Abstract
We aimed to examine outcomes, moderators and mediators of a preventive school-based mental health intervention implemented by paraprofessionals in a war-affected setting in northern Sri Lanka. A cluster randomized trial was employed. Subsequent to screening 1,370 children in randomly selected schools, 399 children were assigned to an intervention (n=199) or waitlist control condition (n=200). The intervention consisted of 15 manualized sessions over 5 weeks of cognitive behavioral techniques and creative expressive elements. Assessments took place before, 1 week after, and 3 months after the intervention. Primary outcomes included post-traumatic stress disorder (PTSD), depressive, and anxiety symptoms. No main effects on primary outcomes were identified. A main effect in favor of intervention for conduct problems was observed. This effect was stronger for younger children. Furthermore, we found intervention benefits for specific subgroups. Stronger effects were found for boys with regard to PTSD and anxiety symptoms, and for younger children on pro-social behavior. Moreover, we found stronger intervention effects on PTSD, anxiety, and function impairment for children experiencing lower levels of current war-related stressors. Girls in the intervention condition showed smaller reductions on PTSD symptoms than waitlisted girls. We conclude that preventive school-based psychosocial interventions in volatile areas characterized by ongoing war-related stressors may effectively improve indicators of psychological wellbeing and posttraumatic stress-related symptoms in some children. However, they may undermine natural recovery for others. Further research is necessary to examine how gender, age and current war-related experiences contribute to differential intervention effects.
Keywords: Armed conflict, political violence, post-traumatic stress disorder, anxiety, depression, school-based intervention, prevention, Sri Lanka
The civil war in Sri Lanka, which ended in 2009 when government security forces claimed victory over the Liberation Tigers of Tamil Eelam, has had an extensive impact on the mental health of the population 1,2. A number of epidemiological studies have documented the high prevalence of mental disorders among children in Sri Lanka. Two studies in the northeast of the country found prevalence rates of 25% and 30% for post-traumatic stress disorder (PTSD) and 20% for major depression 3,4. In addition, researchers have observed increased psychological distress among the general population and detrimental impacts of the long-term conflict on social structures, including family and community functioning in the north and east of Sri Lanka 5,6.
Despite this evidence of augmented mental health and psychosocial problems, resources for mental health in Sri Lanka remain scarce and centralized, as is common in low- and middle-income countries (LMIC) 7. Given this existing gap in health services, there is a need for easily accessible interventions that can rapidly be disseminated to larger groups of children. To this end, school-based interventions implemented by trained non-specialized staff have often been advocated 8,9,10.
A recent paper reviewed the evidence base of mental health and psychosocial support interventions for children in humanitarian settings 11. It reported two separate meta-analyses, focused on the most commonly used outcomes measured across studies: PTSD and internalizing symptoms. The first meta-analysis focused on four randomized controlled studies evaluating outcomes of school-based interventions for war-affected children and adolescents in Bosnia and Herzegovina 12, Indonesia 13,14, Nepal 15, and the Palestinian Territories 16, as well as a school-based intervention for children affected by the 2004 Tsunami in Sri Lanka 17. This meta-analysis did not find an overall effect for PTSD symptoms, and very high statistical heterogeneity of intervention effects on PTSD across studies. The second meta-analysis, including the studies in the first meta-analysis, as well as interpersonal group psychotherapy and creative play with adolescents affected by armed conflict in northern Uganda 18, and a group psychosocial intervention with mothers of young children affected by armed conflict in Bosnia Herzegovina 19, did show significant intervention benefits for internalizing symptoms. Given the high prevalence of mental health problems in settings of armed conflict and the increasing popularity of interventions for war-affected children in LMIC, more rigorous studies are clearly needed to assess outcomes of interventions.
This study aimed to evaluate the outcomes of a school-based secondary prevention intervention for children affected by ongoing war in northern Sri Lanka. We hypothesized that the intervention would lead to improved child mental health. In addition, we were interested in moderators and mediators of the intervention. Since school-based interventions for war-affected children have sorted diverse effects, examining moderators presents an important strategy to identify for whom and under what conditions intervention is most effective. Study of mediators is aimed at identifying why and how interventions have effects 20,21.
Gender and age have previously been shown to moderate effects of school-based interventions for children affected by armed conflict. In Indonesia, intervention was effective for PTSD and function impairment only for girls, whereas it was effective with regard to maintaining hope for both boys and girls 13,14. In Nepal, no main effects were found, but intervention effects were found for boys on general psychological difficulties and aggression and for girls on pro-social behavior. In addition, an age effect was observed, such that older children in the intervention condition showed larger improvements with respect to feelings of hope. Age and gender effects were also identified in the Palestinian Territories, where a school-based intervention showed treatment effects on diverse emotional and behavioral outcomes with school-aged children, particularly boys. For older children, intervention effects were only observed with adolescent girls 16.
Furthermore, the importance of past exposure to violence in relation to current experience of war-related stressors for mental health has been debated, but not assessed in evaluation studies among children 22,23,24. Several studies have shown that current experience of war-related “daily stressors” (e.g., lack of access to basic needs, domestic and neighborhood violence, substance use) partly mediated the association between exposure to violence events (witnessing/experiencing murders, bomb blasts, sexual violence, getting caught in crossfires, etc.) and PTSD symptomatology 25,26. Given this mediating role identified in cross-sectional surveys, we expected that intervention would be less effective in reducing psychological complaints for those experiencing continuing high levels of war-related daily stressors (i.e., a moderating relationship in this evaluation study).
Finally, we were interested in coping behavior as a potential mediator of intervention effects. Previous research with war-affected children has generally confirmed a relation between coping behavior and psychological symptoms, although it is not clear which specific coping styles (e.g., emotion-focused vs. problem-focused) are most protective in such settings 27. The evaluated intervention (described below) specifically aimed to enhance coping behavior. We expected that the intervention would increase the number of coping methods used by children, as well as their satisfaction with these coping methods, and that these increases would in turn be associated with decreases in psychological symptoms.
METHODS
Setting and participants
We collected data in the Tellippalai and Uduvil divisions of the Jaffna district in northern Sri Lanka, between September 2007 and March 2008. In August 2006, a peace agreement that had been observed since 2002 was abandoned, followed by closure of the only land road into the Jaffna peninsula. The subsequent period was characterized by rationed food and other essential supplies, curfews, road blocks, disappearances, extrajudicial killings, and skirmishes between the army and Liberation Tigers. Based on experiences in previous periods of intensified armed conflict in the region, we expected that safety of participants and staff, and continuation of schooling, could be guaranteed in this specific area.
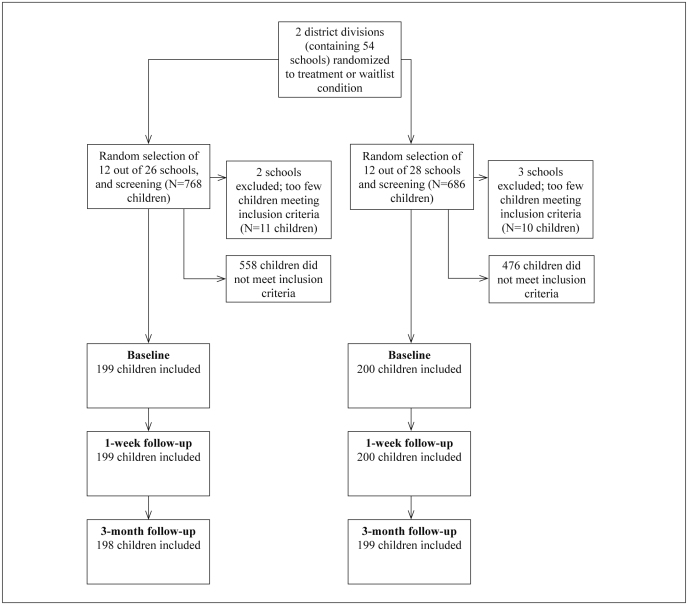
We implemented a cluster randomized trial rather than an individually randomized trial to avoid contamination of the intervention within schools. We used a two-step randomization procedure. First, within district divisions, we randomly allocated each division to either the intervention or waitlist control condition (see Figure 1). Second, we randomly selected schools for inclusion in the study. All schools on the government-provided list were eligible.
Figure 1 Participant flow diagram.
In randomly selected schools, we screened children in grades 4 through 7 (ages 9-12) for meeting inclusion criteria using the Child Psychosocial Distress Screener (CPDS), a screening instrument with established cross-cultural construct validity that was developed for use with children affected by armed conflict 28,29. In accordance with the secondary prevention aims of the intervention (i.e., targeting symptoms of psychological distress and common mental disorders, and strengthening protective factors), this 7-item screening procedure assesses, with both children and teachers: a) the existence of risk factors (i.e., reporting exposure to war-related events, distress during such exposure, current psychological symptoms, and affected school functioning); b) the absence of protective factors (i.e., reporting a lack of social support and coping capacity). No children were excluded after meeting inclusion criteria, and a small group of children reporting severe mental problems during screening were provided individual supportive counseling in addition to being enrolled in the study (N=19, 4.8%).
We based our selection of 12 schools per study condition on an a priori power calculation. We calculated effect sizes of 1.10 for PTSD and 0.78 for depressive symptoms in earlier intervention outcome studies which applied the same instruments 30,31. To detect changes with the same effect sizes, with β equal to .02 (2-sided) and α equal to .95, we calculated that we needed a minimum of 18 and 35 children (for PTSD and depressive symptoms respectively) per study condition. To account for intracluster correlation, we multiplied 35 by 1 + (m–1)ρ, with m=30 (average cluster size), ρ =0.1 (intracluster correlation), and a power of 95%, resulting in an appropriate sample size of 137. To compensate attrition, we aimed at oversampling to reach approximately 180 children per study condition. We estimated that at least one group of 15 children per school would meet inclusion criteria after screening, and therefore decided to sample 12 schools per study condition.
Intervention
The mental health intervention consisted of 15 sessions over 5 weeks of a school-based group intervention implemented by locally identified non-specialized personnel trained and supervised in implementing the intervention for one year prior to the study. Interventionists had at least a high school diploma and were selected for their affinity and capacity to work with children as demonstrated in role-plays and interviews.
The manualized intervention consists of cognitive behavioral techniques (psychoeducation, strengthening coping, and guided exposure to past traumatic events through drawing) and creative expressive elements (cooperative games, structured movement, music, drama, and dance) with groups of around 15 children, aimed at decreasing symptoms of common mental disorders and strengthening protective factors 32.
The intervention follows a specific structure within and between sessions, with the following foci: information, safety, and control in week 1 (sessions 1-3); stabilization, awareness and self-esteem in week 2 (sessions 4-6); the trauma narrative in week 3 (sessions 7-9); resource identification and coping skills in week 4 (sessions 10-12); and reconnection with the social context and future planning in week 5 (sessions 13-15).
Each session is divided into four parts, starting and ending with structured movement, songs and dance with the use of a “parachute” (i.e., large circular colored fabric). The second part is based on a “central activity” focused on the main theme of that week (e.g., a drama exercise to identify social supports in the environment, or drawing of traumatic events), and the third part is a cooperative game (i.e., a game in which all children have to participate in order to promote group cohesion).
The intervention was part of a larger public mental health program for children affected by war, including primary and tertiary prevention approaches.
Outcome measures
All standardized outcome measures were selected based on a preliminary qualitative study, which encompassed 18 key informant interviews, 20 focus group discussions, and 23 semi-structured individual interviews with children and family members identified as having mental health complaints 33. Qualitative data collection was also applied to construct new measures. Standardized rating scales were translated to Tamil using a translation monitoring form, which provides a structured method to prepare instruments for transcultural research 34.
Primary outcome measures
PTSD symptoms were assessed with the Child PTSD Symptom Scale (CPSS), a 17-item scale which measures symptoms of PTSD according to the DSM-IV with a 4-point response scale (range 0-51) 35. Internal reliability (Cronbach alpha) in our sample was .84. Depressive symptoms were examined with the 18-item Depression Self-Rating Scale (DSRS), which employs a 3-point response scale (range 0-36) 36. Internal reliability in our sample was .65. We assessed anxiety symptoms with the 5-item version of the Screen for Anxiety Related Emotional Disorders (SCARED-5; 3-point response scale, range 0-10) 37. Internal reliability in our sample was .52.
Secondary outcome measures
As a broad mental health outcome measure, we used the 25-item Strengths and Difficulties Questionnaire self-report version, which was available in Tamil and was validated in the Jaffna district 38. As suggested by the developers, the four subscales that refer to psychological difficulties were summed into an overall total difficulties score (range 0-40, internal reliability .78), and a fifth 5-item subscale assessed pro-social behavior (range 0-10, internal reliability .60).
Using the qualitative interviews of the preliminary study, we listed and categorized all psychological complaints reported by participants, and identified two groups of symptoms not well covered by standardized rating scales: supernatural complaints (being affected by evil spirits, witchcraft or demons) and war-related conduct problems (use of violence as a way to solve conflicts, imitating soldiers/rebels). Selecting the most commonly mentioned complaints, we constructed 6-item and 8-item scales, both with a 4-point answering format (range 0-18 and 0-24, internal reliability .58 and .61, respectively).
We also constructed a scale to assess function impairment 39. Following brief participant observation, collection of diaries, and focus groups with children, ten activities were selected that represented children’s daily lives with respect to individual (e.g., hygiene, sleep), family (e.g., chores), peer (e.g., play), school (e.g., participation, homework), community (e.g., helping elders), and religious (e.g., worship at home) activities. Children were asked if they felt impaired in these activities on a 4-point answering format (range 0-30, internal reliability .80).
Moderators and mediators
Gender and age (in years) were assessed as part of the demographics section of the questionnaire. Exposure to violence and daily stressors were assessed with a locally constructed rating scale. After free listing major war-related adversities with 20 local humanitarian staff, we selected the most mentioned war-related events that children could be exposed to. This resulted in a dichotomous (yes/no) rating scale with 10 items reflecting past war exposure (range 0-10, e.g., seeing bomb blasts, witnessing murders, experiencing or witnessing torture, sexual violence) and 11 items assessing exposure to current war-related daily stressors (range 0-11, e.g., basic needs not being met, domestic violence, alcohol abuse, separation from family members, displacement).
Coping repertoire and satisfaction were assessed with the child-rated Kidcope (Younger Version for ages 7-2) 40. The Kidcope contains 15 questions concerning 10 coping strategies, which were assessed in relation to an imagined school problem (working hard but receiving bad grades) by asking which coping strategies were used (dichotomous items: yes/no) and how children rated their satisfaction with employed coping methods on a 3-point scale (1. not at all, 2. a little, 3. a lot; range 0-30; coping repertoire internal reliability .77).
Procedures and ethics
All instruments were interview-administered by a group of assessors not involved in service delivery, in a private environment at schools. These assessors were trained in a 3-week period in competently administrating rating scales. Assessors were not informed about which schools received intervention.
Before starting research activities, we discussed our plans with the local leadership, schools, and parents in community meetings. All children and parents provided written consent after being explained the purpose and proceedings of research activities. Formal ethical permission was granted by the VU University international review board and the Jaffna district education committee.
Statistics
To assess comparability of study conditions, demographic and mental health indicators at baseline were compared by ?2 with continuity correction or Fisher exact test for frequencies, and independent sample t-tests for continuous measures.
Longitudinal changes on outcome measures were examined through latent growth curve modeling (LGCM) in a structural equation modeling framework 41. Conditional growth models were used to estimate the intervention main effect and to model moderating effects while controlling for main effects accordingly. All models controlled for clustering at the school level. LGCM was conducted in two steps. In a first step we modeled growth curves, using 1, 6 and 18 weeks as time points, and estimated the effect of intervention on changes over time. In the second step we added moderators and their main effects to explore potential variations in intervention effects.
Because only two participants had missing data on outcome measures at the third assessment (lost to follow-up at 18 weeks), we conducted a complete case analysis, excluding the two participants with missing data.
RESULTS
Characteristics at baseline
We compared demographic characteristics (gender, religion, type of house, occupation caregiver, household size), exposure to violence, ongoing war-related stressors, and scores on outcome measures, and found no statistically significant differences between study conditions (Table 1). The sample consisted of more boys (61.4%) than girls, was dominantly of Hindu religion (81.0%), and children were between 9 and 12 years old (mean 11.03±1.05).
Table 1.
Table 1 Baseline comparison of scores on exposure and outcome measures
| Treatment condition (N=199) | Waitlist condition (N=200) | t(df=397) | p | ICC | |
| Mean±SD | Mean±SD | ||||
| Exposure | 1.93±1.34 | 1.91±1.45 | .141 | .888 | -.006 |
| Ongoing stressors | 4.05±1.94 | 4.16±1.98 | -.559 | .576 | .174 |
| Screening | 6.27±1.44 | 6.34±1.44 | -.476 | .634 | .050 |
| PTSD complaints | 15.03±8.89 | 15.70±9.12 | -.748 | .455 | .002 |
| Depressive complaints | 8.39±4.54 | 8.56±4.37 | -.388 | .698 | .000 |
| Anxiety complaints | 3.29±2.13 | 3.17±2.16 | .566 | .571 | -.005 |
| Supernatural complaints | 2.21±2.59 | 1.97±1.92 | 1.034 | .302 | .008 |
| Behavioral complaints | 2.00±2.84 | 1.99±2.23 | .039 | .969 | -.029 |
| Total difficulties (SDQ) | 10.74±5.57 | 10.29±5.44 | .823 | .411 | .005 |
| Pro-social behavior | 8.21±1.82 | 8.34±1.72 | -.755 | .451 | .021 |
| Coping methods | 7.89±3.07 | 7.87±2.88 | .082 | .935 | -.032 |
| Coping satisfaction | 18.29±8.11 | 18.23±7.44 | .079 | .937 | -.034 |
| Function impairment | 3.64±4.47 | 3.23±4.37 | .933 | .351 | .003 |
| ICC - intracluster correlation coefficient; PTSD - post-traumatic stress disorder; SDQ - Strengths and Difficulties Questionnaire | |||||
Children were exposed to an average of two types of war-related events. The most common types were: seeing murdered bodies (51.9%), witnessing the death of family members (35.3%), and being involved in round-ups (32.6%). In addition, children reported an average of four types of ongoing daily stressors, most commonly: having been displaced (73.9%); being affected by poverty (67.9%), having difficulty meeting basic needs (62.7%), and quarrels in the neighborhood (62.7%). Intracluster correlation coefficients of outcome measures (ICC) ranged from -0.034 to 0.174.
Changes on outcome measures, moderators and mediators
First, we assessed crude mean changes (i.e., not corrected for clustered variance) as an exploratory analysis of changes on outcome measures (Table 2). These analyses showed statistically significantly larger improvement for boys in the intervention condition on anxiety and function impairment (effect sizes .27 to .29). For girls, we found an unintended harmful effect, such that girls in the waitlist condition showed larger improvements in PTSD symptoms than girls in the intervention condition (effect size .37).
Table 2.
Table 2 Mean change differences on outcome measures for boys and girls (baseline to 3-month follow-up)
| Outcome | Boys | Girls | ||||||
| Treatment condition (N=122) | Waitlist condition (N=123) | Treatment vs. waitlist | Treatment condition (N=76) | Waitlist condition (N=78) | Treatment vs. waitlist | |||
| Mean± SD | Mean± SD | t (df=243) | p | Mean±SD | Mean±SD | t(df=152) | p | |
| PTSD symptoms | 5.49±8.15 | 5.49±7.75 | -.004 | .997 | 4.83±8.17 | 7.88±8.49 | -2.274 | .024b |
| Depressive symptoms | 1.64±4.80 | 1.62±4.48 | .033 | .974 | 1.42±3.86 | 2.03±4.02 | -.951 | .343 |
| Anxiety symptoms | 1.70±2.46 | 1.07±2.21 | 2.090 | .038a | 1.29±2.44 | 1.55±2.43 | -.667 | .506 |
| Total difficulties | 3.35±5.55 | 2.07±5.55 | 1.809 | .072 | 3.37±5.18 | 3.06±5.59 | .350 | .727 |
| Supernatural complaints | 1.11±2.53 | 0.43±1.75 | 1.667 | .097 | 1.09±2.49 | 0.77±1.97 | .895 | .323 |
| Conduct problems | 0.94±2.55 | 0.60±2.21 | 1.103 | .271 | 0.55±1.85 | 0.27±2.83 | .733 | .465 |
| Pro-social behavior | 0.11±2.11 | 0.12±1.91 | -.067 | .947 | -0.30±1.49 | -0.09±1.87 | -.780 | .437 |
| Function impairment | 2.13±4.27 | 0.94±3.89 | 2.276 | .24a | 2.00±4.15 | 1.60±5.33 | .515 | .607 |
| PTSD - post-traumatic stress disorder; aeffect sizes .27 to .29; beffect size .37 | ||||||||
Second, to assess longitudinal trajectories of changes on outcome measures and the influence of moderating variables, we conducted LGCM, while correcting for clustering of variance within schools. We examined if the study condition predicted different growth trajectories and if gender, age, past exposure to violence and current experience of war-related stressors moderated the effects of intervention over time (Table 3). No statistically significant relationships between study condition and intercept estimates for our outcomes were found, confirming the comparability of study conditions at baseline. Longitudinal trajectories did not significantly differ between study conditions for our primary outcome measures (PTSD, anxiety, depression); however, we did find significantly different trajectories for a secondary outcome measure. Participants in the intervention condition showed more improvement (a decrease) in conduct problems over time than participants in the waitlist condition (slope estimate -.132; p=0.003). There was also a significant interaction of study condition and age for conduct problems, such that younger children showed more improvement than older children in the intervention condition (p=0.019).
Table 3.
Table 3 Model estimates of longitudinal changes on outcome measures, with gender and age as moderators
| Outcome | Intercepta | Slope: main effectb | Slope: interaction with genderc | Slope: interaction with aged | Slope: interaction with past violence exposurea | Slope: interaction with current stressors | ||||||
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| PTSD symptoms | -.306 | .879 | .281 | .332 | -1.169 | .444** | -.293 | .261 | .001 | .134 | .244 | .108** |
| Depressive symptoms | -.385 | .454 | .115 | .112 | -.206 | .242 | .134 | .152 | ||||
| Anxiety symptoms | -.075 | .188 | -.037 | .065 | -.308 | .144** | .035 | .062 | -.048 | .050 | .066 | .032** |
| Total difficulties | .037 | .516 | -.198 | .280 | -.409 | .225 | -.102 | .184 | ||||
| Supernatural complaints | .149 | .280 | -.121 | .064* | -.116 | .101 | -.022 | .071 | ||||
| Conduct problems | .080 | .209 | -.132 | .045*** | -.089 | .100 | .112 | .048** | -.028 | .076 | .015 | .043 |
| Pro-social behavior | -.030 | .166 | .016 | .052 | -.101 | .095 | -.107 | .050** | .014 | .032 | -.035 | .020 |
| Function impairment | -.427 | .482 | -.036 | .143 | -.346 | .178 | .102 | .109 | .000 | .111 | .167 | .069** |
| PTSD - post-traumatic stress disorder; aaverage score at baseline corrected for clustering; bchange on outcome measure over 0, 6 and 18 weeks; ca negative estimate indicates decreases in the outcome for boys; da negative estimate indicates decreases in the outcome for every year older; *statistically significant at α <0.06, **statistically significant at α <0.05, ***statistically significant at α <0.01 | ||||||||||||
In addition, we found a number of intervention effects for specific subgroups. Gender significantly moderated PTSD (slope estimate -1.169; p=0.009) and anxiety symptoms (slope estimate -.308; p=0.032), such that boys in the intervention condition showed more improvement over time than boys in the waitlist control condition. Also, a statistically significant interaction with age was identified for pro-social behavior (slope estimate .112; p=0.032). Increases in age were associated with smaller intervention benefits; in other words the intervention was effective in increasing pro-social behavior only for younger children.
We examined past violence exposure and current experience of war-related daily stressors as moderators (Table 3). Because none of the previous analyses showed statistically significant different change trajectories on depressive symptoms, supernatural complaints, and general psychological symptoms, we did not examine this group of outcome measures in these analyses. We identified an important moderating role in experience of current war-related daily stressors. This experience moderated treatment effects, such that children in the intervention condition with low levels of such stressors showed larger improvements on PTSD (estimate .244; p=0.024), anxiety (estimate .066; p=0.039), and function impairment (estimate .167; p=0.016) than children in the waitlist condition. Model fit of the LGCM were acceptable for just about all models, ranging from 0.87 to 1.00 on the comparative fit index.
Finally, we examined coping behavior as a possible mediator of intervention effects. Analysis of both crude mean changes and LGCM failed to show differences between study conditions with regard to trajectories of coping repertoire and coping satisfaction. Since a significant relation between intervention and a putative mediator is a precondition for a mediating role (and this condition was not met), we did not further investigate the potential role of coping behavior.
DISCUSSION
This evaluation of a secondary preventive intervention with school-going children in Sri Lanka adds to the emerging evidence for mental health and psychosocial support interventions in areas affected by armed conflict. Similar to earlier school-based interventions for war-affected children, differential intervention effects were observed. We found a main effect on a locally constructed scale for conduct problems, with stronger intervention benefits for younger children. These conduct problems, including for example a tendency to use violence as a means to solve conflict, imitation of soldiers, showing disrespect to elders, formed an important category of war-related psychological complaints as explained by children, parents, and teachers in our qualitative study. Furthermore, intervention effects were identified for children experiencing lower levels of current war-related daily stressors (PTSD, anxiety, function impairment), boys (PTSD and anxiety complaints), and younger children (pro-social behavior). However, we identified an unintended harmful effect of intervention for girls on PTSD symptoms.
Before we discuss these findings in more detail, we point to a number of limitations of the applied study methodology. First, although we did not disclose study condition to assessors and we selected research assessors external to intervention activities, we were not able to control possible disclosure of study condition by children participating in the study. Second, although we did include a locally validated measure (the Strengths and Difficulties Questionnaire), our primary outcome measures for PTSD, depression, and anxiety have unknown local criterion validity. Third, internal reliability of some of the measures was slightly less than acceptable (notably for anxiety symptoms). Despite these limitations, this study adds to the literature a rigorous intervention outcome study adhering to the CONSORT guidelines, in a pragmatic trial design 42.
Although some promising intervention effects were identified, the finding that girls in the waitlist condition showed better improvements over time on PTSD symptoms than girls in the intervention condition is an important unexpected outcome of this study. As a possible explanation of this finding, we point to the overlap in the moderating effects of gender and current experience of war-related daily stressors. Both variables moderated relations between study condition and changes on PTSD and anxiety. It is possible that the experience of current war-related daily stressors was different for boys and girls, and that these differences are driving the differential effects of intervention. In addition, it is possible that specific aspects of the working ingredients of the intervention (e.g., strengthening specific coping methods or social support strategies) contributed to differential effects for boys and girls. Such assumption would be consistent with findings of previous psychological interventions with war-affected children and adolescents, in which gender-specific effects are often observed 13,14,15,18. In the case of this intervention, it may be important to consider implementation with separate gender groups.
Our findings highlight the question of what may be appropriate interventions to target the mental health impacts of war on children. On the one hand, based on the lack of identified main intervention effects on primary outcomes in this study, it may be argued that clinical psychotherapeutic interventions rather than school-based interventions would be a more appropriate choice of intervention. For example, studies in high-income countries have found support for trauma-focused cognitive behavioral therapy and eye movement and desensitization reprocessing 43. However, we would still argue for the importance of primary and secondary prevention interventions with children affected by armed conflict for two reasons. First, these interventions may have benefits on outcomes beyond PTSD, which are important – albeit much less studied – consequences of war on the mental health of children 33. For example, this study showed improvements on conduct problems, anxiety, pro-social behavior, and function impairment, and earlier studies additionally showed benefits on hope, social support, aggression, and general psychological difficulties 13,14,15. Second, although observed effects of such interventions may have so far been smaller in effect size compared to individual clinical interventions and may be limited to specific population groups, such interventions carry the potential to reach larger population groups with fewer resources and in more accessible settings, and therefore may have similar effects on the wellbeing of populations at large as clinical interventions 44. However, our findings clearly point to the need for more careful efforts to identify the specific modifiable pathways of risk and protective factors for children affected by armed conflict 45,46, in order to prevent undermining natural recovery 14,47. Such research was judged a key priority in a recent effort to set research priorities for mental health and psychosocial support in humanitarian settings 48,49.
This study shows the possible limitations of the current tendency in LMIC for task shifting and integration of mental health interventions in community-based settings. It is not unreasonable to expect that when interventions move from clinics to community settings, and from being implemented by specialized professionals to implementation by lay workers, intervention effects will be more strongly moderated by contextual factors (e.g., poverty, exposure to violence, social marginalization). This study suggests that it will be crucial for evaluations of mental health interventions to explore not only if interventions are effective but also how they may be effective, in order to tailor interventions to context and population groups.
It has previously been argued that – given the great scarcity of mental health professionals in LMIC – the role of the clinician in LMIC should primarily be that of a public health practitioner leading the effort to scale-up mental health services and increase coverage of care 50. This and other studies show that clinicians in violence-affected areas may to this end successfully oversee task shifting to trained lay health workers to promote mental health (e.g., increase coping, social support, hope) and decrease distress and impairment. In settings with ongoing stressors, however, clinicians need to be wary of contextual moderators of preventive efforts, and treatment of PTSD symptoms specifically may require a more specialized approach, or a different treatment modality (e.g., an individual or family-based approach).
Acknowledgements
We would like to thank PLAN Netherlands for funding this study. The funder had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
References
- 1.Somasundaram D. Scarred minds: the psychological impacts of war on Sri Lankan Tamils. New Delhi: Sage Publications; 1998. [Google Scholar]
- 2.Somasundaram D, Jamunanantha CS. Psychosocial consequences of war: Northern Sri Lankan experience. In: de Jong JTVM, editor. Trauma, war, and violence: public mental health in socio-cultural context. New York: Kluwer Academic/Plenum Publishers; 2002. pp. 205–258. [Google Scholar]
- 3.Catani C, Jacob N, Schauer E. Family violence, war, and natural disasters: a study of the effect of extreme stress on children’s mental health in Sri Lanka. BMC Psychiatry. 2008;8:33–34. doi: 10.1186/1471-244X-8-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elbert T, Schauer M, Schauer E. Trauma-related impairment in children: a survey in Sri Lankan provinces affected by armed conflict. Child Abuse & Neglect. 2009;33:238–246. doi: 10.1016/j.chiabu.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 5.Somasundaram D. Collective trauma in northern Sri Lanka: a qualitative psychosocial-ecological study. Int J Ment Health Syst. 2007;1:5–5. doi: 10.1186/1752-4458-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Catani C, Schauer E, Neuner F. Beyond individual war trauma: domestic violence against children in Sri Lanka and Afghanistan. J Marital Fam Ther. 2008;34:165–176. doi: 10.1111/j.1752-0606.2008.00062.x. [DOI] [PubMed] [Google Scholar]
- 7.Saxena S, Thornicroft G, Knapp M. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370:878–889. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
- 8.Panter-Brick C, Eggerman M, Gonzalez V. Violence, suffering, and mental health in Afghanistan: a school-based survey. Lancet. 2009;374:807–816. doi: 10.1016/S0140-6736(09)61080-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stein BD, Jaycox LH, Kataoka SH. A mental health intervention for schoolchildren exposed to violence: a randomized controlled trial. JAMA. 2003;290:603–611. doi: 10.1001/jama.290.5.603. [DOI] [PubMed] [Google Scholar]
- 10.Kavanagh J, Oliver S, Caird J, editors. Inequalities and the mental health of young people: a systematic review of secondary school-based cognitive behavioural intervention. London: EPPI Centre, University of London; 2009. [Google Scholar]
- 11.Tol WA, Barbui C, Galappatti A. Mental health and psychosocial support in humanitarian settings: linking practice and research. Lancet. 2011;378:1581–1591. doi: 10.1016/S0140-6736(11)61094-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Layne CM, Saltzman WR, Poppleton L. Effectiveness of a school-based group psychotherapy program for war-exposed adolescents: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2008;47:1048–1062. doi: 10.1097/CHI.0b013e31817eecae. [DOI] [PubMed] [Google Scholar]
- 13.Tol WA, Komproe IH, Susanty D. School-based mental health intervention for children affected by political violence in Indonesia: a cluster randomized trial. JAMA. 2008;300:655–662. doi: 10.1001/jama.300.6.655. [DOI] [PubMed] [Google Scholar]
- 14.Tol WA, Komproe IH, Jordans MJ. Mediators and moderators of a psychosocial intervention for children affected by political violence. J Consult Clin Psychol. 2010;78:818–828. doi: 10.1037/a0021348. [DOI] [PubMed] [Google Scholar]
- 15.Jordans MJ, Komproe IH, Tol WA. Evaluation of a classroom-based psychosocial intervention in conflict-affected Nepal: a cluster randomized controlled trial. J Child Psychol Psychiatry. 2010;51:818–826. doi: 10.1111/j.1469-7610.2010.02209.x. [DOI] [PubMed] [Google Scholar]
- 16.Khamis V, Macy R, Coignez V. Save the Children. USA: 2004. The impact of the Classroom/Community/Camp-based Intervention (CBI) Program on Palestinian children. [Google Scholar]
- 17.Berger R, Gelkopf M. School-based intervention for the treatment of Tsunami-related distress in children: a quasi-randomized controlled trial. Psychother Psychosom. 2009;78:364–371. doi: 10.1159/000235976. [DOI] [PubMed] [Google Scholar]
- 18.Bolton P, Bass J, Betancourt T. Interventions for depression symptoms among adolescent survivors of war and displacement in northern Uganda: a randomized controlled trial. JAMA. 2007;298:519–527. doi: 10.1001/jama.298.5.519. [DOI] [PubMed] [Google Scholar]
- 19.Dybdahl R. Children and mothers in war: an outcome study of a psychosocial intervention program. Child Dev. 2001;72:1214–1230. doi: 10.1111/1467-8624.00343. [DOI] [PubMed] [Google Scholar]
- 20.Kraemer HC, Wilson T, Fairburn CG. Mediators and moderators of treatment effects in clinical trials. Arch Gen Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 21.Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annu Rev Clin Psychol. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- 22.Miller KE, Rasmussen A. War exposure, daily stressors, and mental health in conflict and post-conflict settings: bridging the divide between trauma-focused and psychosocial frameworks. Soc Sci Med. 2010;70:7–16. doi: 10.1016/j.socscimed.2009.09.029. [DOI] [PubMed] [Google Scholar]
- 23.Neuner F. Assisting war-torn populations: should we prioritize reducing daily stressors to improve mental health? Comment on Miller and Rasmussen (2010) Soc Sci Med. 2010;71:1381–1384. doi: 10.1016/j.socscimed.2010.06.030. [DOI] [PubMed] [Google Scholar]
- 24.Miller KE, Rasmussen A. Mental health and armed conflict: the importance of distinguishing between war exposure and other sources of adversity: a response to Neuner. Soc Sci Med. 2010;71:1385–1389. [Google Scholar]
- 25.Fernando G, Miller KE, Berger DE. Growing pains: the impact of disaster-related and daily stressors on the psychological and psychosocial functioning of youth in Sri Lanka. Child Dev. 2010;81:1192–1210. doi: 10.1111/j.1467-8624.2010.01462.x. [DOI] [PubMed] [Google Scholar]
- 26.Rasmussen A, Nguyen L, Wilkinson J. Rates and impact of trauma and current stressors among Darfuri refugees in eastern Chad. Am J Orthopsychiatry. 2010;80:227–236. doi: 10.1111/j.1939-0025.2010.01026.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Punamaki RL. Resiliency in conditions of war and military violence: preconditions and developmental processes. In: Garalda ME, Flament M, editors. Working with children and adolescents: an evidence-based approach to risk and resilience. Lanham: Jason Aronson; 2006. pp. 129–178. [Google Scholar]
- 28.Jordans MJD, Komproe IH, Tol WA. Screening for psychosocial distress amongst war-affected children: cross-cultural construct validity of the CPDS. J Child Psychol Psychiatry. 2009;50:514–523. doi: 10.1111/j.1469-7610.2008.02028.x. [DOI] [PubMed] [Google Scholar]
- 29.Jordans MJD, Komproe IH, Ventevogel P. Development and validation of the Child Psychosocial Distress Screener in Burundi. Am J Orthopsychiatry. 2008;78:290–299. doi: 10.1037/a0014216. [DOI] [PubMed] [Google Scholar]
- 30.Cohen JA, Deblinger E, Mannarino AP. A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. J Am Acad Child Adolesc Psychiatry. 2004;43:393–402. doi: 10.1097/00004583-200404000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Layne CM, Pynoos RS, Saltzman WR. Trauma/grief-focused group psychotherapy: school-based postwar intervention with traumatized Bosnian adolescents. Group Dynamics: Theory, Research and Practice. 2001;5:277–290. [Google Scholar]
- 32.Macy RD, Johnson Macy D, Gross SI. Healing in familiar settings: support for children and youth in the classroom and community. New Directions in Youth Development. 2003;98:51–79. doi: 10.1002/yd.44. [DOI] [PubMed] [Google Scholar]
- 33.Tol WA, Reis R, Susanty D. Communal violence and child psychosocial wellbeing: qualitative findings from Poso, Indonesia. Transcult Psychiatry. 2010;47:112–135. doi: 10.1177/1363461510364573. [DOI] [PubMed] [Google Scholar]
- 34.van Ommeren M, Sharma B, Thapa SB. Preparing instruments for transcultural research: use of the Translation Monitoring Form with Nepali-speaking Bhutanese refugees. Transcult Psychiatry. 1999;36:285–301. [Google Scholar]
- 35.Foa EB, Johnson KM, Feeny NC. The Child PTSD Symptom Scale: a preliminary examination of its psychometric properties. J Clin Child Psychol. 2001;30:376–384. doi: 10.1207/S15374424JCCP3003_9. [DOI] [PubMed] [Google Scholar]
- 36.Birleson P. The validity of depressive disorder in childhood and the development of a self-rating scale - a research report. J Child Psychol Psychiatry All Discipl. 1981;22:73–88. doi: 10.1111/j.1469-7610.1981.tb00533.x. [DOI] [PubMed] [Google Scholar]
- 37.Birmaher B, Brent DA, Chiappetta L. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 38.Lukumar P, Wijewardana K, Hermansson J. Validity and reliability of Tamil version of Strengths and Difficulties Questionnaire self-report. Ceylon Med J. 2008;53:48–52. doi: 10.4038/cmj.v53i2.232. [DOI] [PubMed] [Google Scholar]
- 39.Tol WA, Komproe IH, Jordans MJD. Developing a function impairment measure for children affected by political violence: a mixed methods approach in Indonesia. Int J Qual Health Care. 2011;23:5–83. doi: 10.1093/intqhc/mzr032. [DOI] [PubMed] [Google Scholar]
- 40.Spirito A, Stark LJ, Williams C. Development of a brief coping checklist for use with pediatric populations. J Pediatr Psychol. 1988;13:555–574. doi: 10.1093/jpepsy/13.4.555. [DOI] [PubMed] [Google Scholar]
- 41.Duncan TE, Duncan SC. An introduction to latent growth curve modeling. Behav Ther. 2004;35:333–363. [Google Scholar]
- 42.Thorpe KE, Zwarenstein M, Oxman OD. A pragmatic explanatory continuum indicator summary (PRECIS): a tool to help trial designers. J Clin Epidemiol. 2009;62:464–475. doi: 10.1016/j.jclinepi.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 43.Silverman WK, Ortiz CD, Viswesvaran C. Evidence-based psychosocial treatments for children and adolescents exposed to traumatic events. J Clin Child Adolesc Psychol. 2008;37:156–183. doi: 10.1080/15374410701818293. [DOI] [PubMed] [Google Scholar]
- 44.Patel V, Flisher AJ, Nikapota A. Promoting child and adolescent mental health in low and middle income countries. J Child Psychol Psychiatry. 2008;49:313–334. doi: 10.1111/j.1469-7610.2007.01824.x. [DOI] [PubMed] [Google Scholar]
- 45.Betancourt TS, Brennan RT, Rubin-Smith J. Sierra Leone’s former child soldiers: a longitudinal study of risk, protective factors, and mental health. J Am Acad Child Adolesc Psychiatry. 2010;49:606–615. doi: 10.1016/j.jaac.2010.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Panter-Brick C, Goodman A, Tol WA. Mental health and childhood adversities: a longitudinal study in Kabul, Afghanistan. J Am Acad Child Adolesc Psychiatry. 2011;50:349–363. doi: 10.1016/j.jaac.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tol WA, Jordans MJD, Reis R. Ecological resilience: working with child-related psychosocial resources in war-affected communities. In: Brom D, Pat-Horenczyk R, Ford J, editors. Treating traumatized children: risk, resilience, and recovery. London: Routledge; 2009. pp. 164–182. [Google Scholar]
- 48.Tol WA, Patel V, Tomlinson M. Research priorities for mental health and psychosocial support in humanitarian settings. PLoS Med. 2011;8 doi: 10.1371/journal.pmed.1001096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tol WA, Patel V, Tomlinson M. Relevance or excellence? Setting research priorities for mental health and psychosocial support in humanitarian settings. Harv Rev Psychiatry. 2012;20:25–36. doi: 10.3109/10673229.2012.649113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Patel V. The future of psychiatry in low-and middle-income countries. Psychol Med. 2009;39:1759–1762. doi: 10.1017/s0033291709005224. [DOI] [PubMed] [Google Scholar]