Abstract
Short-term breastfeeding and early exposure to complex dietary proteins, such as cow milk proteins and cereals, or to fruit, berries, and roots have been implicated as risk factors for β cell autoimmunity, clinical type 1 diabetes, or both. The Trial to Reduce Insulin-dependent diabetes mellitus in the Genetically at Risk (TRIGR) is an international, randomized, double-blind, controlled intervention trial designed to answer the question of whether weaning to an extensively hydrolyzed formula in infancy will decrease the risk of type 1 diabetes later in childhood. In our pilot study, weaning to a highly hydrolyzed formula decreased by ≈50% the cumulative incidence of one or more diabetes-associated autoantibodies by a mean age of 4.7 y. This finding was confirmed in a recent follow-up analysis to 10 y of age. Currently, the full-scale TRIGR takes place in 77 centers in 15 countries. The TRIGR initially recruited 5606 newborn infants with a family member affected by type 1 diabetes and enrolled 2159 eligible subjects who carried a risk-conferring HLA genotype. All recruited mothers were encouraged to breastfeed. The intervention lasted for 6–8 mo with a minimum study formula exposure time of 2 mo, and hydrolyzed casein and standard cow milk–based weaning formulas were compared. Eighty percent of the participants were exposed to the study formula. The overall retention rate over the first 5 y was 87%, and protocol compliance was 94%. The randomization code will be opened when the last recruited child turns 10 y of age (ie, in 2017).
INTRODUCTION
Type 1 diabetes is characterized by the selective loss of insulin-producing β cells in the pancreatic islets in genetically susceptible individuals. The clinical disease presentation is preceded by an asymptomatic period of highly variable duration (1). During that period diabetes-associated autoantibodies appear in the peripheral circulation as markers of emerging β cell autoimmunity. Evidence suggests that β cell autoimmunity may be induced early in life (2, 3). In parallel, recent studies have shown that the incidence of type 1 diabetes is increasing even faster than before among children in developed countries, among those <5 y of age in particular (4, 5). This scenario implies that any measure aimed at primary prevention of type 1 diabetes (ie, prevention of the initiation of the diabetic disease process) has to start in infancy. Early feeding may modify the risk of type 1 diabetes later in life. Short-term breastfeeding and early exposure to complex dietary proteins, such as cow milk proteins and cereals, or to fruit, berries, and vegetable roots have been implicated as risk factors for advanced β cell autoimmunity or clinical type 1 diabetes (6, 7). Early nutritional intervention could offer a safe, preventive modality for type 1 diabetes without the risks of aggressive immune interventions and has, in fact, been successful in relevant animal models of autoimmune diabetes, although the data are not uniform (8–11).
TRIGR stands for Trial to Reduce Insulin-dependent diabetes mellitus in the Genetically at Risk. It is an international, randomized, double-blind, controlled intervention trial designed to answer the question of whether weaning to an extensively hydrolyzed formula in infancy will decrease the risk of type 1 diabetes later in childhood. This review focuses on the rationale, design, accomplishments, and challenges of the trial, and possible mechanisms to mediate the putative protective effect. In addition, we present preliminary outcome data from the Finnish TRIGR pilot.
EARLY FEEDING AS A RISK FACTOR FOR TYPE 1 DIABETES
We have recently reviewed the role of factors related to infant nutrition in the development of β cell autoimmunity and type 1 diabetes, and the potential mechanistic pathways involved (12). Early nutrition clearly represents one of the first environmental determinants to which an infant is exposed. Given that the first signs of β cell autoimmunity may emerge during the first year of life in subjects who later progress to overt type 1 diabetes, it is likely that in most cases the disease process is initiated early in life. So far, no specific dietary factor or nutrient in infancy has been unequivocally shown to be involved in the development of type 1 diabetes. Evidence suggests, however, that dietary components may be critical factors that predispose to or protect against type 1 diabetes. In addition to short breastfeeding and early exposure to complex foreign proteins or fruit, berries, and root vegetables, lack of supplementation with vitamin D, heavy birth weight, and rapid weight gain in infancy have been implicated as risk candidates.
More research is definitely needed to confirm the contribution of early dietary factors to the development of β cell autoimmunity and clinical type 1 diabetes. The mechanistic pathways have to be defined as well. It is important to identify early dietary elements involved in the disease process that results in clinical type 1 diabetes, because the recognition of such determinants may provide measures for safe and effective primary prevention of type 1 diabetes aimed at inhibition of the initiation of β cell autoimmunity.
RATIONALE FOR THE TRIGR
A group of international investigators reached a consensus in the late 1990s that there is sufficient evidence that suggests a deleterious effect of early weaning to complex diets for the design of a primary prevention trial in children who carry genetic susceptibility to type 1 diabetes. It is important to note that the TRIGR does not, in fact, test the cow milk risk hypothesis, but instead analyses the effect of an extensively hydrolyzed weaning diet. Epidemiologic studies in this area have reached conflicting conclusions, likely explained by insufficient power and inability to address confounding factors such as the variations in feeding practices and the varied prevalence of hydrolyzed formula use and other foreign protein additives. Observational studies require wide differences, and the brevity of exclusive breastfeeding in most developed countries limits the power of such studies. Poor associations can be expected in studies of a ubiquitous agent such as cow milk, where exposure is nearly uniform. For example, the causal link between wheat and celiac disease was only uncovered through unplanned intervention (13): the wheat-deficient World War II diet in The Netherlands and its postwar improvement identified a culprit autoimmune disease–causing agent (ie, dietary gluten). This substantiates the critical importance of controlled intervention trials with sufficient power to arrive at conclusive outcomes.
The principal hypothesis in the TRIGR is simple and has proved testable: weaning to an extensively hydrolyzed formula will decrease the likelihood of type 1 diabetes in genetically susceptible children. If the hypothesis is proven correct, primary prevention of a considerable number of affected cases, with a decrease in the associated morbidity, mortality, and health care costs, would for the first time become a realistic goal. An additional benefit of the study is the provision of a platform, as well as a large data and sample repository for mechanistic studies that will shed new light on the progression of diabetic autoimmunity from its early beginnings, and for collaborations with other trials and studies in the field. If the intervention proves ineffective, this would obviate the need for more expensive association studies and remove the anxieties that surround weaning and infant feeding in families with type 1 diabetes, which would avoid unnecessary use of expensive hydrolysates. This would uncover a major, unprecedented difference from the rodent models, where casein hydrolysate has a uniformly preventive effect. Such a difference between rodent and human diabetes would affect the way we transfer insight from mouse to man.
The TRIGR effort constitutes the first-ever primary prevention trial for type 1 diabetes. In contrast to secondary prevention strategies, which attempt to arrest the progression of established islet autoimmunity and must identify prediabetes through screening, the innocuous TRIGR strategy could be applied to the general population with increased genetic risk, from which 83–98% of new cases with type 1 diabetes are derived (14).
EXPERIENCES FROM THE TRIGR PILOT
One of the few intervention trials of infant nutrition performed to date is the TRIGR pilot (15, 16). In this pilot, 230 Finnish infants at increased risk of type 1 diabetes were randomly assigned at weaning to either an extensively hydrolyzed formula or a conventional cow milk–based formula before 8 mo of age. The increased diabetes risk was based on a positive history of type 1 diabetes in a first-degree relative and, in addition, the participant had to carry an HLA genotype that conferred enhanced disease risk (14). During the intervention period the families were asked not to give any food products that contained cow milk or bovine serum albumin to their infants. The intervention resulted in a postponement of the introduction of intact cow milk proteins by several months in the active intervention group. After follow-up to a mean age of 4.7 y, an interim analysis showed that the nutritional intervention in infancy resulted in a decrease in most signs of β cell autoimmunity in the range of 50–60%. After adjustment for the observed difference in the exposure time to the study formula there was a significant decrease in the cumulative incidence of both islet cell antibodies and positivity for at least one of the 4 autoantibody reactivities analyzed (15).
A recent follow-up analysis up to 10 y of age showed that this early nutritional intervention significantly decreased the appearance of one or more autoantibodies. The hazard ratio decreased further after adjustment for the duration of study formula exposure. Sixteen out of 230 participants (7%), 7 (6%) in the casein hydrolysate group and 9 (8%) in the control group, had progressed to overt type 1 diabetes. In an intention-to-treat analysis, the risk of type 1 diabetes was not significantly associated with the feeding intervention (casein hydrolysate compared with control; hazard ratio: 0.80; 95% CI: 0.30, 2.14). However, 3 children who progressed to overt type 1 diabetes dropped out before 3 mo of age, 2 within 2–4 d after birth and the third just before the 3-mo visit. All 3 children had been randomly assigned to the casein hydrolysate group, but none had received any study formula. Accordingly, the number of progressors per protocol (“treatment received”) was 4 (4%) in the casein hydrolysate group and 9 (8%) in the control group. The per protocol hazard ratio for type 1 diabetes was 0.40 (95% CI: 0.11, 1.51). The results from the TRIGR pilot suggest that it may be possible to manipulate spontaneous β cell autoimmunity by nutritional intervention during infancy. Accordingly, early nutritional intervention as applied in the TRIGR provides an attractive preventive strategy, because it can be implemented relatively easily as a public health measure.
DESIGN OF THE TRIGR
The full-scale TRIGR asks whether it is possible to decrease 1) the frequency of disease-associated autoantibodies and/or clinical diabetes by 6 y of age and 2) the cumulative incidence of diabetes by 10 y of age by weaning to a highly hydrolyzed formula over the first 6–8 mo of life. The study design has been described in detail previously (17, 18). In brief, the TRIGR study population comprises newborn infants who have first-degree relatives affected by type 1 diabetes (ie, a mother, father, or sibling) and who meet the HLA inclusion but none of the exclusion criteria. Blood for HLA genotyping was collected from cord blood and sent to the continental central laboratory within 8 d of birth, and results were sent to the Data Management Unit within 2 wk of age for assessment and confirmation of eligibility, which were then forwarded electronically to the centers. This international, double-blinded, prospective, placebo-controlled intervention trial comprises 77 centers in 15 countries on 3 continents. The enrollment began on 1 May 2002, and ended on 6 February 2007.
The sample size estimate was based on the following assumptions: 1) a confidence level of 95%, 2) a statistical power of 80%, 3) a decrease of 40% in the hazard rate of type 1 diabetes in the intervention group, 4) a dropout rate of 20%, and 5) a frequency of 10% of exclusive breastfeeding up to 6 mo of age. The spontaneous cumulative incidence of type 1 diabetes by 10 y of age was estimated to be ≥7.6% among children who fulfilled the inclusion criteria of the trial (19). These assumptions resulted in a recruitment target of 2032 eligible infants. As a consequence of successful recruitment the enrollment target was exceeded by 6% to 2159 randomly assigned and eligible subjects.
The children were randomly assigned to the 2 treatment groups in a 1:1 ratio with the use of randomly permuted blocks. Random assignment was balanced within each center/country that participated. Web-based randomization procedures proceeded efficiently. The infants were assigned one of the 4 color-coded, blinded formulas, 2 of which contained the hydrolyzed test formula, 2 the control formula. The randomization code is known only to the manufacturer and the principal investigator of the Data Management Unit, under supervision of the Data Safety and Monitoring Board. The code will be opened when the youngest participant turns 10 y.
HLA genotyping
Cord blood was obtained whenever possible and, if unobtainable, a heel stick blood sample was collected on filter paper and sent immediately to the Turku (Europe and Australia) or Pittsburgh (North America) laboratories for HLA genotyping. HLA genotyping for the selected DQB1 and DQA1 alleles was performed with the use of sequence-specific oligonucleotide hybridization, and quality control was maintained between the 2 laboratories. The following genotypes were regarded as eligible: 1) HLA-DQB1*02/ DQB1*0302; 2) HLA-DQB1*0302/x (x ≠ DQB1*02, DQB1*0301, or DQB1*0602); 3) HLA-DQA1*05-DQB1*02/y (y ≠ DQA1*0201-DQB1*02, DQB1*0301, DQB1*0602, or DQB1*0603); and 4) HLA-DQA1*03-DQB1*02/z (z ≠ DQA1*0201-DQB1*02, DQB1*0301, DQB1*0602, or DQB1*0603).
Intervention
Whenever supplementary milk feeding was needed during the intervention period, subjects received either the test formula based on extensively hydrolyzed casein (Nutramigen; Mead Johnson Nutrition, Evansville, IN) or a control formula created by the company for this study made with intact (80%) and hydrolyzed (20%) milk protein to mask the taste and smell differences between the 2 formulas. All recruited mothers were encouraged to breastfeed their infants.
Follow-up during and after intervention
Clinical assessment, interviews, and blood sampling were performed at the ages of 3, 6, 9, 12, 18, and 24 mo and continue annually until 10 y of age or until manifestation of type 1 diabetes. Clinical data at each visit (eg, weight, height, adverse events, infections, and so forth) are recorded and transmitted electronically to the Data Management Unit. Cow milk antibodies [immunoglobulin (Ig) G and IgA] (20) and α-casein antibodies (IgG and IgA) (21) were measured within 2 mo of sampling up to the 9-mo visit, to be used as efficacy and compliance markers of the intervention, whereas other laboratory tests are scheduled in batches. Diabetes-predictive autoantibodies (islet cell antibodies, insulin autoantibodies, and antibodies to the 65-kDa isoform of glutamic acid decarboxylase and the protein tyrosine phosphatase-related IA-2A protein) are analyzed from the autoantibody specimens obtained at each study center visit. A heparin blood sample is also obtained at each sampling time. These samples are sent fresh to the core laboratories in Helsinki and Toronto for isolation of mononuclear cells for mechanistic studies of T cell responses. Local measurements of random plasma glucose and glycosylated hemoglobin are performed at each visit from 12 mo onwards and are reported to the Data Management Unit. The specimen for plasma glucose is preferentially obtained 1–2 h postprandially. In the presence of hyperglycemia or elevated glycosylated hemoglobin, an oral-glucose-tolerance test (OGTT) is recommended to exclude or confirm the diagnosis of diabetes. An OGTT is performed in all nondiabetic subjects at 6 and 10 y of age. If the first OGTT is diabetic according to World Health Organization criteria, a second confirmatory test is required to verify the diagnosis.
WHY SHOULD AN EXTENSIVELY HYDROLYZED FORMULA PROTECT AGAINST beta CELL AUTOIMMUNITY AND TYPE 1 DIABETES?
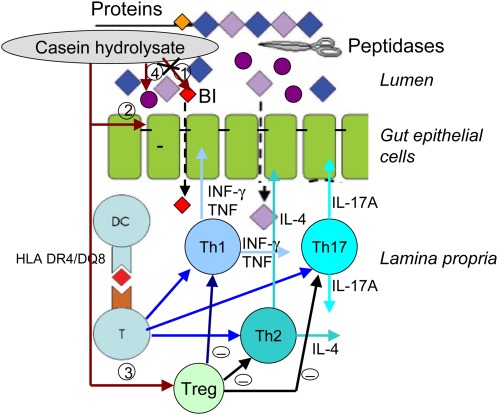
The mechanism or mechanisms through which a highly hydrolyzed formula may provide protection against β cell autoimmunity and type 1 diabetes are not delineated. One may speculate about potential mechanisms, such as 1) elimination of early exposure to intact bovine insulin, 2) decreased gut permeability, 3) induction of the maturation of regulatory T cells in the gut-associated lymphoid tissue, and/or 4) modification of the gut microflora (Figure 1).
FIGURE 1.
Possible mechanisms by which an extensively hydrolyzed formula may protect against β cell autoimmunity and type 1 diabetes in children at increased genetic disease risk. The highly hydrolyzed formula (1) eliminates the exposure to intact bovine insulin (BI) present in conventional cow milk–based formulas (2); may decrease intestinal permeability, thereby decreasing the load of foreign peptides and proteins on the gut-associated lymphoid tissue in lamina propria (3); may induce the maturation of regulatory T cells (Treg) in the gut-associated lymphoid tissue, the function of which suppresses other T cells and their cytokine production, resulting in decreased intestinal inflammation; and/or (4) may support “healthy” microbial (•) diversity in the gut. DC, dendritic cell; HLA, human leukocyte antigen; IL, interleukin; INF-γ, interferon γ; T, T cell; Th, T helper; TNF, tumor necrosis factor.
The casein-based formula used as the intervention modality in this study is highly hydrolyzed and does not contain intact proteins. Less than 0.3% of the peptides have a molecular weight >2000 Da. Accordingly, the formula is free of intact bovine insulin, which is present in cow milk (22). Vaarala et al (23) showed that infants who were fed a conventional cow milk–based formula before 3 mo of age developed an immune response to bovine insulin that differs from human insulin by 3 amino acids. Normally, these infants developed oral tolerance to bovine insulin over time, reflected by the decline in immune responses to insulin. Interestingly, those infants who presented with early signs of β cell autoimmunity lacked the capacity to mount oral tolerance to bovine insulin. In such individuals the immune response induced by bovine insulin might at some point be diverted to target self-insulin and insulin-producing β cells, and thereby contribute to the disease process that results in type 1 diabetes. Weaning to a highly hydrolyzed formula will postpone the exposure to intact bovine insulin and allow for maturation of the mechanisms that control oral tolerance.
Some evidence suggests that children who present with type 1 diabetes have increased gut permeability. Such children have been reported to have elevated concentrations of antibodies and higher levels of T cell responses to certain dietary antigens (20, 24–28). Recent observations based on the TRIGR pilot have shown that those children who later progressed to clinical type 1 diabetes already had elevated antibody concentrations to cow milk proteins in infancy (29). This may imply that children who present with type 1 diabetes have increased gut permeability early in life. On the other hand, elevated concentrations of such antibodies may reflect dysregulation of the gut-associated immune system, which is the most extensive immune organ in the body.
In addition to increased gut permeability, subclinical intestinal inflammation has been reported in children with type 1 diabetes. Intestinal biopsies from such children without concomitant celiac disease have shown signs of intestinal immune activation (30, 31). Special interest has been focused on regulatory T cells, which are perceived to be crucially involved in the regulation of autoimmunity. Intestinal biopsy studies showed a lack of intestinal activation of regulatory T cells in patients with type 1 diabetes, which might explain the subclinical intestinal immune activation and altered responses to dietary antigens seen in subjects with type 1 diabetes (32). No data are available on the effect of highly hydrolyzed formulas on the maturation of regulatory T cells in infants.
The microbial colonization of the gut experiences 2 critical phases in the infant period, the first soon after birth and the other in the weaning period. A Dutch study showed that the most important determinants of the gut microbiota composition in infants were the mode of delivery, type of infant feeding, gestational age, infant hospitalization, and antimicrobial use (33). A comparison of the intestinal microflora of breastfed and formula-fed infants showed that bifidobacteria become dominant in all breastfed infants after the initial colonization, whereas most formula-fed infants had similar amounts of Bacteroides and bifidobacteria (34). Fecal samples from breastfed infants comprised lactobacilli and streptococci, whereas samples from formula-fed infants often contained staphylococci, Escherichia coli, and clostridia. These data show that infant feeding has an indisputable effect on the intestinal microbiota. A very recent study indicates that the level of bacterial diversity diminishes over time in children en route to type 1 diabetes relative to that of matched nonautoimmune individuals (35). A striking finding of that analysis was the decline in Firmicutes and increase in Bacteroidetes seen in the gut microbiome in the prediabetic period in those who progressed to overt diabetes; the pattern was in conspicuous contrast to the trend observed in healthy children in whom Firmicutes increased as the Bacteroidetes declined. Another recent study confirmed that Nutramigen prevents autoimmune diabetes in the disease-prone biobreeding rat and has beneficial effects on intestinal barrier integrity, regulatory cytokine production, and the microflora composition in the gut (36).
It is intriguing that in a German intervention trial the same extensively hydrolyzed formula as the one used in the TRIGR decreased the risk of another immune-mediated disease (ie, allergic dermatitis) during the first year of life in infants with a positive parental history of atopy (37). A significant protective effect could still be observed at 6 y of age, although the relative risk had increased from 0.42 at 1 y of age to 0.80 (38). No protective effect could be observed in terms of asthma and allergic rhinitis. Given that both autoimmune diseases, such as type 1 diabetes, and atopic diseases, such as allergic dermatitis, are considered to reflect dysfunctional immune regulation, one is tempted to suggest that the protective effect conferred by the extensively hydrolyzed formula may be related to the function of regulatory T cells. However, this is not the only possibility. Feeding with the extensively hydrolyzed formula led to a transient lower weight gain during the first year of life in the German trial (39). Increased weight gain in infancy has been reported repeatedly to be a risk factor for type 1 diabetes later in childhood (12) and, accordingly, a decreased weight gain in infancy could be protective. However, we could not find any difference in linear growth and weight gain over the first 5 y of life between those randomly assigned to the extensively hydrolyzed formula and those assigned to the conventional cow milk–based formula in the TRIGR pilot (15).
ACCOMPLISHMENTS OF THE TRIGR
Enrollment in the study cohort was completed in early 2007. All the study planning parameters have been met or bettered: the rate of exclusive breastfeeding is less than expected and subject retention is better than expected. The additional 6% enrollment provides a cushion against any greater than expected lost-to-follow-up rate. Major study accomplishments are shown in Table 1.
TABLE 1.
Major accomplishments and milestones in the full-scale Trial to Reduce Insulin-dependent diabetes mellitus in the Genetically at Risk (TRIGR)
| Milestone | Current level (31 May 2010) |
| Design, translation, and distribution of the Manual of Operations, forms and questionnaires; Web-based in 12 languages | Achieved in 6 mo |
| Identification and consent of 4936 pregnant mothers with at least one family member with type 1 diabetes | 5156 registered mothers (105% of the target) |
| 2032 (45% of screened) HLA eligible infants enter intervention study | 2160 (106% of the target) eligible infants entered the trial, which allowed for a 45% eligibility rate |
| Forms and visit compliance >80% | 97.6% |
| Blood sample compliance >70% | 92.6% |
| Lost to follow-up and not participating <20% | 13.2% |
| Exclusive breastfeeding >6 mo 10% | 3.6% |
| Exposed to study formula | ≈80% |
| Blood sample repository (n = 200,000/10 y) | ≈145,000 collected to date (94% of scheduled samples) |
All adverse events are reported electronically with the use of on-line event-monitoring systems developed and supported by the Data Management Unit. Serious events are also reported to the local institutional review boards and the TRIGR International Coordinating Center, and the Data Safety and Monitoring Board Growth data are monitored routinely by the Data Safety Monitoring Board. No differences in growth variables (heights, weights, and body mass indexes) by treatment arm have been observed to date. All adverse events, which include those categorized as serious, are summarized by the TRIGR Data Management Unit and reviewed at each Data Safety and Monitoring Board meeting. To date there have been no concerns regarding safety issues and the study intervention.
Compliance with study visits, completion of data forms, and collection and submission of serum samples is also monitored closely. Subject-lost-to-follow-up and protocol-noncompliance rates are currently ≈13.2% (an estimate of 20% was used in the TRIGR planning parameters). The study planned on a 10% rate of exclusive breastfeeding by 6 mo of age and the observed cumulative rate was 3.6%. Compliance with forms submission (and, by implication, study visits) was, by the end of May 2010, 97.6%, adjusted for subjects lost to follow-up. Similarly, compliance with the collection and submission of required study samples is 92.6%.
Another important measure of protocol compliance is the extent to which study families comply with the study intervention and avoid intake of cow milk–containing foods during the intervention period. Self-reported dietary compliance rates have been very high. In addition, the study protocol routinely screens for cow milk antibodies and this has shown a high degree of dietary compliance during the intervention period, which confirms the self-reported data.
CHALLENGES OF THE TRIGR
The primary challenge of the TRIGR study in its present phase is how to keep the families in the study until the participant reaches the age of 10 y. The Study Group has recently decided to extend the follow-up of all participants until the youngest child turns 10 y of age. At that time the oldest participants will be 14 y old, and the mean age of the participants will be ≈12 y. This further increases the retention challenge. The arguments for the extended follow-up are based on the considerations that the extension increases the number of follow-up years by ≈4000 y (an increase of 20%) and provides information on whether the expected protective effect of the intervention extends into puberty.
The dropouts in the TRIGR are classified into 2 categories. The lost-to-follow-up subjects come from families who have not attended 2 sequential follow-up visits and who cannot be located and contacted. In addition, this category includes those families who have refused any further contacts from the TRIGR. The number of subjects lost to follow-up amounted to 35 (1.6%) at the end of May 2010. The children who did not participate represent families who have failed to attend 2 sequential study center visits but with whom the study center remains in contact. The number of such families was 249 (11.5%) by 31 May 2010. Over the last year each study center has been asked to contact the families that did not participate and invite them to rejoin and come to the next follow-up visit. This retrieval activity has resulted in an increasing number of families who have rejoined the study.
One issue that has been discussed by the Study Group is the scenario that will arise if an autoantibody-positive TRIGR participant is invited to a trial aimed at secondary prevention of type 1 diabetes. The results of the autoantibody screening are released to the families for the first time after the 6-y follow-up visit, and subsequently the results are provided after each annual visit. Accordingly, children with signs of β-cell autoimmunity are identified. The TRIGR Study Group has decided that the autoantibody-positive TRIGR participants may take part in secondary prevention trials, provided they fulfill the inclusion criteria. This decision is based on ethical considerations, because from a scientific point of view an effective secondary prevention should decrease the number of endpoints in the TRIGR and thereby introduce a bias. Most secondary prevention trials have so far excluded subjects who have or are involved in other intervention trials. If an effective secondary prevention strategy for type 1 diabetes emerges before the end of the TRIGR, the participants and their families will be informed and encouraged to engage in such a treatment.
FUTURE SCENARIOS
As mentioned earlier, the TRIGR study has 2 endpoints. The first endpoint (ie, positivity of ≥2 diabetes-associated autoantibodies and/or clinical diabetes by 6 y of age) will be reached in early 2013, when the youngest participant turns 6. The second and final endpoint (ie, clinical diabetes by 10 y of age) will be reached in early 2017. The issue has been raised as to whether the follow-up of the trial participants should continue if there is a highly significant difference or no difference whatsoever in the 6-y endpoint. The Study Group feels strongly that the follow-up should continue in any case up to early 2017, when the youngest participant turns 10 y, to assess the final outcome of the trial. At this point one cannot exclude the possibility that the intervention may modify the natural history of β cell autoimmunity in any direction without necessarily affecting progression to clinical disease.
There are 2 possible scenarios in terms of the outcome of the TRIGR. If the intervention significantly decreases the rate of type 1 diabetes by 10 y of age, this would imply that infants at increased risk of type 1 diabetes should be weaned to a highly hydrolyzed formula. If the intervention does not have an effect, this would lead to a recommendation that weaning to a highly hydrolyzed formula does not decrease the risk of type 1 diabetes and, accordingly, such formulas do not provide any benefits to infants who carry increased genetic susceptibility to the disease. The TRIGR study is powered to provide a definite answer to the controversial question of whether weaning to a hydrolyzed formula protects against initiation and progression of type 1 diabetes. This effort is the first-ever primary prevention trial for type 1 diabetes. If the main hypothesis of the study is proven correct, primary prevention of at least some cases of type 1 diabetes will become a realistic goal.
Acknowledgments
We thank the Finnish TRIGR Study Group for its contribution to the TRIGR pilot; Mead Johnson Nutrition for provision of the study formulas free of charge and James W Hansen of the company for his collaboration, wisdom, and support; Gilman Grave, program official for the TRIGR at the National Institute of Child Health and Development, for stimulating encouragement and collaboration over the years; and the chair of the Data Safety and Monitoring Board, Thomas Mandrup-Poulsen, and the other board members for their critical evaluation and encouraging attitude toward the project. We also thank the TRIGR staff at all the clinical sites, the Data Management Unit, laboratories, and administrative centers for their enthusiastic and excellent performance, and the TRIGR families for their willingness to participate.
The authors’ responsibilities were as follows—MK: principal investigator (PI) of the trial after being the deputy PI 2002–2008 and writing of the first version of the manuscript; SMV: responsible for the nutritional intervention; DB: PI in the United States; JD: PI in Canada; JPK: PI for the Data Management Unit; and HKÅ: deputy PI after being the PI for the entire trial until 2008. All authors were involved in the planning of TRIGR, played an important role in the implementation of the trial, and contributed to the final version of the manuscript. The authors had no conflicts of interest.
REFERENCES
- 1.Knip M. Natural course of preclinical type 1 diabetes. Horm Res 2002;57(suppl 1):6–11 [DOI] [PubMed] [Google Scholar]
- 2.Ziegler A-G, Hummel M, Schenker M, Bonifacio E. Autoantibody appearance and risk for development of childhood diabetes in offspring of parents with type 1 diabetes: the 2-year analysis of the German BABYDIAB Study. Diabetes 1999;48:460–8 [DOI] [PubMed] [Google Scholar]
- 3.Kimpimäki T, Kupila A, Hämäläinen A-M, et al. The first signs of β-cell autoimmunity appear in infancy in genetically susceptible children from the general population: The Finnish Type 1 Diabetes Prediction and Prevention Study. J Clin Endocrinol Metab 2001;86:4782–8 [DOI] [PubMed] [Google Scholar]
- 4.Harjutsalo V, Sjöberg L, Tuomilehto J. Time trends in the incidence of type 1 diabetes in Finnish children: a cohort study. Lancet 2008;371:1777–82 [DOI] [PubMed] [Google Scholar]
- 5.Patterson CC, Dahlquist CG, Gyürus E, Green A, Soltesz G. the EURODIAB Study Group. Incidence trends for childhood type 1 diabetes in Europe during 1989-2003 and predicted new cases 2005-20: a multicentre prospective registration study. Lancet 2009;373:2027–33 [DOI] [PubMed] [Google Scholar]
- 6.Virtanen SM, Knip M. Nutritional risk predictors of β cell autoimmunity and type 1 diabetes at a young age. Am J Clin Nutr 2003;78:1053–67 [DOI] [PubMed] [Google Scholar]
- 7.Virtanen SM, Kenward MG, Erkkola M, et al. Age at introduction of new foods and advanced beta-cell autoimmunity in young children with HLA-conferred susceptibility to type 1 diabetes. Diabetologia 2006;49:1512–21 [DOI] [PubMed] [Google Scholar]
- 8.Karges W, Hammond-McKibben D, Cheung RK, et al. Immunological aspects of nutritional diabetes prevention in NOD mice: a pilot study for the cow's milk-based IDDM prevention trial. Diabetes 1997;46:557–64 [DOI] [PubMed] [Google Scholar]
- 9.Malkani S, Nompleggi D, Hansen JW, Greiner DL, Mordes JP, Rossini AA. Dietary cow's milk protein does not alter the frequency of diabetes in the BB rat. Diabetes 1997;46:1133–40 [DOI] [PubMed] [Google Scholar]
- 10.Paxson JA, Weber JG, Kulzycki A., Jr Cow's milk-free diet does not prevent diabetes in NOD mice. Diabetes 1997;46:1711–7 [DOI] [PubMed] [Google Scholar]
- 11.Simonson W, Ramanathan S, Bieg S, Poussier P, Lernmark A. Protein-free diets do not protect high-incidence diabetes-prone biobreeding rats from diabetes. Metabolism 2002;51:569–74 [DOI] [PubMed] [Google Scholar]
- 12.Knip M, Virtanen SM, Åkerblom HK. Infant feeding and risk of type 1 diabetes. Am J Clin Nutr 2010;91:1506S–13S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Streng J. Over de beoordeling van de voedingstoestand in de praktijk. [On the judgment of the state of nutrition in practice.] Maandschrift v Kindergen 1946;14:67–78 (in Dutch, summary in English) [Google Scholar]
- 14.The EURODIAB ACE Study Group and The EURODIAB ACE Substudy 2 Study Group Familial risk of type 1 diabetes in European children. Diabetologia 1998;41:1151–6 [DOI] [PubMed] [Google Scholar]
- 15.Åkerblom HK, Virtanen SM, Ilonen J, et al. Dietary manipulation of beta-cell autoimmunity in infants at increased risk for type 1 diabetes. Diabetologia 2005;48:829–37 [DOI] [PubMed] [Google Scholar]
- 16.Åkerblom HK, Virtanen SM, Ilonen J, et al. Weaning to a highly hydrolyzed formula in infancy decreases the cumulative incidence of beta-cell autoimmunity in young children with increased genetic risk for type 1 diabetes. Pediatr Diabetes 2006;7(suppl 5):58–9 [Google Scholar]
- 17.The TRIGR Study Group Study design of the Trial to Reduce IDDM in the Genetically at Risk (TRIGR). Pediatr Diabetes 2007;8:117–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Åkerblom HK, Knip M, Becker D, et al. The TRIGR trial: testing the potential link between weaning diet and type 1 diabetes. Immun Endoc Metab Agents Med Chem 2007;7:251–63 [Google Scholar]
- 19.Kimpimäki T, Kulmala P, Savola K, et al. Disease-associated autoantibodies as surrogate markers of type 1 diabetes in young children at increased genetic risk. J Clin Endocrinol Metab 2000;85:1126–30 [DOI] [PubMed] [Google Scholar]
- 20.Savilahti E, Akerblom HK, Tainio VM, Koskimies S. Children with newly diagnosed insulin dependent diabetes mellitus have increased levels of cow's milk antibodies. Diabetes Res 1988;7:137–40 [PubMed] [Google Scholar]
- 21.Vaarala O, Saukkonen T, Savilahti E, Klemola T, Akerblom HK. Development of immune response to cow's milk proteins in infants receiving cow's milk or hydrolyzed formula. J Allergy Clin Immunol 1995;96:917–23 [DOI] [PubMed] [Google Scholar]
- 22.Aranda P, Sanchez L, Perez MD, Ena JM, Calvo M. Insulin in bovine colostrum and milk: evolution throughout lactation and binding to caseins. J Dairy Sci 1991;74:4320–5 [DOI] [PubMed] [Google Scholar]
- 23.Vaarala O, Knip M, Paronen J, et al. Cow milk formula feeding induces primary immunization to insulin in infants at genetic risk for type 1 diabetes. Diabetes 1999;48:1389–94 [DOI] [PubMed] [Google Scholar]
- 24.Dahlquist G, Savilahti E, Landin-Olsson M. An increased level of antibodies to beta-lactoglobulin is a risk determinant for early-onset type 1 (insulin-dependent) diabetes mellitus independent of islet cell antibodies and early introduction of cow's milk. Diabetologia 1992;35:980–4 [DOI] [PubMed] [Google Scholar]
- 25.Savilahti E, Saukkonen TT, Virtala ET, Tuomilehto J, Åkerblom HK. the Childhood Diabetes in Finland (DiMe) Study Group. Increased levels of cow's milk and beta-lactoglobulin antibodies in young children with newly diagnosed IDDM. Diabetes Care 1993;16:984–9 [DOI] [PubMed] [Google Scholar]
- 26.Saukkonen T, Savilahti E, Vaarala O, et al. Children with newly diagnosed insulin-dependent diabetes mellitus have increased levels of antibodies to bovine serum albumin but not to ovalbumin. Diabetes Care 1994;17:970–6 [DOI] [PubMed] [Google Scholar]
- 27.Vaarala O, Klemetti P, Savilahti E, Reijonen H, Ilonen J, Åkerblom HK. Cellular immune response to cow's milk beta-lactoglobulin in patients with newly diagnosed IDDM. Diabetes 1996;45:178–82 [DOI] [PubMed] [Google Scholar]
- 28.Klemetti P, Savilahti E, Ilonen J, Åkerblom HK, Vaarala O. T-cell reactivity to wheat gluten in patients with insulin-dependent diabetes mellitus. Scand J Immunol 1998;47:48–53 [DOI] [PubMed] [Google Scholar]
- 29.Luopajärvi K, Savilahti E, Virtanen SM, et al. Enhanced levels of cow's milk antibodies in infancy in children who develop type 1 diabetes later in childhood. Pediatr Diabetes 2008;9:434–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Westerholm-Ormio M, Vaarala O, Pihkala P, Ilonen J, Savilahti E. Immunological activity in the small intestinal mucosa of pediatric patients with type 1 diabetes. Diabetes 2003;52:2287–95 [DOI] [PubMed] [Google Scholar]
- 31.Auricchio R, Paparo F, Maglio M, et al. In-vitro-deranged intestinal immune response to gliadin in type 1 diabetes. Diabetes 2004;53:1680–3 [DOI] [PubMed] [Google Scholar]
- 32.Vaarala O, Atkinson M, Neu J. The “perfect storm” for type 1 diabetes: the complex interplay between intestinal microbiota, gut permeability, and mucosal immunity. Diabetes 2008;57:2555–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Penders J, Thijs C, Voink C, et al. Factors influencing the composition of the intestinal microbiota in early infancy. Pediatrics 2006;118:511–21 [DOI] [PubMed] [Google Scholar]
- 34.Harmsen HJ, Wildeboer-Veloo AC, Raangs GC, et al. Analysis of intestinal flora development in breast-fed and formula-fed infants by using molecular identification and detection methods. J Pediatr Gastroenterol Nutr 2000;30:61–7 [DOI] [PubMed] [Google Scholar]
- 35.Giongo A, Mukherjee N, Gano KA, et al. Toward defining the autoimmune microbiome for type 1 diabetes. ISME J 2011;5:82–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Visser JT, Bos NA, van Tool EA, Harthoorn LC, Rozing J. Differential preventive effect of casein hydrolysates in autoimmune diabetes development involves intestinal barrier integrity and gut flora composition. Eur J Immunol 2009;39(suppl1):S674 (abstr) [Google Scholar]
- 37.von Berg A, Koletzko S, Grübl A, et al. The effect of hydrolyzed cow's milk formula for allergy prevention in the first year of life: the German Infant Nutritional Intervention Study, a randomized double-blind trial. J Allergy Clin Immunol 2003;111:533–40 [DOI] [PubMed] [Google Scholar]
- 38.von Berg A, Filipiak-Pittroff B, Krämer U, et al. Preventive effect of hydrolyzed infant formulas persists until age 6 years: long-term results from the German Infant Nutritional Intervention Study (GINI). J Allergy Clin Immunol 2008;121:1442–7 [DOI] [PubMed] [Google Scholar]
- 39.Rzehak P, Sausenthaler S, Koletzko S. Short- and long-term effects of feeding hydrolyzed protein infant formulas on growth at < or = 6 y of age: results from the German Infant Nutritional Intervention Study. Am J Clin Nutr 2009;89:1846–56 [DOI] [PubMed] [Google Scholar]