 1037 (72.0) | 90 (62.1) | 1096 (72.4) | |||
| Occupation | |||||||||
| Housewife | 159 (51.6) | 610 (45.2) | 0.040 | 105 (48.2) | 664 (46.1) | 0.565 | 57 (39.3) | 712 (47.0) | 0.075 |
| Working | 149 (48.4) | 741 (54.8) | 113 (51.8) | 777 (53.9) | 88 (60.7) | 802 (53.0) | |||
| Household income (QR) | |||||||||
| <10,000 | 129 (41.9) | 650 (48.1) | 0.082 | 112 (51.4) | 667 (46.3) | 0.161 | 69 (47.6) | 710 (46.9) | 0.668 |
| 10,000–20,000 | 139 (45.1) | 568 (42.0) | 80 (36.7) | 627 (43.5) | 64 (44.1) | 643 (42.5) | |||
| >20,000 | 40 (13.0) | 133 (9.8) | 26 (11.9) | 147 (10.2) | 12 (8.3) | 161 (10.6) | |||
| Sheesha smoker | |||||||||
| Yes | 20 (6.5) | 76 (5.6) | 0.556 | 16 (7.3) | 80 (5.6) | 0.292 | 9 (6.2) | 87 (5.7) | 0.821 |
| No | 288 (93.5) | 1275 (94.4) | 202 (92.7) | 1361 (94.4) | 136 (93.8) | 1427 (94.3) | |||
| Parental consanguinity | |||||||||
| Yes | 130 (42.2) | 508 (37.6) | 0.134 | 83 (38.1) | 555 (38.5) | 0.901 | 59 (40.7) | 579 (38.2) | 0.563 |
| No | 178 (57.8) | 843 (62.4) | 135 (61.9) | 886 (61.5) | 86 (59.3) | 935 (61.8) | |||
| Baby’s sex | |||||||||
| Male | 168 (54.5) | 675 (50.0) | 0.147 | 105 (48.2) | 738 (51.2) | 0.401 | 74 (51.0) | 769 (50.8) | 0.956 |
| Female | 140 (45.5) | 676 (50.0) | 113 (51.8) | 703 (48.8) | 71 (49.0) | 745 (49.2) | |||
| People living at home (mean ± SD) | 6.0 ± 2.9 | 6.1 ± 3.0 | 0.810 | 5.9 ± 2.6 | 6.1 ± 3.1 | 0.581 | 6.2 ± 2.9 | 6.1 ± 3.0 | 0.747 |
Abbreviation: DASS-21, 21-item Depression Anxiety Stress Scale.
Figure 1.
Classification of postpartum women on the DASS-21 questionnaire: prevalence and their 95% CI.
Abbreviations: CI, confidence interval; DASS-21, Depression Anxiety Stress Scales.
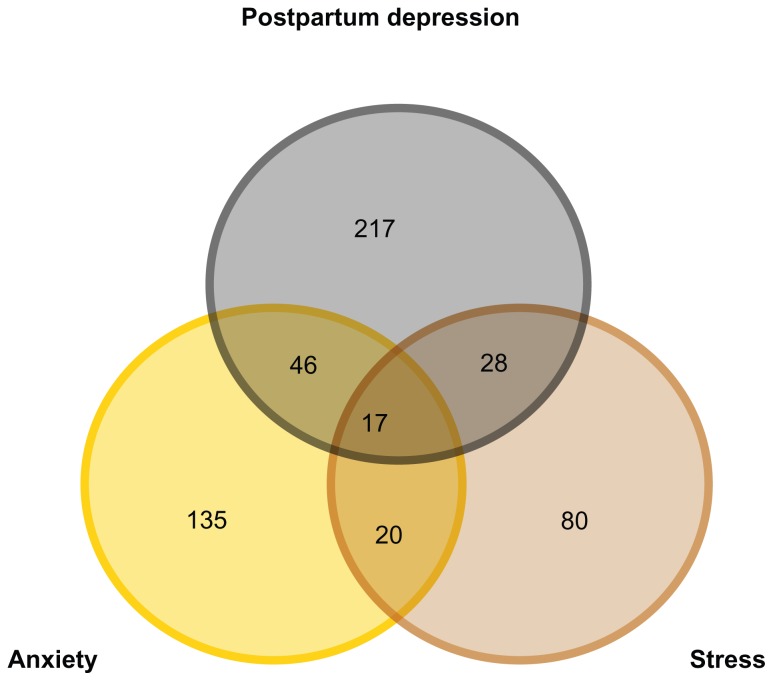
Table 3 examines the association of depression, anxiety, and stress with stressful life events in postpartum women. Nearly half of the depressed mothers reported experiencing more than one stressful life event in their postpartum period, such as low income (41.9%; P = 0.05) or unplanned pregnancy (60.4%; P < 0.001). Nearly a quarter of mothers with depression and anxiety had less family support (21.8% and 25.2%, respectively) and difficulty managing with their monthly income (23.1% and 29.4%, respectively). Three-quarters of mothers with depression (78.2%), anxiety (78.9%), and stress (75.2%) experienced poor relationships with their mothers-in-law. There was a significant association between mothers with/without depression and anxiety in their stressful life events, such as strong family support, poor marital relationships, and unplanned pregnancy (P < 0.05). Postpartum mothers under stress had significant associations with their counterparts in poor marital relationships and pregnancy complications (P < 0.05). Furthermore, the Venn diagram (Figure 2) reveals the overlap of postpartum depression, anxiety, and stress among mothers.
Table 3.
Association of depression, anxiety and stress with stressful life events in postpartum women (n = 1659)
| Depressed DASS ≥ 10 (n = 308) n (%) |
P§ value | Anxiety DASS ≥ 8 (n = 218) n (%) |
P§ value | Stress DASS ≥ 15 (n = 145) n (%) |
P§ value | |
|---|---|---|---|---|---|---|
| Relationship stressors | ||||||
| Relations with mother-in-law | ||||||
| Good | 67 (21.8) | 0.521 | 46 (21.1) | 0.442 | 36 (24.8) | 0.615 |
| Bad | 241 (78.2) | 172 (78.9) | 109 (75.2) | |||
| Strong family support | ||||||
| Yes | 241 (78.2) | 0.001 | 163 (74.8) | <0.001 | 122 (84.1) | 0.880 |
| No | 67 (21.8) | 55 (25.2) | 23 (15.9) | |||
| Satisfaction with marital life | ||||||
| Yes | 258 (83.8) | 0.004 | 177 (81.2) | <0.001 | 118 (81.4) | 0.005 |
| No | 50 (16.2) | 41 (18.8) | 27 (18.6) | |||
| Financial stressors | ||||||
| Difficult to manage within income | ||||||
| Yes | 237 (76.9) | 0.505 | 154 (70.6) | 0.003 | 35 (24.1) | 0.259 |
| No | 71 (23.1) | 64 (29.4) | 110 (75.9) | |||
| Low income | ||||||
| Yes | 129 (41.9) | 0.048 | 112 (51.4) | 0.161 | 69 (47.6) | 0.874 |
| No | 179 (58.1) | 106 (48.6) | 76 (52.4) | |||
| Maternal stressors | ||||||
| Planned pregnancy | ||||||
| Yes | 122 (39.6) | <0.001 | 98 (45.0) | 0.006 | 78 (53.8) | 0.958 |
| No | 186 (60.4) | 120 (55.0) | 67 (46.2) | |||
| Pregnancy complications | ||||||
| Yes | 100 (32.5) | 0.887 | 75 (34.4) | 0.440 | 61 (42.1) | 0.007 |
| No | 208 (67.5) | 143 (65.6) | 84 (57.9) | |||
| Parity | ||||||
| Primarous | 35 (11.4) | 0.807 | 28 (12.8) | 0.342 | 16 (11.0) | 0.979 |
| Multiparous | 273 (88.6) | 190 (87.2) | 129 (89.0) | |||
Notes: DASS-21 = 21-item Depression, Anxiety, Stress Scale;
comparison between depressed vs nondepressed, anxious vs nonanxious, stressed vs nonstressed.
Figure 2.
Venn diagram showing the overlapping of postpartum depression, anxiety, and stress among mothers in Qatar (N = 1659).
Notes: Postpartum depression, 308; anxiety, 218; stress, 145.
Table 4 shows the postpartum depression correlates of anxiety and stress using a multivariate analysis. Unplanned pregnancy (odds ratio [OR] = 1.9; P < 0.001), a lack of family support (OR = 1.6; P = 0.005), and housewives (OR = 1.6; P = 0.001) were the most significant correlates for postpartum depression, while a lack of family support (OR = 1.9; P < 0.001) and dissatisfaction in married life (OR = 1.6; P = 0.02) were the significant correlates for postpartum anxiety. Delivery by cesarean section was a significant factor of postpartum depression (OR = 1.4; P = 0.004) and anxiety (OR = 1.5; P = 0.012). For stress, being an older mother (40 to 45 years old; OR = 2.0, P = 0.04) and dissatisfaction in married life (OR = 1.9; P = 0.006) were the significant correlates. Furthermore, the Venn diagram in Figure 2 reveals the overlap of postpartum depression, anxiety, and stress among mothers.
Table 4.
Correlates of postpartum depression, anxiety, and stress in Qatar using multivariate analysis (n = 1659)
| Adj. OR (95% CI) | P value | |
|---|---|---|
| Depression | ||
| Education level | ||
| ≥Secondary | 1 ref | 0.006 |
| <Secondary | 1.5 (1.1–2.0) | |
| Occupation | ||
| Working | 1 ref | 0.001 |
| Housewife | 1.6 (1.2–2.1) | |
| Family support | ||
| Yes | 1 ref | 0.005 |
| No | 1.6 (1.2–2.3) | |
| Nature of pregnancy | ||
| Planned | 1 ref | <0.001 |
| Unplanned | 1.9 (1.5–2.6) | |
| Type of delivery | ||
| Vaginal | 1 ref | 0.004 |
| C-section | 1.4 (1.1–1.9) | |
| Anxiety | ||
| Family support | ||
| Yes | 1 ref | <0.001 |
| No | 1.9 (1.3–2.8) | |
| Nature of pregnancy | ||
| Planned | 1 ref | 0.035 |
| Unplanned | 1.4 (1.1–1.8) | |
| Type of delivery | ||
| Vaginal | 1 ref | 0.012 |
| C-section | 1.5 (1.1–2.0) | |
| Marital satisfaction | ||
| Yes | 1 ref | 0.018 |
| No | 1.6 (1.1–2.5) | |
| Stress | ||
| Age | ||
| <30 | 1 ref | 0.043 |
| 30–34 | 1.5 (1.1–2.5) | |
| 35–39 | 1.6 (1.1–2.6) | |
| 40–45 | 2.0 (1.2–3.5) | |
| Education level | ||
| ≥Secondary | 1 ref | 0.043 |
| <Secondary | 1.5 (1.1–2.2) | |
| Marital satisfaction | ||
| Yes | 1 ref | 0.006 |
| No | 1.9 (1.2–3.1) | |
Note: Adjusted OR are adjusted for all the variables present in the table.
Abbreviation: Ref, reference category.
Table 5 compares the global prevalence rates of postpartum depression.
Table 5.
Prevalence rate for postpartum depression according to ethnicity: global comparison
| Country | Age group | Sample size | Prevalence rate (%) | Year | Reference |
|---|---|---|---|---|---|
| Australia | 16–35 years | 4366 | 17.4% | 2010 | Yelland et al3 |
| Australia | 18–44 years | 80 | 24.7% | 2006 | Miller et al12 |
| Australia | 17–36 years | 52 | 25.1% | 2007 | Phillips et al24 |
| Brazil | 14–47 years | 271 | 20.7% | 2008 | Tannous et al25 |
| Brazil | 3–31 years | 410 | 19.0% | 2000 | Moraes et al26 |
| Goa, India | 18–37 years | 59 | 23% | 2001 | Patel et al27 |
| Pakistan | 17–40 years | 149 | 36% | 2006 | Husain et al19 |
| Morrocco | 18–44 years | 144 | 18.7% | 2005 | Agoub et al28 |
| Oklahoma | 18–35 years | 5586 | 26% | 2000–2006 | Lincoln et al29 |
| Turkey | 15–44 years | 1447 | 29.0% at 0–2 months 36.6% at 3–6 months 36.0% at 7–12 months 42.7% at >13 months |
2004 | Bugdayci et al30 |
| Dubai | 25–34 years | 90 | 18.0% | 1997 | Abou Saleh and Ghubash31 |
| Bangladesh | 17–41 years | 361 | 33% | 2009 | Gausia et al32 |
| USA | 17–47 years | 192 | 23.4% | 1995 | Hobfoll et al33 |
| Qatar (current study) | 18–45 years | 1659 | 18.6% | 2010–2011 | Bener et al |
Discussion
Having a child is a time of biological, psychological, and social change in a woman’s life. These changes can contribute to personal growth and happiness, but may also predispose women to emotional distress. In the present study, the DASS-21 instrument was used to assess the comorbidity of the three negative emotional states of depression, anxiety, and stress as separate phenomena in postpartum women. The study identified a higher prevalence of depression (18.6%) in Arab women during their postpartum period compared to the prevalence of anxiety (13.1%) and stress (8.7%). A study by Matthey et al11 showed a similar psychological morbidity, with 17% experiencing depression and 13% experiencing anxiety. Also, a recent population-based survey of Australian women3 reported rates of 12.7% for anxiety and 17.4% for depression. These study results consistently suggest that more than 10% of mothers suffer from depression, anxiety, and stress in the early postpartum period. A lower prevalence was observed in a study12 using the DASS-21, which found that 7% of women had symptoms of anxiety and depression during their postpartum period. It is widely acknowledged8 that the 21 DASS items measure the severity of symptoms common to anxiety and depression in postpartum women.
Depression is a mood disorder that manifests itself in various ways. According to Beck et al,13 depression can negatively influence a person’s motivation and affect their cognition and physiology. The prevalence of postpartum depression in the present study is higher than those reported in countries such as England,14 Japan,15 and Hong Kong,16 but similar to rates reported in other Arab countries such as Morocco,17 Lebanon, 18 and the UAE.19 Postpartum depression is an important public health problem that has negative effects on the mother, the infant, and the whole family. Affonso et al20 found that postpartum depressive symptoms were lowest among European and Australian women, and highest among mothers from non-Western countries like Taiwan and India. This shows a higher prevalence of postpartum depression and anxiety in women from Asian countries compared to non-Western populations. The higher prevalence of psychological distress in Asian women might be due to cultural differences, such as relationships with in-laws and the influence of extended family members.
In the studied postpartum women, women who reported more depressive disorders were more likely to be under 30 years old (35.7%), housewives (51.6%), women who have at least completed their secondary education or higher (67.5%), or have low income (<QR10,000) (41.9%). A similar pattern was observed in women who reported anxiety disorders, except for occupation; women aged under 30 years reported in at 34.9%, women who completed their secondary education and above reported in at 68.3%, and low income women reported in at 51.4%, whereas stress was more frequent among women in the 30- to 34-year-old age group (29.7%). Anxiety (51.8%) and stress (60.7%) disorders were observed more among working women in their postpartum period. Further studies11,21 have identified sociodemographic associations with postpartum depression, anxiety, and stress disorders.
The study analysis revealed that the studied postpartum women experienced a range of stressful live events, such as relationship, financial, and maternal stressors. It was reported by Baker et al22 that a history of marital discord, a poor parenting relationship experienced during childhood, low self-esteem, low socioeconomic status, unwanted pregnancy, and stressful life events during pregnancy have been associated with postpartum mental disorders. More than three-quarters of postpartum mothers with depression (78.2%), anxiety (78.9%), and stress (75.2%) reported poor relationships with their mothers-in-law. Nearly half of the postpartum mothers with depression and anxiety reported experiencing more than one stressful life event, such as low income (58.1% and 48.6%, respectively) and unplanned pregnancy (60.4% and 55%, respectively), with a significant association with their counterparts. The major significant correlates of depression were unplanned pregnancy, lack of family support, and mothers as housewives, whereas for anxiety disorders, lack of family support and dissatisfaction in married life were the significant correlates. Older mothers (40 to 45 years old) and marital dissatisfaction were the major significant correlates for stress disorders. These study results reveal that the depression, anxiety and stress, the quality of relationships with husbands, and family support are all significantly intercorrelated. There was a nearly two-fold increase in the odds of reporting depression, anxiety, and stress in women experiencing one to two stressful life events, confirming the marked association between stressful life events and emotional distress in their postpartum period. The most common life events that affected our postpartum mothers were unplanned pregnancy and poor relationships with their mothers-in-law. International studies2,23 have also identified similar associations between stressful life events and psychological ill health.
The current study results make us believe that the provision of adequate postpartum care is crucial in the identification of emotional distress. Considering the high prevalence of psychological morbidity during the postpartum period of mothers and their association with social health issues, health care personnel need to be alert to a wide range of social health issues. The present study recommends education programs for health care professionals to increase their awareness of postpartum mental illness. Health care providers should provide women with opportunities and encouragement to talk in-depth about their feelings, including stressful life events. Antenatal screening programs can identify women who are at risk of mental disorders.
The limitations of the study need to be noted. The study did not assess the prevalence of stress, anxiety, and depression in the studied women during their antenatal period. Also, information like paternal stress, previous psychiatric history, and family histories of psychiatric illnesses were not included in the questionnaire. Approximately 20% of the approached mothers declined to participate, and these women may have had a higher frequency of risk factors.
Conclusion
In general, our study findings are consistent with the results observed in the literature. Young mothers presented higher levels of postnatal distress, including depression, anxiety, and stress. Sociodemographic factors such as younger ages, higher education levels, and lower household income were associated with depression, anxiety, and stress disorders. Working women were more affected by anxiety and stress disorders, whereas most of the depressed mothers were housewives. Similarly, stressful life events were associated with the development of probable postpartum depression, anxiety, and stress disorders. Identifying correlates of postnatal distress can lead to more detailed investigation to identify contributory factors for such distress. Finally, preventive strategies designed to attenuate or eliminate the impact of such contributory factors can substantially improve the emotional well-being of women in the vulnerable postnatal period.
Acknowledgments
This study was generously supported and funded by the Qatar National Research Fund (QNRF NPRP 30-6-7-44) and the Weill Cornell Medical College Institutional Review Board’s Ethical Approval (WCMC-Q #2011-0008). The authors would like to thank the Hamad Medical Corporation for their support and ethical approval (HMC MRC #10119/10).
Footnotes
Author contributions
AB contributed to the research idea design of this study, and to the collection and analysis of the data and the preparation of the manuscript. LMG and JS contributed to the design and preparation of the manuscript. All authors have read and approved the final version of the manuscript.
Disclosure
The authors declare that they have no competing interests in this work.
References
- 1.Johnson J, Weissman MM, Klerman GL. Service utilization and social morbidity associated with depressive symptoms in the community. JAMA. 1992;267(11):1478–1483. [PubMed] [Google Scholar]
- 2.Braveman P, Marchi K, Egerter S, et al. Poverty, near poverty, and hardship around the time of pregnancy. Matern Child Health J. 2010;14(1):20–35. doi: 10.1007/s10995-008-0427-0. [DOI] [PubMed] [Google Scholar]
- 3.Yelland J, Sutherland G, Brown SJ. Postpartum anxiety, depression and social health: findings from a population-based survey of Australian women. BMC Public Health. 2010;10:771. doi: 10.1186/1471-2458-10-771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Austin MP, Hadzi-Pavlovic D, Priest SR, et al. Depressive and anxiety disorders in the postpartum period: how prevalent are they and can we improve their detection? Arch Womens Ment Health. 2010;13(5):395–401. doi: 10.1007/s00737-010-0153-7. [DOI] [PubMed] [Google Scholar]
- 5.O’Hara MW, Swain AM. Rates and risk of postpartum depression – a meta-analysis. Int Rev Psychiatry. 1996;8(1):37–54. [Google Scholar]
- 6.Heron J, O’Connor TG, Evans J, Golding J, Glover V ALSPAC Study Team. The course of anxiety and depression through pregnancy and the postpartum in a community sample. J Affect Disord. 2004;80(1):65–73. doi: 10.1016/j.jad.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- 8.Glasheen C, Richardson GA, Fabio A. A systematic review of the effects of postnatal maternal anxiety on children. Arch Womens Ment Health. 2010;13(1):61–74. doi: 10.1007/s00737-009-0109-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crawford JR, Henry JD. The Depression Anxiety Stress Scales (DASS): normative data and latent structure in a large non-clinical sample. Br J Clin Psychol. 2003;42(Pt 2):111–131. doi: 10.1348/014466503321903544. [DOI] [PubMed] [Google Scholar]
- 10.Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd ed. Sydney, Australia: Psychology Foundation; 1995. [Google Scholar]
- 11.Matthey S, Barnett B, Howie P, Kavanagh DJ. Diagnosing postpartum depression in mothers and fathers: whatever happened to anxiety? J Affect Disord. 2003;74(2):139–147. doi: 10.1016/s0165-0327(02)00012-5. [DOI] [PubMed] [Google Scholar]
- 12.Miller RL, Pallant JF, Negri LM. Anxiety and stress in the postpartum: is there more to postnatal distress than depression? BMC Psychiatry. 2006;6:12. doi: 10.1186/1471-244X-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 14.Evans J, Heron J, Francomb H, Oke S, Golding J Avon Longitudinal Study of Parents and Children Study Team. Cohort study of depressed mood during pregnancy and after child birth. BMJ. 2001;323:257. doi: 10.1136/bmj.323.7307.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kitamura T, Yoshida K, Okano T, et al. Multicentre prospective study of perinatal depression in Japan: incidence and correlates of antenatal and postnatal depression. Arch Womens Ment Health. 2006;9(3):121–130. doi: 10.1007/s00737-006-0122-3. [DOI] [PubMed] [Google Scholar]
- 16.Lau Y, Keung DW. Correlates of depressive symptomatology during the second trimester of pregnancy among Hong Kong Chinese. Soc Sci Med. 2007;64(9):1802–1811. doi: 10.1016/j.socscimed.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 17.Chaaya M, Campbell OM, El Kak F, Shaar D, Harb H, Kaddour A. Postpartum depression: prevalence and determinants in Lebanon. Arch Womens Ment Health. 2002;5(2):65–72. doi: 10.1007/s00737-002-0140-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alami KM, Kadri N, Berrada S. Prevalence and Psychosocial correlates of depressed mood during pregnancy and after childbirth in a Moroccan sample. Arch Womens Ment Health. 2006;9(6):343–346. doi: 10.1007/s00737-006-0154-8. [DOI] [PubMed] [Google Scholar]
- 19.Husain N, Bevc I, Husain M, Chaudhry IB, Atif N, Rahman A. Prevalence and social correlates of postnatal depression in a low income country. Arch Womens Ment Health. 2006;9(4):197–202. doi: 10.1007/s00737-006-0129-9. [DOI] [PubMed] [Google Scholar]
- 20.Affonso DD, De AK, Horowitz JA, Mayberry LJ. An international study exploring levels of postpartum depressive symptomatology. J Psychosom Res. 2000;49(3):207–216. doi: 10.1016/s0022-3999(00)00176-8. [DOI] [PubMed] [Google Scholar]
- 21.Beck CT. Predictors of postpartum depression: an update. Nurs Res. 2001;50(5):278–285. doi: 10.1097/00006199-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Baker L, Cross S, Greaver L, Wei G, Lewis R Healthy Start CORPS. Prevalence of postpartum depression in a native American population. Matern Child Health J. 2005;9(1):21–25. doi: 10.1007/s10995-005-2448-2. [DOI] [PubMed] [Google Scholar]
- 23.Dennis CL, Janssen P, Singer J. Identifying women at-risk for postpartum depression in the immediate postpartum period. Acta Psychiatr Scand. 2004;110(5):338–346. doi: 10.1111/j.1600-0447.2004.00337.x. [DOI] [PubMed] [Google Scholar]
- 24.Phillips J, Sharpe L, Matthey S. Rates of depressive and anxiety disorders in a residential mother-infant unit for unsettled infants. Aust N Z J Psychiatry. 2007;41(10):836–842. doi: 10.1080/00048670701579108. [DOI] [PubMed] [Google Scholar]
- 25.Tannous L, Gigante LP, Fuchs SC, Busnello ED. Postnatal depression in Southern Brazil: prevalence and its demographic and socioeconomic determinants. BMC Psychiatry. 2008;8:1. doi: 10.1186/1471-244X-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moraes IGS, Pinheiro RT, da Silva RA, Horta BL, Paulo Luis Rosa Sousa PLR, Faria AD. Prevalence of postpartum depression and associated factors. Rev Saude Publica. 2006;40(1):65–70. doi: 10.1590/s0034-89102006000100011. [DOI] [PubMed] [Google Scholar]
- 27.Patel V, Rodrigues M, DeSouza N. Gender, poverty, and postnatal depression: a study of mothers in Goa, India. Am J Psychiatry. 2002;159(1):43–47. doi: 10.1176/appi.ajp.159.1.43. [DOI] [PubMed] [Google Scholar]
- 28.Agoub M, Moussaoui D, Battas O. Prevalence of postpartum depression in a Moroccan sample. Arch Womens Ment Health. 2005;8(1):37–43. doi: 10.1007/s00737-005-0069-9. [DOI] [PubMed] [Google Scholar]
- 29.Lincoln A, Feyerharm R, Damron P, DeVault M, Lorenz D, Dooley S. Maternal depression after delivery in Oklahoma. J Okla State Med Assoc. 2008;101(12):307–311. [PubMed] [Google Scholar]
- 30.Bugdayci R, Sasmaz CT, Tezcan H, Kurt AO, Oner S. A cross-sectional prevalence study of depression at various times after delivery in Mersin province in Turkey. J Womens Health (Larchmt) 2004;13(1):63–68. doi: 10.1089/154099904322836465. [DOI] [PubMed] [Google Scholar]
- 31.Abou-Saleh MT, Ghubash R. The prevalence of early postpartum psychiatric morbidity in Dubai: a transcultural perspective. Acta Psychiatr Scand. 1997;95(5):428–432. doi: 10.1111/j.1600-0447.1997.tb09657.x. [DOI] [PubMed] [Google Scholar]
- 32.Gausia K, Fisher C, Ali M, Oosthuizen J. Antenatal depression and suicidal ideation among rural Bangladeshi women: a community-based study. Arch Womens Ment Health. 2009;12(5):351–358. doi: 10.1007/s00737-009-0080-7. [DOI] [PubMed] [Google Scholar]
- 33.Hobfoll SE, Ritter C, Lavin J, Hulsizer MR, Cameron RP. Depression prevalence and incidence among inner-city pregnant and postpartum women. J Consult Clin Psychol. 1995;63(3):445–453. doi: 10.1037//0022-006x.63.3.445. [DOI] [PubMed] [Google Scholar]