Abstract
Background
Individuals differ in the response to regular exercise. Whether there are people who experience adverse changes in cardiovascular and diabetes risk factors has never been addressed.
Methodology/Principal Findings
An adverse response is defined as an exercise-induced change that worsens a risk factor beyond measurement error and expected day-to-day variation. Sixty subjects were measured three times over a period of three weeks, and variation in resting systolic blood pressure (SBP) and in fasting plasma HDL-cholesterol (HDL-C), triglycerides (TG), and insulin (FI) was quantified. The technical error (TE) defined as the within-subject standard deviation derived from these measurements was computed. An adverse response for a given risk factor was defined as a change that was at least two TEs away from no change but in an adverse direction. Thus an adverse response was recorded if an increase reached 10 mm Hg or more for SBP, 0.42 mmol/L or more for TG, or 24 pmol/L or more for FI or if a decrease reached 0.12 mmol/L or more for HDL-C. Completers from six exercise studies were used in the present analysis: Whites (N = 473) and Blacks (N = 250) from the HERITAGE Family Study; Whites and Blacks from DREW (N = 326), from INFLAME (N = 70), and from STRRIDE (N = 303); and Whites from a University of Maryland cohort (N = 160) and from a University of Jyvaskyla study (N = 105), for a total of 1,687 men and women. Using the above definitions, 126 subjects (8.4%) had an adverse change in FI. Numbers of adverse responders reached 12.2% for SBP, 10.4% for TG, and 13.3% for HDL-C. About 7% of participants experienced adverse responses in two or more risk factors.
Conclusions/Significance
Adverse responses to regular exercise in cardiovascular and diabetes risk factors occur. Identifying the predictors of such unwarranted responses and how to prevent them will provide the foundation for personalized exercise prescription.
Introduction
Physical activity level and cardiorespiratory fitness are strongly and inversely associated with the risk of cardiovascular-, metabolic-, and aging-related morbidities, as well as premature mortality [1]. To alleviate the health burden associated with sedentary behavior and poor fitness, public health recommendations are that adults be physically active at a moderate intensity for 150 minutes per week or at a vigorous intensity for 75 minutes per week [2].
However, there is considerable interindividual variability in the ability to improve one's cardiorespiratory fitness and cardiometabolic and diabetes risk factor profile in response to regular exercise. This clear finding of the HERITAGE Family Study has been replicated [3], [4], [5], [6]. A fundamental question is whether there are individuals who experience one or several adverse responses (ARs) in terms of exercise-induced changes in common risk factors. This issue is addressed herein based on data from six exercise intervention studies, with a focus on exercise-induced changes in resting systolic blood pressure (SBP), fasting insulin (FI), HDL-cholesterol (HDL-C), and triglycerides (TG). The studies used for this purpose are: HERITAGE Family Study (HERITAGE), DREW, INFLAME, STRRIDE, University of Maryland Gene Exercise Research Study (MARYLAND), and University of Jyväskylä study (JYVASKYLA).
Methods
Data on a maximum of 1687 adults from six studies were available for analysis. These studies will be briefly described, followed by the definition of AR and the statistical procedures employed. More information on each study is available in Information S1.
HERITAGE (Health, Risk Factors, Exercise Training And Genetics) Family Study
The sample, study design, and exercise training protocol of HERITAGE have been described elsewhere [7]. Briefly, 473 adults from 99 families of Caucasian descent and 250 Blacks from 105 families or sibships completed the 20-week endurance training program. Parents were 65 years of age or less while offspring ranged in age from 17 to 41 years.
Dose Response to Exercise in Women (DREW) Study
A complete description of the DREW design and methods and details of the study participants have been published [8]. In brief, it was a randomized, dose-response exercise trial with sedentary, high-normal blood pressure, postmenopausal, overweight or obese women (N = 326: 63% White) assigned to either a nonexercise control group or to endurance exercise groups that expended 4, 8, or 12 kcal/kg of body weight per week for a period of 6 months [6].
Inflammation and Exercise (INFLAME) Study
Sedentary men and women between the ages of 30 and 75 years who had an elevated plasma C-reactive protein (CRP) concentration (≥2.0 mg/L but <10.0 mg/L) were randomized to an endurance exercise or a control group [9]. Completers (70% Whites) exercised a mean of 204 minutes per week.
Studies of a Targeted Risk Reduction Intervention through Defined Exercise (STRRIDE)
STRRIDE (84% Whites) includes two complementary studies [10], [11]. STRRIDE was composed of 40- to 65-year-old, sedentary, overweight or class 1 obese (BMI 25–35 kg/m2), dyslipidemic men and women. They were assigned to one of three aerobic exercise groups and exercised for 6 months. The STRRIDE aerobic training versus resistance training (AT/RT) cohort was very similar to STRRIDE, but only those who were enrolled in endurance exercise programs are included in the present report.
University of Maryland Gene Exercise Research Study (MARYLAND)
Briefly, 160 men and women (100% Whites) ages 50 to 75 years who were sedentary, nondiabetic, and nonsmoking, with no prior history of cardiovascular disease but with one National Cholesterol Education Program lipid abnormality or blood pressure in the prehypertensive range, exercised three times per week for a period of 6 months [12].
University of Jyväskylä Study (JYVASKYLA)
Healthy, sedentary 40- to 67-year-old men and women were recruited [13]. A total of 206 subjects were randomized to one of four groups. Here we used the data on 25 men and 26 women of the endurance training group and on 30 men and 24 women (all Whites) of the combined endurance and strength training group who exercised for 21 weeks.
Definition of adverse responses
For the four traits studied, some subjects experienced changes in an opposite, unfavorable direction compared to the expected beneficial effects. This is analogous to an AR pattern. Defining an AR for any given risk factor is a challenge. A robust definition takes into account the measurement error of the trait, including the variance among laboratories or laboratory technicians, and the normal day-to-day biological variation of the trait. The parameter that captures the totality of these sources of variance in a trait is known as the technical error (TE), defined as the within-subject standard deviation as derived from repeated measures (or assays) over a given period of time, as used in the National Health and Nutrition Examination Survey (NHANES) [14]. An ancillary study designed to quantify TE for several biological traits was undertaken in HERITAGE. Sixty subjects were measured three times (except for FI) over a period of 3 weeks for each trait [15], [16], [17], [18], [19]. TEs and other useful indicators of reproducibility are shown in Table 1. In the case of FI, the assays were performed only twice, and we used other HERITAGE data plus observations from the literature to develop an estimate of TE for FI (Information S1). Here, we have conservatively defined an AR as a response beyond 2×TE in a direction indicating a worsening of the risk factor. For the four traits in the present study, twice the value of TE would mean that ARs would be reached if the exercise training-induced increases are ≥10 mm Hg for SBP, ≥0.42 mmol/L for plasma TG, and ≥24 pmol/L for plasma FI or if there is a decrease of ≤0.12 mmol/L for HDL-C. These AR definitions are used in the remainder of this report.
Table 1. Reproducibility of Risk Factors from Measurements Repeated Over 3 Days on 60 Subjects.
| Variable | Mean ± SD (at first test) | CV | ICC | TE |
| Stature, cm | 171.7±8.3 | 0.2 | 1.00 | 0.3 |
| Body weight, kg | 71.5±12.8 | 0.9 | 1.00 | 0.7 |
| Fasting insulin*, pmol/L | 65.8±40.0 | 19–29 | 0.78–0.94 | 13.2–19.8 (12) |
| HDL-C, mmol/L | 1.08±0.25 | 6.0 | 0.94 | 0.06 |
| Triglycerides, mmol/L | 1.04±0.47 | 21.8 | 0.79 | 0.21 |
| Systolic BP, mm Hg | 118.7±10.3 | 4.1 | 0.76 | 4.9 |
ICC = intraclass correlation computed from the within-subject variance compared to the overall measurement variance.
TE = technical error defined by the within-subject standard deviation calculated from repeated measurements. It includes a combination of measurement error plus day-to-day variation.
CV = Coefficients of variation is expressed as a percentage and is derived from the technical error and the measurement mean.
Note on insulin: The values reported here are from the repeated measurements obtained at baseline (N = 779) and after (N = 624) the exercise program in HERITAGE (Information S1). The TE used for this report is shown in parentheses.
To convert pmol/L of insulin to mU/L, divide by 6.945. To convert mmol/L of HDL-C to mg/dL, divide by 0.02586. To convert mmol/L of triglycerides to mg/dl, divide by 0.01129.
Statistical procedures
Data are expressed as means and standard deviations or standard errors as specified. Intraclass correlations were computed from the within-subject variance relative to the overall measurement variance. The coefficient of variation is expressed as a percentage and is derived from the TE relative to the measurement mean. The significance of the gains in VO2max and of the mean changes in the four targeted risk factors within each cohort was assessed with paired t tests. The comparisons of VO2max gains between adverse responders and non-adverse responders for each risk factor trait for each study was undertaken as follows: The difference between the changes in VO2max with exercise training expressed in ml O2 per minute was tested with the general linear model and is reported as least squares (LS) means with age, sex, and baseline VO2max as covariates. The gain in VO2max % is reported as LS means with age and sex as covariates.
Results
Subjects in DREW, INFLAME, STRRIDE, MARYLAND, and JYVASKYLA were about 20 years older than HERITAGE Whites and Blacks (Table 2). All cohorts had a mean BMI in the overweight range (i.e., >25.0 but <30.0 kg/m2), with the exception of DREW and INFLAME, with mean values of about 31 kg/m2. Mean baseline VO2max was considerably lower in DREW and INFLAME compared to the other studies. The mean increase in VO2max (ml O2 per minute) ranged from 108 (DREW) to 395 (HERITAGE Whites). The percent increase of VO2max ranged from 8.7% (DREW) to 18.9% (HERITAGE Blacks).
Table 2. Descriptive Data, Including Baseline  O2max and its Response to Training, for the Six Cohorts.
O2max and its Response to Training, for the Six Cohorts.
| HERITAGE Whites | HERITAGE Blacks | DREW | INFLAME | STRRIDE | MARYLAND | JYVASKYLA | |
| Maximum number of subjects | 473 | 250 | 326 | 70 | 303 | 160 | 105 |
| Age, yrs | 35.8 (14.5) | 33.6 (11.5) | 57.9 (6.5) | 51.2 (10) | 51.0 (7.7) | 58.0 (5.8) | 53.5 (7.6) |
| Baseline BMI, kg/m2 | 25.8 (4.9) | 27.8 (5.8) | 31.5 (3.9) | 31.1 (4.3) | 29.9 (2.9) | 28.3 (4.6) | 25.4 (3.1) |
Baseline O2max, mL/min O2max, mL/min |
2458 (740) | 2086 (629) | 1312 (240) | 1629 (567) | 2466 (694) | 2060 (536) | 2262 (616) |
Baseline O2max, mL/kg/min O2max, mL/kg/min |
33.2 (8.9) | 27.3 (7.3) | 15.8 (2.5) | 19.0 (5.6) | 28.2 (6.0) | 25.3 (4.6) | 29.8 (6.2) |
 O2max response, mL/min O2max response, mL/min |
395 (215) | 362 (171) | 108 (132) | 204 (213) | 281 (273) | 250 (228) | 259 (223) |
 O2max response, % O2max response, % |
16.9 (9.0) | 18.9 (10.3) | 8.7 (10.5) | 14.1 (13.5) | 12.0 (12.0) | 12.3 (10.1) | 13.0 (11.7) |
Values are given as mean (SD).  O2max response = post-training
O2max response = post-training  O2max minus baseline
O2max minus baseline  O2max (positive value represents improvement in
O2max (positive value represents improvement in  O2max).
O2max).
All gains in VO2max are significant at p<0.05.
Baseline values and the mean (±SD) changes of the risk factors in response to exercise programs are shown in Table 3 for each cohort. There was a wide range of baseline values for all risk factors. For instance, mean baseline HDL-C levels ranged from 1.04 mmol/L (HERITAGE Whites) to about 1.50 mmol/L (INFLAME and all DREW exercise groups). The mean changes induced by the exercise programs were generally in the expected direction (i.e., decreases in FI, TG, and SBP and increases in HDL-C). There were, however, some statistically nonsignificant exceptions to these general trends.
Table 3. Baseline and training-induced changes in the four risk factors for the five cohorts (mean ± SD).
| HERITAGE | DREW | INFLAME | STRRIDE | Maryland | Jyvaskyla | ||||
| Variable | Whites (n≤473) | Blacks (n≤250) | 4 kcal/kg/wk (n≤143) | 8 kcal/kg/wk (n≤89) | 12 kcal/kg/wk (n≤94) | (n≤70) | (n≤303) | (n≤160) | (n≤105) |
| Baseline fasting insulin, pmol/L | 65.7±40.0 | 79.7±63.2 | 74±41.24 | 75.85±42.34 | 70.93±41.08 | 82.30±40.77 | −65.3±41.8 | 83±31 | 31.6±16.7 |
| Change in fasting insulin, pmol/L | −5.2±24.9††† | −10.8±44.6††† | −2.02±31.06 | −7.98±27.59† | −1.95±29.54 | −5.58±31.33 | −11.6±29.1††† | −11±21††† | −3.2±14.0 |
| Baseline HDL-C, mmol/L | 1.04±0.26 | 1.09±0.32 | 1.50±0.38 | 1.49±0.40 | 1.50±0.35 | 1.50±0.39 | 1.17±0.35 | 1.24±0.41 | 1.28±0.40 |
| Change in HDL-C, mmol/L | 0.04±0.12††† | 0.03±0.13††† | −0.01±0.21 | −0.01±0.21 | −0.04±0.20 | −0.05±0.14†† | 0.04±0.16 | 0.08±0.21††† | 0.01±0.21 |
| Baseline Tg, mmol/L | 1.38±0.78 | 1.04±0.62 | 1.45±0.67 | 1.47±0.68 | 1.44±0.81 | 1.28±0.56 | 1.72±0.89 | 1.67±1.08 | 1.19±0.71 |
| Change in Tg, mmol/L | −0.02±0.42 | −0.03±0.41 | −0.08±0.47 | −0.02±0.50 | 0.03±0.56 | 0.00±0.46 | −0.24±0.64†† | −0.21±0.74††† | −0.11±0.54† |
| Baseline SBP, mm Hg | 116.2±10.9 | 122.8±12.0 | 138.9±13.4 | 139.9±13.6 | 138.5±12.7† | 131.3±20.4 | N/A | 133 + 16 | 131.7±15.6 |
| Change in SBP, mm Hg | 0.2±6.2 | −1.2±7.8† | 1±12.7 | −1.6±15.1 | −3.1±11.8 | −4.3±13.8† | N/A | 1 + 13 | −3.7±10.9†† |
p≤0.05.
p<0.01.
p<0.001 indicates significant change score within a group.
To convert pmol/L of insulin to mU/L, divide by 6.945. To convert mmol/L of HDL-C to mg/dL, divide by 0.02586. To convert mmol/L of triglycerides to mg/dl, divide by 0.01129.
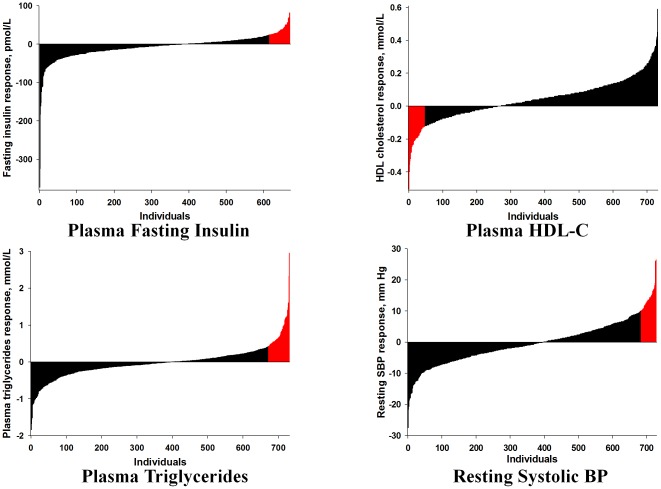
Using the definitions outlined in Table 1, the prevalence of ARs for the four risk factors was first explored in the 473 Whites and 250 Blacks of HERITAGE who were all exposed to the same standardized exercise programs and were all qualified as completers. The results are depicted in Figure 1 and are summarized in Table 4. Although HERITAGE subjects were apparently healthy and not taking medication for blood pressure, glucose, or lipid anomalies and were exposed to the same exercise program, 6% to 9% of Blacks and Whites experienced ARs for each of the four risk factors, with no substantive differences between the two ethnic groups.
Figure 1. Distribution of the response to the HERITAGE exercise program with adverse responders highlighted in red.
To convert pmol/L of insulin to mU/L, divide by 6.945. To convert mmol/L of HDL-C to mg/dL, divide by 0.02586. To convert mmol/L of triglycerides to mg/dl, divide by 0.01129.
Table 4. Prevalence of Adverse Responders in HERITAGE.
| HERITAGE Whites (≤473) | HERITAGE Blacks (≤250) | ||||
| Risk factor | 2×TE | N | % | N | % |
| Δ Fasting insulin | N≥24 pmol/L | 38 | 9 | 17 | 9 |
| Δ HDL-C | N≤0.12 mmol/L | 28 | 6 | 19 | 8 |
| Δ Triglycerides | N≥0.42 mmol/L | 37 | 8 | 19 | 8 |
| Δ Systolic BP | N≥10 mm Hg | 28 | 6 | 16 | 7 |
To convert pmol/L of insulin to mU/L, divide by 6.945. To convert mmol/L of HDL-C to mg/dL, divide by 0.02586. To convert mmol/L of triglycerides to mg/dl, divide by 0.01129.
To gain a better understanding of the true prevalence of ARs for each risk factor, we compared the data obtained in HERITAGE with those of five other exercise training studies. The results are summarized in Table 5. It is quite obvious that the findings in HERITAGE are not unique to the HERITAGE subjects and exercise protocol. Based on a maximum of 1687 subjects, the prevalence of an AR reached 8.3% for the changes in FI, 13.3% for the changes in fasting HDL-C, 10.3% for TG, and 12.2% for resting SBP. The percentages of adverse responders for each trait for each study are depicted in Figure 2. It is remarkable that such cases were found in each study, even though the age and health status of the subjects were widely divergent and the exercise programs were quite heterogeneous.
Table 5. Prevalence of Adverse Responders to Regular Exercise in Six Studies.
| HERITAGE | DREW | INFLAME | STRRIDE | MARYLAND | JYVASKYLA | TOTAL | %* | |
| N subjects | ≤723 | ≤326 | ≤70 | ≤303 | ≤160 | ≤105 | ≤1687 | |
| Δ Fasting insulin | 55 | 36 | 12 | 17 | 4 | 2 | 126 | 8.3 |
| Δ HDL-C | 47 | 87 | 21 | 32 | 8 | 27 | 222 | 13.3 |
| Δ Triglycerides | 56 | 51 | 9 | 34 | 11 | 11 | 172 | 10.3 |
| Δ Systolic BP | 44 | 58 | 11 | NA | 43 | 10 | 166 | 12.2 |
% represents the proportion of adverse responders in relation to the total number of subjects exercise trained for each of the four traits.
Figure 2. Percentages of adverse responders for each risk factor trait by study, with number of adverse responder subjects in each bar.
One important question to consider is whether those who respond adversely for a given risk factor are also those who experience the least improvement in cardiorespiratory fitness with regular exercise. This question was addressed by comparing the gains in VO2max between the subgroups of adverse responders and non-adverse responders for a given risk factor. The results of these analyses are shown in Table 6 for the gains in ml O2 per minute and the percentage increases in VO2max. A total of 56 differences were tested with age, sex, and baseline VO2max as covariates for the gain in ml O2 per minute and age and sex for the percentage increase. Only two such differences reached the 0.05 level of significance, and they were far from reaching a multiple test Bonferroni adjusted P value of 0.0009. These data indicate that AR traits are independent of the improvement in cardiorespiratory fitness.
Table 6. Comparison of the VO2max response to regular exercise between adverse responders and non-adverse responders for each response trait in each study.
| HERITAGE Whites | HERITAGE Blacks | DREW | INFLAME | |||||
| Adverse responders | Non-adverse responders | Adverse responders | Non-adverse responders | Adverse responders | Non-adverse responders | Adverse responders | Non-adverse responders | |
| Δ Fasting insulin | ||||||||
| N subjects | 38 | 411 | 17 | 184 | 36 | 290 | 12 | 58 |
| Δ VO2max (ml/min) | 382 (34) | 399 (10) | 472 (43) | 385 (14) | 76 (22) | 69 (7) | 99 (61) | 226 (28) |
| Δ VO2max (%) | 16.1 (1.4) | 17.0 (0.4) | 20.6 (2.5) | 18.3 (0.8) | 6.0 (1.7) | 5.8 (0.6) | 8.0 (3.4) | 14.5 (1.6) |
| Δ HDL-C | ||||||||
| N subjects | 28 | 443 | 19 | 220 | 87 | 239 | 21 | 49 |
| Δ VO2max (ml/min) | 384 (40) | 400 (10) | 348 (39) | 388 (12) | 68 (14) | 71(8) | 219 (48) | 196 (32) |
| Δ VO2max (%) | 16.2 (1.7) | 17.0 (0.4) | 15.5 (2.3) | 18.4 (0.7) | 5.4 (1.1) | 6.0 (0.7) | 14.2 (2.7) | 12.9 (1.8) |
| Δ Triglycerides | ||||||||
| N subjects | 37 | 434 | 19 | 220 | 51 | 275 | 9 | 61 |
| Δ VO2max (ml/min) | 424 (34) | 397 (10) | 332 (39) | 392 (13) | 72 (18) | 70 (8) | 136 (72) | 213 (28) |
| Δ VO2max (%) | 17.7 (1.4) | 16.9 (0.4) | 16.9 (2.3) | 18.3 (0.7) | 6.1 (1.5) | 5.8 (0.6) | 8.6 (4.0) | 14.0 (1.6) |
| Δ Systolic BP | ||||||||
| N subjects | 28 | 442 | 16 | 220 | 58 | 268 | 11 | 59 |
| Δ VO2max (ml/min) | 348 (40) | 401 (10) | 396 (42) | 386 (12) | 60 (17) | 72 (8) | 140 (65) | 215 (28) |
| Δ VO2max (%) | 14.8 (1.7) | 17.0 (0.4) | 16.7 (2.5) | 18.2 (0.7) | 4.9 (1.4) | 6.1 (0.6) | 7.5 (3.6) | 14.4 (1.6) |
Data expressed as means and standard deviations.
Δ VO2max expressed as the change with exercise training in ml O2 per minute, reported as LS means with age, sex, and baseline VO2max as covariates. Δ VO2max % reported as LS means with age and sex as covariates.
p≤0.05 indicates significant difference in VO2max training response between adverse responders and non-adverse responders.
One could hypothesize that the proportion of ARs should decrease as the amount of exercise increases. We tested this hypothesis with the data of DREW, and the results are summarized in Table 7. No substantive differences were observed in the prevalence of ARs among the three levels of exercise energy expenditure, which ranged from 4 to 12 kcal/kg of body weight per week.
Table 7. Adverse and Excellent Responders to Regular Exercise in DREW*.
| DREW4 kcal/kg/wk | DREW8 kcal/kg/wk | DREW12 kcal/kg/wk | |||||
| N subjects | 143 | 89 | 94 | ||||
| ADVERSE RESPONDERS | N | % | N | % | N | % | |
| Δ Fasting insulin | N≥24 pmol/L | 16 | 11 | 9 | 10 | 11 | 12 |
| Δ HDL-C | N≤0.12 mmol/L | 35 | 25 | 21 | 24 | 31 | 33 |
| Δ Triglycerides | N≥0.42 mmol/L | 19 | 13 | 14 | 16 | 18 | 19 |
| Δ SBP | N≥10 mm Hg | 32 | 22 | 14 | 16 | 12 | |
A postmenopausal woman who follows the 2008 Physical Activity Guidelines for Americans expends about 8 kcal/kg/week in her exercise program. The 4 kcal/kg/week is about 50% the current recommendation whereas the 12 kcal/kg/week is about 50% above the recommended dose.
Another important question is that of the proportion of subjects who experienced ARs for more than one risk factor. We tabulated the number of participants in the six studies who registered ARs for two or more risk factors, and the results are shown in Table 8. Approximately 7% of sedentary adults experienced ARs for at least two common cardiometabolic and diabetes risk factors following exposure to regular exercise. Only a small minority of participants (<1%) exhibited ARs for three or more traits.
Table 8. Percentage of Subjects in Each Study with 1, 2, or 3 and More Adverse Responses.
| 1 Adverse Response | 2 Adverse Responses | 3 or 4 Adverse Responses | ||||
| N | % | N | % | N | % | |
| HERITAGE | ||||||
| Blacks | 51 | 20% | 11 | 4% | 0 | 0% |
| Whites | 94 | 20% | 17 | 4% | 3 | 1% |
| DREW | 131 | 40% | 37 | 11% | 9 | 3% |
| INFLAME | 32 | 46% | 9 | 13% | 1 | 1% |
| STRRIDE | 71 | 24% | 9 | 3% | 0 | 0% |
| MARYLAND | 54 | 34% | 5 | 3% | 0 | 0% |
| JYVASKYLA | 35 | 33% | 7 | 7% | 0 | 0% |
| TOTALS (mean %) | 468 | 31% | 95 | 6% | 13 | 0.8% |
The four traits considered were the exercise training-induced changes in fasting insulin, HDL-cholesterol, triglycerides, and resting systolic blood pressure.
Discussion
The prevalence of ARs for select risk factors varied from 8.3% for the exercise training-induced changes in FI to 13.3% for the changes in HDL-C, with about 7% of participants experiencing adverse changes in two or more risk factors. This subgroup should receive urgent attention. The prevalence of ARs appears to be similar at low and high doses of exercise. However, we do not know whether some adverse responders would revert to a more positive response pattern if exposed to different exercise doses or exercise modalities.
It is important to differentiate between ARs for risk factors for common chronic diseases, as referred to in the present study, from other more acute ARs such as cardiac events related to exertion during an exercise bout [20], [21], [22], sudden cardiac death during or immediately after exercise typically associated with a cardiomyopathy or a congenital abnormality [23], or even exercise intolerance due to abnormal skeletal muscle energy metabolism [24]. These events are fortunately rare among physically active people. In contrast, ARs as defined herein for common cardiometabolic and diabetes risk factors are much more prevalent and become evident with exposure to regular exercise. It is not known whether such ARs can be detected after a single or a few bouts of exercise.
Even though the presence of ARs was first detected among completers in Blacks and Whites of the HERITAGE Family Study, in which subjects were confirmed to be sedentary at baseline, with a rather healthy profile, the phenomenon was confirmed in five other exercise intervention studies. The consistency in the prevalence of ARs across heterogeneous studies in terms of health status of subjects at baseline and of exercise training regimen is notable.
One question that may arise is whether ARs are the result of unwarranted exercise-drug interaction effects. The question cannot be answered with direct experimental data at the moment, but based on our analysis of the results of the six studies, it is highly unlikely that it is the case. For instance, HERITAGE and JYVASKYLA subjects were healthy adults taking no medication for high blood pressure, hypercholesterolemia, or hyperglycemia. However, many subjects in DREW, INFLAME, MARYLAND, and STRRIDE were taking medications for high blood pressure, hyperglycemia, or dyslipoproteinemia. Yet substantial numbers of subjects with or without medication in these cohorts experienced one or more ARs.
The challenge is now to investigate whether baseline predictors of ARs can be identified to screen individuals at risk so that they can be offered alternative approaches to modifying cardiometabolic risk factors. Research based on HERITAGE has amply demonstrated that the response pattern to exercise training aggregates in families [25], [26], [27], 28. In fact, the heritability of the changes induced by the exercise program reached about 30% for plasma HDL-C and TG [26] and about 20% to 25% for indicators of insulin metabolism and resting SBP [29], [30]. There are strong indications from a baseline skeletal muscle gene expression profile and from a genome-wide association study performed on the Whites of HERITAGE that the genetic component of a response trait can be defined in terms of RNA abundance observed in the sedentary state or by specific genomic variants [31], [32], [33]. This suggests that it may be possible with further research to identify molecular predictors of the inability to benefit from regular exercise and of adverse changes in specific cardiometabolic and diabetes risk factors.
In summary, we did not find any evidence for differences in the prevalence of ARs between Blacks and Whites or between men and women. Moreover, the AR traits are not explained by prior health status of subjects, age, amount of exercise imposed by the program, or lack of improvement in cardiorespiratory fitness. No evidence could be found for the hypothesis that ARs were the result of drug-exercise interactions. Thus, some individuals experience ARs when exposed to regular exercise, but the causes of the phenomenon are unknown at this time. The observations reported herein need to be extended to other cardiometabolic and diabetes risk factors such as LDL-cholesterol, small, dense LDL particles, markers of low-grade inflammation, adiposity traits, and ectopic fat depots. We conclude that it is critical to search for potential physiological and molecular predictors so that individuals at risk for adverse response patterns can be identified and offered proper guidance in an exercise medicine preventive or therapeutic context.
Supporting Information
Detailed description of the six studies and the background material used to determine the technical error for fasting insulin.
(DOCX)
Acknowledgments
The contribution of Dr. Jack Wilmore, Professor Emeritus, University of Texas at Austin, to the HERITAGE Family Study is gratefully acknowledged. The authors would also like to express their gratitude to Allison Templet for her numerous contributions to the development of this manuscript.
Footnotes
Competing Interests: C. Bouchard is a member of the Science Advisory Board of Pathway Genomics. This does not alter the authors' adherence to all the PLoS ONE policies on sharing data and materials.
Funding: Studies used for this report were supported by multiple grants from the National Institutes of Health (NIH): HL-45670, HL-47323, HL-47317, HL-47327, HL-47321, HL-66262, HL-57354, AG-17474, and AG-15389. C. Bouchard is partially supported by the John W. Barton, Sr. Chair in Genetics and Nutrition. T. Church is partially supported by the John S. McIlhenny Chair in Health Wisdom. N.T. Jenkins was supported by NIH T32 AG00068 and NIH T32 AR048523. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee report, 2008. Washington, DC: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- 2.U.S. Department of Health and Human Services. 2008 activity guidelines for Americans. Washington, DC: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- 3.Bouchard C, Rankinen T. Individual differences in response to regular physical activity. Med Sci Sports Exerc. 2001;33:S446–S451. doi: 10.1097/00005768-200106001-00013. [DOI] [PubMed] [Google Scholar]
- 4.Boule NG, Weisnagel SJ, Lakka TA, Tremblay A, Bergman RN, et al. Effects of exercise training on glucose homeostasis: The HERITAGE Family Study. Diabetes Care. 2005;28:108–114. doi: 10.2337/diacare.28.1.108. [DOI] [PubMed] [Google Scholar]
- 5.Leon AS, Gaskill SE, Rice T, Bergeron J, Gagnon J, et al. Variability in the response of HDL cholesterol to exercise training in the HERITAGE Family Study. Int J Sports Med. 2002;23:1–9. doi: 10.1055/s-2002-19270. [DOI] [PubMed] [Google Scholar]
- 6.Church TS, Earnest CP, Skinner JS, Blair SN. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure: a randomized controlled trial. JAMA. 2007;297:2081–2091. doi: 10.1001/jama.297.19.2081. [DOI] [PubMed] [Google Scholar]
- 7.Bouchard C, Leon AS, Rao DC, Skinner JS, Wilmore JH, et al. The HERITAGE family study. Aims, design, and measurement protocol. Med Sci Sports Exerc. 1995;27:721–729. [PubMed] [Google Scholar]
- 8.Morss GM, Jordan AN, Skinner JS, Dunn AL, Church TS, et al. Dose Response to Exercise in Women aged 45–75 yr (DREW): Design and rationale. Med Sci Sports Exerc. 2004;36:336–344. doi: 10.1249/01.MSS.0000113738.06267.E5. [DOI] [PubMed] [Google Scholar]
- 9.Thompson AM, Mikus CR, Rodarte RQ, Distefano B, Priest EL, et al. Inflammation and exercise (INFLAME): study rationale, design, and methods. Contemp Clin Trials. 2008;29:418–427. doi: 10.1016/j.cct.2007.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kraus WE, Torgan CE, Duscha BD, Norris J, Brown SA, et al. Studies of a targeted risk reduction intervention through defined exercise (STRRIDE). Med Sci Sports Exerc. 2001;33:1774–1784. doi: 10.1097/00005768-200110000-00025. [DOI] [PubMed] [Google Scholar]
- 11.Bateman LA, Slentz CA, Willis LH, Shields AT, Piner LW, et al. Comparison of aerobic versus resistance exercise training effects on metabolic syndrome (from the Studies of a Targeted Risk Reduction Intervention Through Defined Exercise - STRRIDE-AT/RT). Am J Cardiol. 2011;108:838–844. doi: 10.1016/j.amjcard.2011.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilund KR, Colvin PL, Phares D, Goldberg AP, Hagberg JM. The effect of endurance exercise training on plasma lipoprotein AI and lipoprotein AI:AII concentrations in sedentary adults. Metabolism. 2002;51:1053–1060. doi: 10.1053/meta.2002.33356. [DOI] [PubMed] [Google Scholar]
- 13.Karavirta L, Hakkinen K, Kauhanen A, Arija-Blazquez A, Sillanpaa E, et al. Individual responses to combined endurance and strength training in older adults. Med Sci Sports Exerc. 2011;43:484–490. doi: 10.1249/MSS.0b013e3181f1bf0d. [DOI] [PubMed] [Google Scholar]
- 14.Malina RM, Hamill PVV, Lemeshow S. Selected body measurements of children 6–11 years. Rockville, MD: National Center for Health Statistics. (DHEW publication no. (HSM) 73-1605.) (DHEW publication no. (HSM) 73-1605.); 1973. [Google Scholar]
- 15.Gagnon J, Province MA, Bouchard C, Leon AS, Skinner JS, et al. The HERITAGE Family Study: Quality assurance and quality control. Ann Epidemiol. 1996;6:520–529. doi: 10.1016/s1047-2797(96)00068-3. [DOI] [PubMed] [Google Scholar]
- 16.Wilmore JH, Stanforth PR, Domenick MA, Gagnon J, Daw EW, et al. Reproducibility of anthropometric and body composition measurements: the HERITAGE Family Study1. Int J Obes Relat Metab Disord. 1997;21:297–303. doi: 10.1038/sj.ijo.0800404. [DOI] [PubMed] [Google Scholar]
- 17.Wilmore JH, Stanforth PR, Turley KR, Gagnon J, Daw EW, et al. Reproducibility of cardiovascular, respiratory, and metabolic responses to submaximal exercise: the HERITAGE Family Study. Med Sci Sports Exerc. 1998;30:259–265. doi: 10.1097/00005768-199802000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Despres JP, Gagnon J, Bergeron J, Couillard C, Leon AS, et al. Plasma post-heparin lipase activities in the HERITAGE Family Study: the reproducibility, gender differences, and associations with lipoprotein levels. HEalth, RIsk factors, exercise Training and GEnetics. Clin Biochem. 1999;32:157–165. doi: 10.1016/s0009-9120(98)00106-4. [DOI] [PubMed] [Google Scholar]
- 19.Skinner JS, Wilmore KM, Jaskolska A, Jaskolski A, Daw EW, et al. Reproducibility of maximal exercise test data in the HERITAGE family study. Med Sci Sports Exerc. 1999;31:1623–1628. doi: 10.1097/00005768-199911000-00020. [DOI] [PubMed] [Google Scholar]
- 20.Siscovick DS, Weiss NS, Fletcher RH, Lasky T. The incidence of primary cardiac arrest during vigorous exercise. N Engl J Med. 1984;311:874–877. doi: 10.1056/NEJM198410043111402. [DOI] [PubMed] [Google Scholar]
- 21.Thompson PD, Mitchell JH. Exercise and sudden cardiac death: protection or provocation. N Engl J Med. 1984;311:914–915. doi: 10.1056/NEJM198410043111410. [DOI] [PubMed] [Google Scholar]
- 22.Kim JH, Malhotra R, Chiampas G, d'Hemecourt P, Troyanos C, et al. Cardiac arrest during long-distance running races. N Engl J Med. 2012;366:130–140. doi: 10.1056/NEJMoa1106468. [DOI] [PubMed] [Google Scholar]
- 23.Thompson PD. Athletes, athletics, and sudden cardiac death. Med Sci Sports Exerc. 1993;25:981–984. [PubMed] [Google Scholar]
- 24.Rankinen T, Perusse L, Rauramaa R, Rivera MA, Wolfarth B, et al. The human gene map for performance and health-related fitness phenotypes: the 2001 update. Med Sci Sports Exerc. 2002;34:1219–1233. doi: 10.1097/00005768-200208000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Bouchard C, An P, Rice T, Skinner JS, Wilmore JH, et al. Familial aggregation of VO(2max) response to exercise training: results from the HERITAGE Family Study. J Appl Physiol. 1999;87:1003–1008. doi: 10.1152/jappl.1999.87.3.1003. [DOI] [PubMed] [Google Scholar]
- 26.Rice T, Despres JP, Perusse L, Hong Y, Province MA, et al. Familial aggregation of blood lipid response to exercise training in the health, risk factors, exercise training, and genetics (HERITAGE) Family Study. Circulation. 2002;105:1904–1908. doi: 10.1161/01.cir.0000014969.85364.9f. [DOI] [PubMed] [Google Scholar]
- 27.Katzmarzyk PT, Perusse L, Rice T, Gagnon J, Skinner JS, et al. Familial resemblance for coronary heart disease risk: the HERITAGE Family Study. Ethn Dis. 2000;10:138–147. [PubMed] [Google Scholar]
- 28.Hong Y, Rice T, Gagnon J, Perusse L, Province M, et al. Familiality of triglyceride and LPL response to exercise training: the HERITAGE study. Med Sci Sports Exerc. 2000;32:1438–1444. doi: 10.1097/00005768-200008000-00012. [DOI] [PubMed] [Google Scholar]
- 29.An P, Teran-Garcia M, Rice T, Rankinen T, Weisnagel SJ, et al. Genome-wide linkage scans for prediabetes phenotypes in response to 20 weeks of endurance exercise training in non-diabetic whites and blacks: the HERITAGE Family Study. Diabetologia. 2005;48:1142–1149. doi: 10.1007/s00125-005-1769-4. [DOI] [PubMed] [Google Scholar]
- 30.Rice T, An P, Gagnon J, Leon AS, Skinner JS, et al. Heritability of HR and BP response to exercise training in the HERITAGE Family Study. Med Sci Sports Exerc. 2002;34:972–979. doi: 10.1097/00005768-200206000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Bouchard C, Sarzynski MA, Rice TK, Kraus WE, Church TS, et al. Genomic predictors of the maximal O uptake response to standardized exercise training programs. J Appl Physiol. 2011;110:1160–1170. doi: 10.1152/japplphysiol.00973.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Timmons JA, Knudsen S, Rankinen T, Koch LG, Sarzynski M, et al. Using molecular classification to predict gains in maximal aerobic capacity following endurance exercise training in humans. J Appl Physiol. 2010;108:1487–1496. doi: 10.1152/japplphysiol.01295.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rankinen T, Sung YJ, Sarzynski MA, Rice TK, Rao DC, et al. The heritability of submaximal exercise heart rate response to exercise training is accounted for by nine SNPs. J Appl Physiol. 2012;112:892–897. doi: 10.1152/japplphysiol.01287.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Detailed description of the six studies and the background material used to determine the technical error for fasting insulin.
(DOCX)