Abstract
Objective
To chronicle the conservative treatment and management of a 32-year old female patient presenting with radial wrist pain of 4 months duration, diagnosed as De Quervain’s stenosing tenosynovitis.
Clinical features
The primary clinical feature is wrist pain at the radial styloid with resultant impairment of wrist, hand, and thumb function.
Intervention and outcome
The conservative treatment approach consisted of activity modification, Graston Technique®, and eccentric training. Outcome measures included verbal pain rating scale, QuickDASH Disability/Symptom Score, and a return to activities of daily living (ADLs). The patient attained symptom resolution and at 6 month follow-up reported no recurrence of wrist pain.
Conclusion
A combination of conservative rehabilitation strategies may be used by chiropractors to treat De Quervain’s stenosing tenosynovitis and allow for an individual to return to pain free ADLs in a timely manner.
Keywords: radial wrist pain, stenosing tenosynovitis, De Quervain’s, Graston Technique®, eccentric training
Abstract
Objectif
Rendre compte du traitement et de la prise en charge conventionnels d’une patiente âgée de 32 ans souffrant de douleurs au bord radial du poignet depuis 4 mois, qui avait reçu le diagnostic de ténosynovite sténosante de De Quervain.
Caractéristiques cliniques
La principale caractéristique clinique est la douleur au poignet au niveau de la styloïde radiale ayant pour conséquence une défaillance de la fonction du poignet, de la main et du pouce.
Intervention et résultat
L’approche conventionnelle du traitement a inclus un changement de ses activités, la technique Graston® et un entraînement excentrique. Dans les indicateurs de résultats, on a pris en compte notamment l’échelle verbale d’évaluation de la douleur, le questionnaire QuickDASH/Symptom Socre, et la reprise de ses activités de la vie quotidienne (AVQ). Les symptômes de la patiente ont disparu et, après six mois de suivi, elle n’a constaté aucune réapparition de ses douleurs au poignet.
Conclusion
Les chiropraticiens peuvent avoir recours à une combinaison des stratégies conventionnelles de réadaptation afin de traiter la ténosynovite sténosante de De Quervain et permettre aux patients de reprendre rapidement leurs activités de la vie quotidienne sans souffrir.
Keywords: douleurs au niveau du bord radial du poignet, ténosynovite sténosante, De Quervain, technique Graston®, entraînement excentrique
Introduction
De Quervain’s stenosing tenosynovitis (DQST) is a disorder that is characterised by wrist pain and tenderness at the radial styloid.1,2 It is caused by impaired gliding of the tendons of the abductor pollicis longus (APL) and extensor pollicis brevis (EPB) muscles.1 These musculotendinous units control the position and orientation, force application and joint stability of the thumb. The impaired gliding is believed to be as a result of thickening of the extensor retinaculum at the first dorsal (extensor) compartment of the wrist, with subsequent narrowing at the fibro-osseous canal.3–7 Severe cases of DQST have been associated with extensor retinaculum thickening that is three to four times greater than normal.3,5
The term “tenosynovitis” implies the presence of an inflammatory condition. However, the pathophysiology of DQST does not involve inflammation and has histopathological findings similar to those of other tendinopathies such as fibrocartilagenous metaplasia, deposition of mucopolysaccharide,8,9 and neovascularization.10 Neovascularization is known to be accompanied by an in-growth of nerve fascicles that have both sensory and sympathetic components capable of transmitting pain.11 Thus, the mechanical impingement of the APL and EPB tendons in the narrowed fibro-osseous canal is the likely stimulus of nociceptors and pain.7,8 This creates resultant impairment of wrist, hand, and thumb function with activities such as lifting, pushing, pulling, and gripping.
In a large community based study from the United Kingdom, the prevalence of DQST was found to be 0.5% in men and 1.3% in women.12 Epidemiological studies in industrial settings have shown a point prevalence of 8% when wrist pain and a positive Finkelstein’s test, with or without tenderness to palpation of the radial wrist were used as diagnostic criteria.13,14 The highest prevalence of DQST has been reported among subjects 30–55 years of age.1,3,5 There are no reports available that definitively describe the natural history of untreated DQST.2
According to the National Board of Chiropractic Examiners 2005 Job Analysis of Chiropractic, the chief presenting complaint on initial visit of 8.3% of chiropractic patients in 2003 was in an upper extremity.15 Chronic tendon pathology is a soft tissue condition commonly seen in chiropractic practice.16 Chiropractors offer a number of conservative interventions that can be employed to treat tendinopathy.17 This case study was conducted to chronicle the conservative treatment and management of a 32-year old female patient presenting with chronic pain at the radial styloid diagnosed as DQST.
Case report
A 32-year old, right hand dominant female presented with gradual onset over four months of right-sided radial wrist pain. The patient was a stay at home mother. Her pain started after pulling her two children (boys aged seven months and three years old) in a wagon during her daily walks. She originally felt only mild discomfort in the right wrist and base of the thumb that did not limit any of her activities of daily living (ADLs). Over the following weeks, she noticed a gradual increase in her wrist and thumb pain, especially after holding her seven-month old son at her side. She visited her family physician who provided a diagnosis of “tendonitis.” The physician recommended over the counter medication (ibuprofen), and a thumb spica splint to manage her symptoms. She found the thumb spica splint to be cumbersome and impractical during participation in most household chores and child minding activities, and therefore discontinued use.
The patient rated her current pain level on the Verbal Pain Rating Scale (VPRS) where 0 is “no pain” and 10 is the “worst pain that she had ever experienced”. She reported her pain as ranging from 3/10 at rest to 8/10 when aggravated by activity. Evaluation of her disability was completed using the QuickDASH (disability of the arm, shoulder and hand). Her QuickDASH Disability/Symptom Score (QDDSS) was 80 out of a possible score of 100. The pain was described as a constant ache that became sharp in character with use of her right hand. This resulted in functional limitations with many of her ADLs (i.e. meal preparation, carrying laundry and groceries, home cleaning duties, vacuuming, picking up her children). She did not report any other previous history of significant right upper extremity injury. A systems review and family health history was unremarkable.
Upon examination, inspection did not reveal any swelling of the right wrist, hand, or thumb. A cervical spine screen and neurological screen (reflex, motor, sensory testing) for the upper extremities were within normal limits. Radial nerve tension testing as described by Magee18 and Butler19 was unremarkable. Provocative joint testing and range of motion (ROM) for the right elbow joint were within normal limits. Active wrist ROM revealed discomfort at end ranges of flexion, extension, and radial deviation. Ulnar deviation as well as active thumb extension and abduction movements were limited by 50%. In addition, Finklestein’s test (deviating the wrist to the ulnar side while grasping the thumb) was positive for pain. The first CMC joint grind test18 did not reproduce the patient’s symptoms. There was no reported tenderness with joint play of the metacarpals and no evidence of instability. Palpation revealed tenderness and hypertonicity in the muscles of the thenar eminence (Abductor Pollicis Brevis, Flexor Pollicis Brevis, and Opponens Pollicis). Soft tissue tenderness with accompanying lumpy tissue texture was palpated most notably in the proximal APL and EPB, and to a lesser extent the extensor muscle groups of the forearm (Extensor Digitorum, Extensor Carpi Radialis Longus and Brevis). Tenderness was also palpated at the radial styloid and first dorsal compartment of the wrist. There was only mild tenderness palpated in the flexor muscle groups of the forearm.
Based on the above historical and physical examination findings the patient was diagnosed with DQST and treatment was initiated. The importance of activity modification and minimizing exposure to positions that aggravated the symptomatic right wrist was discussed at the outset. This included increasing the use of her unaffected left arm and hand during ADLs, task division and pacing strategies, and temporarily assigning some of the problematic household chores to her husband. Graston Technique® (GT®) was administered by a certified provider using GT® protocols to all the affected soft tissues of the right upper extremity. Care was taken in the initial stages to not administer treatment over the painful first dorsal compartment at the radial styloid.
The patient was initially prescribed exercises consisting of static stretching for the thenar muscle group (Figure 1) and forearm extensors/flexors. In addition, eccentric unweighted hammer curl exercises with no concentric component were prescribed (Figure 2A–C). The patient was instructed to assist with the other hand during the concentric (radial deviation) movement phase. In week 3, eccentric thumb extension and abduction exercises with an elastic band (Figure 3 and 4), were introduced. At the beginning of week 5, eccentric wrist extension and flexion exercises with a dumbbell (Figure 5 and 6), along with eccentric forearm pronation and supination exercises with theraband® (Figure 7 and 8) were introduced. All eccentric exercises were performed without the concentric component permitted. A summary of the full rehabilitative exercise treatment protocol is included in Table 1.
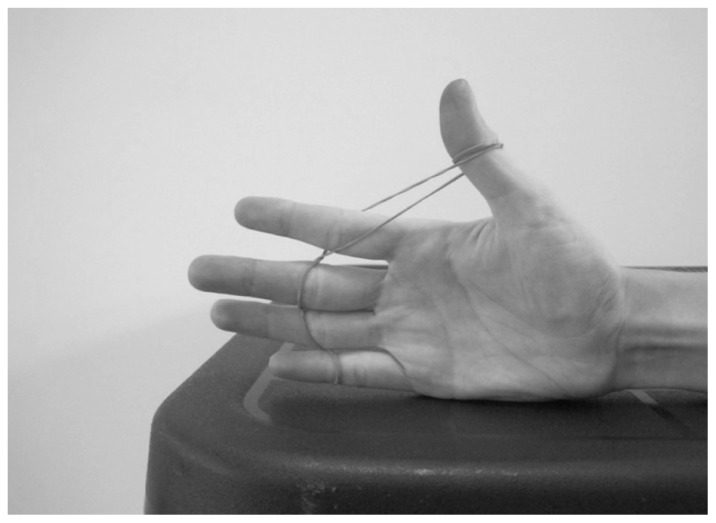
Figure 1.
Stretching for the thenar muscle group
Figure 2.
A–C The eccentric training protocol. (A) The patient starts with the unweighted hand in the hammer curl position. (B) The wrist is then eccentrically loaded by slowly lowering the hand into a position of ulnar deviation. (C) The patient returns to the starting position using the contralateral unaffected hand to avoid concentric loading (radial deviation)
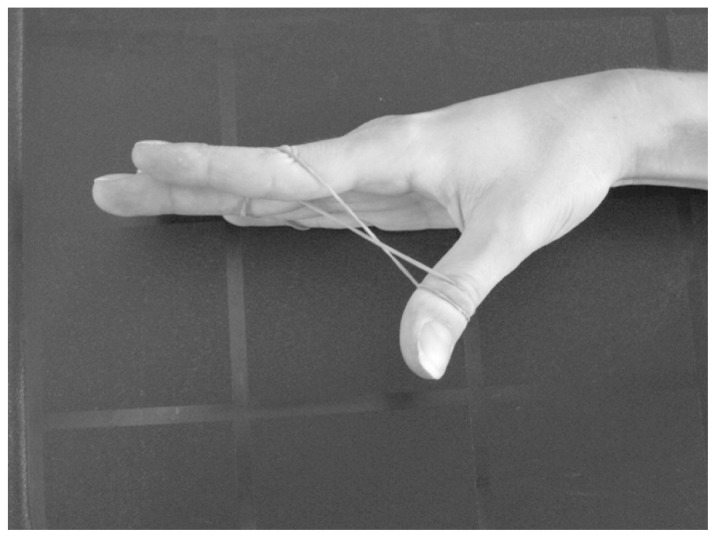
Figure 3.
Starting position for eccentric thumb extension exercise
Figure 4.
Starting position for eccentric thumb abduction exercise
Figure 5.
Starting position for eccentric wrist extension
Figure 6.
Starting position for eccentric wrist flexion
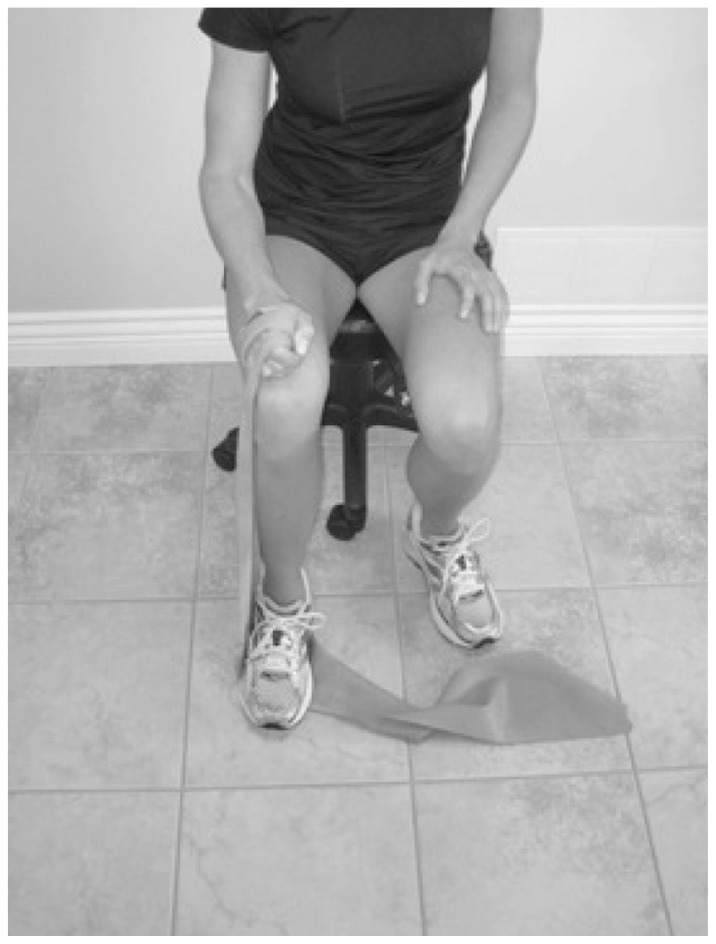
Figure 7.
Starting position for eccentric forearm pronation
Figure 8.
Starting position for eccentric forearm supination
Table 1.
Overview of the rehabilitative exercises prescribed in this case
| EXERCISE | INSTRUCTIONS |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
The patient was seen twice a week for 4 weeks and then once per week for 4 weeks. At the end of week 8, the patient reported a VPRS score of 0/10 consistently at rest, and 1–2/10 with functional activities formerly reported as painful. The patient began gradually resuming her previously problematic ADLs in week 8. She continued with her home exercise program over the next 4 weeks. She had one treatment visit in week 10. At week 12, the patient continued to report a VPRS score of 0/10 at rest, and now reported a VPRS score of 0/10 with resumption of functional activities. Her QDDSS was calculated as 0 indicating no disability. Physical examination at this time was unremarkable for pain, with only mild stiffness reported during Finklestein’s test and end ranges of thumb extension and abduction movements. The patient was subsequently discharged from active care and advised to return if her symptoms recurred. At 6 month follow-up conducted via telephone, the patient reported no recurrence of wrist pain.
Discussion
DQST has traditionally been linked to a combination of repetitive movements involving pronation and supination of the forearm, ulnar and radial deviation of the wrist, and abduction/extension of the thumb.3 It is believed the consequence of this biomechanical overloading is that the extensor retinaculum thickens to resist the cumulative strain.3,4 As a result, individuals who use their thumbs in repetitive pinching, wringing, lifting, grasping, or extension activities with the wrist and hand become susceptible to progressive stenosis in the first dorsal compartment of the wrist.1,4 Welch20 postulated that the primary predisposing factor for the development of DQST is small muscles with inadequate blood supply. He indicates that training the muscles would increase vascular supply thereby decreasing the degree of predisposition. Anatomical variations with partitioning of the first dorsal compartment and its tendons into several sub-compartments and tendon strands has been observed more commonly among individuals with DQST than controls.1,3,4 A relationship between pregnancy and DQST in lactating mothers within the first three months of delivery has also been reported.21–23 Endocrine influences on fluid retention are thought to be the primary contributor to this association,24 although the role of mechanical stress on the thumb from holding the baby may also be responsible.22
Individuals with DQST often report a gradual onset of pain or tenderness at the radial styloid that may be accompanied by swelling.1,3,5 Additional findings on physical examination may include decreased abduction and extension ranges of motion at the first carpometacarpal joint, pain with isometric activation of the APB and EPB tendons, and crepitus of tendons moving through the thickened extensor sheath.25 Finkelstein’s test is typically positive but should not be relied upon as the only finding for diagnosis of DQST. Ruling out other causes of pain along the radial aspect of the wrist and forearm is critical for accurate diagnosis. The superficial radial nerve supplies sensation to the radial aspect of the forearm and wrist, with the anterior terminal branch passing almost directly over the first dorsal compartment and providing sensation to the dorsum of the thumb.1 As a result, an entrapment of the sensory branch of the superficial radial nerve (Wartenberg’s Syndrome) may result in a positive Finklestein’s test. Osteoarthritis of the carpometacarpal joint of the thumb can imitate the pain of DQST and also produce a positive Finkelstein’s test.6 The differential diagnostic list in patients with radial wrist pain should also include C6 cervical radiculopathy, intersection syndrome, intercarpal instabilities, scaphoid fracture, and arthroses of the intercarpal (IC) and radiocarpal (RC) joints.26 Radiographic examination may be useful for ruling out any offending bony pathology.
Initial conservative management of DQST should consist of relative rest and activity modification, primarily to minimize repetitive loading of the first dorsal compartment.27,28 The use of a thumb spica splint is commonly employed to immobilize the wrist and thumb. Splinting may reduce gliding of the APL and EPB tendons through the stenosed fibro-osseous canal, thereby minimizing mechanical impingement of the tendons against the retinaculum.1 As demonstrated in this case, modifying activities to reduce repetitive and sustained loading on the first dorsal compartment may also be sufficient for management.
GT® is a form of augmented soft tissue mobilization (ASTM) in which stainless steel instruments are utilized to apply controlled microtrauma to the affected soft tissues.29 Studies suggest that the controlled microtrauma induces healing via fibroblast proliferation,30 which is necessary for tendon healing.30,31 Additional studies have shown clinical efficacy using GT® for the treatment of various soft tissue disorders.29,32–36 The soft tissue healing effect of GT® was combined with active physical conditioning (Table 1). Resistance exercise is believed to deliver cyclical tensile loads to stimulate the remodelling of collagen31, and has demonstrated efficacy in the management of chronic tendinopathy.37 Eccentric training has demonstrated some application in the treatment of DQST. In a study by Knobloch et al, it was shown that the combined treatment of Power Doppler controlled sclerosing therapy and consecutive eccentric training led to encouraging pilot results in terms of pain reduction and functional improvement within one month of therapy.10 An eccentric exercise program was implemented in this case and well tolerated by the patient.
Corticosteroid injection is a common non-operative treatment utilized in the treatment of DQST. The apparent effectiveness of these injections has been previously reported in a systematic review by Ritchie et al.,38 however, a recent Cochrane Review found major shortcomings with this report.2 The Cochrane group concluded that given the weak evidence base it is not possible to draw any firm conclusions regarding the effectiveness of steroid injections for DQST.2 Furthermore, several potential complications have been cited following steroid injections including local infection and depigmentation of the skin, atrophy of subcutaneous fat, and less frequently, tendon rupture.39,40 Surgical intervention (slitting or removing a strip of the tendon sheath) has been reported to be effective with a 91% cure rate, but is more invasive and associated with higher costs and the possibility of surgical complications.41
The treatment program in this case was multi-modal, thus several factors may have influenced the favourable outcome attained. Initial management consisted of activity modification and minimizing repetitive and sustained loading of the right wrist and thumb regions during problematic ADLs. This prevented ongoing injury and decreased pain levels while still allowing for the patient to participate in less aggravating activities. Graston Technique® was useful in decreasing the soft tissue tenderness and dysfunction and theoretically aiding soft tissue healing. In consideration of the time consuming nature of eccentric loading exercises, it is noted that the patient in this case was strictly compliant with her scheduled office visits and the prescribed active exercise conditioning protocol outlined in Table 1. This active exercise conditioning protocol also likely played an important role in the resolution of radial wrist pain.
Summary
DQST shares histopathological and clinical characteristics similar to other tendinopathies. This case demonstrates the management of DQST using conservative interventions that can be employed by chiropractic practitioners. Although favourable results were obtained, it is important to note that the nature of this investigation was that of a case study, and therefore the treatment protocol utilized may not be appropriate for all individuals presenting with DQST. There is a dearth of quality scientific research documenting conservative management strategies for DQST.42 Interventions that focus on returning individuals back to ADLs in a timely manner require further investigation to evaluate short and long-term benefits.
Acknowledgements
I would like to thank Ms. Anne Taylor-Vaisey, CMCC Reference Librarian for her assistance with searching the literature. I would also like to thank Dr. Sean Delanghe for his assistance with editing and proof reading this manuscript.
References
- 1.Moore JS. De Quervain’s tenosynovitis. Stenosing tenosynovitis of the first dorsal compartment. J Occup Environ Med. 1997 Oct;39(10):990–1002. doi: 10.1097/00043764-199710000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Peters-Veluthamaningal C, van der Windt DA, Winters JC, Meyboom-de Jong B. Corticosteroid injection for de Quervain’s tenosynovitis. Cochrane Database Syst Rev. 2009 Jul 8;(3):CD005616. doi: 10.1002/14651858.CD005616.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finkelstein H. Stenosing tendovaginitis at the radial styloid process. J Bone Joint Surg [Am] 1930;12:509–540. [Google Scholar]
- 4.Muckart RD. Stenosing tendovaginitis of abductor pollicis longus and extensor pollicis brevis at the radial styloid (de Quervain’s disease) Clin Orthop Relat Res. 1964 Mar-Apr;33:201–8. [PubMed] [Google Scholar]
- 5.Lamphier TA, Crooker C, Crooker JL. De Quervain’s disease. Ind Med Surg. 1965;34:847–856. Bibliographic Links. [PubMed] [Google Scholar]
- 6.Kay NR. De Quervain’s disease. Changing pathology or changing perception? J Hand Surg Br. 2000 Feb;25(1):65–9. doi: 10.1054/jhsb.1999.0277. [DOI] [PubMed] [Google Scholar]
- 7.Ilyas AM, Ast M, Schaffer AA, Thoder J. De quervain tenosynovitis of the wrist. J Am Acad Orthop Surg. 2007 Dec;15(12):757–64. doi: 10.5435/00124635-200712000-00009. Review. Erratum in: J Am Acad Orthop Surg. 2008 Feb; 16(2):35A. Ilyas, Asif [corrected to Ilyas, Asif M] [DOI] [PubMed] [Google Scholar]
- 8.Clarke MT, Lyall HA, Grant JW, Matthewson MH. The histopathology of de Quervain’s disease. J Hand Surg Br. 1998 Dec;23(6):732–4. doi: 10.1016/s0266-7681(98)80085-5. [DOI] [PubMed] [Google Scholar]
- 9.Read HS, Hooper G, Davie R. Histological appearances in post-partum de Quervain’s disease. J Hand Surg Br. 2000 Feb;25(1):70–2. doi: 10.1054/jhsb.1999.0308. [DOI] [PubMed] [Google Scholar]
- 10.Knobloch K, Gohritz A, Spies M, Vogt PM. Neovascularisation in de Quervain’s disease of the wrist: novel combined therapy using sclerosing therapy with polidocanol and eccentric training of the forearms and wrists-a pilot report. Knee Surg Sports Traumatol Arthrosc. 2008 Aug;16(8):803–5. doi: 10.1007/s00167-008-0555-5. [DOI] [PubMed] [Google Scholar]
- 11.Andersson G, Danielson P, Alfredson H, Forsgren S. Nerve-related characteristics of ventral paratendinous tissue in chronic Achilles tendinosis. Knee Surg Sports Traumatol Arthrosc. 2007 Oct;15(10):1272–9. doi: 10.1007/s00167-007-0364-2. [DOI] [PubMed] [Google Scholar]
- 12.Walker-Bone K, Palmer KT, Reading I, Coggon D, Cooper C. Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis and Rheumatism. 2004;51(4):642–51. doi: 10.1002/art.20535. [DOI] [PubMed] [Google Scholar]
- 13.Pascarelli EF, Hsu YP. Understanding work-related upper extremity disorders: clinical findings in 485 computer users, musicians, and others. J Occup Rehabil. 2001 Mar;11(1):1–21. doi: 10.1023/a:1016647923501. [DOI] [PubMed] [Google Scholar]
- 14.Punnett L, Robins JM, Wegman DH, Keyserling WM. Soft tissue disorders in the upper limbs of female garment workers. Scand J Work Environ Health. 1985 Dec;11(6):417–25. doi: 10.5271/sjweh.2205. [DOI] [PubMed] [Google Scholar]
- 15.NBCE. Job Analysis of Chiropractic. 2005. http://ibce.org/publication/job-analysis.html.
- 16.Christensen MG, Delle Morgan DR. Job analysis of chiropractic: a project report, survey analysis, and summary of the practice of chiropractic within the United States. Greeley (Colo): National Board of Chiropractic Examiners; 1993. p. 78. [Google Scholar]
- 17.Pfefer MT, Cooper SR, Uhl NL. Chiropractic management of tendinopathy: a literature synthesis. JMPT. 2009 Jan;32(1):41–52. doi: 10.1016/j.jmpt.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 18.Magee DJ. Orthopaedic Physical Assessment. Third Ed. W.B. Saunders Company; 1997. [Google Scholar]
- 19.Butler DS. Mobilization of the Nervous System. London, UK: Churchill-Livingstone; 1991. [Google Scholar]
- 20.Welch R. The causes of tenosynovitis in industry. Ind Med. 1972;41:16–19. [PubMed] [Google Scholar]
- 21.Nygaard IE, Saltzman CL, Whitehouse MB, Hankin FM. Hand problems in pregnancy. Am Fam Physician. 1989;39:123–126. [PubMed] [Google Scholar]
- 22.Schned ES. De Quervain tenosynovitis in pregnant and postpartum women. Obstet Gynecol. 1986;68:411–414. doi: 10.1097/00006250-198609000-00025. [DOI] [PubMed] [Google Scholar]
- 23.Johnson CA. Occurrence of de Quervain’s disease in postpartum women. J Fam Pract. 1991;32:325–327. [PubMed] [Google Scholar]
- 24.Capasso G, Vittorino T, Maffulli N, Turco G, Piluso G. Surgical release of de Quervain’s stenosing tenosynovitis postpartum: can it wait? Int Orthop. 2002;26:23–25. doi: 10.1007/s00264-001-0302-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Backstrom KM. Mobilization with movement as an adjunct intervention in a patient with complicated de Quervain’s tenosynovitis: a case report. J Orthop Sports Phys Ther. 2002 Mar;32(3):86–94. doi: 10.2519/jospt.2002.32.3.86. discussion 94–7. [DOI] [PubMed] [Google Scholar]
- 26.Walker MJ. Manual physical therapy examination and intervention of a patient with radial wrist pain: a case report. J Orthop Sports Phys Ther. 2004 Dec;34(12):761–9. doi: 10.2519/jospt.2004.34.12.761. [DOI] [PubMed] [Google Scholar]
- 27.Rees JD, Maffulli N, Cook J. Management of tendinopathy. Am J Sports Med. 2009 Sep;37(9):1855–67. doi: 10.1177/0363546508324283. [DOI] [PubMed] [Google Scholar]
- 28.Fu SC, Rolf C, Cheuk YC, Lui PP, Chan KM. Deciphering the pathogenesis of tendinopathy: a three-stages process. Sports Med Arthrosc Rehabil Ther Technol. 2010 Dec 13;2:30. doi: 10.1186/1758-2555-2-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hammer WI. The effect of mechanical load on degenerated soft tissue. J Body Mov Ther. 2008 Jul;12(3):246–56. doi: 10.1016/j.jbmt.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 30.Gehlsen GM, Ganion LR, Helfst R. Fibroblast responses to variation in soft tissue mobilization pressure. Med Sci Sports Exerc. 1999 Apr;31(4):531–5. doi: 10.1097/00005768-199904000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Kraushaar BS, Nirschl RP. Tendinosis of the elbow (tennis elbow). Clinical features and findings of histological, immunohistochemical, and electron microscopy studies. J Bone Joint Surg Am. 1999 Feb;81(2):259–78. [PubMed] [Google Scholar]
- 32.Burke J, Buchberger DJ, Carey-Loghmani MT, Dougherty PE, Greco DS, Dishman JD. A pilot study comparing two manual therapy interventions for carpal tunnel syndrome. JMPT. 2007 Jan;30(1):50–61. doi: 10.1016/j.jmpt.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 33.Howitt S, Wong J, Zabukovec S. The conservative treatment of Trigger thumb using Graston Techniques and Active Release Techniques. J Can Chiropr Assoc. 2006 Dec;50(4):249–54. [PMC free article] [PubMed] [Google Scholar]
- 34.Howitt S, Jung S, Hammonds N. Conservative treatment of a tibialis posterior strain in a novice triathlete: a case report. J Can Chiropr Assoc. 2009 Mar;53(1):23–31. [PMC free article] [PubMed] [Google Scholar]
- 35.Black DW. Treatment of knee arthrofibrosis and quadriceps insufficiency after patellar tendon repair: a case report including use of the graston technique. Int J Ther Massage Bodywork. 2010 Jun 23;3(2):14–21. [PMC free article] [PubMed] [Google Scholar]
- 36.Looney B, Srokose T, Fernández-de-las-Penas C, Cleland JA. Graston instrument soft tissue mobilization and home stretching for the management of plantar heel pain: a case series. JMPT. 2011 Feb;34(2):138–42. doi: 10.1016/j.jmpt.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 37.Kristensen J, Franklyn-Miller A. Resistance training in musculoskeletal rehabilitation: a literature review. Br J Sports Med. 2011 Jul 26; doi: 10.1136/bjsm.2010.079376. [DOI] [PubMed] [Google Scholar]
- 38.Richie CA, 3rd, Briner WW., Jr Corticosteroid injection for treatment of de Quervain’s tenosynovitis: a pooled quantitative literature evaluation. J Am Board Fam Pract. 2003 Mar-Apr;16(2):102–6. doi: 10.3122/jabfm.16.2.102. [DOI] [PubMed] [Google Scholar]
- 39.Sampson SP, Wisch D, Badalamente MA. Complications of conservative and surgical treatment of de Quervain’s disease and trigger fingers. Hand Clin. 1994 Feb;10(1):73–82. [PubMed] [Google Scholar]
- 40.Cardone DA, Tallia AF. Joint and soft tissue injection. American Family Physician. 2002;66(2):283–8. [PubMed] [Google Scholar]
- 41.Ta KT, Eidelman D, Thomson JG. Patient satisfaction and outcomes of surgery for de Quervain’s tenosynovitis. J Hand Surgery. 1999;24A(5):1071–7. doi: 10.1053/jhsu.1999.1071. [DOI] [PubMed] [Google Scholar]
- 42.Huisstede BM, van Middelkoop M, Randsdorp MS, Glerum S, Koes BW. Effectiveness of interventions of specific complaints of the arm, neck, and/or shoulder: 3 musculoskeletal disorders of the hand. An update. Arch Phys Med Rehabil. 2010 Feb;91(2):298–314. doi: 10.1016/j.apmr.2009.09.023. [DOI] [PubMed] [Google Scholar]