Abstract
Background:
Initial reports have shown the efficacy of fixed distraction for the treatment of ankle osteoarthritis. We hypothesized that allowing ankle motion during distraction would result in significant improvements in outcomes compared with distraction without ankle motion.
Methods:
We conducted a prospective randomized controlled trial comparing the outcomes for patients with advanced ankle osteoarthritis who were managed with anterior osteophyte removal and either (1) fixed ankle distraction or (2) ankle distraction permitting joint motion. Thirty-six patients were randomized to treatment with either fixed distraction or distraction with motion. The patients were followed for twenty-four months after frame removal. The Ankle Osteoarthritis Scale (AOS) was the main outcome variable.
Results:
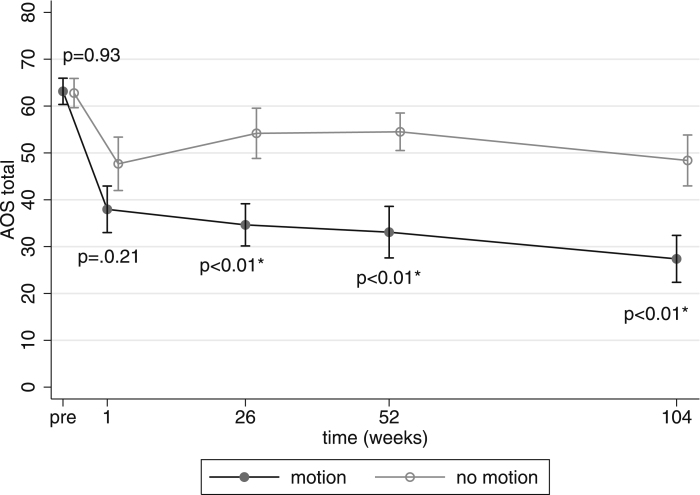
Two years after frame removal, subjects in both groups showed significant improvement compared with the status before treatment (p < 0.02 for both groups). The motion-distraction group had significantly better AOS scores than the fixed-distraction group at twenty-six, fifty-two, and 104 weeks after frame removal (p < 0.01 at each time point). At 104 weeks, the motion-distraction group had an overall mean improvement of 56.6% in the AOS score, whereas the fixed-distraction group had a mean improvement of 22.9% (p < 0.01).
Conclusion:
Distraction improved the patient-reported outcomes of treatment of ankle osteoarthritis. Adding ankle motion to distraction showed an early and sustained beneficial effect on outcome.
Level of Evidence:
Therapeutic Level I. See Instructions for Authors for a complete description of levels of evidence.
Posttraumatic osteoarthritis is the most common form of ankle osteoarthritis. Nonoperative treatments are used in the early stages of the disease and yield modest but inconsistent improvement1. Osteoarthritis generally progresses over time, and, as with other major lower extremity joints, the treatment of choice for end-stage ankle osteoarthritis is surgical. In young patients, debridement, resurfacing, and realignment have limited indications2-5. Ankle arthrodesis and ankle replacement, currently the most commonly performed procedures, have recognized potential complications and long-term problems6-12.
Joint distraction is a promising treatment approach for ankle osteoarthritis; however, its efficacy and role are not well defined. The treatment of ankle osteoarthritis with fixed distraction with use of thin-wire external fixators has been reported in both retrospective and prospective clinical series13-15. Those studies documented measurable and clinically important improvements in clinical and radiographic parameters in at least half of the patients undergoing non-articulated (fixed) thin-wire joint distraction.
Joint motion has been accepted as an essential adjunctive component in the biological restoration of articular cartilage after injury16-22, whereas joint immobilization can be deleterious to joint function20,22-24. Distraction alone, particularly with the use of external fixation, carries the potential for the development of arthrofibrosis, which can be deleterious to joint reconstruction25,26. Early joint motion allows decreased accumulation of periarticular interstitial fluid and helps to maintain normal soft-tissue compliance around the joint, thus decreasing the potential for arthrofibrosis27-30.
On the basis of the available clinical evidence, we hypothesized that ankle motion during distraction would result in clinically important improvements in outcomes compared with the use of distraction without ankle motion. The present study evaluated the patient-assessed outcomes of a prospective randomized controlled trial of distraction with or without ankle motion as treatment for advanced ankle osteoarthritis.
Materials and Methods
The inclusion and exclusion criteria for the selection of subjects are listed in the Appendix. Patients who met the study criteria were invited to participate in the study. Verbal and written explanations of the study procedures and the potential benefits and risks were provided. Written, witnessed consent was obtained from all subjects with use of approved forms under institutional review board approval (#200208025, University of Iowa).
Protocol
A physician clinical investigator first evaluated all patients. A complete history was obtained, a physical examination was performed, and routine standing radiographs were made, including standing anteroposterior, mortise, and lateral views of the ankle. Patients who met the inclusion criteria were told about the study by the physician and, when interested, were given more detail by the Research Coordinator. An external fixator and photographs of the fixator in use were shown to all patients as part of the institutional review board-approved consent process.
The primary outcome was the change in the overall Ankle Osteoarthritis Scale (AOS) score31. The AOS was selected because it has been shown to be a reliable, valid, and relatively simple instrument that measures physical function in patients with ankle osteoarthritis. The secondary outcomes were change in (1) the pain and disability AOS subscale scores and (2) the Physical Component Summary (PCS) score of the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36)32 (version 2). The AOS and SF-36 questionnaires were completed at the initial evaluation and then at one, twenty-six, fifty-two, and 104 weeks after fixator removal.
Surgical Procedure
All procedures were performed by one of two attending surgeons (A.A., C.L.S.) using the same technique. The patient was placed supine on the operating table. An arthroscopic ankle joint lavage with removal of any extra-articular anterior osseous osteophytes was performed with use of standard anterior portals and a 4.0-mm arthroscope without joint distraction. We avoided plantar flexion of the ankle because plantar flexion can pull the anterior capsule tightly over the joint and can limit accurate and full arthroscopic resection of anterior osteophytes. If the anterior osteophytes were too large to remove arthroscopically, they were removed by means of an open incision through an extension of the arthroscopic portals. We used three methods to determine the adequacy of the cheilectomy: (1) resection of the anterior tibial bone spur to the level of the anterior margin of the medial malleolus, (2) visual assessment and removal of any anterior joint impingement, and (3) intraoperative inspection of true lateral fluoroscopic images. The same criteria were used for both open and arthroscopic osteophyte resections. Intra-articular joint debridement was not performed.
The circumferential external fixator was applied in a standardized fashion. The tibial frame was applied with the rings perpendicular to the tibia, and the foot frame was placed in line with the foot. The upper tibial ring was secured with two 5-mm half-pins, and the lower ring was secured with one 5-mm half-pin and a crossing 1.8-mm (“thin”) wire tensioned to 110 to 130 lb. The foot frame was then attached with a thin wire placed transversely across the talus, two crossing thin wires across the calcaneus, and two crossing thin wires across the metatarsals, all tensioned to 70 to 90 lb.
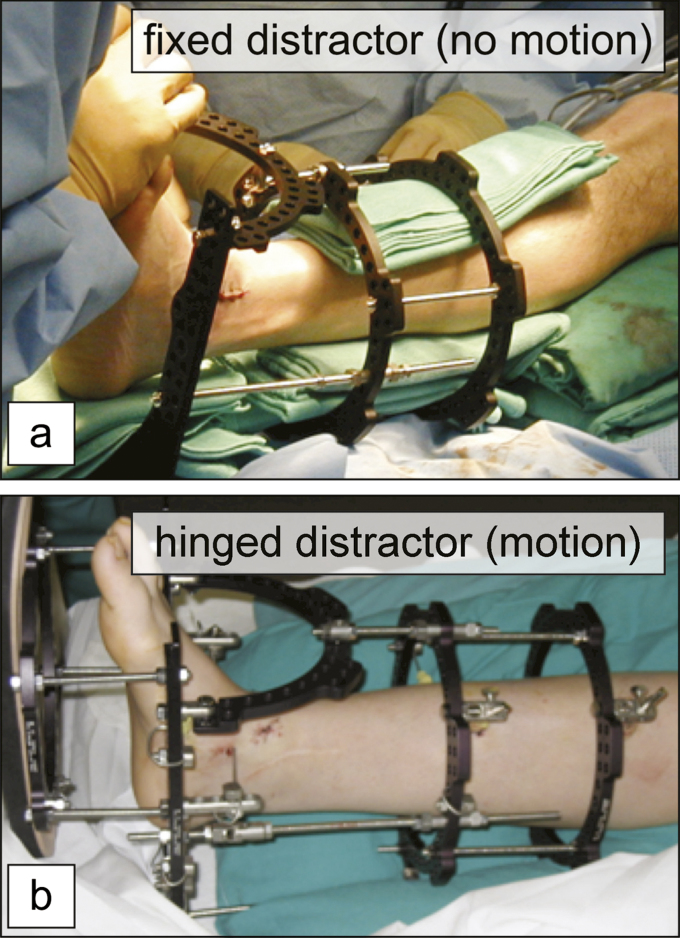
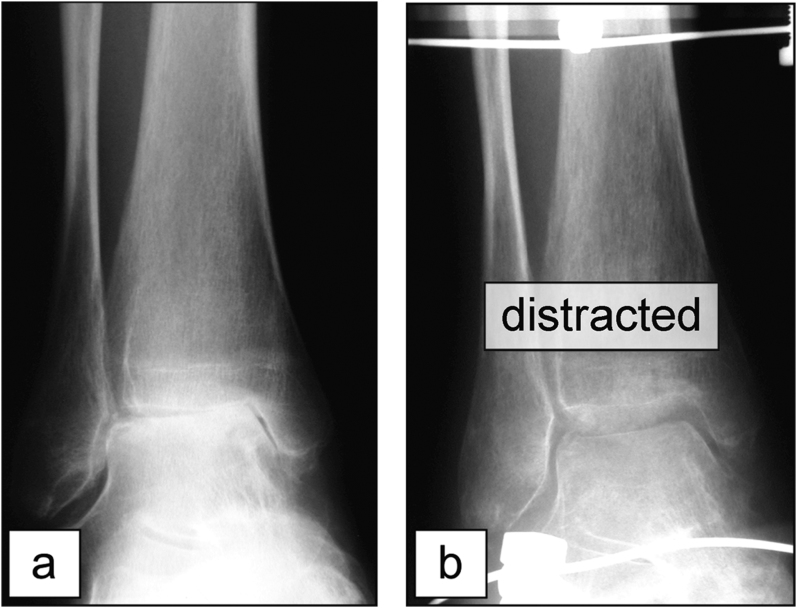
For patients who were allocated to fixed distraction without motion (hereafter denoted as the fixed group), distraction rods without hinges were used (Fig. 1-A). For patients who were allocated to distraction with motion (hereafter denoted as the motion group), distraction rods with hinges were used, with an unhinged posterior rod being detached during motion therapy. Universal hinges were placed at the level of the tips of the medial and lateral malleoli to roughly approximate the mean location of the ankle joint axis (Fig. 1-B)33. Intraoperatively, the ankle was distracted 5 mm as measured with use of fluoroscopy (Fig. 2).
Fig. 1.
Photographs showing the fixed distractor (no motion) (Fig. 1-A) and hinged distractor (motion) (Fig. 1-B) frames.
Fig. 2.
Anteroposterior radiographs of an ankle, made before treatment (Fig. 2-A) and after thin-wire distraction (Fig. 2-B).
Follow-up Protocol
Follow-up evaluations were done at one, three, six, and nine weeks. At each visit, the surgeon and a dedicated physical therapist saw the patient. Distraction of the ankle was assessed with radiographs and was adjusted as necessary. The motion group began therapy after Week 1. Patients in the motion group were instructed how to remove the posterior stabilizing bar and how to use a stockinette placed on the foot frame to passively dorsiflex and plantar flex the ankle (twenty repetitions, three times per day) for Weeks 2 through 12. The motion exercises were done through the entire potential range of ankle motion that the patient tolerated comfortably. Muscle conditioning was encouraged with use of a green (“heavy”) Thera-Band (Hygenic, Akron, Ohio) for resisted strengthening of both foot dorsiflexor and plantar flexor muscles (twenty repetitions, three times per day).
The fixator was removed between eighty-five and ninety-five days after application. The patient then wore a removable below-the-knee Velcro-strapped rocker-bottom boot for one month after fixator removal and began weight-bearing in the boot. The patient gradually returned to full weight-bearing without boot immobilization by six months.
The patient returned for study evaluations at one, twenty-six, fifty-two, and 104 weeks after fixator removal. The patient independently completed the self-assessment AOS and SF-36 questionnaires at each visit, and lateral radiographs with maximum dorsiflexion and maximum plantar flexion were made to measure the range of motion of the ankle at the one, fifty-two, and 104-week visits.
Subject Randomization
Eligible patients were randomized to one of the two treatment groups with use of a randomization schedule that had been prepared in advance. Randomization took place in the operating room after arthroscopic or open resection of the anterior osteophytes had been performed. Subjects were randomized in block sizes of two and four, determined at random. Sealed envelopes containing the treatment assignments for sequential patients were opened and assignments were made in the operating room after osteophyte removal had been completed and the incisions had been closed.
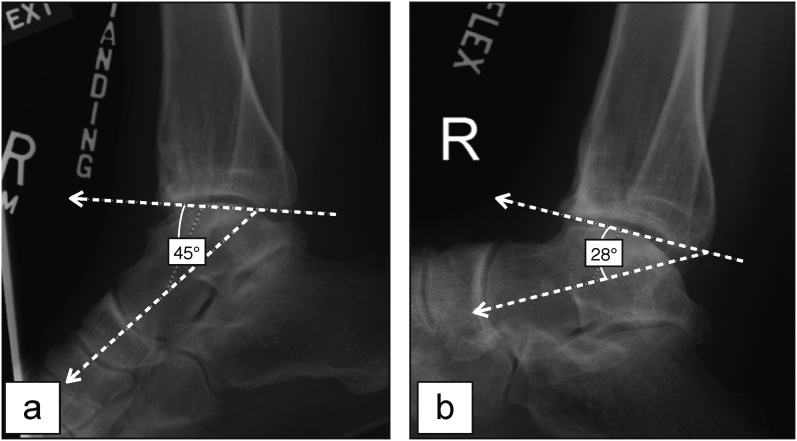
Ankle Range of Motion
A secondary study goal was to monitor sagittal plane ankle range of motion, before and after treatment, with use of lateral radiographs (Fig. 3). Intraoperative images were made after anterior osteophyte resection under fluoroscopic control. In the clinic, the patient was seated and was asked to forcibly plantar flex or dorsiflex the ankle with the sole of the foot supported by a soft foam wedge stabilizing the foot.
Fig. 3.
Figs. 3-A and 3-B Sagittal plane ankle range of motion was evaluated with use of lateral radiographs. The position of the ankle was expressed as the angle between the distal articular surface of the tibia and a line parallel to the longitudinal axis of the talus. The ankle range of motion was expressed as the difference between the angular position of the ankle on a maximum plantar flexion lateral ankle radiograph (Fig. 3-A) and that on a maximum dorsiflexion simulated weight-bearing lateral radiograph (Fig. 3-B). In this case, the range of motion of the ankle was 17° (45° − 28°).
Statistical Analysis
Because of randomization, we expected the distributions of both known and unknown confounders to be similar at baseline. Thus, baseline differences were not evaluated statistically unless they were deemed clinically meaningful.
Patients were evaluated at baseline and at one, twenty-six, fifty-two, and 104 weeks after fixator removal (hereafter denoted as pretreatment, T1, T26, T52, and T104, respectively). The primary hypothesis was that patients in the motion group would show increased improvement compared with patients in the fixed group at T52 and T104 with respect to combined AOS scores. A longitudinal analysis was used to test this primary hypothesis by testing if there was a difference between the groups at T52 and T104. This primary hypothesis was concluded at alpha = 0.05 if both of the individual comparisons of the combined AOS scores at T52 and T104 were each significant at alpha = 0.025; this represents a Bonferroni multiple-comparison correction. The other group comparisons at pretreatment, T1, and T26 were considered to be secondary (or exploratory) tests; alpha = 0.05 was used for these tests to determine significance, with no correction for multiple comparisons.
A statistical discussion of the longitudinal analysis approach, with examples, is provided elsewhere34. Briefly, the longitudinal analysis assumes a multivariate normal model and yields parameter estimates that maximize the likelihood of the observed data. It assumes a separate mean for each of the ten group-time combinations and an unstructured covariance matrix that allows for different variances at each time point and different covariances between the time points for each group.
Inferences for this longitudinal approach are valid if the data are missing at random (MAR). Although a subject may not have data for a particular time point, the subject’s data from other visits influences the estimate at the particular time point. For the present study, there were two kinds of missing data: (1) dropouts (when a patient left the study early) and (2) instances in which a patient missed the T1 visit. The few values that were missing at the T1 visit were due to administrative problems unrelated to the patient’s condition; therefore, these missing values satisfy the MAR assumption. The MAR assumption holds for dropouts if missingness depends on values recorded prior to dropout but not on values after dropout35 that would have been recorded had the patient stayed in the study.
Secondary analyses consisted of similarly testing if patients in the motion group showed increased improvement compared with patients in the fixed group at T26, T52, and T104 with respect to AOS pain, AOS disability, and PCS scores. Outcomes at pretreatment and T1 were compared as a test of the randomization. In addition, the same likelihood methods were used for testing if subjects in each group showed improvement over time by comparing T104 to pretreatment scores. For the range-of-motion analysis, nonparametric tests (Wilcoxon rank-sum test, Spearman rank correlation coefficient) were used because the smaller sample sizes prevented us from fitting a full multivariate model. A significance level of alpha = 0.05 was used for all of these secondary tests with no correction for multiple comparisons; i.e., comparisons were deemed to be significant if p ≤ 0.05.
Sample Size
Our goal was to recruit twenty-six patients in each treatment group to be able to detect a 0.8-standard-deviation difference in the AOS scores, which would have been about a 10-point difference based on an initial standard deviation estimate of 12.1. With this effect size, a patient in the more effective group would have a 0.76 probability of having a lower AOS score than a patient in the other group.
Source of Funding
This project was funded by a research grant from the National Institutes of Health. Funds were used to support the costs of salaries, imaging, subject travel, and supplies.
Results
Recruitment and Follow-up
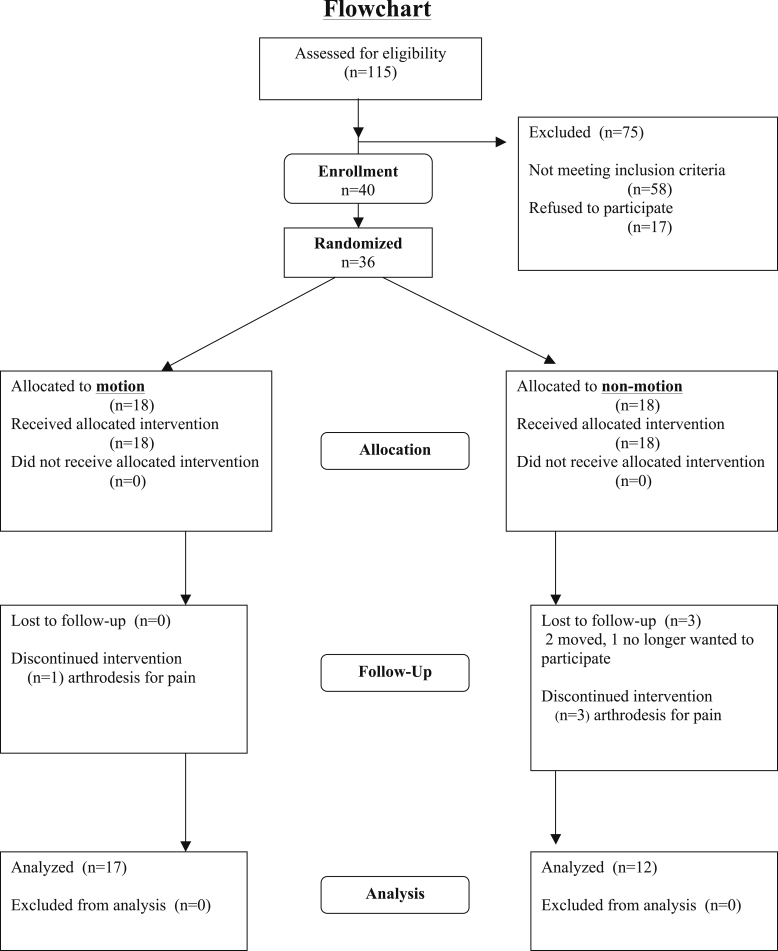
The study was opened for enrollment in December 2002 and was closed in October 2006. Follow-up was completed for the last patient in March 2009. During the enrollment period, 115 patients were screened and forty were entered into the study (Fig. 4). Four patients who enrolled in the study withdrew prior to having surgery.
Fig. 4.
Flowchart illustrating the patient recruitment and retention in this randomized controlled trial. In the motion group, no patients were lost to follow-up and one subject had conversion to an arthrodesis between the fifty-two and 104-week follow-up visits. In the fixed (non-motion) group, one subject dropped out prior to the T1 visit, one subject dropped out after the twelve-month return visit, and one subject dropped out after the T52 visit. The latter two patients moved out of state. In the fixed (non-motion) group, three additional patients had arthrodesis surgery, one before the T52 visit and two between the T52 and T104 visits.
Of the patients who were screened, seventeen who met the study criteria declined to participate. The sex distribution (ten males, seven females) and mean age (40.9 years) for these seventeen patients were similar to those for the patients who volunteered for the trial. The reasons for refusal included the need to think about options (nine patients), financial concerns with time off work or insurance coverage (four patients), a preference for ankle arthrodesis (one patient) or isolated osteophyte removal (one patient), a need for total hip replacement first (one patient), and a refusal of any treatment (one patient).
In the motion group, no patients were lost to follow-up and one patient had conversion to an arthrodesis between the T52 and T104 visits. In the fixed group, one subject dropped out before the T1 visit, one dropped out after the T1 visit, and one dropped out after the T52 visit. In the fixed group, three additional patients underwent ankle arthrodesis, one before the T52 visit and two between the T52 and T104 visits.
Baseline Data/Patient Characteristics
The age, sex, and body mass index of the patients were clinically similar between the groups (Table I) and were not evaluated statistically.
TABLE I.
Baseline Data and Patient Characteristics
| Treatment | Age* (yr) | Female:Male Ratio (no. of patients) | BMI*† (kg/m2) |
| Fixed | 42.4 (18 to 53) | 7:11 | 31.9 (23.1 to 40.8) |
| Motion | 42.7 (27 to 59) | 5:13 | 30.0 (23.3 to 36.2) |
The values are given as the mean, with the range in parentheses.
BMI = body mass index.
Outcomes
With regard to our primary outcomes, the combined AOS score (descriptive statistics in Table II) consists of the average of the AOS pain and disability scores. There were eighteen patients in each of the two treatment groups, and, at the time of the latest visit (T104), data were available for seventeen patients in the motion group and eleven patients in the fixed group.
TABLE II.
Descriptive Statistics for Combined AOS Score
| AOS Score (points) |
|||||
| Time Point* | Mean | Standard Deviation | Median | Minimum | Maximum |
| Pretreatment | |||||
| Motion (n = 18) | 63.14 | 11.88 | 64.09 | 39.00 | 79.15 |
| Fixed (n = 18) | 62.77 | 13.23 | 68.36 | 39.00 | 78.80 |
| T1 | |||||
| Motion (n = 16) | 38.38 | 20.50 | 36.49 | 0.00 | 82.40 |
| Fixed (n = 17) | 46.16 | 23.53 | 41.10 | 1.67 | 86.25 |
| T26 | |||||
| Motion (n = 18) | 34.64 | 19.12 | 33.66 | 0.05 | 68.90 |
| Fixed (n = 16) | 54.29 | 21.74 | 54.83 | 25.35 | 88.00 |
| T52 | |||||
| Motion (n = 18) | 33.09 | 23.33 | 28.53 | 1.50 | 79.28 |
| Fixed (n = 14) | 54.69 | 15.46 | 53.34 | 25.72 | 78.50 |
| T104 | |||||
| Motion (n = 17) | 26.61 | 21.01 | 21.93 | 0.02 | 65.45 |
| Fixed (n = 11) | 48.78 | 20.22 | 47.72 | 20.69 | 87.65 |
T1, T26, T52, T104 = one, twenty-six, fifty-two, and 104 weeks after fixator removal, respectively.
The results of the longitudinal analysis are given in Table III, with mean estimates plotted in Figure 5. The mean estimates from the longitudinal analysis were quite similar to the means based only on non-missing values given in Table II. As expected, as this was a randomized study, the means were not significant at the pretreatment or T1.
TABLE III.
Longitudinal Analysis Comparison of Combined AOS Outcome Scores
| AOS Score (points) |
||||
| Time Point* | Fixed Group† | Motion Group† | Difference (Fixed Group – Motion Group) | P Value‡ |
| Pretreatment | 62.8 | 63.1 | −0.4 | 0.93 |
| T1 | 47.7 | 38.0 | 9.7 | 0.21 |
| T26 | 54.2 | 34.6 | 19.5 | <0.01* |
| T52 | 54.5 | 33.1 | 21.4 | <0.01* |
| T104 | 48.4 | 27.4 | 21.0 | <0.01* |
T1, T26, T52, T104 = one, twenty-six, fifty-two, and 104 weeks after fixator removal, respectively.
AOS estimates.
The p values pertain to testing if the means of the AOS outcome scores for the two groups were equal at the given time point.
Fig. 5.
Mean estimates of the combined AOS score versus time. The p values are for testing for a group difference at the particular time point; the mean values for the fixed (no motion) group have been moved slightly to the right to make the plot more readable. *P < 0.05.
In our primary longitudinal analysis, we concluded from the data in Table III and Figure 5 that the motion group had significantly better combined AOS outcome scores at T52 and T104. Specifically, at T52, the AOS score was 33.1 for the motion group compared with 54.5 for the fixed group (p < 0.01), and, at T104, the score was 27.4 for the motion group compared with 48.4 for the fixed group (p < 0.01).
In secondary analyses, there was also a significant difference between the two groups at T26 (p < 0.01). When the combined AOS scores at T104 were compared with the pretreatment scores, the motion group showed an improvement (decrease) of 35.8 (p < 0.01) whereas the fixed group showed an improvement of 14.4 (p < 0.02). The improvement in mean scores at T104 over baseline was 56.6% for the motion group and 22.9% for the fixed group. Thus, on average, the motion group demonstrated 2.47 times the improvement seen in the fixed group.
The results of comparisons of the two groups at each time point were similar for the separate AOS scales (see Appendix). For both pain and disability, the motion group showed significantly better outcomes at T26, T52, and T104, but, as expected, there were no significant differences at pretreatment or T1. Each group performed better at T104 than at pretreatment (p < 0.02 for both groups).
The motion group showed better PCS outcomes than the fixed group at T26 (p = 0.02) and T104 (p = 0.05) but not at T52 (p = 0.49) (see Appendix). Each group performed better at T104 compared with pretreatment (p < 0.01). In the entire study group, there were twelve open debridements and twenty-five arthroscopic debridements. With the numbers available, there was not a significant association between the type of debridement and increased pain or disability (p = 0.12, Fisher exact test).
Ankle Range of Motion
For the range-of-motion outcomes, there was not a significant group difference between change scores (p = 0.76; Wilcoxon rank-sum test), with the change score defined as the two-year minus the intraoperative outcome. However, because of the low numbers of subjects (ten in the motion group and fourteen in the fixed group) with two-year follow-up data, the power for this test was low, and thus this nonsignificant difference should not be interpreted as meaning that the two treatments have similar population means. When the observations were pooled, the two-year range-of-motion outcomes were not significantly different from the preoperative values (p = 0.06) or the intraoperative values (p = 0.08). For the pooled data, there was not a significant correlation between pretreatment and two-year range-of-motion outcomes (p = 0.88) or between intraoperative and two-year range-of-motion outcomes (Spearman rho = 0.14, p = 0.60).
Adverse Events
The distributions of adverse events experienced in this trial were not related to treatment randomization.
Any redness, increasing pain, warmth, drainage, or swelling around a pin site was classified as a probable infection. On the basis of this criterion, there were forty-three episodes of pin-track infection in nineteen patients. All infections were treated initially with oral antibiotics (cephalexin, 250 mg four times daily for seven days). Four persisted, and the pins were removed. Two of these four infections occurred in patients who were thought to have acute osteomyelitis and were treated to resolution with six weeks of intravenous antibiotics.
Eight patients had areas of numbness in the medial calcaneal branch of the tibial nerve and the deep peroneal distribution onto the great toe after distractor placement. When numbness was identified, radiographs were made and, if distraction exceeded 5 mm, it was reduced to this level. No other treatment was given. Four cases resolved with the frame on, two resolved within three months after frame removal, and two patients were left with residual numbness. Two years after frame removal, one patient had mild decreased sensation on the dorsal aspect of the hallux, and the other had mild tingling on the plantar aspect of the foot that continued to decrease. With the small numbers studied, a significant association between neuropraxia and treatment group could not be identified.
One patient, in the fixed group, developed a symptomatic deep venous thrombosis distal to the knee that was treated with anticoagulation therapy.
Discussion
We performed a randomized controlled trial comparing two forms of distraction as treatment for end-stage ankle osteoarthritis. Both forms of distraction treatment were associated with improvement in reported outcomes as compared with the pretreatment status. Treatment with a motion distractor resulted in early and consistently better improvement in outcomes and treatment effect compared with fixed distraction.
Our results were quite similar to those described in previous reports. Van Valburg et al. presented a case series of eleven patients with posttraumatic ankle osteoarthritis who were managed with fixed distraction, with good initial results15. Those investigators then performed a prospective series and found that more than two-thirds of patients demonstrated significant improvement at two years36. When that cohort was followed to an average of ten years (minimum, seven years), 73% of the patients reported good results37.
Our inclusion criteria were selected to identify a single cohort of patients with limited confounding variables. The use of patients with symptomatic isolated, unilateral end-stage ankle osteoarthritis was essential to avoid the potential confounder of pain and limited function from other lower extremity joints.
Several potential issues may limit the generalizability of the trial findings. One limitation is that inferences based on a predominantly white sample could be strictly generalizable only to a predominantly white population. However, we are not aware of a study that suggests that the pathogenesis, clinical presentation, or response to treatment of ankle osteoarthritis varies by race.
Another potential concern is the relatively high loss of patients (seven of eighteen) at the time of the two-year follow-up for the fixed group and its influences on estimates of the outcome at the time of the two-year follow-up. However, estimates from the longitudinal analysis remain valid under the assumption that the data are missing at random (MAR). As previously noted, the MAR assumption holds for dropouts if missingness depends on values recorded prior to dropout, but not on values after dropout; thus, it appears to be a reasonable assumption for our data. Furthermore, the similarity between the longitudinal analysis estimates (Table III) and the raw means (Table II) strongly suggests that the data are missing completely at random (MCAR), which is an even more stringent assumption than MAR35. We note that results based on two-sample t tests comparing the groups, based only on the data at each time point, yielded results similar to the longitudinal analysis; specifically, there were significant group differences at twenty-six, fifty-two, and 104 weeks for combined AOS outcomes (p ≤ 0.01 for each comparison).
A third concern is that we performed osteophyte removal at the time of distractor placement. We do not think it confounded our results because we performed this procedure in the same way on every patient prior to randomization, and the preponderance of clinical evidence suggests that arthroscopy alone does not have any long-term beneficial effects on end-stage arthritic joint symptoms or function38-41. In patients with ankle osteoarthritis, osteophytes are extremely common and can have a mechanical effect on the outcome if the lack of ankle dorsiflexion is due to painful osseous impingement38,41.
The ankle distraction treatment involves a relatively prolonged period of convalescence, with associated adverse events. In our study of thirty-six patients, there were forty-three episodes of pin-track infection in nineteen patients, with two patients receiving six weeks of antibiotics because of a suspicion of acute osteomyelitis. This rate of pin-track infection was higher than that generally reported in association with the use of this form of external fixation for three months42-44. In bone-transport studies, the rates of pin-track infection have ranged from relatively low to very high42-47. We attribute the high rate in our series to two factors. First, we classified any redness, increasing pain, warmth, drainage, or swelling around a pin site as an infection. Some of these findings may have been secondary to irritation of the skin rather than true infection. Second, this was a well-controlled, prospective study. Every adverse event, regardless of how minor, was meticulously documented.
In addition, eight patients in the present study had neurapraxias, two that persisted at two years. The use of gradual distraction, rather than distracting the ankle in a single maneuver with the patient under anesthesia just after frame application, may have avoided the creation of the neurapraxias. After study closure, we changed our technique from intraoperative to gradual postoperative distraction under patient control, as originally described by van Valburg and colleagues15.
Ankle motion did not significantly change from either preoperative or intraoperative values, nor did it differ between groups. Immediately after fixator removal, motion was extremely limited for both groups. Over the subsequent two years, motion continued to improve slowly. The mechanism that resulted in the beneficial effect found in association with the use of a motion distractor rather than a fixed distractor appears not to have been directly related to the magnitude of motion. Rather, the data suggest that the mechanism is related to some other factor such as (1) improved joint shock absorption with a motion distractor, (2) improved motor control around the joint, or (3) improved quality of the resurfacing soft tissue that fills the joint during the treatment period.
Ankle distraction is not a procedure to be done for patients or by surgeons who want a “quick fix.” In the present study, the frame was worn for three months, and then the patients progressed to full weight-bearing without boot immobilization at six months. In general, subjects reported feeling much better between the six and twelve-month follow-up appointments. We now advise patients who are considering this treatment that they may not see the benefits of the procedure until one year after surgery. Compared with alternative treatments, such as arthrodesis or ankle replacement, this is a relatively long period of time to wait for a treatment benefit. Whether the total time of distraction can be shortened or the time to unrestricted weight-bearing period after frame removal can be shortened remains to be established.
In conclusion, we performed a prospective randomized controlled trial of distraction for the treatment of ankle osteoarthritis by comparing patients with ankle motion with those without ankle motion. Both approaches led to improved outcomes. Adding motion to distraction roughly doubled the response to treatment with the outcomes measurement instruments used. On the basis of these results, we recommend that motion be included when using distraction to treat ankle osteoarthritis.
Appendix
A table showing the inclusion and exclusion criteria for the selection of subjects and figures showing the mean estimates of the AOS pain, AOS disability, and PCS outcome scores versus time are available with the online version of this article as a data supplement at jbjs.org.
Acknowledgments
Note: This project was supported by Grant Number P50AR048939 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health, U.S. Department of Health & Human Services.
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Saltzman CL, Shurr D, Kamp J, Cook TA. The leather ankle lacer. Iowa Orthop J. 1995;15:204-8 [PMC free article] [PubMed] [Google Scholar]
- 2.Baltzer AW, Arnold JP. Bone-cartilage transplantation from the ipsilateral knee for chondral lesions of the talus. Arthroscopy. 2005;21:159-66 [DOI] [PubMed] [Google Scholar]
- 3.Pagenstert GI, Hintermann B, Barg A, Leumann A, Valderrabano V. Realignment surgery as alternative treatment of varus and valgus ankle osteoarthritis. Clin Orthop Relat Res. 2007;462:156-68 [DOI] [PubMed] [Google Scholar]
- 4.Takakura Y, Tanaka Y, Kumai T, Tamai S. Low tibial osteotomy for osteoarthritis of the ankle. Results of a new operation in 18 patients. J Bone Joint Surg Br. 1995;77:50-4 [PubMed] [Google Scholar]
- 5.Tanaka Y, Takakura Y, Hayashi K, Taniguchi A, Kumai T, Sugimoto K. Low tibial osteotomy for varus-type osteoarthritis of the ankle. J Bone Joint Surg Br. 2006;88:909-13 [DOI] [PubMed] [Google Scholar]
- 6.Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg Am. 2001;83:219-28 [DOI] [PubMed] [Google Scholar]
- 7.Glazebrook MA, Arsenault K, Dunbar M. Evidence-based classification of complications in total ankle arthroplasty. Foot Ankle Int. 2009;30:945-9 [DOI] [PubMed] [Google Scholar]
- 8.Haddad SL, Coetzee JC, Estok R, Fahrbach K, Banel D, Nalysnyk L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J Bone Joint Surg Am. 2007;89:1899-905 [DOI] [PubMed] [Google Scholar]
- 9.Lee KB, Cho SG, Hur CI, Yoon TR. Perioperative complications of HINTEGRA total ankle replacement: our initial 50 cases. Foot Ankle Int. 2008;29:978-84 [DOI] [PubMed] [Google Scholar]
- 10.Morrey BF, Wiedeman GP., Jr Complications and long-term results of ankle arthrodeses following trauma. J Bone Joint Surg Am. 1980;62:777-84 [PubMed] [Google Scholar]
- 11.Saltzman CL, Amendola A, Anderson R, Coetzee JC, Gall RJ, Haddad SL, Herbst S, Lian G, Sanders RW, Scioli M, Younger AS. Surgeon training and complications in total ankle arthroplasty. Foot Ankle Int. 2003;24:514-8 [DOI] [PubMed] [Google Scholar]
- 12.Spirt AA, Assal M, Hansen ST., Jr Complications and failure after total ankle arthroplasty. J Bone Joint Surg Am. 2004;86:1172-8 [DOI] [PubMed] [Google Scholar]
- 13.Marijnissen AC, Vincken KL, Viergever MA, van Roy HL, Van Roermund PM, Lafeber FP, Bijlsma JW. Ankle images digital analysis (AIDA): digital measurement of joint space width and subchondral sclerosis on standard radiographs. Osteoarthritis Cartilage. 2001;9:264-72 [DOI] [PubMed] [Google Scholar]
- 14.van Roermund PM, Lafeber FP. Joint distraction as treatment for ankle osteoarthritis. Instr Course Lect. 1999;48:249-54 [PubMed] [Google Scholar]
- 15.van Valburg AA, van Roermund PM, Lammens J, van Melkebeek J, Verbout AJ, Lafeber EP, Bijlsma JW. Can Ilizarov joint distraction delay the need for an arthrodesis of the ankle? A preliminary report. J Bone Joint Surg Br. 1995;77:720-5 [PubMed] [Google Scholar]
- 16.Buckwalter JA. Effects of early motion on healing of musculoskeletal tissues. Hand Clin. 1996;12:13-24 [PubMed] [Google Scholar]
- 17.Fu LL, Maffulli N, Yip KM, Chan KM. Articular cartilage lesions of the knee following immobilisation or destabilisation for 6 or 12 weeks in rabbits. Clin Rheumatol. 1998;17:227-33 [DOI] [PubMed] [Google Scholar]
- 18.Haapala J, Arokoski J, Pirttimäki J, Lyyra T, Jurvelin J, Tammi M, Helminen HJ, Kiviranta I. Incomplete restoration of immobilization induced softening of young beagle knee articular cartilage after 50-week remobilization. Int J Sports Med. 2000;21:76-81 [DOI] [PubMed] [Google Scholar]
- 19.Haapala J, Arokoski JP, Rönkkö S, Agren U, Kosma VM, Lohmander LS, Tammi M, Helminen HJ, Kiviranta I. Decline after immobilisation and recovery after remobilisation of synovial fluid IL1, TIMP, and chondroitin sulphate levels in young beagle dogs. Ann Rheum Dis. 2001;60:55-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jortikka MO, Inkinen RI, Tammi MI, Parkkinen JJ, Haapala J, Kiviranta I, Helminen HJ, Lammi MJ. Immobilisation causes longlasting matrix changes both in the immobilised and contralateral joint cartilage. Ann Rheum Dis. 1997;56:255-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O’Connor KM. Unweighting accelerates tidemark advancement in articular cartilage at the knee joint of rats. J Bone Miner Res. 1997;12:580-9 [DOI] [PubMed] [Google Scholar]
- 22.Setton LA, Mow VC, Müller FJ, Pita JC, Howell DS. Mechanical behavior and biochemical composition of canine knee cartilage following periods of joint disuse and disuse with remobilization. Osteoarthritis Cartilage. 1997;5:1-16 [DOI] [PubMed] [Google Scholar]
- 23.Buckwalter JA. Activity vs. rest in the treatment of bone, soft tissue and joint injuries. Iowa Orthop J. 1995;15:29-42 [PMC free article] [PubMed] [Google Scholar]
- 24.Haapala J, Lammi MJ, Inkinen R, Parkkinen JJ, Agren UM, Arokoski J, Kiviranta I, Helminen HJ, Tammi MI. Coordinated regulation of hyaluronan and aggrecan content in the articular cartilage of immobilized and exercised dogs. J Rheumatol. 1996;23:1586-93 [PubMed] [Google Scholar]
- 25.Pavolini B, Maritato M, Turelli L, D’Arienzo M. The Ilizarov fixator in trauma: a 10-year experience. J Orthop Sci. 2000;5:108-13 [DOI] [PubMed] [Google Scholar]
- 26.Velazquez RJ, Bell DF, Armstrong PF, Babyn P, Tibshirani R. Complications of use of the Ilizarov technique in the correction of limb deformities in children. J Bone Joint Surg Am. 1993;75:1148-56 [DOI] [PubMed] [Google Scholar]
- 27.Moran ME, Kim HK, Salter RB. Biological resurfacing of full-thickness defects in patellar articular cartilage of the rabbit. Investigation of autogenous periosteal grafts subjected to continuous passive motion. J Bone Joint Surg Br. 1992;74:659-67 [DOI] [PubMed] [Google Scholar]
- 28.O’Driscoll SW, Salter RB. The induction of neochondrogenesis in free intra-articular periosteal autografts under the influence of continuous passive motion. An experimental investigation in the rabbit. J Bone Joint Surg Am. 1984;66:1248-57 [PubMed] [Google Scholar]
- 29.O’Driscoll SW. The healing and regeneration of articular cartilage. J Bone Joint Surg Am. 1998;80:1795-812 [PubMed] [Google Scholar]
- 30.Salter RB. The biologic concept of continuous passive motion of synovial joints. The first 18 years of basic research and its clinical application. Clin Orthop Relat Res. 1989;242:12-25 [PubMed] [Google Scholar]
- 31.Domsic RT, Saltzman CL. Ankle osteoarthritis scale. Foot Ankle Int. 1998;19:466-71 [DOI] [PubMed] [Google Scholar]
- 32.Ware JE, Jr, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473-83 [PubMed] [Google Scholar]
- 33.Bottlang M, Marsh JL, Brown TD. Articulated external fixation of the ankle: minimizing motion resistance by accurate axis alignment. J Biomech. 1999;32:63-70 [DOI] [PubMed] [Google Scholar]
- 34.Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. New York: Springer-Verlag; 2000 [Google Scholar]
- 35.Little RJ, Rubin DB. Statistical analysis with missing data. Hoboken, NJ: Wiley; 2002 [Google Scholar]
- 36.van Valburg AA, van Roermund PM, Marijnissen AC, van Melkebeek J, Lammens J, Verbout AJ, Lafeber FP, Bijlsma JW. Joint distraction in treatment of osteoarthritis: a two-year follow-up of the ankle. Osteoarthritis Cartilage. 1999;7:474-9 [DOI] [PubMed] [Google Scholar]
- 37.Ploegmakers JJ, van Roermund PM, van Melkebeek J, Lammens J, Bijlsma JW, Lafeber FP, Marijnissen AC. Prolonged clinical benefit from joint distraction in the treatment of ankle osteoarthritis. Osteoarthritis Cartilage. 2005;13:582-8 [DOI] [PubMed] [Google Scholar]
- 38.Hassouna H, Kumar S, Bendall S. Arthroscopic ankle debridement: 5-year survival analysis. Acta Orthop Belg. 2007;73:737-40 [PubMed] [Google Scholar]
- 39.Laupattarakasem W, Laopaiboon M, Laupattarakasem P, Sumananont C. Arthroscopic debridement for knee osteoarthritis. Cochrane Database Syst Rev. 2008;1:CD005118 [DOI] [PubMed] [Google Scholar]
- 40.Moseley JB, O’Malley K, Petersen NJ, Menke TJ, Brody BA, Kuykendall DH, Hollingsworth JC, Ashton CM, Wray NP. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81-8 [DOI] [PubMed] [Google Scholar]
- 41.Tol JL, Verheyen CP, van Dijk CN. Arthroscopic treatment of anterior impingement in the ankle. J Bone Joint Surg Br. 2001;83:9-13 [DOI] [PubMed] [Google Scholar]
- 42.Paley D. The correction of complex foot deformities using Ilizarov’s distraction osteotomies. Clin Orthop Relat Res. 1993;293:97-111 [PubMed] [Google Scholar]
- 43.Katsenis D, Bhave A, Paley D, Herzenberg JE. Treatment of malunion and nonunion at the site of an ankle fusion with the Ilizarov apparatus. J Bone Joint Surg Am. 2005;87:302-9 [DOI] [PubMed] [Google Scholar]
- 44.Salem KH, Kinzl L, Schmelz A. Ankle arthrodesis using Ilizarov ring fixators: a review of 22 cases. Foot Ankle Int. 2006;27:764-70 [DOI] [PubMed] [Google Scholar]
- 45.Kesemenli C, Subasi M, Kirkgoz T, Kapukaya A, Arslan H. Treatment of traumatic bone defects by bone transport. Acta Orthop Belg. 2001;67:380-6 [PubMed] [Google Scholar]
- 46.Mekhail AO, Abraham E, Gruber B, Gonzalez M. Bone transport in the management of posttraumatic bone defects in the lower extremity. J Trauma. 2004;56:368-78 [DOI] [PubMed] [Google Scholar]
- 47.Sen C, Kocaoglu M, Eralp L, Cinar M. Correction of ankle and hindfoot deformities by supramalleolar osteotomy. Foot Ankle Int. 2003;24:22-8 [DOI] [PubMed] [Google Scholar]