Abstract
Background
Registering complications is important in surgery, since complications serve as outcome measures and indicators of quality of care. Few studies have addressed the variation in severity and consequences of complications. We hypothesized that complications show much variation in consequences and severity.
Methods
We conducted a prospective observational cohort study to evaluate consequences and severity of complications in surgical practice. All recorded complications of patients admitted to our hospital between June 1, 2005, and Dec. 31, 2007, were prospectively recorded in an electronic database. Complications were classified according to the system of the Trauma Registry of the American College of Surgeons. We graded the severity of complications according to the system proposed by Clavien and colleagues, and the consequences of each complication were registered.
Results
During the study period, 3418 complications were recorded; consequences and severity were recorded in 89% of them. Of 3026 complications, 987 (33%) were grade I, 781 (26%) were grade IIa, 1020 (34%) were grade IIb, 150 (5%) were grade III and 88 (3%) were grade IV. The consequences and severity of identically registered complications showed a large degree of variation, best illustrated by wound infections, which were grade I in 50%, grade IIa in 22%, grade IIb in 28% and grade III and IV in 0.3% of patients.
Conclusion
Severity should be routinely presented when reporting complications in clinical practice and surgical research papers to adequately compare quality of care and results of clinical trials.
Abstract
Contexte
En chirurgie, il importe de consigner les complications puisqu’elles servent de mesure des résultats et d’indicateurs de la qualité des soins. Peu d’études ont évalué les variations de la gravité et des conséquences des complications. Selon notre hypothèse, les complications ont des conséquences de nature et d’intensité très diverses.
Méthodes
Nous avons effectué une étude de cohorte d’observation prospective afin de mesurer les conséquences et la gravité des complications dans la pratique chirurgicale. Toutes les complications rapportées chez les patients admis dans notre hôpital entre le 1 juin 2005 et le 31 décembre 2007 ont été saisies de manière prospective dans une base de données électronique puis on les a classées dans l’une ou l’autre des catégories du Registre des traumatismes de l’American College of Surgeons. Nous en avons mesuré la gravité en nous inspirant du système proposé par Clavien et ses collaborateurs et nous avons consigné les conséquences de chaque complication.
Résultats
Au cours de la période de l’étude, 3418 complications ont été recensées; les conséquences et la gravité de 89 % d’entre elles ont été notées. Sur 3026 complications, 987 (33 %) étaient de grade I, 781 (26 %) étaient de grade IIa, 1020 (34 %) étaient de grade IIb, 150 (5 %) étaient de grade III et 88 (3 %), de grade IV. Les conséquences et la gravité des complications d’une même catégorie ont montré un fort degré de variation, comme en témoignent le plus éloquemment les infections de plaies, qui étaient de grade I dans 50 % des cas, de grade IIa dans 22 % des cas, de grade IIb dans 28 % des cas et de grade III et IV dans 0,3 % des cas.
Conclusion
Dans la pratique clinique et dans les comptes rendus de recherche, il faut indiquer la gravité des complications chirurgicales pour pouvoir effectuer une comparaison valide de la qualité des soins et des résultats des essais cliniques.
Complications in surgery are an important cause of morbidity and mortality and may result in an increased length of stay in hospital, repeat surgery, additional medical treatment, legal issues and increased costs.1–5 Apart from mortality, complications are among the most frequently measured and reported outcomes used to evaluate surgical treatment.6 They are used as an indicator of quality, and their continuous evaluation can identify possible flaws in the process of care. Although efforts are being made to improve quality of care by means of uniform registration of adverse events and mortality,7 unfortunately, in many countries, comparison of outcomes among health care providers is hampered by the lack of a clear definition of complications.8,9 Moreover, when comparing outcomes of treatment, the severity of complications is usually not taken into account; however, differences in recorded severity may reveal differences in quality of care and subsequently provide opportunities for improving quality of care.
In 1992, Clavien and colleagues10 developed a classification system that defined the severity of the complication based on the actions necessary to treat it. The system initially was not widely used, although a modified version substantially gained popularity after it was validated in a large cohort of patients and was shown to have good reproducibility among surgeons.11 Limited information on the consequences and severity of complications is found in the surgical literature. We hypothesized that the impact of comparable complications is highly variable. The aim of our study was to prospectively evaluate the severity and consequences of all complications arising in a general surgical practice and to evaluate whether identically recorded complications had predictable and consistent severity grades. From these results, we can infer whether crude complication rates can serve as indicators of quality of care and outcome measures in scientific research, or whether gradation of complications is obligatory for adequate comparison of outcomes.
Methods
We analyzed all recorded complications of patients admitted to our hospital between June 1, 2005, and Dec. 31, 2007. The registration methods and classifying systems used have been previously described in detail.12 Negative outcomes were differentiated into 3 categories: complications, sequalae and failure to cure.10 Traditionally, our hospital used the Association of Surgeons of the Netherlands definition of complication: “A complication is any state or event, unfavourable to the patient’s health, that arose during admission or 30 days after discharge that either causes unintentional injury or requires additional treatment.”13 Over the years, this definition has been broadened. Complications that arise more than 30 days after discharge are also recorded, and measurable negative effects or additional treatment are no longer absolute requirements. Thus, undesirable events without directly noticeable negative effects on the patient’s health or without need for additional treatment are recorded as well, regardless of the actual effect on the patient. These events are recorded as provider-related complications and account for up to 4% of events in our registry.13
In the present study, we classified complications according to the system of the Trauma Registry of the American College of Surgeons (TRACS). The system does not provide information about the severity of the complication. The TRACS system was originally developed as a complication list to record the morbidity in trauma patient populations.14 It explicitly defines complications and uses 4-digit codes. Although this list was developed for the trauma population, its design is broad and encompasses complications applicable to general surgery.
When an event occurs, it is immediately registered in the patient’s electronic medical record by the physician who identified the event. The complication, including its severity grade and consequences, is recorded in an electronic medical file within the patient’s record that is specially designed for registering complications. This file is operational on all computers throughout the hospital and the outpatient clinic, which makes recording easy. All complications recorded for admitted patients and patients in the emergency department and the outpatient clinic are automatically presented at the daily surgical conference and discussed by the entire surgical staff before they are definitively recorded in the database. The software used for the electronic medical record is a Microsoft Access application with an Oracle database, which was developed in our hospital.
For the purpose of this study, the severity of the complication was graded according to the system proposed in 1992 by Clavien and colleagues.10 In this system, the severity of the complication is defined by its consequences. Thus, the most severe complications are those resulting in death (grade IV). The severity of complications not resulting in death is defined by the morbidity it inflicts on the patient. Morbidity may vary from no consequences/very minor consequences (grade I), pharmacologic treatment (grade IIa), additional diagnostic or therapeutic procedures (grade IIb) or lasting disability (grade III). The classification system was designed for recording severity of complications after cholecystectomy, but is applicable to all surgical procedures.
In addition, the recording physician scored the immediate consequences of each complication qualitatively. The following consequences could be scored: readmission, complication expected to prolong hospital stay, transfer to another department or hospital, surgical reintervention, pharmacologic treatment, radiologic drainage, opening of the wound for drainage, intubation and mechanical ventilation, delay of surgery, death, other, or a combination of these consequences. A free-text description of the consequences of the complication was also recorded. Since the registration and coding of complications is known to be frequently incomplete and inconsistent,12 all complications, consequences of complications and Clavien severity grades were reviewed and the coding checked against the recorded free-text description of the complication. If incorrectly coded, the registered entries were corrected using the TRACS manual or the instructions in the paper by Clavien and colleagues.10 Documented entries that were not complications, but rather failures of therapy, negative effects of the primary disease or sequalae were identified and excluded from analysis.
Statistical analysis
Statistical analysis involved calculating frequencies and cross-tabulations, which we performed using the Statistical Package for the Social Sciences (SPSS) software version 16.0.
Results
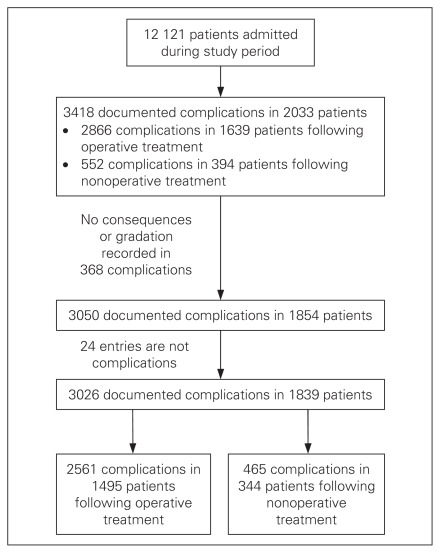
During the study period, a total of 12 121 patients were admitted to our hospital, 8384 (69%) of whom underwent a total of 15 058 surgical procedures. Of the patients who received surgery, 1639 (20%) of all patients had 1 or more complications registered, whereas 394 of 3737 (10%) who were treated nonsurgically experienced complications. We documented a total of 3418 complications in 2033 patients (17% of all admitted patients). In 368 complications, no consequences or severity grades were recorded; these were excluded from the analysis. The consequences of 3050 of 3418 (89%) complications were adequately registered. After reviewing the nature and description of all documented complications, 24 of 3050 (0.8%) events were actually either new pathology, negative effects of the primary disease or sequalae and were also excluded, leaving 3026 documented complications for analysis (Figure 1). Among admitted patients who did not undergo surgery, 465 of 552 (84%) consequences of the complication were recorded. The various types of procedures performed, and their respective complication rates are outlined in Table 1.
Fig. 1.
Summary of complications included in the analysis.
Table 1.
Complications in relation to type of surgery
| Type of surgery | No. patients | No. operative procedures | No. patients with ≥ 1 complication registered | Complication rate, % | No. complications registered | No. patients with ≥ 1 complication with severity grades and consequences registered | Complications with severity grade and consequences registered, no. (%) |
|---|---|---|---|---|---|---|---|
| Vascular | 989 | 2 188 | 280 | 13 | 515 | 243 | 444 (86) |
| Gastrointestinal | 2 212 | 4 439 | 630 | 14 | 1 252 | 583 | 1 147 (92) |
| Trauma | 1 093 | 2 101 | 231 | 11 | 347 | 215 | 312 (90) |
| Breast | 541 | 1 126 | 122 | 11 | 151 | 104 | 124 (82) |
| Thoracic | 101 | 330 | 50 | 15 | 93 | 49 | 85 (91) |
| General | 3 294 | 4 674 | 306 | 6 | 481 | 284 | 428 (89) |
| Head and neck | 154 | 200 | 20 | 10 | 27 | 17 | 21 (78) |
| Total | 8 384 | 15 058 | 1 639 | 11 | 2 866 | 1 495 | 2 561 (89) |
Table 2 illustrates the severity of complications following various types of surgery. Of all complications, 92% had no lasting effects for the patients (grade I, IIa and IIb), although one-third required major additional interventions. To compare the incidence of severe complications (grade III and grade IV), we related the number of complications to the total number of patients treated. The most severe complications occurred in patients who had vascular surgery (30 of 989 [3%] for grade III and 29 of 989 [3%] for grade IV complications), gastrointestinal surgery (59 of 2212 [3%] for grade III and 33 of 2212 [2%] for grade IV complications) and trauma surgery (24 of 1093 [2%] for grade III and 5 of 1093 [0.5%] for grade IV complications).
Table 2.
Severity of complications in relation to type of surgery
| Type of surgery | Complications; no. (%)* | Total no. complications | |||||
|---|---|---|---|---|---|---|---|
| No. patients | I | IIa | IIb | III | IV | ||
| No surgery | 3 737 | 248 (53) | 99 (21) | 95 (20) | 14 (3) | 9 (2) | 465 |
| Vascular | 989 | 107 (24) | 143 (32) | 135 (30) | 30 (7) | 29 (6) | 444 |
| Gastrointestinal | 2 212 | 324 (28) | 344 (30) | 387 (34) | 59 (5) | 33 (3) | 1 147 |
| Trauma | 1 093 | 105 (34) | 61 (20) | 117 (38) | 24 (8) | 5 (2) | 312 |
| Breast | 541 | 25 (20) | 19 (15) | 80 (64) | 0 | 0 | 124 |
| Thoracic | 101 | 25 (29) | 23 (27) | 37 (44) | 0 | 0 | 85 |
| General | 3 294 | 148 (34) | 83 (19) | 162 (38) | 23 (5) | 12 (3) | 428 |
| Head and neck | 154 | 5 (24) | 9 (43) | 7 (33) | 0 | 0 | 21 |
| Total | 12 121 | 987 (33) | 781 (26) | 1 020 (34) | 150 (5) | 88 (3) | 3 026 |
Complications graded according to Clavien and colleagues.10 The percentages reported with each severity grade represent the proportion of the total number of complications for this type of procedure.
Table 3 shows the consequences of complications with respect to different complication grades. For example, 22% of all readmissions resulted from grade I complications, 17% from grade IIa complications and 60% from grade IIb complications. The category “other” encompassed potential damage to the patient, delay of adequate treatment and additional minor procedures, such as new plaster casts, new intravenous lines and new nasogastric tubes or urinary catheters. Even grade I complications had a broad spectrum of consequences, including readmissions, increased length of stay in hospital, pharmacologic treatment (although these only included antiemetics, antipyretics, analgesics, antidiarrheal drugs and drugs required for urinary retention)10 and transfers to other departments. Although in grade III and IV complications disability and death were the ultimate consequences, the complication often had many other consequences, such as reoperations, medical treatment and mechanical ventilation.
Table 3.
Consequences of complications in relation to severity grade
| Recorded consequence | Complications; no. (%)* | Total no. complications | ||||
|---|---|---|---|---|---|---|
| I, n = 987 | IIa, n = 781 | IIb, n = 1020 | III, n = 150 | IV, n = 88 | ||
| Readmission | 72 (22) | 55 (16) | 198 (60) | 6 (2) | 1 (0.3) | 332 |
| Reoperation | 21† (2) | 0 | 823 (93) | 28 (3) | 13 (1) | 885 |
| Radiological drain | 0 | 0 | 84 (100) | 0 | 0 | 84 |
| Opening of wound abscess | 217 (89) | 26 (11) | 0 | 0 | 0 | 243 |
| Expected increased length of stay | 129 (20) | 175 (27) | 284 (43) | 49 (8) | 16 (2) | 653 |
| Pharmacological treatment | 58 (6) | 754 (74) | 138 (14) | 46 (4) | 21 (2) | 1017 |
| Intubation/mechanical ventilation | 0 | 0 | 83 (85) | 7 (7) | 8 (8) | 98 |
| Transfer to another department | 14 (8) | 75 (43) | 49 (28) | 25 (14) | 10 (6) | 173 |
| Delay of operation | 168 (85) | 15 (8) | 8 (4) | 4 (2) | 2 (1) | 197 |
| Other | 506 (88) | 24 (4) | 34 (6) | 7 (1) | 2 (0.3) | 573 |
NA = not applicable.
Complications graded according to Clavien and colleagues.10 The percentages reported with each severity grade represent the proportion of the total number of complications for this recorded consequence.
Bedside procedure.
Table 4 shows the 5 most frequent reasons for readmission for every severity grade. In grade I, most readmissions were owing to complications recorded with TRACS codes that denominate provider errors. The complications recorded with TRACS code 9003 “delay to operating room” were all cases in which an elective operation was cancelled either owing to low operating room or intensive care unit capacity or to the patient’s condition. The operation was then rescheduled and the patient readmitted on another day. The complications recorded with TRACS code 9008 “error in judgement” encompassed cases in which patients were admitted as a consequence of inadequate analgesic prescription, an erroneous therapeutic regimen or an erroneous diagnostic work-up. The complications recorded with TRACS code 9004 “delay in MD response” included a case in which a patient was admitted for an endovascular aneurysm repair for which the device was not present. The operating surgeon, although aware of this fact, failed to cancel the operation. The other 2 cases were severe hypertension that was known to the operating surgeon who did not take appropriate measures and a case in which an operating procedure was planned despite there being no operating surgeon available. The complications recorded with TRACS code 9007 ”error in diagnosis” were 3 cases in which an incorrect diagnosis (perioperatively in 2 cases) lead to a readmission. Finally, in grade IIb complications, 27 surgical technical errors, as documented with TRACS code 9009 “error in technique,” caused the patient to be readmitted; these cases included incorrectly placed vascular access ports, incorrectly performed osteosynthesis and insufficiently drained abscesses.
Table 4.
Registered complications requiring readmission
| Grade; TRACS description | No. (%)* |
|---|---|
| Grade I | 72 |
| Delay to operating room | 26(36) |
| Wound infection | 19 (26) |
| Error in judgement | 5 (7) |
| Delay in physician response | 3 (4) |
| Error in diagnosis | 3 (4) |
| Grade IIa | 55 |
| Wound infection | 20 (36) |
| Postoperative hemorrhage | 4 (7) |
| Pneumonia | 3 (5) |
| Pulmonary embolus | 3 (5) |
| Urinary tract infection | 3 (5) |
| Grade IIb | 198 |
| Wound infection | 60 (30) |
| Error in technique | 27 (14) |
| Intra-abdominal abscess | 19 (10) |
| Postoperative hemorrhage | 15 (8) |
| Loss of reduction/fixation | 9 (4) |
| Grade III | 6 |
| Myocardial infarction | 1 (17) |
| Bowel injury — iatrogenic | 1 (17) |
| Dehiscence — evisceration | 1 (17) |
| Necrotizing fasciitis | 1 (17) |
| Other infection | 1 (17) |
| Grade IV | 1 |
| Septicemia | 1 (100) |
TRACS = Trauma Registry of the American College of Surgeons.
Complications graded according to Clavien and colleagues.10 The percentages reported with each severity grade represent the proportion of the total number for this severity grade.
Table 5 shows the severity of the most commonly encountered complications in surgery. Similar complications vary widely in consequences and, thus, severity grade. This is best illustrated by wound infections, which were grade I in 50% of cases, grade IIa in 22%, grade IIb in 28%, grade III in 0.3% and grade IV in 0.3%. Pneumonia could be treated medically in 90% of cases, but required intubation and mechanical ventilation (grade IIb) in 5% and caused death in 3% of patients. Postoperative hemorrhage required reoperation (grade IIb) in 72% of patients, but was treated conservatively in 26% and caused death in 2% of patients. Most other complications also showed a fairly wide spectrum of severity.
Table 5.
Severity grades of the most frequently occurring complications
| TRACS | Description | Complications; no. (%)* | |||||
|---|---|---|---|---|---|---|---|
| I | IIa | IIb | III | IV | Total, n = 3026 | ||
| 5509 | Wound infection | 197 (50) | 85 (22) | 111 (28) | 1 (0.3) | 1 (0.3) | 395 (13.1) |
| 8508 | Postoperative hemorrhage | 55 (24) | 5 (2) | 165 (72) | 0 | 5 (2) | 230 (7.6) |
| 3008 | Pneumonia | 5 (3) | 155 (90) | 8 (5) | 0 | 5 (3) | 173 (5.7) |
| 5507 | Septicemia | 5 (4) | 78 (69) | 18 (16) | 1 (0.9) | 11 (10) | 113 (3.7) |
| 6003 | Urinary tract infection | 3 (3) | 104 (96) | 1 (1) | 0 | 0 | 108 (3.6) |
| 4003 | Abdominal wall dehiscence/evisceration | 11 (11) | 2 (2) | 51 (51) | 35 (35) | 1 (1) | 100 (3.3) |
| 5503 | Intra-abdominal abscess | 4 (4) | 3 (3) | 82 (91) | 0 | 1 (1) | 90 (3.0) |
| 3501 | Cardiac arrhythmia | 11 (18) | 47 (77) | 3 (5) | 0 | 0 | 61 (2.0) |
| 7507 | Arterial thrombosis | 5 (8) | 6 (10) | 40 (67) | 6 (10) | 3 (5) | 60 (2.0) |
| 3505 | Myocardial infarction | 1 (2) | 26 (44) | 0 | 25 (42) | 7 (12) | 59 (1.9) |
| 4001 | Bowel anastomotic leak | 3 (6) | 1 (2) | 43 (84) | 2 (4) | 2 (4) | 51 (1.7) |
| 8502 | Drug related | 19 (39) | 28 (57) | 1 (2) | 0 | 1 (2) | 49 (1.6) |
| 3015 | Respiratory failure | 1 (3) | 3 (8) | 34 (85) | 0 | 2 (5) | 40 (1.3) |
| 3504 | Congestive heart failure | 28 (78) | 3 (8) | 5 (14) | 0 | 36 (1.2) | |
| 5504 | Line infection | 7 (20) | 24 (69) | 3 (9) | 0 | 1 (3) | 35 (1.2) |
| 6506 | Loss of reduction/fixation | 0 | 0 | 29 (85) | 5 (15) | 0 | 34 (1.1) |
| 3009 | Pneumothorax | 2 (9) | 0 | 20 (91) | 0 | 0 | 22 (0.7) |
| 6509 | Orthopedic wound infection | 1 (5) | 7 (35) | 10 (50) | 1 (5) | 1 (5) | 20 (0.7) |
| 4008 | Ileus | 1 (5) | 5 (26) | 13 (68) | 0 | 0 | 19 (0.6) |
| 7011 | Stroke/cerebrovascular accident | 0 | 0 | 0 | 13 (72) | 5 (28) | 18 (0.6) |
| 3014 | Pulmonary embolus | 0 | 9 (53) | 3 (18) | 0 | 5 (29) | 17 (0.6) |
TRACS = Trauma Registry of the American College of Surgeons.
Complications graded according to Clavien and colleagues.10 The percentages reported with each severity grade represent the proportion of the total number for this complication.
Discussion
This study shows that severity grades of complications are highly variable, although they are registered by identical descriptions and codes. Therefore, complication rates are of limited value without specifying severity grades. Furthermore, this study shows that although severity grading of complications tells a lot about their for patients, it certainly does not tell it all since, for example, many grade IIb complications also involved consequences other than re-interventions (e.g., pharmacologic treatment, intubation and mechanical ventilation, readmission, transfer to other departments). Interestingly, many grade I complications were also shown to have consequences, such as readmission, bedside procedures or transfer to another department, which are associated with discomfort for the patient.
The variability of the consequences of complications presumably depends on the nature of the complication, patient factors, individual doctors’ decisions and the quality of care provided to counteract the effects of the complication. In fact, it recently has been shown that hospitals with high mortality rates have similar overall complication rates and a similar incidence of major complications compared with hospitals with the lowest mortality rates. The difference in mortality is probably the result of the way the complication is managed.15 The fact that severity and consequences of complications are variable has important implications for daily clinical practice and for evaluating quality of care. Among the best examples of this variability are wound infections, which are usually presented in the surgical literature as a single entity,9 at best distinguishing between deep and superficial wound infections.16 The results of our study, however, show that the severity and consequences of wound infections are highly variable. Half of all wound infections could be treated by bedside procedures, 22% were treated with antibiotics, but up to 28% required operative treatment. The risk of death from a wound infection in our study was extremely low. Wound infections with major consequences on patient health may represent a group of more serious complications, worse patient health or worse quality of care provided. Other complications with a wide variation in consequences were postoperative hemorrhage, septicemia, abdominal wall dehiscence, cardiac arrhythmias, myocardial infarction and pulmonary embolus. Among the complications that tended to have fairly consistent consequences were anastomotic leak, which almost always needed operative treatment, and urinary tract infection, which could almost exclusively be managed pharmacologically.
In recent years, providing patients with information about the intended treatment has received more and more attention. Information sources are more widely available to patients than ever before and patients expect to be properly informed about a treatment and its associated risk. Although medical professionals are highly committed to patient education, they generally tend to underestimate the patients’ desire to receive extensive information before surgical procedures.17 Complications are now generally discussed with patients, but the consequences of complications usually are not discussed in detail. The results of our study may be used to more thoroughly inform patients about the possible impact of complications.
Assessing the quality of care has become increasingly important to providers, government and patients, with a focus on developing performance indicators for measuring outcome.18 One of the best examples of programs to improve quality of care is the National Surgical Quality Improvement Program by the American College of Surgeons.7 In surgery, complications are generally accepted and used as outcome indicators to compare quality of care. Public opinion and leading medical opinion have traditionally focused on crude mortality and general complication rates, sometimes distinguishing between minor and major complications without properly defining them.8,9,12 Up to now, the lack of a uniformly adopted system for classifying severity of complications has hampered comparability of the events reported in the surgical literature, although the modified Clavien–Dindo system11 is used with increasing frequency. The results of our study signify the need for a uniform grading system for complications, especially if these are used as outcome measures. The modified system proposed by Clavien and colleagues11 is a serious candidate to become (if it is not already) the uniform manner of grading the severity of a complication. The system has been used for complications from liver surgery, pancreatic surgery and laparoscopic urologic procedures.19–22 Compared with the original system, the theoretical framework of the new classification is the same, but the authors added more subclassifications, including stay in the intensive care unit, differentiation between procedures under local and general anesthesia and differentiation between single and multiple organ failure. Recently, another modification of the system was proposed: the Accordion Severity Grading System.23 This system has similarities to both the 1992 classification system by Clavien and colleagues and the Clavien–Dindo system presented in 2004. Although the new classification systems may have advantages over the original, we elected to use the original for the present study because, at the time of designing our study, we had no experience with the revised (Clavien–Dindo) system, and extensive support in the literature was lacking at the time. Although some classification systems may have advantages over others, it is far more important that a single classification system is used throughout the surgical literature to facilitate the comparison of outcomes in surgical research or in clinical practice. The extensive efforts that have been made to validate the Clavien–Dindo system,11,24 as well as the vast number of authors using the this system,24 may favour it as the most appropriate international standard for reporting complications.
The original Clavien system and its modifications are valuable tools in complication registries and outcomes research; however, there are also some drawbacks. Disadvantages of both the original and revised systems are that they define severity of complications solely from the doctors’ point of view and that the duration of the effect of the complication is not taken into account. For example, a reoperation for anastomotic leak is classified identically to a reoperation for postoperative hemorrhage in patients who have had mastectomies. Almost every surgeon will agree that the former is a more severe complication, with far more devastating and longer-lasting impact. Furthermore, whether a complication necessitating a single reoperation is more severe than a complication requiring prolonged medical treatment is probably not up to the doctor to decide; defining the severity of complications at some point should take into account the patient’s point of view. Recently, an effort was made to correlate the Clavien–Dindo classification to patients’ and nurses’ perceptions of the severity of the complication by using written clinical scenarios; it was shown that patients perceived grade III and IV complications more severely than doctors and nurses.24 Although at present this is the only evidence available relating the severity of complications and patients’ perceptions, it would be better to relate the severity of complications to validated psychological constructs, such as quality of life, health status, anxiety and depression. However, to our knowledge, there are no studies investigating the effect of surgical complications on these psychological phenomena. At the moment, a prospective study is being conducted in our hospital specifically to evaluate the psychological impact of complications following gastroenterological surgery.
Limitations
The results of the present study are both valid and valuable, although there are some limitations. It is a well-known problem that complications tend to be subject to underreporting, which may be the case in our hospital. Underreporting of complications most frequently occurs when complications are nonsevere and not prospectively recorded.25 Prospective registration has shown to be far superior to morbidity and mortality rounds and has been suggested as a standard by different authors.25,26 In our hospital, such a registry has existed for many years, with a strong focus on quality improvement. A previous study by our group27 has shown a clear learning curve, with increasing numbers of recorded complications over the years more likely reflecting better registration than higher complication rates. A change in attitude, definition of complications and real-time registry had a severe influence on the incidence of complications.27 Although in our registry, 90% of complications among patients undergoing laparoscopic cholecystectomy were adequately registered,13 some under-reporting of complications probably is inevitable. However, underreporting would not render our conclusions invalid, since the variation in gradation of complications will not differ substantially when registration is complete.
Conclusion
Our study illustrates the applicability and usefulness of recording the severity and consequences of complications, and provides insight into the severity and consequences of complications in a general surgical practice. It shows that severity grades within complications are highly variable. There is a need for a universal system for grading severity of complications to compare quality of care between different health care providers. Further studies are needed to investigate the effect of complications on patients’ quality of life and health status. These results must then be used to validate and, if necessary, modify the systems used to grade the severity of complications. Finally, we suggest that registering and recording the severity of complications should become standard practice when reporting complications in clinical practice and in the surgical literature to adequately compare quality of care and the results of clinical trials.
Footnotes
Competing interests: None declared.
Contributors: E. Bosma, E.J. Veen and J.A. Roukema designed the study. E. Bosma and M.A.C. de Jongh acquired the data, which E. Bosma and M.A.C. de Jongh analyzed. E. Bosma wrote the article. All authors reviewed the article and approved its publication.
References
- 1.Collins TC, Daley J, Henderson WH, et al. Risk factors for prolonged length of stay after major elective surgery. Ann Surg. 1999;230:251–9. doi: 10.1097/00000658-199908000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coello R, Charlett A, Wilson J, et al. Adverse impact of surgical site infections in English hospitals. J Hosp Infect. 2005;60:93–103. doi: 10.1016/j.jhin.2004.10.019. [DOI] [PubMed] [Google Scholar]
- 3.Roukema JA, van der WC, Leenen LP. Registration of postoperative complications to improve the results of surgery. Ned Tijdschr Geneeskd. 1996;140:781–4. [PubMed] [Google Scholar]
- 4.Zhan C, Miller MR. Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. JAMA. 2003;290:1868–74. doi: 10.1001/jama.290.14.1868. [DOI] [PubMed] [Google Scholar]
- 5.Khuri SF, Henderson WG, DePalma RG, et al. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg. 2005;242:326–41. doi: 10.1097/01.sla.0000179621.33268.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin RC, Brennan MF, Jaques DP. Quality of complication reporting in the surgical literature. Ann Surg. 2002;235:803–13. doi: 10.1097/00000658-200206000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rowell KS, Turrentine FE, Hutter MM, et al. Use of national surgical quality improvement program data as a catalyst for quality improvement. J Am Coll Surg. 2007;204:1293–300. doi: 10.1016/j.jamcollsurg.2007.03.024. [DOI] [PubMed] [Google Scholar]
- 8.Sokol DK, Wilson J. What is a surgical complication? World J Surg. 2008;32:942–4. doi: 10.1007/s00268-008-9471-6. [DOI] [PubMed] [Google Scholar]
- 9.Bruce J, Russell EM, Mollison J, et al. The measurement and monitoring of surgical adverse events. Health Technol Assess. 2001;5:1–194. doi: 10.3310/hta5220. [DOI] [PubMed] [Google Scholar]
- 10.Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–26. [PubMed] [Google Scholar]
- 11.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Veen EJ, Steenbruggen J, Roukema JA. Classifying surgical complications: a critical appraisal. Arch Surg. 2005;140:1078–83. doi: 10.1001/archsurg.140.11.1078. [DOI] [PubMed] [Google Scholar]
- 13.Veen EJ, Bik M, Janssen-Heijnen ML, et al. Outcome measurement in laparoscopic cholecystectomy by using a prospective complication registry: results of an audit. Int J Qual Health Care. 2008;20:144–51. doi: 10.1093/intqhc/mzm073. [DOI] [PubMed] [Google Scholar]
- 14.American College of Surgeons Committee on Trauma. Resources for the optimal care of the injured patient. Chicago (IL): The College; 1999. Performance improvement; pp. 69–79. [Google Scholar]
- 15.Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med. 2009;361:1368–75. doi: 10.1056/NEJMsa0903048. [DOI] [PubMed] [Google Scholar]
- 16.Smith RL, Bohl JK, McElearney ST, et al. Wound infection after elective colorectal resection. Ann Surg. 2004;239:599–605. doi: 10.1097/01.sla.0000124292.21605.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keulers BJ, Scheltinga MR, Houterman S, et al. Surgeons underestimate their patients’ desire for preoperative information. World J Surg. 2008;32:964–70. doi: 10.1007/s00268-008-9581-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mainz J. Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care. 2003;15:523–30. doi: 10.1093/intqhc/mzg081. [DOI] [PubMed] [Google Scholar]
- 19.DeOliveira ML, Winter JM, Schafer M, et al. Assessment of complications after pancreatic surgery: a novel grading system applied to 633 patients undergoing pancreaticoduodenectomy. Ann Surg. 2006;244:931–7. doi: 10.1097/01.sla.0000246856.03918.9a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kocak B, Koffron AJ, Baker TB, et al. Proposed classification of complications after live donor nephrectomy. Urology. 2006;67:927–31. doi: 10.1016/j.urology.2005.11.023. [DOI] [PubMed] [Google Scholar]
- 21.Permpongkosol S, Link RE, Su LM, et al. Complications of 2775 urological laparoscopic procedures: 1993 to 2005. J Urol. 2007;177:580–5. doi: 10.1016/j.juro.2006.09.031. [DOI] [PubMed] [Google Scholar]
- 22.Tamura S, Sugawara Y, Kaneko J, et al. Systematic grading of surgical complications in live liver donors according to Clavien’s system. Transpl Int. 2006;19:982–7. doi: 10.1111/j.1432-2277.2006.00375.x. [DOI] [PubMed] [Google Scholar]
- 23.Strasberg SM, Linehan DC, Hawkins WG. The accordion severity grading system of surgical complications. Ann Surg. 2009;250:177–86. doi: 10.1097/SLA.0b013e3181afde41. [DOI] [PubMed] [Google Scholar]
- 24.Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–96. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 25.Feldman L, Barkun J, Barkun A, et al. Measuring postoperative complications in general surgery patients using an outcomes-based strategy: comparison with complications presented at morbidity and mortality rounds. Surgery. 1997;122:711–9. doi: 10.1016/s0039-6060(97)90078-7. [DOI] [PubMed] [Google Scholar]
- 26.Hutter MM, Rowell KS, Devaney LA, et al. Identification of surgical complications and deaths: an assessment of the traditional surgical morbidity and mortality conference compared with the American College of Surgeons-National Surgical Quality Improvement Program. J Am Coll Surg. 2006;203:618–24. doi: 10.1016/j.jamcollsurg.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 27.Veen EJ, Janssen-Heijnen ML, Leenen LP, et al. The registration of complications in surgery: a learning curve. World J Surg. 2005;29:402–9. doi: 10.1007/s00268-004-7358-8. [DOI] [PubMed] [Google Scholar]