Abstract
Background
Several activities of the transmembrane form of TNF (memTNF) in immune responses to intracellular bacterial infection have been shown to be different from those exerted by soluble TNF. Evidence is based largely on studies in transgenic mice expressing memTNF, but precise cellular mechanisms are not well defined and the importance of TNF receptor regulation is unknown. In addition, memTNF activities are defined for a particular modification of the extracellular domain of TNF but a direct comparison of different mutant memTNF molecules has not been done in vivo.
Methodology
To understand the activities of memTNF we compared two commonly used mouse strains lacking soluble TNF but possessing functional and normally regulated membrane-bound TNF knockin (memTNF KI) for their capacity to generate cell-mediated immune responses and resistance to M. bovis BCG infection, and to regulate TNF receptors.
Principal Findings
M. bovis BCG infection resulted in similar bacterial loads in one strain of memTNF KI (memTNFΔ1–9,K11E) and in wild-type mice, in contrast, the other strain of memTNF KI mice (memTNFΔ1–12) showed higher sensitivity to infection with high mortality (75%), greater bacterial load and massive lung pathology. The pattern of cytokines/chemokines, inflammatory cells, pulmonary NF-κB phosphorylation, antigen-dependent IFN-γ response, and splenic iNOS was impaired in M. bovis BCG-infected memTNFΔ1–12 KI mice. Macrophages expressing TNFR2 were reduced but soluble TNFRs were higher in memTNFΔ1–12 KI mice during the infection. In vitro, M. bovis BCG-induced NF-κB activation and cytokines were also decreased in memTNFΔ1–12 KI bone marrow-derived macrophages.
Conclusion
Our data show that two memTNF molecules exerted very different activities upon M. bovis BCG infection resulting in protection or not to bacterial infection. These results suggest a regulatory mechanism of memTNF and TNF receptors being critical in the outcome of the infection and highlight the role of cell-bound and soluble TNFR2 in memTNF-mediated anti-microbial mechanisms.
Introduction
Tumor necrosis factor (TNF) is a major pro-inflammatory cytokine playing an important role in the pathogenesis of chronic inflammatory diseases such as rheumatoid arthritis, Crohn's disease or psoriatic arthritis [1]. Most activities exerted by TNF were originally attributed to the soluble form of TNF (solTNF), a 17-kDa soluble TNF molecule generated by cleavage of its 26-kDa precursor, transmembrane or membrane TNF (memTNF). The generation of uncleavable memTNF by mutations in the region cleaved by the TACE (TNF-α converting enzyme) and subsequent studies on cells, transgenic mice and later in memTNF knockin (KI) mice without soluble TNF and in human cells have shown the importance of activities mediated by the transmembrane form of TNF [2], [3]. However, it is still unclear how memTNF-mediated effects are influenced by several factors including the nature of mutations generated on the memTNF molecule, and regulatory mechanisms involving TNFR and their soluble forms which have not been explored in vivo. As an example of the reported complexity, studies on the same memTNF expressed in mice either as a transgene or as a knockin have resulted in opposite effects, as a memTNF (deletion 1–12, memTNFΔ1–12) was previously shown to mediate inflammatory reactions in a transgenic mouse model [4], while memTNFΔ1–12 KI mice did not show liver inflammation after LPS/D-GalN challenge [5]. We have recently reported that another variant of memTNF (deletion 1–9 and substitution Lys to Glu in position 11, memTNFΔ1–9,K11E) in KI mice [6] was not pathogenic for liver inflammation but only soluble TNF was causing hepatitis in LPS/BCG and LPS/D-GalN-induced liver damage [7].
Host protection mechanisms mediated by transmembrane TNF against bacterial and parasitic infections have been studied mainly using memTNFΔ1–9,K11E KI mice. It was reported that memTNFΔ1–9,K11E KI mice were protected from low-dose Listeria monocytogenes infection but only partially or not protected from high dose infection [8], [9]. A study of L. monocytogenes infection in memTNFΔ1–12 KI mice showed partial survival of these mice to low bacterial dose [5]. The memTNFΔ1–9,K11E form was shown to be sufficient to develop partial innate immunity to Francisella tularensis live vaccine strain [10]. An important role of memTNFΔ1–9,K11E was observed in the resolution of the inflammatory lesion induced by Leishmania major infection [11]. Infection with M. tuberculosis of memTNFΔ1–9,K11E KI mice showed protection against acute but not to chronic infection [12], [13]. These studies confirmed our previous results on transgenic mice expressing a different mutant memTNF (Δ-12 to −10, Δ-2 to +1, K11E) expressed as a transgene in mice deficient in both TNF and LTα (transgenic memTNF in TNF/LTα−/−) [14], [15], [16]. Only one study has been reported for M. tuberculosis infection using memTNFΔ1–12 KI mice showing protection to acute but not to chronic infection, and the infection dosage were lower than those used in the studies of memTNFΔ1–9,K11E KI mice [17] (Table 1).
Table 1. M. tuberculosis and M. bovis BCG infection studies performed in memTNF KI mice.
| MemTNF KI mouse strain | Mycobacteria | Dose and route of inoculation | Survival | References |
| MemTNFΔ1–9,K11E | M. tuberculosis | 70–100 CFU by aerosol | Succumbed:130–200 days | [13] |
| MemTNFΔ1–9,K11E | M. tuberculosis | 100 CFU intranasally | Succumbed:110–200 days | [12] |
| MemTNFΔ1–9,K11E | BCG Pasteur | 106 CFU intranasally | 100% survival at 120 days | [18] |
| MemTNFΔ1–9,K11E | M. tuberculosis | 50–100 CFU by aerosol | Succumbed: 150–230 days | [18] |
| MemTNFΔ1–12 | BCG Pasteur | 2×106 intravenously | 50% survival at 90 days | [17] |
| MemTNFΔ1–12 | M. tuberculosis | 10–30 CFU by aerosol | Succumbed: 50–170 days | [17] |
| MemTNFΔ1–9,K11E | BCG Connaught | 10×106 intravenously | 93% survival at 100 days | Present study |
| MemTNFΔ1–9,K11E | BCG Pasteur | 10×106 intravenously | 100% survival at 100 days | Present study |
| MemTNFΔ1–12 | BCG Connaught | 10×106 intravenously | 30% survival at 100 days | Present study |
| MemTNFΔ1–12 | BCG Pasteur | 10×intravenously | 20% survival at 100 days | Present study |
Infection with M. bovis BCG in memTNF KI mice has shown differential susceptibilities of these mice. MemTNFΔ1–9,K11E KI mice intranasally infected showed total resistance to M. bovis BCG infection, whereas memTNFΔ1–12 KI mice intravenously (i.v.) infected were only 50% resistant [17], [18]. The reasons of differential susceptibility of the two memTNF KI mouse strains were not addressed in previous publications. To date, a rigorous comparison of immune responses elicited by intracellular bacterial infection in the two memTNF KI mice has not been performed and the importance of TNF receptors during a bacterial infection is unknown.
To gain insights into the role of memTNF and its interaction with TNF receptors in protection against intracellular bacterial infection, we have compared resistance and cell-mediated immunity to M. bovis BCG infection of memTNFΔ1–9,K11E KI and memTNFΔ1–12 KI mice, and studied the pattern of cytokine and TNF receptor expression, and NF-κB activation. We used a systemic M. bovis BCG infection that allows these studies in highly sensitive mice such as TNF−/− mice in which the pattern of inflammatory lesions have been well characterized. Considering that M. bovis BCG is the most widely distributed vaccination with live bacteria, deep investigation on the factors influencing protective immunity is still required.
Our results show important differences between the two memTNF KI mouse strains in both resistance and cell-mediated immune responses to M. bovis BCG infection. These differences reveal distinct activities mediated by the interaction of either memTNFΔ1–9,K11E KI or memTNFΔ1–12 with TNF receptors. Our data show that cell-bound as well as soluble TNFR2 play a critical role in the outcome of the infection.
Results
Mice without solTNF and expressing only memTNFΔ1–9,K11E are more resistant to M. bovis BCG infection than mice with memTNFΔ1–12
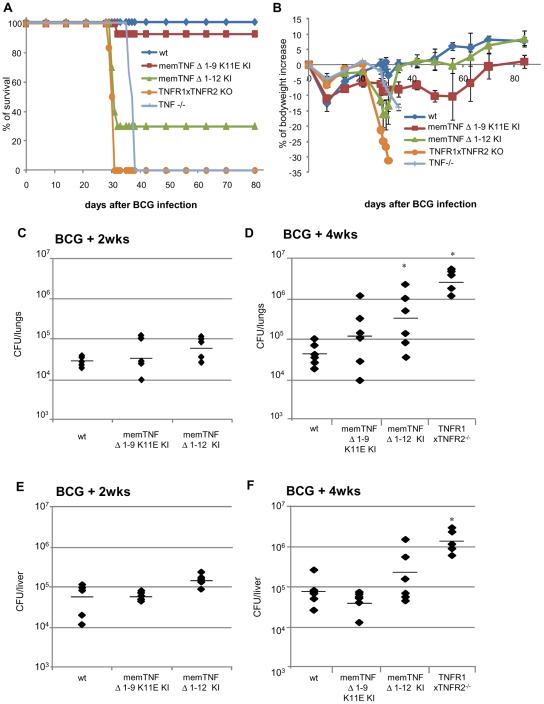
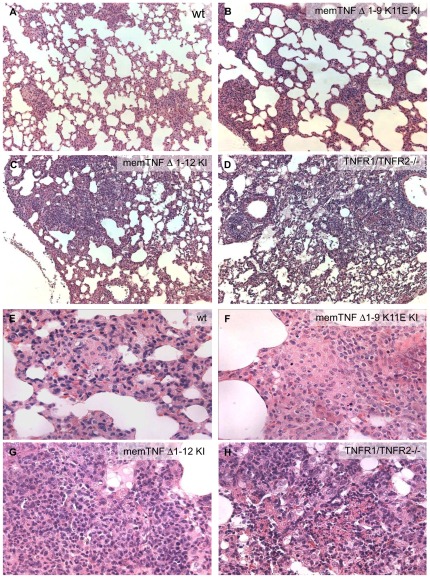
To explore the protective activities of the transmembrane form of TNF against M. bovis BCG infection, we compared the development of host defense mechanisms against this pathogen in two different memTNF KI mouse strains. We infected wild-type, memTNFΔ1–9,K11E [6] and memTNFΔ1–12 [5], double TNFR1/TNFR2−/−, and TNF−/− mice by the i.v. route. Wild-type mice were resistant to M. bovis BCG infection; one out of 14 (93% survival) memTNFΔ1–9,K11E KI mice died, whereas 7 out of 10 (30% survival) memTNFΔ1–12 KI mice succumbed to the infection with loss of body weight, and all TNFR1/TNFR2 −/− and TNF−/− mice died (Fig. 1A, B). After infection with a different strain of M. bovis BCG (Pasteur), we observed total survival of memTNFΔ1–9,K11E KI mice, while 80% of memTNFΔ1–12 KI mice succumbed to the infection between days 25 and 45 and exhibited significant loss of body weight (Fig. S1). Infection of memTNFΔ1–12 KI mice deficient in TNFR1 or TNFR2 resulted in similar pattern than memTNFΔ1–12 KI mice at day 50 after infection (Fig. S1A, B). Therefore, both infections with M. bovis BCG strains confirmed the higher susceptibility of memTNFΔ1–12 KI mice compared to memTNFΔ1–9,K11E KI and wild-type mice. The enhanced susceptibility of memTNFΔ1–12 KI mice versus memTNFΔ1–9,K11E KI mice was confirmed by bacterial load in lungs and liver as shown in Figure 1C–F. Deficiency of either TNFR1 or TNFR2 in memTNFΔ1–12 KI mice showed an increased bacterial load in liver and lungs at 4 weeks after M. bovis BCG infection as compared to memTNFΔ1–12 KI mice, indicating that both receptors could play a role in memTNFΔ1–12 KI signalling (Fig. S1C, D). Histopathological examination of lungs at 4 weeks post-infection revealed that memTNFΔ1–9,K11E KI mice formed granulomas of larger size than wild-type mice (average diameter was 197±87 versus 170±30 µm in wild-type) (Fig. 2A, B), and that these granulomas contained multinucleated giant cells as in wild-type pulmonary granulomas (Figure 2E, F). This pathology contrasted with that observed in memTNFΔ1–12 KI and TNFR1/TNFR2−/− mice which showed extended pulmonary lesions (average diameter of inflammatory foci was 310±100 µm and 481±120 µm, p<0,01 and p<0,02 vs wild-type, respectively) (Fig. 2C, D) exhibiting abundant lymphocytes and absence of multinucleated giant cells (Fig. 2G, H). In particular, TNFR1/TNFR2−/− mice developed extensive necrotic pulmonary lesions (Fig. 2H).
Figure 1. Survival curve, body weight and bacterial loads in lung and liver of mice infected with 107CFU of M. bovis BCG.
(A) Long-term survival of mice infected with living M. bovis BCG Connaught (107). (B) Body weight change after M. bovis BCG infection. Wild-type and memTNFΔ1–9,K11E KI, (n = 14 mice per group), memTNFΔ1–12 (n = 10 mice), and TNF−/− mice (n = 6 per group). Data from two representative experiments are shown. CFU were determined in lungs (C, D) and liver (E, F) at 2 and 4 weeks after infection with 107 CFU of M. bovis BCG. Data are represented as individual values and horizontal bars indicate mean (n = 4–6 mice per group). Asterisks indicate statistically significant differences between wild type and indicated group (*, p<0.03).
Figure 2. Histopathology of pulmonary lesions 4 weeks after M. bovis BCG infection.
Wild-type mouse lung (A, E) shows small granulomas containing multinucleated giant cells, memTNFΔ1–9,K11E KI mouse lung (B, F) shows larger granulomas compared with wild-type, also presenting multinucleated giant cells, and memTNFΔ1–12 KI (C, G) and TNFR1/TNFR2−/− (D, H) mouse lungs exhibit large lesions containing numerous lymphocytes, neutrophils and monocytes, but lacking multinucleated giant cells. Regions of necrosis are observed in TNFR1/TNFR2−/− lungs. Figure is representative of two experiments (n = 6 per group). Magnification A–D 100× and E–H 400×.
Different cytokine, chemokine, inflammatory cell and NF-κB activation during M. bovis BCG infection in memTNFΔ1–9,K11E and memTNFΔ1–12 KI mice
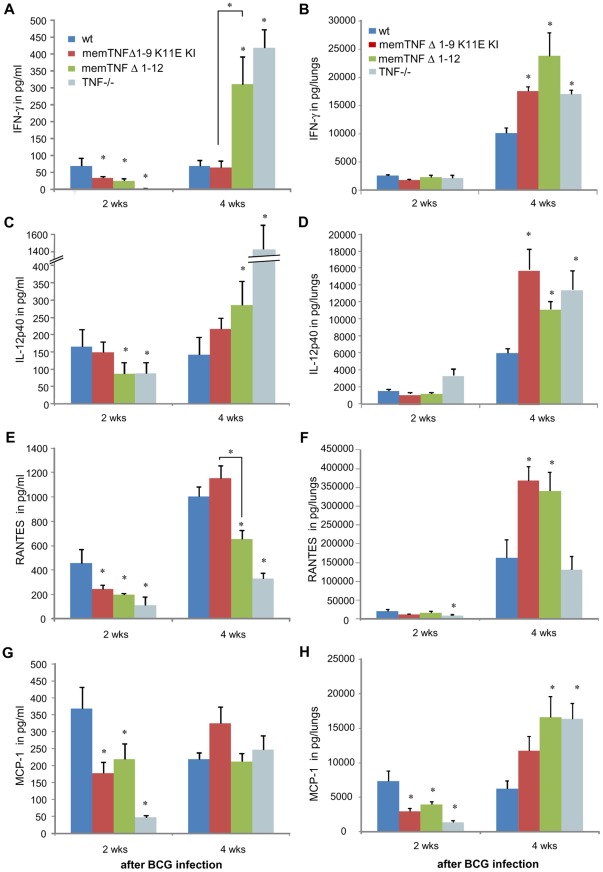
To determine whether memTNFΔ1–9,K11E KI mice and memTNFΔ1–12 KI mice are able to induce Th-1 type cytokines as well as chemokines upon M. bovis BCG infection, the levels of IFN-γ, IL-12p40, RANTES and MCP-1 were evaluated in the serum and lungs and compared to those of wild-type mice. IFN-γ serum levels of memTNFΔ1–9,K11E KI and memTNFΔ1–12 KI mice were lower than those in wild-type mice at 2 weeks, but at 4 weeks after M. bovis BCG infection, exacerbated expression of IFN-γ was observed only in memTNFΔ1–12 KI and TNF−/− mice, whereas memTNFΔ1–9,K11E KI mice exhibited similar level to wild-type mice (Fig. 3A). In the lung, IFN-γ amounts were similar in all groups of mice at 2 weeks and increased in all mutant mice 4 weeks post-infection (Fig. 3B). IL-12p40 serum amounts were comparable in memTNFΔ1–9,K11E KI and wild-type mice but lower in memTNFΔ1–12 KI and TNF−/− mice at 2 weeks, and at 4 weeks, they were higher in memTNFΔ1–12 KI, and TNF−/− mice (Fig. 3C). IL-12p40 lung content also revealed increased values in all mutant mice at 4 weeks infection compared to wild-type mice (Fig. 3D).
Figure 3. Serum and lung levels of cytokines and chemokines after M. bovis BCG infection.
IFN-γ levels were assessed in serum (A) and in lungs (B) at 2 and 4 weeks after M. bovis BCG infection. Serum (C) and lung (D) amounts of IL-12p40 were measured at 2 and 4 weeks after M. bovis BCG infection. Data are mean ± SEM and are representative of two independent experiments (n = 6–10 per group). *, p<0.03. RANTES (E, F) and MCP-1 (G, H) amounts were measured in serum (E, G) and in lungs (F, H) at 2 and 4 weeks after M. bovis BCG infection. Data are represented as means ± SEM from two independent experiments (n = 4–6 per group). *, p<0.04.
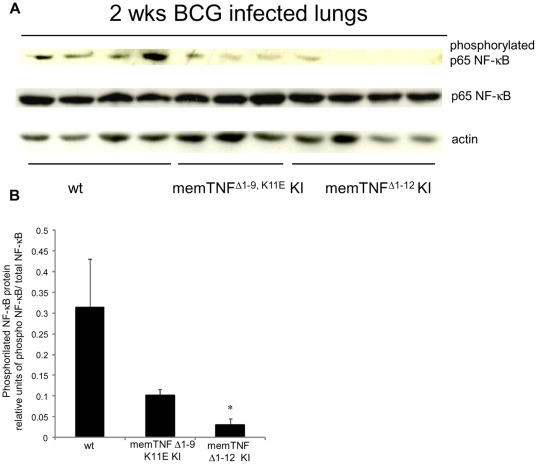
Serum amounts of RANTES at 2 weeks infection were reduced in mutant mice, but at 4 weeks, levels were only lower in memTNFΔ1–12 KI and TNF−/− mice compared to wild-type mice (Fig. 3E). RANTES lung amounts were increased at 4 weeks of infection in memTNFΔ1–9,K11E KI and in memTNFΔ1–12 KI mice compared to wild-type mice (Fig. 3F). MCP-1 serum levels were decreased in mutant mice at early infection as also observed for lung levels in all mutant mice, but at 4 weeks infection they were increased in memTNFΔ1–12 KI and TNF−/− mice but not in memTNFΔ1–9,K11E KI mice compared to wild-type mice, suggesting an enhanced activity of lung macrophages (Fig. 3G, H). A general pattern of activation of inflammatory mediators revealed a delay in mutant mice at early infection which was attenuated in memTNFΔ1–9,K11E KI mice. At late infection in mice suffering of progressive disease, an exacerbation of cytokine release was observed such as in memTNFΔ1–12 KI and TNF−/− mice whereas memTNFΔ1–9,K11E KI mice exhibited normal or attenuated responses. To gain insight into the deficient pattern of activation observed at two weeks infection in memTNF KI mice, NF-κB phosphorylation patterns were analyzed by western blot. The pulmonary protein expression of the phosphorylated form of the p65 NF-κB subunit was compared with the unphosphorylated form. Phosphorylated p65 NF-κB was reduced in memTNFΔ1–9,K11E KI mice but significantly much lower in memTNFΔ1–12 KI after M. bovis BCG infection indicating impaired cell activation in memTNFΔ1–12 KI mice (Fig. 4).
Figure 4. Decreased pulmonary phosphorylated p65 NF-κB in memTNFΔ1–12 KI mice after 2 weeks of M. bovis BCG infection.
(A) Phosphorylated and unphosphorylated p65 NF-κB and actin protein expressions were detected in lungs by western blot 2 weeks after M. bovis BCG infection. (B) Quantification of phosphorylated and unphosphorylated p65 NF-κB on western blot was done by Quantity One® analysis software on two different experiments. Results are expressed as mean ± SEM of relative units of phosphorylated p65 NF-κB/total p65 NF-κB (n = 4–5 mice/group) (*, p<0.02).
To explore whether the deficient pattern of cytokines in the circulation observed in mutant mice corresponds to the ability to mobilize and activate inflammatory cells to the site of infection, circulating activated inflammatory cells were characterized at early infection. Peripheral blood leucocytes after 1 week of M. bovis BCG infection were analyzed in memTNFΔ1–9,K11E KI and memTNFΔ1–12 KI mice. Blood granulocytes (Gr1+) were lower in memTNFΔ1–12 KI mice which showed no difference before and after M. bovis BCG infection (Fig. S2A, B). In addition, the proportion of monocytes CD11b+ Gr1− (resident macrophages) and CD11b+ Gr1+ (inflammatory macrophages) were also lower in memTNFΔ1–12 KI mice (Fig. S2C, D). These data suggest that the capacity to activate NF-κB and inflammatory cells, and to release cytokines and chemokines at early infection is impaired in memTNFΔ1–12 KI mice and this may be critical in the progression of the infection.
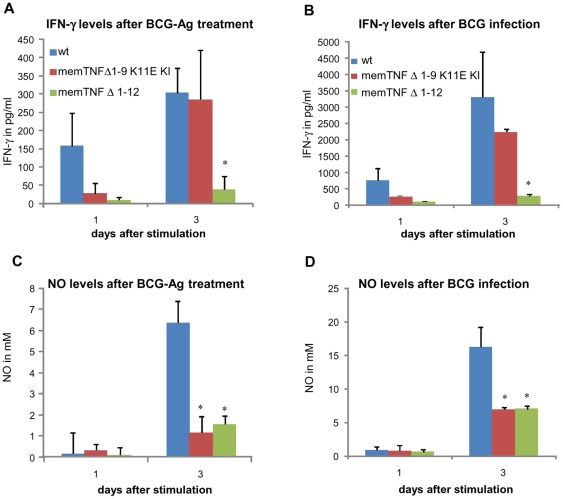
Deficient IFN-γ antigen-specific production in memTNFΔ1–12 but not in memTNFΔ1–9,K11E KI mice
We further analyzed the capacity of lymphocytes to respond to antigen-specific stimulation to explore any difference between memTNFΔ1–9,K11E KI and memTNFΔ1–12 KI mouse Th1 type immune responses. IFN-γ production was assessed after antigen-specific stimulation of splenocytes from 4 weeks M. bovis BCG-infected mice with BCG culture proteins or with living M. bovis BCG. MemTNFΔ1–9,K11E KI splenocytes released comparable amounts of IFN-γ as wild-type, whereas memTNFΔ1–12 KI splenocytes dramatically lacked IFN-γ production (Fig. 5A) indicating a deficiency in T-antigen-specific cell activation in memTNFΔ1–12 but not in memTNFΔ1–9,K11E KI mice. Splenocyte activation with live M. bovis BCG gave similar results; IFN-γ production was lower in memTNFΔ1–12 KI cells (Fig. 5B). We also assessed antigen-activated Nitrite/Nitrate as a surrogate of NO production, which is mainly released by macrophages, and observed that NO production was similar in memTNFΔ1–9,K11E KI and memTNFΔ1–12 KI splenocytes. Amounts were much lower than in wild-type cells after antigen activation and also after M. bovis BCG infection, indicating the importance of soluble TNF for iNOS activity of macrophages (Fig. 5C, D). We further asked if IFN-γ antigen-specific deficient activation of memTNFΔ1–12 cells could be attributed to differences in splenocyte populations in infected mice. But surprisingly, we found that the number of CD4+ T cells was 4 times higher in memTNFΔ1–12 KI compared to memTNFΔ1–9,K11E KI, and wild-type mice (Fig. S3A). However, the total number of CD11b+ was comparable in memTNFΔ1–9,K11E KI, memTNFΔ1–12 KI and wild-type mice (Fig. 6C) suggesting that memTNF cannot replace soluble TNF in activating splenic iNOS ex-vivo.
Figure 5. Antigen-specific IFN-γ and nitric oxide release from splenocytes of M. bovis BCG-infected mice.
IFN-γ and NO (nitric oxide) were evaluated in culture supernatant from cells incubated with antigens derived from M. bovis BCG (A and C) or with 103 viable M. bovis BCG (B and D). Values are represented as mean ± SEM (n = 3 animals per group, assayed in triplicate). * p<0.04.
Figure 6. Decreased iNOS protein in memTNF KI but similar number of splenic CD11b+/TNF+ cells 4 weeks after M. bovis BCG infection.
(A) Spleen iNOS protein expression was detected by western blot 4 weeks after M. bovis BCG infection. (B) iNOS protein was quantified by Image Quant software. Results are expressed as mean ± SEM of relative units of iNOS/actin (n = 4, except for TNFR1/TNFR2−/− mice n = 2 per group). *, p<0.04. FACS analyses showing the number of CD11b+ cells (C) and of CD11b+/TNF+ (D) in the spleen of uninfected, 2 and 4 weeks infected mice. Results are shown as mean ± SEM of positive cells per spleen (n = 4). *, p<0.01 compared to wild-type mice.
iNOS levels are reduced in M. bovis BCG-infected memTNFΔ1–12 KI mice compared to memTNFΔ1–9,K11E KI mice
Activation of iNOS is a bactericidal mechanism essential for M. bovis BCG clearance and mouse survival [19]. The expression of iNOS protein in the spleen at 4 weeks post-infection was evaluated by western blot. MemTNFΔ1–9,K11E KI, memTNFΔ1–12 KI and TNFR1/TNFR2−/− mice showed decreased iNOS protein expression compared to wild-type mice (Fig. 6A). In agreement with previous experiments, memTNFΔ1–9,K11E KI mice had higher iNOS levels than memTNFΔ1–12 KI mice, suggesting that memTNFΔ1–9,K11E activates iNOS in vivo more efficiently than memTNFΔ1–12. These observations were confirmed by the normalization of the iNOS band with actin (Fig. 6B). These results indicate that iNOS activation is deficient in memTNFΔ1–12 KI compared to memTNFΔ1–9,K11E KI mice. We asked if the deficiency of memTNFΔ1–12 KI mice was due to reduced number of macrophages or to a differential expression of transmembrane TNF on macrophages and assessed the total number of CD11b+ and CD11b+/TNF+ cells in spleen before and after the infection (Fig. 6C, D). The number of macrophages expressing TNF was similar in wild-type, memTNFΔ1–9,K11E KI and memTNFΔ1–12 KI mice indicating that this was not accounting for deficient iNOS expression. In contrast, the number of CD4+ T cells expressing TNF was higher in memTNFΔ1–12 KI than in memTNFΔ1–9,K11E KI and wild-type mice (Fig. S3B). Indeed, the lack of iNOS expression in memTNFΔ1–12 KI mice was not due to reduced number of neither macrophages nor CD4 T cells expressing memTNF. These data indicate that interaction of memTNF with both soluble and membrane TNFRs can be implicated in protection and susceptibility to the infection.
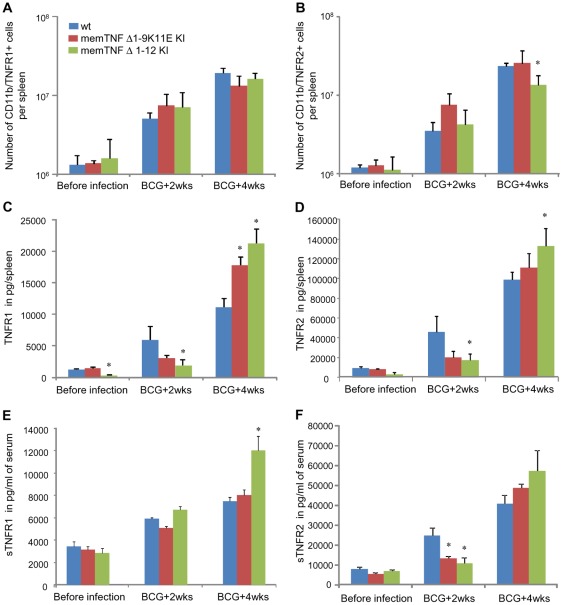
Alteration of TNF receptors in memTNFΔ1–12 KI mice upon M. bovis BCG infection
To investigate whether regulatory mechanisms of membrane TNF receptor as well as TNF receptor shedding could explain the enhanced sensitivity of memTNFΔ1–12 KI mice to intracellular bacterial infection, we analysed cells expressing TNFR1 and TNFR2 and total amounts of TNF receptors in mouse spleen before and after the infection. FACS analyses showed that the number of spleen macrophages expressing TNFR1 was similar in wild-type, memTNFΔ1–9,K11E KI, and memTNFΔ1–12 KI mice. In contrast, after 4 weeks of infection, TNFR2+ macrophages were reduced in memTNFΔ1–12 KI compared to wild-type and memTNFΔ1–9,K11E KI mice indicating a decreased signalling through TNFR2 which is considered to play an important role in memTNF activity (Fig. 7A, B). TNFR2 is cleaved at the cell surface by the TACE (ADAM 17) to form the soluble (s) TNFR2 that can antagonize the activity of solTNF and memTNF. Evaluation of the total amount of TNF receptors by ELISA in spleen homogenates revealed that TNFR1 and TNFR2 levels were lower at 2 weeks infection in memTNFΔ1–12 KI mice, but were significantly increased at 4 weeks infection when mice showed disease symptoms (Fig. 7C, D). It is of interest that the amounts of TNFR1 increased 100-folds after infection in memTNFΔ1–12 KI mouse spleen whereas in memTNFΔ1–9,K11E KI and wild-type mice this increases was only 12 and 9-folds, respectively. Similarly, M. bovis BCG-induced TNFR2 augmented in the spleen of memTNFΔ1–12 KI mice 38-folds whereas in memTNFΔ1–9,K11E KI and wild-type mice was only 13 and 10-folds, respectively. However, the levels of spleen TNFR2 were much higher (6- to 15-folds) than those of TNFR1 before and after infection (Fig. 7C, D). Similarly to the spleen, circulating sTNFR2 amounts were lower in memTNF KI mice and increased at 4 weeks infection suggesting that spleen pattern reflects sTNFR2. The amounts of sTNFR1 were significantly higher in memTNFΔ1–12 KI mice but those of sTNFR2 were again much higher than sTNFR1 indicating a major role in memTNF inhibition (Fig. 7E, F). These data suggest that TNFRs and in particular TNFR2 can be released more abundantly by activated macrophages during an infection leading to neutralization of memTNFΔ1–12 molecules which can be critical in severe progressive infection.
Figure 7. Lower number of macrophages expressing membrane bound TNFR2 but higher soluble TNFRs in memTNFΔ1–12 KI mice.
FACS analyses showing number of spleen CD11b+ cells expressing membrane TNFR1 (A) or TNFR2 (B) before or during M. bovis BCG infection. Results are shown as means ± SEM of spleen cell numbers (n = 3–4). *, p<0.02 compared to wild-type mice. Total amounts of TNFR1 (C) and TNFR2 (D) were evaluated on total spleen extracts during M. bovis BCG infection. Results are shown as means ± SEM of pg per spleen (n = 4–6). *, p<0.05 compared to wild-type mice. Amounts of solTNFR1 (E) and solTNFR2 (F) were assessed in the serum of mice before and after infection. Results as represented as means ± SEM of pg/ml of serum (n = 6–10). *, p<0.05 compared to wild-type.
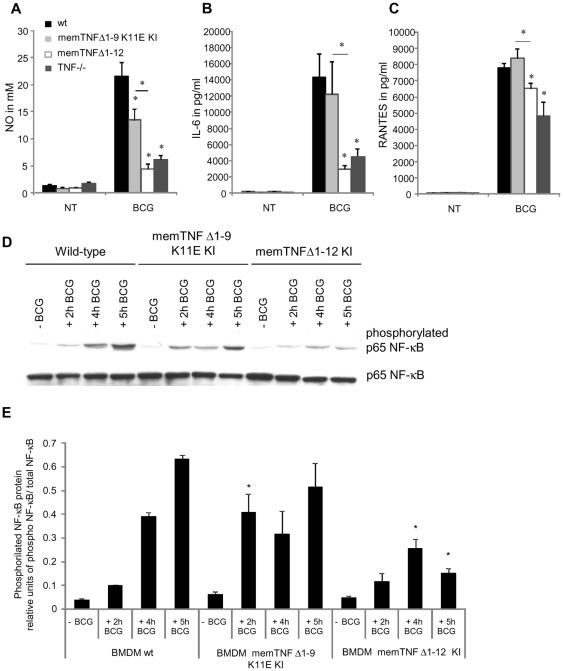
Altered M. bovis BCG-induced nitric oxide, cytokine and chemokine responses and NF-κB activation of bone marrow-derived macrophages from memTNFΔ1–12 KI mice
To explore whether the differences observed between the two memTNF KI mice reflect a deficiency in macrophage activity of memTNFΔ1–12 KI mice, bone marrow-derived macrophages (BMDM) were infected with M. bovis BCG and production of NO, IL-6 and RANTES was assessed. Production of NO was significantly lower in memTNFΔ1–12 KI than in memTNFΔ1–9,K11E KI BMDM although the latter was reduced when compared to wild-type BMDM (Fig. 8A). M. bovis BCG-induced IL-6 and RANTES was similar or increased in memTNFΔ1–9,K11E KI and in wild-type BMDM but lower in memTNFΔ1–12 KI and TNF−/− BMDM (Fig. 8B, C).
Figure 8. BMDM nitric oxide, IL-6, RANTES production and p65 NF-κB activation by M. bovis BCG infection.
NO (A), IL-6 (B) and RANTES (C) levels were assessed in supernatant of BMDM 24 hours after M. bovis BCG infection. These results are representative of two independent experiments and values are represented as mean ± SEM (n = 3 animals per group, assayed in triplicate) *p<0.05. (D) Phosphorylated and unphosphorylated p65 NF-κB proteins were detected by western blot in BMDM not infected or infected with M. bovis BCG at different time points. (E) Quantification of phosphorylated p65 NF-κB on western blot was done by Quantity One® analysis software on two different experiments. Results are expressed as mean ± SEM of relative units of phosphorylated p65 NF-κB/total p65 NF-κB (n = 2/group). *, p<0.05 compared to wild-type BMDM.
To gain insight into difference in M. bovis BCG-induced cellular activation of the two memTNF molecules, NF-κB phosphorylation patterns were analyzed by western blot. Phosphorylated p65 NF-κB progressively increased in wild-type BMDM up to 5 hours after M. bovis BCG infection. In memTNFΔ1–9,K11E KI BMDM, the activation of phosphorylated p65 NF-κB was faster than in wild-type BMDM and was already increased 2 hours after M. bovis BCG infection to similar levels as observed in wild-type BMDM 4 hours post-infection. In contrast, in M. bovis BCG-infected memTNFΔ1–12 KI BMDM, phosphorylation of p65 NF-κB protein was significantly reduced which confirms that memTNFΔ1–12 KI BMDM but not memTNFΔ1–9,K11E KI BMDM are deficient in NF-κB activation (Fig. 8D, E).
Discussion
The role of transmembrane TNF has been analyzed in different systems and it is now accepted that memTNF mediates important activities at the cellular level as well as in host defense mechanisms. Early reports of memTNF-mediated activities described the human memTNFΔ1–12 molecule which was shown to induce cell death and to be a predominant ligand for human TNFR2 [20], [21], [22]. The activities of mouse memTNF molecules used in the present study were originally analyzed by Decoster et al. on transfected mouse cells [23]. This study showed that deletion of the first 9 amino acids corresponding to mature TNF still led to production of soluble TNF, but that an additional Lys to Glu substitution at amino acid 11 gave rise to uncleavable membrane-bound TNF (memTNFΔ1–9,K11E) with biological activities similar to wild-type TNF. Comparison of memTNFΔ1–9, K11E with the murine mutant memTNFΔ1–12 showed that the latter induced 3-fold lower GM-CSF responses and involved cooperative effects of TNFR1 and TNFR2 [23]. The present study explores these two memTNF molecules expressed in mouse lacking solTNF for their capacity to stimulate cell-mediated immune responses to intracellular bacteria. Our data indicate that memTNFΔ1–9,K11E KI mice are substantially more resistant to M. bovis BCG infection than memTNFΔ1–12 KI mice, as demonstrated both by lower survival and significantly higher bacterial load, severity of pulmonary lesions and deficient pulmonary NF-κB activation in memTNFΔ1–12 KI mice. The deficiency of memTNFΔ1–12 KI mice to M. bovis BCG was confirmed by patterns of cytokine/chemokine and inflammatory cells that resembled TNF−/− whereas memTNFΔ1–9,K11E KI mice were more similar to wild-type mice or showed an intermediate phenotype that was in general sufficient to mount an efficient immune response to M. bovis BCG infection.
These two memTNF mouse strains have been previously infected with M. bovis BCG using two different routes and dosages. All memTNFΔ1–9,K11E KI mice survived to an intranasal infection with 106 CFU and only 50% of memTNFΔ1–12 KI mice survived to an intravenous infection (2×106 ) but infection conditions cannot be properly compared [17], [18] (see Table 1). Infection with L. monocytogenes showed difference in protection of the two memTNF strains as 100% memTNFΔ1–9,K11E KI resisted [8] whereas only 10% memTNFΔ1–12 KI mice survived to 104 CFU [5]. Similarly, infection with M. tuberculosis showed different susceptibilities since memTNFΔ1–9,K11E KI mice infected with 50–100 CFU died 150–230 days whilst memTNFΔ1–12 KI mice infected with 10–30 CFU died 50–170 days after (Table 1). M. bovis BCG-infected mice expressing memTNFΔ1–12 but neither TNFR2 nor TNFR1 showed no significant differences in survival at day 50 compared to memTNFΔ1–12 KI mice although memTNFΔ1–12 KI-TNFR2−/− started to succumb earlier. A previous report has shown that 45 days after M. tuberculosis infection about 20% of memTNFΔ1–12 KI-TNFR2−/− died while about 50% of memTNFΔ1–12 KI-TNFR1−/− and memTNFΔ1–12 KI mice succumbed [17]. Similarly to results shown for M. tuberculosis infection, the pattern of pulmonary bacterial load was not significantly different in memTNFΔ1–12 KI compared to memTNFΔ1–12 KI-TNFR2−/− and memTNFΔ1–12 KI-TNFR1−/− mice after M. bovis BCG infection. Our interpretation is that memTNF-TNFR2 interaction may play a role at early infection but then, the incidence on bacterial load at 4 weeks infection is minimal as protection can be mediated by cooperation of both TNF receptors, and in addition, other regulatory mechanisms such as TNFR regulation can be critical in disease outcome.
To further explore other factors of interest favouring protection, we analysed the capacity of spleen cells to respond to antigens and to produce IFN-γ and observed that memTNFΔ1–12 KI were deficient whereas memTNFΔ1–9,K11E KI cells were similar to wild-type cells. Surprisingly, the number of CD4+ T cells was four-fold higher in the spleen of memTNFΔ1–12 KI indicating that memTNFΔ1–12 KI cells are unable to respond to antigenic stimulation spite the moderated expansion of spleen CD4+ T cells. Previous report identified TNF as a negative regulator of Th1 type immune response during intracellular bacterial infection and showed an uncontrolled expansion of spleen CD4+ T cells, a marked increase of circulating and antigen-specific IFN-γ in TNF−/− mice [24]. Our data suggest that memTNF molecule appears to restrain exacerbation of Th1 immune response caused by lack of TNF. This is of interest considering the possibility of using the novel class of TNF inhibitors, dominant-negative (DN)-TNF biologics, that antagonize solTNF but not memTNF. We have shown that DN-TNF biologics protects from hepatitis but did not alter immunity against mycobacterial infections, presumably by maintenance of physiological memTNF signalling [7], [25].
We asked if anti-mycobacterial effector mechanisms in vivo such as iNOS were impaired and found that iNOS was much lower in the spleen of memTNFΔ1–12 KI than in memTNFΔ1–9,K11E KI mice, confirming a decrease in bactericidal mechanisms of memTNFΔ1–12 form. To further explore the mechanisms that can influence the activity of memTNF, we focus on the investigation of spleen macrophages expressing TNF and TNFRs during the infection. The number of macrophages expressing TNF increased with the infection similarly in the three groups of mice. Interestingly, memTNFΔ1–12 KI mice showed a decrease in the number of macrophages expressing TNFR2 suggesting that macrophages cannot respond to M. bovis BCG-activated memTNFΔ1–12. In addition, the observation that total amount of TNFR2 is higher in spleen homogenates from memTNFΔ1–12 KI mice indicates over-shedding of TNFR2 and that a regulatory mechanism of memTNF inhibition may be involved in the pathogenicity. We have previously shown that M. bovis BCG infection induces high levels of serum TNF in parallel to the release of TNF receptors and this is influenced by iNOS activity since iNOS−/− mice showed enhanced serum levels of TNF and TNFR2 [19]. We have also reported that circulating M. bovis BCG-induced TNF is not bioactive but rapidly neutralized by sTNFRs during an infection [25]. The presence of high amounts of sTNFR2 as observed in iNOS−/− mice indicates abnormal TACE activity in memTNFΔ1–12 KI cells leading to memTNF inactivation by sTNFR2. Although that both receptors are enzymatically digested from cells, the amounts of sTNFR2 are much higher (in general 5 to 15-folds) than sTNFR1 which means that the neutralizing activity of sTNFR2 may play a predominant role compared to sTNFR1. Several studies have pointed out the critical role of sTNFR2 in bacterial and viral infections. A report showed that apoptosis of M. tuberculosis-infected alveolar macrophages was inhibited by the release of TNFR2 that inactivated TNF [26]. It has been shown that the immunopathology associated with T-cell-mediated influenza clearance was abrogated in TNFR2−/− mice and that TNFR2 was not need for memTNF to activate MCP-1 activation, whereas both receptors were required for MCP-1 expression by solTNF in alveolar epithelial cells showing the complexity of sol/memTNF-mediated activities with receptors in different systems [27].
SolTNF can mediate optimal protection against mycobacterial infections by providing exocrine and paracrine signalling to many cell types. In contrast, the signal of transmembrane TNF is restricted to cell-to-cell contact which limits the intensity of the activity. Our study shows that both memTNF molecules mediate protection but the effect of memTNFΔ1–9,K11E appears clearly higher than the memTNFΔ1–12 molecule. The fact that memTNFΔ1–9,K11E KI mice can eventually become sensitive and succumb to the infection highlights a complex regulation of factors mediating innate and adaptive immune responses that can be subjected to individual situations. Among these factors the equilibrium between memTNF and cell-bound and sTNFRs can play a critical role in host defense against intracellular bacteria in vivo. Our hypothesis is that the activities of memTNF can be modulated by the levels of membrane and soluble TNF receptors which may influence the outcome of the infection thus explaining why memTNF KI mice can be protected or can die from the infection. We have previously shown, using transgenic mice expressing human soluble TNFR1-IgG, that expression levels of the TNF neutralizing transgene determined the enhanced protection to M. bovis BCG infection or the higher susceptibility of mice compared to littermate control mice. We found that low levels of soluble receptors were activating TNF expression and macrophage effector mechanisms whilst high levels of soluble receptors were neutralizing both sol and memTNF blocking all protective TNF-mediated activities [16]. The immune cellular activation was attributed to reverse signaling of memTNF binding to solTNFRs. We hypothesize that a precise regulation of memTNF activity can be orchestrated by membrane and soluble TNFRs and an unbalance of this regulatory and complex system can modify the outcome of the disease.
We finally investigate if memTNF bone-marrow derived macrophages could show different responses upon M. bovis BCG infection in vitro and observed that macrophages from memTNFΔ1–12 KI mice produced lower amounts of cytokines/chemokines and showed an impaired p65 NF-κB phosphorylation pattern indicating that the deficiency is already on memTNFΔ1–12 KI macrophages which will influence the host immune response. These data suggest that the small difference of the two memTNF molecules results in major effects in signalling and memTNF-mediated activities.
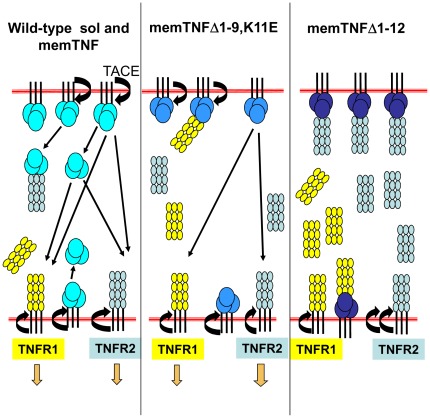
The mechanisms explaining the differences between memTNF molecules with only a minor change of 3 amino acids at positions 10–12 are still not elucidated. Some hypothesis can be envisaged to understand why such important consequence can occur in vivo. We hypothesize that TACE can still bind to memTNFΔ1–9,K11E although unable to digest whereas the deletion of 3 amino acids prevent the binding of TACE to memTNFΔ1–12. Upon TNF activation, TACE activity is directed to TNFR2 which can be found decreased on macrophages but substantially increased as solTNFR2 form that will neutralize memTNF thus preventing its biological activities (Figure 9).
Figure 9. Hypothesis explaining differences between memTNF molecules.
This figure presents the three situations explored in this work: wild-type TNF molecules which are digested by the TACE, and the two memTNF forms which cannot be digested and exert their activities by cell-to-cell contact. The difference between memTNFΔ1–9,K11E and memTNFΔ1–12 molecules may reside in the possibility of the TACE to bind but not cleave the memTNF Δ1–9,K11E, but in memTNFΔ1–12 the TACE binding site is not accessible and the protease activity is exerted on TNFR2 which became more frequently soluble thus neutralising memTNFΔ1–12 activities.
Materials and Methods
Mice
C57BL/6 mice, memTNFΔ1–9,K11E KI mice [6], memTNFΔ1–12 KI mice [5] memTNFΔ1–12×TNFR1−/− mice, memTNFΔ1–12×TNFR2−/− mice, TNFR1×TNFR2−/− mice and TNF−/− [28] mice were maintained under conventional conditions in the animal facility of the Medical Faculty, University of Geneva. All animal experiments were carried out in accordance with institutional guidelines and were approved by the academic ethical committee on animal experimentation and the Cantonal Veterinary Office from Geneva, authorization number: 31.1.1005/3202/2.
M. bovis BCG infection
Mice were infected intravenously (i.v.) with 107 living M. bovis BCG Connaught [29], or BCG Pasteur GFP [30] (used for survival curve in figure S1). Body weights were monitored during infection, and mice were sacrificed at 2 and 4 weeks post-infection, or 24 weeks post-infection for survival monitoring.
Determination of colony forming units (CFU) from infected organs
The number of viable bacteria recovered from frozen organs was evaluated as previously described [19].
Histological analyses
Histological analyses of liver were performed at 4 weeks after BCG infection. Livers were fixed in 4% buffered formaldehyde and embedded in paraffin for subsequent hematoxylin/eosin (H&E) staining. Evaluation of the lesions was done with Metamorph sofware.
Evaluation of serum, organ and cell culture supernatant levels of cytokines and chemokines
For cytokine and chemokine detection, organs were homogenized in 0.04% Tween 80/saline buffer (125 mg of tissue/mL) as previously described [31]. IFN-γ, IL-12p40, IL-6, MCP-1 RANTES, sTNFR1 and sTNFR2 amounts were evaluated in serum, organ extracts or cellular supernatant by ELISA with a sensitivity of 5–2000 pg/ml.
Western blot analysis
Splenic proteins were prepared and western blot performed as previously described [32]. Primary antibody was a polyclonal rabbit anti-mouse iNOS (Calbiochem, San Diego, CA; 1∶2000 dilution). A rabbit polyclonal anti-actin was used as control antibody. Goat anti-rabbit HRP was the secondary antibody (Bio-Rad, Hercules, CA; 1∶5000 dilution). Western blot was also used to measure expression of the phosphorylated form of NF-κB in lungs and bone marrow derived macrophages, which were lysed in RIPA buffer complete with phosphatase (phosSTOP, Roche, Germany) and protease inhibitors (Complete mini, Roche, Germany). Primary antibody was either a rabbit polyclonal anti-NF-κB p65 antibody (Santa Cruz Biotechnology, USA; 1∶500 dilution) or a rabbit monoclonal anti-phosphorylated NF-κB p65 antibody (Cell Signaling Technology, USA; 1∶1000 dilution). Goat anti-rabbit HRP was used as secondary antibody (Bio-Rad, USA; 1∶5000 dilution). Blots were developed with Immobilon western chemiluminescent HRP substrate kit (Millipore, USA). The density of bands was quantified by using Image Quant 3.3 measurement software (Molecular Dynamics, USA) or by Quantity One® analysis software (Bio-Rad, USA).
Antigen-specific release of nitric oxide and cytokines from spleen cells
Mice were infected and sacrificed 4 weeks later, and spleen cells were prepared as previously described [15]. Briefly, spleen cells were treated for 5 min with a 0.155 M ammonium chloride/0.010 M potassium bicarbonate solution for erythrocyte lysis, washed and resuspended in DMEM+10% FCS. Cells were plated at 5×105 cells per well in 96-well plates and were stimulated with either medium alone, living M. bovis BCG (103 CFU/well), or M. bovis BCG culture protein extracts (17 mg/ml) for one or three days. Cell culture medium was harvested for NO and cytokine determination. Nitrite accumulation was evaluated in culture medium as an indicator of NO production by Griess reagent (1% sulfanilamide and 0.1% naphtylethylenediamide in 2.5% phosphoric acid). Absorption was measured at 550 nm and nitrite concentrations were determined by comparison with OD of the NaNO2 standards. Cytokines were determined in cell supernatants as described below.
Flow cytometry analyses
Flow cytometry was performed on peripheral blood leukocytes and splenocytes. To obtain peripheral blood leukocytes, mice were bled one week after BCG infection, and flow cytometry was performed as previously described [33]. Spleen cells were obtained from uninfected and at 2 and 4 weeks after M. bovis BCG infection. Flow cytometry was performed using three- or four-color staining and analyzed with a FACSCalibur (BD Biosciences, Mountain View, CA). The following antibodies were used: anti-Gr1 (RB6-8C5) (eBioscience), anti-CD11b (clone M1/70) (BD Biosciences), anti-CD4 (clone GK1.5) (ImmunoTools GmbH, Germany), polyclonal anti-TNF, polyclonal anti-TNFR1 and polyclonal anti-TNFR2 (Hycult biotech). Staining was performed in the presence of a saturating concentration of 2.4G2 anti-Fcγ RII/III mAb. For spleen, data were calculated in total number of positive cells.
Bone marrow-derived macrophage (BMDM) culture and treatment
Macrophages were derived from bone marrow cells as previously described [34]. Briefly, bone marrow cells were flushed aseptically from the femurs of mice and cultured in DMEM supplemented with 10% fetal calf serum and 20% L929 cell-conditioned medium [34]. After 6 days of culture, BMDM were infected with M. bovis BCG (60 000 CFU/well) during 2, 4, 5 or 24 hours. The supernatant was harvested for NO and cytokine determination.
Statistical analyses
The one-way ANOVA was used for all analyses. P values<0.05 were considered as statistically significant.
Supporting Information
Survival curve and body weight of M. bovis BCG infected mice. (A) Long-term survival of mice infected with living M. bovis BCG Pasteur (107). (B) Body weight change after M. bovis BCG infection (n = 4–5 mice per group). Data from one representative experiment are shown. (C and D) CFU at 4 weeks after infection with 107 CFU of M. bovis BCG Connaught were determined in lungs (C) and liver (D). Data are represented as individual values and horizontal bars indicate mean (n = 4–6 mice per group). Asterisks indicate statistically significant differences between wild type and indicated group (*, p<0.03).
(TIF)
Peripheral blood mononuclear cells (PBMC) were reduced in memTNFΔ1–12 KI after 1 week of M. bovis BCG infection. (A) PBMC before infection and 1 week after M. bovis BCG infection were stained with anti-Gr1 monoclonal antibody (mAb). PBMC were gated for cells with higher granularity (high side–scatter properties) to distinguish polymorphonuclear cells. Numbers indicate the mean percentages of Gr1+ polymorphonuclear cells. (B) Percentages of Gr1+ cells are shown (n = 3 mice per group) (*, p<0.04). (C) PBMC from the same group of mice before and 1 week after M. bovis BCG infection were stained with a combination of anti-CD11b and anti-Gr1 monoclonal antibodies (mAb) and were gated for cells with lower granularity (low side–scatter properties) to distinguish them from polymorphonuclear cells. (D) Percentage of cells is shown in histogram (n = 3 mice per group) (*, p<0.03).
(TIF)
Decreased number of splenic CD4+ and CD4+/TNF+ cells 4 weeks after M. bovis BCG infection. Number of CD4+ T (A) and CD4+/TNF+ T (B) cells in spleen at 4 weeks of M. bovis BCG infection were increased in memTNFΔ1–12 KI mice. Data were represented as means ± SEM of positive cell number per spleen (n = 3–4 mice per group) (*, p<0.02).
(TIF)
Acknowledgments
The authors thank Ms. Joanne Stalder, and Mr. Tri Le Minh for their contribution to this work. We thank Dr. David Szymkowski for reading and comments on the manuscript. We are grateful to Dr. Fabien Depis for helpful discussions.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: The work was supported by Grants 3200A0-118196 (to I.G.) from the Swiss National Foundation for Scientific Research and from the Science and Technology Cooperation Program Switzerland-Russia. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Tracey D, Klareskog L, Sasso EH, Salfeld JG, Tak PP. Tumor necrosis factor antagonist mechanisms of action: a comprehensive review. Pharmacol Ther. 2008;117:244–279. doi: 10.1016/j.pharmthera.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Garcia I, Olleros ML, Quesniaux VF, Jacobs M, Allie N, et al. Roles of soluble and membrane TNF and related ligands in mycobacterial infections: effects of selective and non-selective TNF inhibitors during infection. Adv Exp Med Biol. 2011;691:187–201. doi: 10.1007/978-1-4419-6612-4_20. [DOI] [PubMed] [Google Scholar]
- 3.Horiuchi T, Mitoma H, Harashima S, Tsukamoto H, Shimoda T. Transmembrane TNF-alpha: structure, function and interaction with anti-TNF agents. Rheumatology (Oxford) 2010;49:1215–1228. doi: 10.1093/rheumatology/keq031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kusters S, Tiegs G, Alexopoulou L, Pasparakis M, Douni E, et al. In vivo evidence for a functional role of both tumor necrosis factor (TNF) receptors and transmembrane TNF in experimental hepatitis. Eur J Immunol. 1997;27:2870–2875. doi: 10.1002/eji.1830271119. [DOI] [PubMed] [Google Scholar]
- 5.Alexopoulou L, Kranidioti K, Xanthoulea S, Denis M, Kotanidou A, et al. Transmembrane TNF protects mutant mice against intracellular bacterial infections, chronic inflammation and autoimmunity. Eur J Immunol. 2006;36:2768–2780. doi: 10.1002/eji.200635921. [DOI] [PubMed] [Google Scholar]
- 6.Ruuls SR, Hoek RM, Ngo VN, McNeil T, Lucian LA, et al. Membrane-bound TNF supports secondary lymphoid organ structure but is subservient to secreted TNF in driving autoimmune inflammation. Immunity. 2001;15:533–543. doi: 10.1016/s1074-7613(01)00215-1. [DOI] [PubMed] [Google Scholar]
- 7.Olleros ML, Vesin D, Fotio AL, Santiago-Raber ML, Tauzin S, et al. J Hepatol; 2010. Soluble TNF, but not membrane TNF, is critical in LPS-induced hepatitis. [DOI] [PubMed] [Google Scholar]
- 8.Torres D, Janot L, Quesniaux VF, Grivennikov SI, Maillet I, et al. Membrane tumor necrosis factor confers partial protection to Listeria infection. Am J Pathol. 2005;167:1677–1687. doi: 10.1016/S0002-9440(10)61250-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Musicki K, Briscoe H, Tran S, Britton WJ, Saunders BM. Differential requirements for soluble and transmembrane tumor necrosis factor in the immunological control of primary and secondary Listeria monocytogenes infection. Infect Immun. 2006;74:3180–3189. doi: 10.1128/IAI.02004-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cowley SC, Goldberg MF, Ho JA, Elkins KL. The membrane form of tumor necrosis factor is sufficient to mediate partial innate immunity to Francisella tularensis live vaccine strain. J Infect Dis. 2008;198:284–292. doi: 10.1086/589620. [DOI] [PubMed] [Google Scholar]
- 11.Allenbach C, Launois P, Mueller C, Tacchini-Cottier F. An essential role for transmembrane TNF in the resolution of the inflammatory lesion induced by Leishmania major infection. Eur J Immunol. 2008;38:720–731. doi: 10.1002/eji.200737662. [DOI] [PubMed] [Google Scholar]
- 12.Fremond C, Allie N, Dambuza I, Grivennikov SI, Yeremeev V, et al. Membrane TNF confers protection to acute mycobacterial infection. Respir Res. 2005;6:136. doi: 10.1186/1465-9921-6-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saunders BM, Tran S, Ruuls S, Sedgwick JD, Briscoe H, et al. Transmembrane TNF is sufficient to initiate cell migration and granuloma formation and provide acute, but not long-term, control of Mycobacterium tuberculosis infection. J Immunol. 2005;174:4852–4859. doi: 10.4049/jimmunol.174.8.4852. [DOI] [PubMed] [Google Scholar]
- 14.Mueller C, Corazza N, Trachsel-Loseth S, Eugster HP, Buhler-Jungo M, et al. Noncleavable transmembrane mouse tumor necrosis factor-alpha (TNFalpha) mediates effects distinct from those of wild-type TNFalpha in vitro and in vivo. J Biol Chem. 1999;274:38112–38118. doi: 10.1074/jbc.274.53.38112. [DOI] [PubMed] [Google Scholar]
- 15.Olleros ML, Guler R, Corazza N, Vesin D, Eugster HP, et al. Transmembrane TNF induces an efficient cell-mediated immunity and resistance to Mycobacterium bovis bacillus Calmette-Guerin infection in the absence of secreted TNF and lymphotoxin-alpha. J Immunol. 2002;168:3394–3401. doi: 10.4049/jimmunol.168.7.3394. [DOI] [PubMed] [Google Scholar]
- 16.Guler R, Olleros ML, Vesin D, Parapanov R, Garcia I. Differential effects of total and partial neutralization of tumor necrosis factor on cell-mediated immunity to Mycobacterium bovis BCG infection. Infect Immun. 2005;73:3668–3676. doi: 10.1128/IAI.73.6.3668-3676.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allie N, Alexopoulou L, Quesniaux VJ, Fick L, Kranidioti K, et al. Immunology; 2008. Protective role of membrane tumour necrosis factor in the host's resistance to mycobacterial infection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dambuza I, Allie N, Fick L, Johnston N, Fremond C, et al. Efficacy of membrane TNF mediated host resistance is dependent on mycobacterial virulence. Tuberculosis (Edinb) 2008;88:221–234. doi: 10.1016/j.tube.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 19.Garcia I, Guler R, Vesin D, Olleros ML, Vassalli P, et al. Lethal Mycobacterium bovis Bacillus Calmette Guerin infection in nitric oxide synthase 2-deficient mice: cell-mediated immunity requires nitric oxide synthase 2. Lab Invest. 2000;80:1385–1397. doi: 10.1038/labinvest.3780146. [DOI] [PubMed] [Google Scholar]
- 20.Eissner G, Kohlhuber F, Grell M, Ueffing M, Scheurich P, et al. Critical involvement of transmembrane tumor necrosis factor-alpha in endothelial programmed cell death mediated by ionizing radiation and bacterial endotoxin. Blood. 1995;86:4184–4193. [PubMed] [Google Scholar]
- 21.Perez C, Albert I, DeFay K, Zachariades N, Gooding L, et al. A nonsecretable cell surface mutant of tumor necrosis factor (TNF) kills by cell-to-cell contact. Cell. 1990;63:251–258. doi: 10.1016/0092-8674(90)90158-b. [DOI] [PubMed] [Google Scholar]
- 22.Grell M, Douni E, Wajant H, Lohden M, Clauss M, et al. The transmembrane form of tumor necrosis factor is the prime activating ligand of the 80 kDa tumor necrosis factor receptor. Cell. 1995;83:793–802. doi: 10.1016/0092-8674(95)90192-2. [DOI] [PubMed] [Google Scholar]
- 23.Decoster E, Vanhaesebroeck B, Vandenabeele P, Grooten J, Fiers W. Generation and biological characterization of membrane-bound, uncleavable murine tumor necrosis factor. J Biol Chem. 1995;270:18473–18478. doi: 10.1074/jbc.270.31.18473. [DOI] [PubMed] [Google Scholar]
- 24.Zganiacz A, Santosuosso M, Wang J, Yang T, Chen L, et al. TNF-alpha is a critical negative regulator of type 1 immune activation during intracellular bacterial infection. J Clin Invest. 2004;113:401–413. doi: 10.1172/JCI18991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Olleros ML, Vesin D, Lambou AF, Janssens JP, Ryffel B, et al. J Infect Dis; 2009. Dominant-Negative Tumor Necrosis Factor Protects from Mycobacterium bovis Bacillus Calmette-Guerin (BCG) and Endotoxin-Induced Liver Injury without Compromising Host Immunity to BCG and Mycobacterium tuberculosis. [DOI] [PubMed] [Google Scholar]
- 26.Balcewicz-Sablinska MK, Keane J, Kornfeld H, Remold HG. Pathogenic Mycobacterium tuberculosis evades apoptosis of host macrophages by release of TNF-R2, resulting in inactivation of TNF-alpha. J Immunol. 1998;161:2636–2641. [PubMed] [Google Scholar]
- 27.Liu J, Zhao MQ, Xu L, Ramana CV, Declercq W, et al. Requirement for tumor necrosis factor-receptor 2 in alveolar chemokine expression depends upon the form of the ligand. Am J Respir Cell Mol Biol. 2005;33:463–469. doi: 10.1165/rcmb.2005-0204OC. [DOI] [PubMed] [Google Scholar]
- 28.Marino MW, Dunn A, Grail D, Inglese M, Noguchi Y, et al. Characterization of tumor necrosis factor-deficient mice. Proc Natl Acad Sci U S A. 1997;94:8093–8098. doi: 10.1073/pnas.94.15.8093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hanus M, Matouskova M, Verner P, Hyrsl L. Immunotherapy of superficial bladder tumors: preliminary results with ImmuCyst–BCG Connaught, Toronto. Neoplasma. 1994;41:25–27. [PubMed] [Google Scholar]
- 30.Kaps I, Ehrt S, Seeber S, Schnappinger D, Martin C, et al. Energy transfer between fluorescent proteins using a co-expression system in Mycobacterium smegmatis. Gene. 2001;278:115–124. doi: 10.1016/s0378-1119(01)00712-0. [DOI] [PubMed] [Google Scholar]
- 31.Olleros ML, Vesin D, Martinez-Soria E, Allenbach C, Tacchini-Cottier F, et al. Interleukin-12p40 overexpression promotes interleukin-12p70 and interleukin-23 formation but does not affect bacille Calmette-Guerin and Mycobacterium tuberculosis clearance. Immunology. 2007;122:350–361. doi: 10.1111/j.1365-2567.2007.02646.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guler R, Olleros ML, Vesin D, Parapanov R, Vesin C, et al. Inhibition of inducible nitric oxide synthase protects against liver injury induced by mycobacterial infection and endotoxins. J Hepatol. 2004;41:773–781. doi: 10.1016/j.jhep.2004.07.031. [DOI] [PubMed] [Google Scholar]
- 33.Santiago-Raber ML, Amano H, Amano E, Baudino L, Otani M, et al. Fcgamma receptor-dependent expansion of a hyperactive monocyte subset in lupus-prone mice. Arthritis Rheum. 2009;60:2408–2417. doi: 10.1002/art.24787. [DOI] [PubMed] [Google Scholar]
- 34.Fotio AL, Olleros ML, Vesin D, Tauzin S, Bisig R, et al. In vitro inhibition of lipopolysaccharide and mycobacterium bovis bacillus Calmette Guerin-induced inflammatory cytokines and in vivo protection from D-galactosamine/LPS -mediated liver injury by the medicinal plant Sclerocarya birrea. Int J Immunopathol Pharmacol. 2010;23:61–72. doi: 10.1177/039463201002300106. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Survival curve and body weight of M. bovis BCG infected mice. (A) Long-term survival of mice infected with living M. bovis BCG Pasteur (107). (B) Body weight change after M. bovis BCG infection (n = 4–5 mice per group). Data from one representative experiment are shown. (C and D) CFU at 4 weeks after infection with 107 CFU of M. bovis BCG Connaught were determined in lungs (C) and liver (D). Data are represented as individual values and horizontal bars indicate mean (n = 4–6 mice per group). Asterisks indicate statistically significant differences between wild type and indicated group (*, p<0.03).
(TIF)
Peripheral blood mononuclear cells (PBMC) were reduced in memTNFΔ1–12 KI after 1 week of M. bovis BCG infection. (A) PBMC before infection and 1 week after M. bovis BCG infection were stained with anti-Gr1 monoclonal antibody (mAb). PBMC were gated for cells with higher granularity (high side–scatter properties) to distinguish polymorphonuclear cells. Numbers indicate the mean percentages of Gr1+ polymorphonuclear cells. (B) Percentages of Gr1+ cells are shown (n = 3 mice per group) (*, p<0.04). (C) PBMC from the same group of mice before and 1 week after M. bovis BCG infection were stained with a combination of anti-CD11b and anti-Gr1 monoclonal antibodies (mAb) and were gated for cells with lower granularity (low side–scatter properties) to distinguish them from polymorphonuclear cells. (D) Percentage of cells is shown in histogram (n = 3 mice per group) (*, p<0.03).
(TIF)
Decreased number of splenic CD4+ and CD4+/TNF+ cells 4 weeks after M. bovis BCG infection. Number of CD4+ T (A) and CD4+/TNF+ T (B) cells in spleen at 4 weeks of M. bovis BCG infection were increased in memTNFΔ1–12 KI mice. Data were represented as means ± SEM of positive cell number per spleen (n = 3–4 mice per group) (*, p<0.02).
(TIF)