Abstract
Objective
Two case reports review the chiropractic treatment and rehabilitation management of Symphysis Pubis Dysfunction (SPD).
Clinical features
Patient 1: a 35-year-old female presented at 30 weeks pregnant with severe left sided Symphysis Pubis Dysfunction and low back pain. Patient 2: a 33-year-old female also 30 weeks pregnant, presented with right sided Symphysis Pubis Dysfunction and sacroiliac pain.
Intervention and Outcome
Treatment included soft tissue therapy, pregnancy support belt, side-lying mobilizations, pelvic blocks and instrument-assisted pubic symphysis adjustments. Home advice included: ice, staying active, moving as a unit, stretching, use of a pillow between the knees while sleeping, regular breaks from sitting and pelvic floor (Kegel) exercises. Both patients reported some relief with treatment and home care. Post-partum, rehabilitation exercises were prescribed to restore muscular endurance, control and pelvic stability. On long-term follow-up patient 1 reported no pubic symphysis pain, but some low back pain secondary to a subsequent knee injury. Patient 2 reported being mostly pain free with a rare re-exacerbation of pubic symphysis pain.
Summary
Conservative chiropractic management appears to reduce pain and improve mobility and function for SPD. Post partum rehabilitation of the associated lumbo-pelvic musculature with specific stabilization exercises is recommended to reduce pain, improve long term outcomes and prevent chronicity.
Keywords: chiropractic, pregnancy, pelvic pain, pubic symphysis, rehabilitation, exercise
Abstract
Objectif
Deux rapports de cas passent en revue les soins chiropratiques et la gestion de la réadaptation dans le cadre d’une dysfonction affectant la région de la symphyse pubienne (DSP).
Caractéristiques cliniques
Patiente 1 : Une femme âgée de 35 ans a ressenti à 30 semaines de grossesse des douleurs intenses liées à une dysfonction de la symphyse pubienne au côté gauche ainsi qu’à une lombalgie. Patiente 2 : une femme âgée de 33 ans également enceinte de 30 semaines a ressenti des douleurs liées à une dysfonction de la symphyse pubienne au côté droit et des douleurs sacro-iliaques.
Intervention et résultat
Leur traitement comportait entre autres une thérapie des tissus mous, le port d’une ceinture de soutien de grossesse, des mobilisations en position couchée sur le côté, des cales pelviennes, et des réajustements de la symphyse pubienne assistés par des instruments. Chez elles, on leur avait conseillé de mettre de la glace, de rester actives, de bouger tous les membres en même temps, de faire des étirements, de placer un cousin entre les genoux en dormant, de ne pas rester trop longtemps en position assise et de pratiquer des exercices pelviens au sol (Kegel). Les deux patientes ont constaté un certain soulagement à la suite du traitement et des soins prodigués chez elles. Les exercices post-partum et de réadaptation ont été prescrits afin de restaurer l’endurance musculaire, le contrôle et la stabilité pelvienne. Après un suivi à long terme, la patiente 1 n’a constaté aucune douleur au niveau de la symphyse pubienne, mais une lombalgie consécutive à une blessure du genou. La patiente 2 ne ressentait presque plus de douleur mise à part une rare ré-exacerbation de la douleur au niveau de la symphyse pubienne.
Resumé
La prise en charge chiropratique conventionnelle semble réduire la douleur et améliorer la mobilité et la fonction de la symphyse pubienne chez les patientes atteintes de DSP. La réadaptation post-partum de la musculature lombo-pelvienne associée à des exercices de stabilisation spécifiques est recommandée en vue de réduire la douleur, améliorer les résultats à long terme et empêcher la chronicité.
Keywords: chiropratique, grossesse, douleurs pelviennes, symphyse pubienne, réadaptation, exercice
Introduction
The incidence of pelvic pain in pregnancy has been reported as between 48–71%.1,2,3 Pubic symphysis dysfunction has been reported in 31.7% of pregnant women.1 The reporting of symphysis pubis pain is also rising due to low reports in the past and/or greater recognition by practitioners.1,2,3 There are many terms describing pelvic pain in pregnancy, including peripartum pelvic pain, Pregnancy-related Pelvic Pain (PRPP), Pregnancy-related pelvic girdle pain (PGP), anterior or posterior pelvic pain, and symphysis pubis dysfunction (SPD). This case report will use SPD as its main descriptor, since this was the primary complaint in both cases. SPD has been long recognized as an obstetrical condition in the literature but, until recently, there has been a lack of clinical interest.2 It is often confused with diastasis pubis (a separated symphysis pubis of more than 10 mm, or symphysiolysis), pelvic rupture (rupture of the symphysis pubis and sacroiliac joints simultaneously, which is extremely rare), and even osteitis pubis (partial or complete rupture of the symphysis pubis and requires aggressive treatment).2,3 The disability related to symphysis pubis pain in pregnancy can vary from mild to severe, but is significant and any therapy that can help to reduce the discomfort is a welcome possibility.2,3,4,5
Symptoms of SPD:
“shooting” pain in the symphysis pubis;
radiating pain into the lower abdomen, back, groin, perineum, thigh, and/or leg;
pain on movement, especially walking, unilateral weight bearing or hip abduction;
pain with activities of daily living, including bending forward, standing on one leg, rising from a chair, go up or down stairs, turning in bed;
pain relieved by rest;
clicking, snapping or grinding heard or felt within the symphysis pubis;
dyspareunia;
occasional difficulty voiding;
Signs of SPD:
tenderness over the pubic symphysis and/or sacroiliac joints;
palpable gap in the pubic symphysis;
suprapubic oedema and swelling;
positive Trendelenberg’s sign on one or both sides;
positive Lesague’s sign on one or both sides;
Patrick test may be positive;
waddling gait with short steps;
paravertebral, gluteal, and piriformis muscles and sacrotuberous ligament tenderness.2,4
self-administered tests (alternative to the painful but highly sensitive and specific symphysis pubis palpation): pain drawing and a painful MAT-test (patient abducts and adducts the hip, simulating the movement of pulling a mat). These have shown the same results as palpation without the increased discomfort.6
Differential diagnosis for SPD:2,4,7
Ectopic pregnancy,
STDs,
urinary tract infection,
round ligament pain,
femoral vein thrombosis,
nerve compression (intervertebral disc lesion),
pubic osteolysis,
osteitis pubis,
bone infection (osteomyelitis, TB, syphilis),
tumours,
mechanical low back pain,
myofascial pain,
pelvic inflammatory disease,
cysts,
IUD displacement,
endometriosis,
postpartum fracture,
abscess,
pelvic mass,
osteomyelitis,
osteoporosis.
Theoretical causes of SPD:3,4,5
biomechanical strains of the pelvic ligaments and associated hyperlordosis,
anatomical pelvic variations,
metabolic (calcium) and hormonal (relaxin and pro-gesterone) changes leading to ligamentous laxity,
pathological weakening of the joint,
tearing of the fibrocartilagenous disc during delivery,
narrowing, sclerosis and degeneration of the joint,
muscle weakness
increased fetal and pregnancy-related weight gain.
Predisposing factors for SPD and pelvic pain:2,3,4,7,9,10
genetics,
family history,
personal pregnancy history,
early menarche,
oral contraceptive use,
multiparity,
high weight,
high levels of stress,
low job satisfaction,
history of low back pain,
previous pelvic or back pathology or trauma,
history of back or pelvic injury,
lack of regular exercise (including long-distance running specifically),
hypermobility,
macrosomia or post-term delivery in pregnancy in labour,
postpartum breast feeding
neonatal developmental hip dysplasia.
The onset of pregnancy-related SPD can vary, with 74% in a first pregnancy and 12% in the first trimester, 34% in the second trimester and 52% in the third trimester.4 Women who develop SPD during pregnancy generally have a good prognosis, as delivery is usually curative. Most women’s pain regresses over the first 1–6 months post partum, with 25% having pain 4 months post partum and only a small number after 12 months.2,4 The exception to this are patients who may develop SPD after a traumatic delivery, which is approximately 1–17.4% of women.2,4 One study reported that non-invasive Doppler imaging of asymmetric laxity of the sacroiliac joints in women with moderate to severe pelvic pain in pregnancy can help to predict persistent pain postpartum (by three times).11 It has also been found that the higher intensity of pain reported during pregnancy and an earlier onset were predictive of pelvic pain persisting post partum.11 The rates of reoccurrence have been reported between 41–77%, including 85% with a new pregnancy, 53–72% with menstruation, 22% with breast feeding.2,4
Case Reports
Case 1
A 30 weeks pregnant, 35-year-old marketing professional presented with pre-partum anterior pelvic pain in her pubic symphysis (worse on the left), left sided low back pain and radiating pain to her inner thigh with standing. She reported the pain had been present for one week prior and was constant. She had no prior occurrence of this type of pain, as this was her first pregnancy. She described the pain as “shooting” and rated it as severe (but could not quantify it when asked a numerical value on the visual analogue scale). She stated that the pain was progressively getting worse over time and greatly interfered with the activities of her daily life, such as walking, stairs, sitting, lying on her sides, rolling over in bed and getting in and out of the car. Relieving factors included lying down in the supine position, having her legs lifted for her and keeping her legs together with most movements. She reported having no previous chiropractic care or any other therapies. She reported taking no medications, and supplementing with a prenatal vitamin and folic acid. She reported that her sleep was “good” and usually lasted 8 hours per night but that she did have some night pain with rolling over in bed. She did not smoke, exercised three times per week (cardiovascular and weight training), and rated her diet as “good”. She reported a previous motor vehicle collision, wisdom teeth surgery and E. coli poisoning in her personal medical history. She stated that she had not been diagnosed with any medical conditions and that she had no significant health conditions in her family history. The red flags were negative (no bowel/bladder function problems, no weight loss, no night sweating, no fevers or infections) and she reported no other areas of complaint.
The physical examination revealed that the visually estimated ranges of motion in the lumbar spine were painful and limited in all directions (by approximately 25% in flexion, rotation and lateral bending and by approximately 50% in extension). Postural observation demonstrated anterior head carriage, increase thoracic kyphosis and increase lumbar lordosis. Motion and static palpation revealed restricted motion of the left sacroiliac joint and the left pubic symphysis. Soft tissue palpation revealed tight and tender muscles: bilateral lumbar erector spinae, quadratus lumborum, gluteals and iliotibial band (all worse on the left side). Neurological examination was unremarkable in the lower limbs. Positive orthopaedic tests include (reproduced her pain): left Thomas, Patrick/Fabere/Distraction test, belt test (patient performs active straight leg raise while therapist holds sides of ilium or puts a pelvic belt on the patient to see if this relieves pain patient experiences, therefore supporting the use of a belt),12 Ober’s, and side SI compression. Active straight leg raise was initially negative, but was positive later as the pregnancy progressed. Prone tests could not be performed.
The working diagnosis was pregnancy-related SPD and pelvic girdle pain. The prognosis was rated as good, since most cases subside within 6 months post delivery.2 The plan of management included weekly visits consisting of soft tissue trigger point therapy, lateral recumbent Diversified mobilizations to the sacroiliac joints, pelvic blocks and instrument-assisted pubic symphysis adjustments.13–19 Home instructions included wearing a pregnancy support belt (Trainer’s Choice®, see Figure 3) as needed, staying as active as possible, moving as a unit (legs together), stretching bilaterally of the iliopsoas, quadratus lumborum and piriformis muscles, icing the pubic symphysis and lower back (as needed), using a pillow between the knees while sleeping, regular breaks from sitting and pelvic floor (Kegel) exercises. She had five subsequent weekly treatments before she delivered her baby. After the initial visit, the patient reported feeling relief, but that the treatment effects did not last very long. She reported not icing, but that she did do her Kegel exercises. On her second visit, she stated that her pubic symphysis pain was “ok” in the morning, increased by midday and was still aggravated with walking. She stated that the overall intensity of pain had decreased, but was unable to quantify it. She reported that her lower back was somewhat “sore” at night. She was given the pregnancy belt at this visit (as it had to be ordered). On her third visit she reported that sitting for shorter periods of time reduced her pain and the belt greatly helped to decrease her pain with walking. On her fourth, fifth and sixth visits she reported that the baby was “lower” in her abdomen and that her pain had plateaued to a “manageable” state.
Figure 3.
Pregnancy pelvic support belt (Trainer’s Choice®)
After approximately eight and a half hours of labour and four hours of active pushing/delivery, the patient delivered a healthy 9lb 5oz baby girl five days past full term.
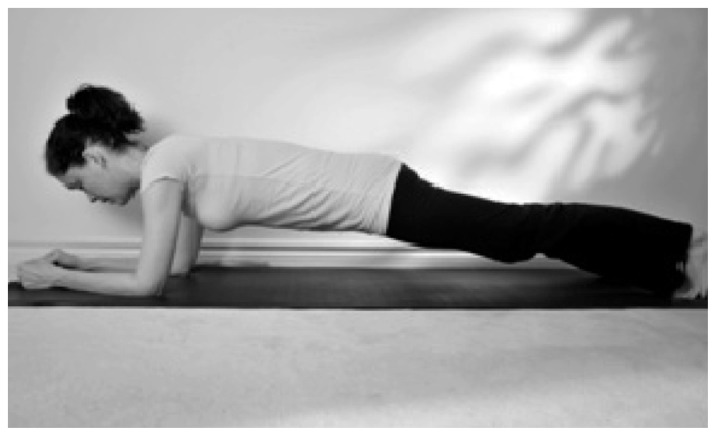
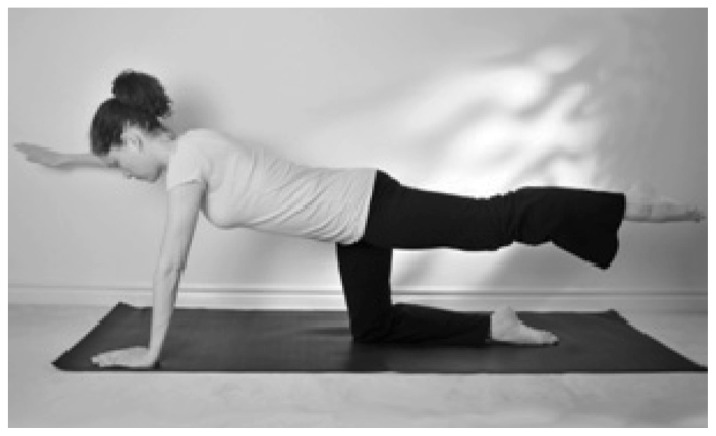
She presented three months post partum after injuring her low back after overexerting herself while doing squats and jumping. She reported that the pubic symphysis pain had started to decrease one week after delivery and was better three months later, with only a little soreness on the left side. She reported that her right sacroiliac joint was now achy and sharp in certain positions. On physical re-examination, the positive orthopaedic tests included: PA SI compression and bilateral Kemp’s. Lumbar spine ranges of motion were restricted with flexion (by approximately 25%), extension (by approximately 75%) and left rotation and lateral bending (by approximately 25%). Static and motion palpation revealed a restrictions at the L4/5 and the right SI joint. Soft tissue palpation revealed tight and tender bilateral lumbar spine erector spinae, quadratus lumborum and gluteal muscles. The working diagnosis was acute right sacroiliac joint dysfuntion and myofascial strain. Treatment included interferential current (IFC), soft tissue trigger point therapy and lateral recumbent sacroiliac and lumbar spine Diversified adjustments.13,14 Home recommendations included: icing, Epson salts baths, continuing pelvic floor exercises (Kegels), as well as adding deep abdominal bracing and gluteus maximus activation during her daily activities to re-establish her core strength and endurance. On her next visit four days later she reported the pain was much better, having greatly decreased in intensity had an increase in her mobility. She reported that taking over-the-counter Tylenol® helped as well. After a similar treatment, home recommendations included the same as the previous visit with the addition of short distance walking (within her tolerance and gradually building up to greater distances and speeds). On the next visit one week later she reported her pain worsening after prolonged standing, but that the pain had resolved again. The next visit nine days later she reported that her back was overall improved and only felt “stiff.” The following visit five days later she reported occasional mild pain and much greater mobility. At this point, she was prescribed rehabilitation exercises progressed to include: prone planks on knees and working to straight legs (instead of modified curl ups, since she tested positive for rectus diastasis with palpation during a supine curl up), side bridges (on knees and working to straight legs) and later bird-dogs (at first with one leg, then one arm working to opposite leg and arm), all in a neutral spine posture and deep rectus abdominus contraction (see figures 4A, 4B, 5A, 5B & 6). The exercises were instructed to be performed daily with 8–10 second holds and progress to more repetitions as tolerated.20
Figure 4A.
Beginner prone plank (on knees)
Figure 4B.
Advanced prone plank (straight legs)
Figure 5A.
Beginner side bridge (on knees)
Figure 5B.
Advanced side bridge (straight legs)
Figure 6.
Bird dog
The patient reported a minor set-back a two weeks later after a long walk while wearing her baby in a front loading baby carrier on the treadmill. Advice was given to walk shorter distances without wearing the baby (which overloaded her anteriorly) and to continue to work on her core endurance training. She had two subsequent visits and reported relief after each, but then then cancelled her next appointment due to scheduling difficulties. The patient then returned to work at 6 months post-partum and therefore was not able to return for treatment.
On long term follow-up (eleven months later) the patient reported low back pain secondary to a knee injury. She reported that the pubic symphysis pain had not returned after it had originally dissipated a few months post partum. She is currently seeing another health professional who is located close to her work.
Case 2
A 30 weeks pregnant, 33-year-old physiotherapist presented with pre-partum right-sided pubic symphysis pain for one week and right sided sacroiliac pain for the previous three months. She described the sacroiliac pain as sharp and intermittent. She reported the pubic symphysis pain as constant and “shooting”. She reported no prior occurrence of this type of pain, as this was her first pregnancy. Activities of daily living that were most affected were turning and standing on one leg at a time (i.e. getting dressed). She reported that the pain worsened as the day progressed and that it was interfering with her work. Relieving factors included wearing a soft elastic pregnancy support belt. Previous therapies included three monthly massage therapy treatments. She reported that she had never received any previous chiropractic care. She reported taking no medications and taking only Pregvit pre-natal vitamins daily. She was a non-smoker, who walked regularly for exercise and rated her diet as “good”. She reported sleeping well for 6–7 hours per night. Her previous history included a right sided knee injury, left elbow surgery, low blood pressure and a history of migraine headaches. She reported having no medical conditions or any relevant family history of medical conditions. Red flags were unremarkable.
The physical examination revealed the visually estimated lumbar ranges of motion to be painful and limited in left rotation (by approximately 25%). Motion and static palpation revealed restricted motion of the right sacroiliac joint and pubic symphysis. Soft tissue palpation revealed tight and tender bilateral gluteal, piriformis, quadratus lumborum, iliotibial bands and psoas muscles. Positive orthopaedic tests (which reproduced the pain she was experiencing) included: bilateral standing Kemp’s, right sided active straight leg raise and belt test.12 Neurological examination of the lower extremities was unremarkable. The working diagnosis was pregnancy-related SPD and posterior pelvic pain due to pregnancy. The prognosis was deemed as good, since most SPD cases tend to resolve after delivery.2 The plan of management included soft tissue trigger point therapy, lateral recumbent Diversified sacroiliac mobilizations, pelvic blocking and instrument-assisted pubic symphysis adjustments.13–19 Home care advice included ice (at the pubic symphysis and lower back as needed), moving as a unit (legs together), pelvic floor exercises (Kegels), gluteus maximus activation and a more structured and supportive pregnancy specific pelvic belt (Trainer’s Choice®, see Figure 3), staying as active as possible, stretching bilaterally of the iliopsoas, quadratus lumborum and piriformis muscles, and using a pillow between the knees while sleeping. On her second visit, the patient reported that she felt much better after the first treatment. She stated that she had scaled back to working half days, since she was pain free in the morning but was re-aggravated by the end of her first full day back. She also reported that the more structured belt really helped her symptoms.
The patient did not return for treatment until after her delivery. After 10 hours of labour and 2 hours of attempted delivery/pushing, the delivering obstetrician used forceps to deliver a healthy 8 lb 1 oz boy at full term.
The patient presented three months post-partum reporting some symphysis pubis pain, no sacroiliac pain and some thoracic spine pain secondary to nursing. She reported that her obstetrician suspected the pubic symphysis pain may have been due to a pubic symphysis separation during the instrument assisted birth. Aggravating factors included sitting on the toilet, standing on one leg, long walks and lifting heavy objects. Relieving factors included wearing the belt, sitting and lying down. Physical re-examination revealed limited visually estimated lumbar ranges of motion with extension, lateral bending and bilateral rotation (all by approximately 25%). Soft tissue palpation revealed tight and tender bilateral thoracic and lumbar erector spinae, rhomboids, trapezius and psoas muscles. Static and motion palpation revealed restrictions at T4-6, T8-10, and the right side of her pubic symphysis. The working differential diagnoses were SPD (secondary to delivery-related trauma), pubic symphysis separation and mechanical thoracic spine dysfunction (secondary to postural strain). Treatment included soft tissue trigger point therapy, lateral recumbent Diversified spinal manipulative therapy, instrument-assisted pubic symphysis adjustments and pelvic blocks.13–19 Home care and rehabilitation exercise advice included: pelvic floor exercises (Kegels), deep abdominal bracing, gluteus maximus activation, stretching of the quadratus lumborum, iliopsoas and pectoral muscles, using a stool while using the toilet, and postural correction. On the next visit one week later she reported tenderness in her pubic symphysis after walking a long distance without wearing the belt. Prone planks (instead of curl-ups, as the patient tested positive for rectus diastasis) and side planks in a neutral spine posture with rectus abdominus contracted were prescribed (see figures 4A, 4B, 5A & 5B). She was instructed to perform the exercises daily with 8–10 second holds and progress to more repetitions and more difficult positions as tolerated (pain free).20 A few weeks later, the patient reported that she had no pubic symphysis or low back pain and that she was able to walk longer and even go on hikes. Two months later the patient came in for treatment for her thoracic spine stiffness and reported her pubic symphysis was still pain free. The patient then moved away from the area seven months post partum, so treatment was discontinued.
On long-term twelve-month post-partum follow-up, she reported being mostly pain free. She stated that she very rarely had mild pubic symphysis pain and sacroiliac pain depending on the type of activity she was doing. Aggravating factors include walking too much, shovelling, lifting any heavy weight, lunges, side squats, and planting her right foot and pivoting (i.e. transferring patients at work). She reported she was planning on using an SI belt at work (since it seemed to relieve her pain), but that she had discontinued doing the rehabilitation exercises.
Discussion
Conservative management of SPD can include pelvic support belts, which have been studied in the literature with contradictory results. One paper reported that belts are no better than exercise alone and recommended that patients strengthen their musculature for longer term stability instead.1 Subjects were given an exercise booklet with un-specified exercises to be performed 3 times daily using a logbook and had a single demonstration.1 Another study recommended 50N of tension and a higher belt position (just caudal to the anterior superior iliac spines) to resist pelvic shear.21 Pelvic belts have also been found to significantly decrease mobility in the sacroiliac joints.12 A belt has also been theorized to be most helpful in the later stages of pregnancy, when deep abdominal muscle activation is not possible, since the belt provides a “locked in” position to decrease the hypermobility in the pelvis that is associated with pregnancy related changes.22 It has been recommended to do muscular core training postpartum to provide this intrinsic stability.22
Other treatments include elbow crutches, a walking frame or wheelchair may have to be used when mobility is compromised in extremely painful cases.2 Simple analgesics can be recommended by the obstetrician or midwife.2,22 TENS, rest, ice, heat, massage, acupuncture and mobilization or manipulation help to reduce discomfort as well.2,5,7,22 One retrospective case report of osteopathic treatment of SPD showed positive results (including soft tissue massage, manipulation the thoracolumbar junction, muscle energy and articulatory mobilization technique to the symphysis pubis, L5 and left innominate and strain-counterstrain technique).22 Chiropractic treatment (including interferential therapy, massage, gentle lateral recumbent mobilization, home cryotherapy and exercises) has been shown to be beneficial and effective in treating SPD in one study that surveyed SPD patients and their chiropractors.8 Postural and ergonomic advice, use of a wedge-shaped pillow, and self-help group information may also help.2 In rare extreme cases of SPD and/or symphysis pubis separation, referral to an orthopaedic surgeon for suturing of the symphysis pubis or a pubic wedge resection may be a last resort treatment.2
Rehabilitation exercise during pregnancy should include isometric and non-isometric exercises with short arc movements of the lower limbs and the avoidance of one-sided movement combinations to prevent aggravating symptoms.24,25 Also, supporting musculature should be targeted locally and globally to support the entire pelvis and low back, including aerobic conditioning, light stretching, relaxation exercises and ergonomic advice.24,25 Water aerobics have been found to help reduce pain and sick days in pregnant women with low back and pelvic pain.23 Much of the research states that individualized physical therapy has shown to lead to better functional outcomes and reduction in pain, but many of the articles do not specify what exercises are prescribed, the dose and the reasons they are chosen.23 One article prescribed three pelvic girdle stabilizing exercises (using a ball between the knees in sitting, standing and kneeling position), plus four strengthening exercises (lateral pulls, standing leg-press, sit-down rowing and curl-ups), as well as stretching of the hamstrings, hip flexors and calf muscles to pregnant participants.5 Unfortunately they found no difference in any of their three groups (information, home exercise and in clinic exercise groups) during pregnancy or on follow-up.5
Post-partum rehabilitation exercise prescription recommendations include: restoring hip stability, lumbo-pelvic stability and motor control by training the transverse abdominis and multifidus muscles, activating the related muscle-fascia-tendon slings and pelvic floor muscles, with slow progressions within patient tolerance.3,5,10 These muscle slings connect with ligaments and fascia to contribute to stability and create a compressive “force closure” on the pelvis.10 This differs from “form closure” of the closely fitting joint surfaces that help to allow the pelvis to resist shear forces.10 Transversus abdominis contraction has been shown to decrease the laxity of the sacroiliac joint in non-pregnant women, while women with pelvic pain three years postpartum have been found to have poor muscle function.12 Stuge et al. used a specific stabilization exercise program to improved functional status and reduce pain in women with postpartum pelvic pain.10 The program included specific transversus abdominis training during daily activities with multifidus coactivation, as well as gluteus maximus, abdominal obliques, erector spinae, quadratus lumborum, hip abductors and adductors training.10 The participants exercised 30–60 minutes, 10 repetitions per exercise, 3 days per week for 18–20 weeks.10 The success of this program was helped by individual training, the use of a training diary, as well as having home equipment.10 The authors found that the participants who did the specific exercises had less pain, improved function and a better quality of life.3,5,10
Pelvic pain is a common presentation in chiropractic practices (up to 23.6% of patients), but chiropractors report that they rarely see pregnant patients.26 Pregnant patients require a gentle, drug-free alternative for treating their discomfort and chiropractic care offers a safe and effective treatment option. In these two cases, it appears that reassurance, symptomatic care of the related structures and advice for self-care improved both patients’ symptoms and their quality of life. The rehabilitation exercises prescribed to the patients had the goal of re-establishing muscular endurance and function to improve overall pelvic stability.
Summary
When reporting on two retrospective pregnancy-related SPD cases, caution must be made to extrapolate any results to other pregnant patient cases since the resolution of their symptoms postpartum could be due to the natural history of the condition. Further study of this condition is recommended to include controls, randomization, the use of objective outcome measures and larger groups with specific individualized exercises. Although SPD tends to be a self-limiting condition, it is a very difficult condition for patients to cope with while they are pregnant. Therefore, it is important to investigate further how to manage this early and proficiently to reduce patient’s pain, improve their outcomes and prevent chronicity.
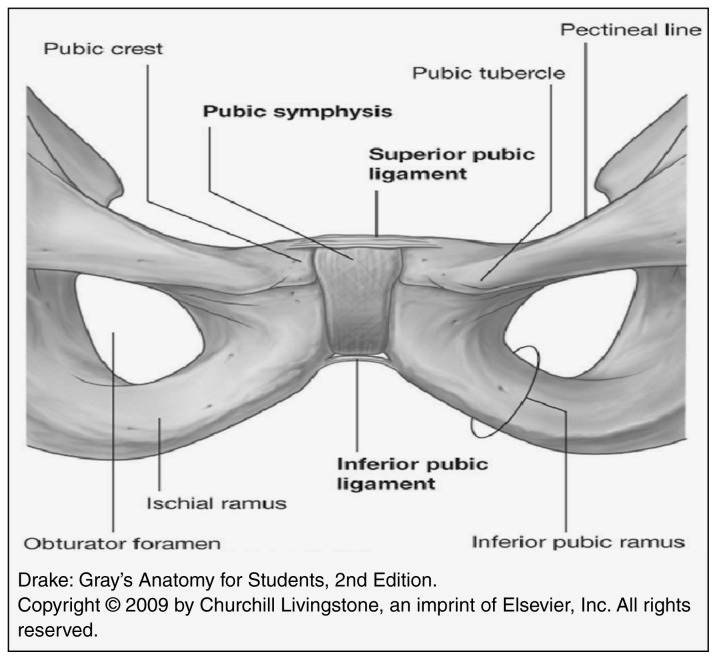
Figure 1.
Pubic symphysis and associated ligaments
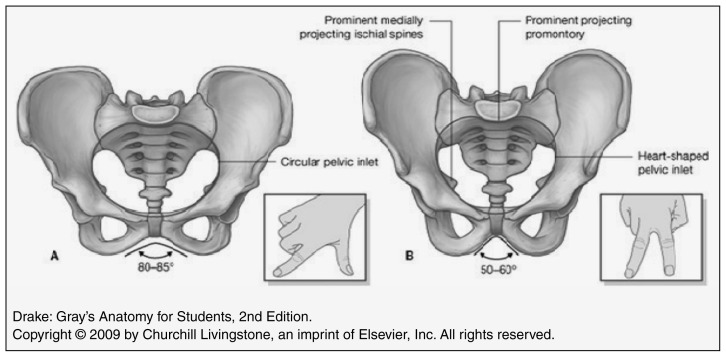
Figure 2.
Structure of the bony pelvis. A. In women. B. In men. The angle formed by the pubic arch can be approximated by the angle between the thumb and index finger for women and the angle between the index finger and middle finger for men as shown in the insets.
Acknowledgements
I would like to thank Dr. Karen Hudes and Dr. Erica Mockler for editing and retrieving some of the references required for this paper.
References
- 1.Depledge J, McNair PJ, Keal-Smith C, Williams M. Management of symphysis pubis dysfunction during pregnancy using exercise and pelvic support belts. Physical Therapy. 2005;85(12):1290–1300. [PubMed] [Google Scholar]
- 2.Leadbetter RE, Mawer D, Lindow SW. Symphysis pubis dysfunction: a review of the literature. J Maternal-Fetal Neonatal Medicine. 2004;16:349–354. doi: 10.1080/14767050400018247. [DOI] [PubMed] [Google Scholar]
- 3.Borg-Stein J, Dugan SA. Musculoskeletal disorders of pregnancy, delivery and postpartum. Phys Med Rehabil Clin N Am. 2007;18(3):459–476. doi: 10.1016/j.pmr.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 4.Leadbetter RE, Mawer D, Lindow SW. The development of a scoring system for symphysis pubis dysfunction. J Obstetrics Gynecology. 2006;26(1):20–23. doi: 10.1080/01443610500363915. [DOI] [PubMed] [Google Scholar]
- 5.Nilsson-Wikmar L, Holm K, Oijerstedt R, Harms-Ringdahl K. Effect of three different physical therapy treatments on pain and activity in pregnant women with pelvic girdle pain: a randomized clinical trial with 3, 6, and 12 months follow-up postpartum. Spine. 2005;30(8):850–856. doi: 10.1097/01.brs.0000158870.68159.d9. [DOI] [PubMed] [Google Scholar]
- 6.Olsen MF, Gutke A, Elden H, Nordenman C, Fabricius L, Gravesen M, Lind A, Kjellby-Wendt G. Self-administered tests as a screening procedure for pregnancy-related pelvic girdle pain. Eur Spine J. 2009;18(8):1121–1129. doi: 10.1007/s00586-009-0948-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karadeli E, Uslu N. Postpartum sacral fracture presenting as lumbar pain. J Women’s Health. 2009;18(5):663–665. doi: 10.1089/jwh.2008.1189. [DOI] [PubMed] [Google Scholar]
- 8.Andrews C, Pedersen P. A study into the effectiveness of chiropractic treatment for pre- and postpartum women with symphysis pubis dysfunction. Eur J Chiro. 2003;48(3):77–95. [Google Scholar]
- 9.Cook C, Massa L, Harm-Ernandes I, Segneri R, Adcock J, Kennedy C, Figuers C. Interrater reliability and diagnostic accuracy of pelvic girdle pain classification. JMPT. 2007 May;30(4):252–258. doi: 10.1016/j.jmpt.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 10.Stuge B, Laerum E, Kikesola G, Vollestad N. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: a randomized controlled trial. Spine. 2004;29(4):351–359. doi: 10.1097/01.brs.0000090827.16926.1d. [DOI] [PubMed] [Google Scholar]
- 11.Damen L, Buyruk HM, Guler-Uysal F, Lotgering FK, Snijders CJ, Stam HJ. The prognostic value of asymmetric laxity of the sacroiliac joints in pregnancy-related pelvic pain. Spine. 2002;27(24):2820–2824. doi: 10.1097/00007632-200212150-00018. [DOI] [PubMed] [Google Scholar]
- 12.Mens JMA, Damen L, Snijeders CJ, Stam HJ. The mechanical effect of a pelvic belt in patients with pregnancy-related pelvic pain. Clin Biomechanics. 2006;21(2):122–127. doi: 10.1016/j.clinbiomech.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 13.Esch S, Zachman Z. Adjustive procedures for the pregnant chiropractic patient. Chiro Tech. 1991;3(2):66–71. [Google Scholar]
- 14.Guadagnino MR. Spinal manipulative therapy for 12 pregnant patients suffering from low back pain. J Chiro Tech. 1999;11(3):108–111. [Google Scholar]
- 15.Hochman JI. The effect of sacro occipital technique category II blocking on spinal ranges of motion: a case series. JMPT. 2005;28(9):719–723. doi: 10.1016/j.jmpt.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 16.Troyanovich SJ, Harrison DE, Harrison DD. Structural rehabilitation of the spine and posture: rationale for treatment beyond the resolution of symptoms. JMPT. 1998;21(1):37–50. [PubMed] [Google Scholar]
- 17.Colloca CJ, Keller TS, Black P, Normand MC, Harrison DE, Harrison DD. Comparison of mechanical force of manually assisted chiropractic adjusting instruments. JMPT. 2005;28(6):414–422. doi: 10.1016/j.jmpt.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 18.Taylor SH, Arnold ND, Biggs L, Colloca CJ, Mierau DR, Symons BP, Triano JJ. A review of the literature pertaining to the efficacy, safety, educational requirements, uses and usage of mechanical adjusting devices. Part 1 of 2. J Can Chiropr Assoc. 2004;48(1):74–108. [PMC free article] [PubMed] [Google Scholar]
- 19.Taylor SH, Arnold ND, Biggs L, Colloca CJ, Mierau DR, Symons BP, Triano JJ. A review of the literature pertaining to the efficacy, safety, educational requirements, uses and usage of mechanical adjusting devices: Part 2 of 2. J Can Chiropr Assoc. 2004;48(2):152–179. [PMC free article] [PubMed] [Google Scholar]
- 20.McGill SM. Low back disorders: Evidence based prevention and rehabilitation. Second Edition. Human Kinetics Publishers; Champaign, IL, U.S.A: 2002. p. 2007. [Google Scholar]
- 21.Damen L, Spoor CW, Snijeders CJ, Stam HJ. Does a pelvic belt influence sacroiliac joint laxity? Clin Biomechanics. 2002;17(7):495–498. doi: 10.1016/s0268-0033(02)00045-1. [DOI] [PubMed] [Google Scholar]
- 22.Cassidy IT, Jones CG. A retrospective case report of symphysis pubis dysfunction in a pregnant woman. J Osteopath Med. 2002;5(2):83–86. [Google Scholar]
- 23.Stuge B, Hilde G, Vollestad N. Physical therapy for pregnancy-related low back and pelvic pain: a systematic review. Acta Obstet Gynecol Scand. 2003;82(11):983–990. doi: 10.1034/j.1600-0412.2003.00125.x. [DOI] [PubMed] [Google Scholar]
- 24.Mens JMA, Snijders CJ, Stam HJ. Diagonal trunk muscle exercises in peripartum pelvic pain: A randomized clinical trial. Physical Therapy. 2000;80(12):1164–1173. [PubMed] [Google Scholar]
- 25.Sanders SG. Dancing through pregnancy: activity guidelines for professional and recreational dancers. J Dance Med Sci. 2008;12(1):17–22. [PubMed] [Google Scholar]
- 26.National Board of Chiropractic Examiners. Practice analysis of chiropractic. Chapter 8: Patient conditions. 2010:95–120. [Google Scholar]