Abstract
Objective:
Experiences of racial/ethnic bias and unfair treatment are risk factors for alcohol problems, and population differences in exposure to these social adversities (i.e., differential exposure) may contribute to alcohol-related disparities. Differential vulnerability is another plausible mechanism underlying health disparities, yet few studies have examined whether populations differ in their vulnerability to the effects of social adversity on psychological stress and the effects of psychological stress on alcohol problems.
Method:
Data from the 2005 U.S. National Alcohol Survey (N = 4,080 adult drinkers) were analyzed using structural equation modeling to assess an overall model of pathways linking social adversity, depressive symptoms, heavy drinking, and alcohol dependence. Multiple group analyses were conducted to assess differences in the model’s relationships among Blacks versus Whites, Hispanics versus Whites, and the poor (income below the federal poverty line) versus non-poor (income above the poverty line).
Results:
The overall model explained 48% of the variance in alcohol dependence and revealed significant pathways between social adversity and alcohol dependence involving depressive symptoms and heavy drinking. The effects of social adversity and depressive symptoms were no different among Blacks and Hispanics compared with Whites. However, the poor (vs. non-poor) showed stronger associations between unfair treatment and depressive symptoms and between depressive symptoms and heavy drinking.
Conclusions:
Contrary to some prior studies, these findings suggest that racial disparities in alcohol problems may be more a function of racial/ethnic minorities’ greater exposure, rather than vulnerability, to chronic stressors such as social adversity. However, observed differences between the poor and non-poor imply that differential vulnerability contributes to socioeconomic disparities in alcohol problems. Efforts to reduce both differential exposure and vulnerability might help to mitigate these disparities.
Chronic exposure to social adversity in the forms of racial/ethnic bias and unfair treatment is associated with a variety of health conditions and risk behaviors, including subclinical cardiovascular disease (Cardarelli et al., 2010; Lewis et al., 2006; Troxel et al., 2003), poor mental health (Williams et al., 2003), tobacco use (Bennett et al., 2005; Chae et al., 2008a), and excessive alcohol use and problems (Gee et al., 2007; Martin et al., 2003; Mulia et al., 2008b). Given the greater exposure of racial/ethnic minorities and low socioeconomic status (SES) groups to chronic stressors (Hatch, 2005; Kessler et al., 1999; Williams et al., 1997), differential stress exposure is increasingly recognized as an important mechanism in health disparities (Egerter et al., 2011). Differential vulnerability is another theoretical mechanism that may underlie disparities. It is the idea that certain individuals or groups are more susceptible than others to health-related consequences once they are exposed to risk factors (Diderichsen et al., 2001). Distinguishing these two mechanisms is crucial because they each imply the need for different strategies to reduce health disparities. Yet despite research suggesting that socially disadvantaged groups may be more vulnerable to the health impacts of exposure to stressors, few studies have assessed whether populations vary in the effects of chronic social adversity on alcohol-related (and other health) problems.
The current study begins to address this gap in knowledge regarding differential vulnerability to chronic social stressors, specifically as it relates to alcohol problems. We tested a conceptual model in which social adversity (in the forms of racial/ethnic stigma and unfair treatment) is positively associated with depressive symptoms, which in turn is directly, positively associated with both heavy drinking and alcohol dependence. (A direct association between heavy drinking and alcohol dependence is also posited.) We focused on the potentially greater vulnerability of racial/ethnic minorities and low-SES groups because both groups have elevated rates of alcohol-related problems, morbidity, and mortality (Grant, 1997; Hilton, 2006; Mulia et al., 2009; Yoon and Yi, 2007) and greater exposure to chronic stressors. Moreover, both groups are disadvantaged in ways that could, theoretically, affect how they cope with stressors and stress. In particular, a lack of economic resources and lower social standing can limit access to opportunities, privileges, and health-enhancing resources (Mulia et al., 2008b; Williams et al., 1994). Thus, there is an important unanswered question as to whether racial/ethnic and socioeconomic disparities in alcohol problems reflect differential exposure and/or differential vulnerability to chronic stressors.
Social adversity and alcohol problems
A number of studies have found that chronic exposure to racial bias and unfair treatment is associated with excessive alcohol use and problems (Chae et al., 2008b; Gee et al., 2007; Martin et al., 2003; Mulia et al., 2008b; Yen et al., 1999; Zemore et al., 2011). Research on these social adversities has been largely directed at understanding minority health and racial disparities in health rather than socioeconomic disparities per se. Most studies have been conducted with Black Americans and, to a lesser extent, other ethnic minorities. A review of the limited research on Whites from the broader health field indicates that they, too, are negatively affected by these social adversities (Paradies, 2006). In our own multiethnic study, we found that Whites who experienced racial stigma and unfair treatment had elevated levels of psychological stress. Further, the positive relationship between unfair treatment and problem drinking in Whites was highly similar to that observed in Blacks and Hispanics (Mulia et al., 2008b). This suggests that racial/ ethnic minorities’ greater prevalence of exposure to chronic social stressors plays a role in racial disparities in alcohol problems.
Although far less is known about the role of social adversity in socioeconomic disparities in alcohol (and other health) problems, low-SES groups are more exposed to a variety of stressors, including unfair treatment (Turner and Avison, 2003), thus suggesting the plausibility of the differential stress hypothesis with respect to socioeconomic disparities in health.
The question of differential vulnerability
The differential vulnerability hypothesis is less often raised in discussions of health disparities, including alcohol-related disparities. This is somewhat surprising. A large body of work demonstrates that individuals respond to stressors and stress differently, depending on cognitive and coping factors (Folkman, 2008; Folkman and Moskowitz, 2004; Lazarus, 1993; Lazarus and Folkman, 1984) such as perceived control and social support (Pearlin et al., 1981; Thoits, 1995). Contextual factors such as drinking norms and the availability of alcohol in the environment can also influence the extent to which individuals drink alcohol in response to stress (e.g., Herd, 1994; Huckle et al., 2008; Lindenberg et al., 1999; Scribner et al., 2000). Importantly, racial/ethnic minorities and low-income persons are more likely to reside in communities with more alcohol outlets and aggressive alcohol advertising (Bluthenthal et al., 2008; Pollack et al., 2005), and have been shown to have fewer stress-buffering and coping resources (Meyer et al., 2008; Pearlin et al., 1981; Thoits, 1995). These groups might, therefore, be more negatively affected by experiences of social adversity and psychological stress.
Few alcohol studies have investigated this possibility, particularly with respect to SES differences in vulnerability. One exception was our previous study of African Americans and Hispanics showing that poverty exacerbates the effects of social adversity on drinking outcomes, particularly among Hispanics (Zemore et al., 2011). More often, alcohol studies of differential vulnerability have compared racial/ethnic minorities with Whites. Research conducted with drinkers in upstate New York found that depression was more strongly related to drinking to cope and alcohol problems among Black compared with White drinkers (Peirce et al., 1994) and that alcohol expectancies of stress reduction were associated more strongly with drinking outcomes among Black (vs. White) drinkers (Cooper et al., 1995). Yet there was only weak evidence of Black-White differences in problem drinking as a result of stressful life events (Cooper et al., 1992).
Furthermore, some studies suggest that racial/ethnic minorities may respond to adversity in roughly similar or even less deleterious ways than Whites. Lloyd and Turner (2008) found no racial/ethnic differences in the effects of cumulative lifetime adversity on alcohol dependence, and that the effects of adversity on drug dependence were strong among Whites and weakest among African Americans. Additionally, our prior work suggests that the relationship between cumulative stressors and problem drinking may be stronger among Whites compared with Blacks and Hispanics (Mulia et al., 2008b), similar to a recent report by Keyes and colleagues (2011).
Prior studies have had some limitations, however. A few were confined to stratified analyses and omitted formal testing for differential relationships across groups. Also, many studies conflate exposure to adversity with psychological stress. This is a limitation when studying differential vulnerability because people vary both in how they perceive and react to stressors (e.g., whether unfair treatment results in stress) and in how they respond to stress (e.g., whether they drink heavily). Only by distinguishing stressors and stress can researchers specify where in the pathway from stressors to health endpoints there arise significant, group differences in vulnerability. Pinpointing these is necessary to tailoring and targeting interventions to address disparities in alcohol and other health problems.
Current study
This study aims to extend the sparse research on differential vulnerability by examining population differences in the effects of social adversity on stress and the effects of stress on heavy drinking and alcohol problems. Specifically, we assessed whether racial/ethnic minorities and low-income persons are more vulnerable. Using data from the 2005 U.S. National Alcohol Survey (NAS), we began by testing an overall, conceptual model of pathways linking social adversity and alcohol problems that includes stress and heavy drinking as intermediary outcomes. We then rigorously examined group differences in these pathways. Consistent with growing interest in the health impacts of unfair treatment and racial/ethnic bias, these two forms of social adversity were investigated here. Our hypotheses included the following: (a) Social adversity would be associated with alcohol problems through its effects on stress and heavy drinking; (b) in view of prior, contradictory findings for racial/ethnic differences and the paucity of research on SES differences, we tested the exploratory hypotheses that racial/ethnic minorities and Whites would show similar effects of social adversity on stress and similar effects of stress on heavy drinking and alcohol problems; and (c) the poor (vs. non-poor) would be more vulnerable to stress as well as to heavy drinking and alcohol problems.
Method
The 2005 NAS is a national household computer-assisted telephone interview survey of persons ages 18 years and older. Data were collected using list-assisted random-digit dialing with a sampling frame of all 50 states and the District of Columbia. In addition to the main sample, the NAS includes oversamples of Blacks and Hispanics. Interviews were conducted in either English or Spanish, according to respondent preference. Completed interviews were obtained for 6,919 respondents, including 3,967 Whites, 1,054 Blacks, and 1,610 Hispanics; among these, there were 2,810 White, 504 Black, and 766 Hispanic current drinkers. The response rate was 56%, consistent with current response rates for telephone surveys (Curtin et al., 2005). Although such rates raise questions about nonresponse bias, methodological studies find that increased nonresponse does not necessarily result in biased population estimates (Groves, 2006; Keeter et al., 2006). Analysis of the telephone-based, 2000 NAS replicate subsamples found that response rate was not associated with the level of alcohol consumption (Greenfield et al., 2006). In addition, methodological studies comparing identical NAS items collected in telephone versus face-to-face surveys showed comparable estimates for alcohol-related variables, despite typically higher response rates for the face-to-face surveys (Greenfield, 2000; Greenfield et al., 2000; Midanik and Greenfield, 2003a, 2003b). This suggests that the impact of nonresponse bias associated with typically lower response rates of telephone surveys might not significantly affect results related to alcohol consumption and problems.
Measures
Heavy drinking was operationalized as the frequency of drunkenness within the past 12 months. Respondents were asked “How often in the past year did you drink enough to feel drunk?” with responses ranging from never (0) to every day or nearly every day (6). This measure has been shown to be a comparable, if not better, predictor of alcohol-related problems than the frequency of 5+ drinking (Greenfield and Kerr, 2008; Midanik, 1999). The frequency of drunkenness was log-transformed to reduce skew (range: 0–5.75).
Alcohol problems was operationalized as alcohol dependence, a dichotomous measure indicating at least one symptom in the past 12 months in three or more of seven dependence domains, consistent with the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (American Psychiatric Association, 1994). This measure was based on 17 items and has been validated in prior NAS studies (for further details, see Caetano and Tam, 1995, and Greenfield et al., 2006).
Similar to some general health studies of discrimination, unfair treatment was assessed using a single-item measure (“How often do you feel that you are treated unfairly”), with responses ranging from almost never (1) to very often (5). Although the use of this single-item measure could potentially yield conservative prevalence rates for perceived unfair treatment (Williams and Williams-Morris, 2000), we have found estimates comparable to others. For example, in the NAS, 35% of Hispanics indicated moderate to high levels of unfair treatment (Mulia et al., 2008b), which is virtually identical to the 34% reported by Pérez et al. (2008) based on a nine-item measure capturing the frequency of unfair treatment. Notably, the NAS measure does not specify attribution and might therefore reflect unfair treatment due to a variety of low social status categories (Williams et al., 2003), which is advantageous in the current study. This unfair treatment measure has been previously associated with homelessness, χ2(2) = 196.3, p < .001; low income (r = -.148, p < .001); and low education (r = -.120, p < .001) (Mulia et al., 2008b).
Our indicator of racial bias, perceived racial/ethnic stigma, was based on three items from Pinel’s stigma consciousness scale, the reliability and validity of which have been previously established (Pinel, 1999). The items include (a) “Stereotypes about my race or ethnic group have affected me personally,” (b) “My race or ethnic group influences how people act with me,” and (c) “Many people have a problem viewing my race or ethnic group as equal.” Responses ranged on a 4-point scale from disagree very much (1) to agree very much (4) (α = .72). A mean score was computed by averaging across items.
Our indicator of psychological stress was depressive symptoms. The NAS uses an eight-item version of the Center for Epidemiologic Studies–Depression (CES-D) scale (Radloff, 1977) that is highly correlated with the full CES-D (r = .93 based on 1995 NAS data) and gauges past-week frequency of feeling bothered by things, depressed, hopeful for the future, happy, lonely, sad, having restless sleep, and enjoying life, on a scale from 1 (rarely or none of the time) to 4 (most or all of the time). Because the multiple group analyses revealed racial/ethnic and poverty status differences in factor loadings of the eight items, two items with low loadings (restless sleep and hopeful) were dropped (see Results). Analysis of the latent variable based on six items indicated measurement invariance across groups. The six items are similar to those used to capture nonspecific psychological stress in studies of social adversity (e.g., Kessler et al., 1999; Schulz et al., 2000).
Key demographic variables included race/ethnicity, assessed by asking participants which group best describes their family of origin, gender, age, employment status, and education. Poverty status (poor vs. non-poor) was based on past-year household income, family composition, and U.S. federal poverty guidelines for 2004 (U.S. Department of Health and Human Services, 2005). Respondents with incomes below the federal poverty level were defined as poor.
Analysis
Analyses were conducted on the sample of respondents who reported any alcohol use in the past 12 months (n = 4,080). The data were weighted to the U.S. Census and all analyses adjusted for oversampling and sampling design. Bivariate relationships were first examined using correlational analyses, t tests, and chi-square analyses. The main analysis was implemented using structural equation modeling and Mplus 5.21 (Muthén and Muthén, 2009) and a multiple groups framework. Racial stigma and depressive symptoms were treated as latent variables to reduce measurement error and to test for measurement invariance across groups. Based on the results of factor analyses, the reference indicators were “Stereotypes about my race or ethnic group have affected me personally” (for racial stigma) and “I felt depressed” (for depressive symptoms). Unfair treatment and heavy drinking were assessed using single items and were observed (continuous) variables. For greater interpretability, alcohol dependence was also treated as an observed (dichotomous) variable.
First, we developed measurement and structural models for the overall sample that achieved acceptable fit. Study hypotheses informed specification of the initial structural model, which was refined based on modification indices and parameter estimates. Second, we tested whether both the measurement and structural parameters varied by race/ethnicity and poverty status. In each case, a satisfactory measurement model was developed before proceeding to the structural model. Based on the results, we then modified the models as needed and tested model fit once again. Models incorporated survey weights and estimation techniques appropriate for the design (i.e., MLMV, maximum likelihood with mean and variance adjusted for the measurement models, and WLSMV, weighted least squares with mean and variance adjusted for the structural models, with theta parameterization for the latter). For the multiple group analyses, thresholds, intercepts, and residual variances were free to vary across groups. Factor means were set to zero in the reference group and free to vary in other groups. Following Muthén and Muthén (2011), difference tests were conducted to evaluate the impact of constraining each pathway across groups on overall model fit using modified chi-square difference tests. To account for repeated significance testing in evaluating measurement invariance, we used a modification of the Bonferroni approach, which, based on Benjamini and Hochberg (1995), involves ordering the p values obtained in a family of analyses from large to small and testing each against a successively more stringent criterion. This approach has been recommended for use in latent variable modeling contexts and appears to provide sufficient control for Type I error while avoiding the problem of overcontrol associated with the Bonferroni method (Cribbie, 2007; Green and Babyak, 1997). Each set of tests for racial/ethnic differences in item loadings associated with our two latent variables (i.e., racial stigma and depressive symptoms) was considered a family of tests.
Overall model fit was assessed using the chi-square test, the comparative fit index (CFI), the Tucker–Lewis index (TLI), and the root mean square error of approximation (RMSEA). Good fit is indicated by CFI and TLI values close to or above .95 and an RMSEA value below .06 (Hu and Bentler, 1999). Preliminary models controlled for sex (male vs. female), age (continuous), employment status (employed vs. not employed), education (high school degree or more vs. less), and poverty status (poor vs. non-poor) in predicting the main outcomes (i.e., depressive symptoms, heavy drinking, and alcohol dependence). For the final model, covariates were removed where nonsignificant. All covariate selection and refinement was accomplished in models for the overall sample; in the multiple group comparisons, pathways between covariates and outcomes were held constant across groups. In general, the literature has given little attention to whether to fix or free covariate pathways in multiple group analysis. We decided to fix pathways for each covariate to equivalence across groups because doing so allows for easier interpretation (i.e., differences in structural pathways could not then be artifacts of changes in relationships involving covariates). Notably, sensitivity analyses (not shown) revealed that freeing covariate pathways produced nearly identical model fit indices, suggesting that our assumptions of equivalence appear to be justifiable.
Results
Bivariate analyses
As expected, racial/ethnic minorities and the poor reported higher levels of unfair treatment, racial stigma, and depressive symptoms (Table 1). Both groups also had higher rates of alcohol dependence, and the poor (vs. non-poor) reported more frequent heavy drinking as well. Also as expected, correlational analyses showed that racial stigma and unfair treatment were positively related to depressive symptoms, and the latter was positively related to heavy drinking and alcohol dependence. The correlations between depressive symptoms and alcohol outcomes were nearly twice as strong among poor (vs. non-poor) drinkers, tentatively suggesting increased vulnerability among the poor. Such pronounced differences were not found between racial/ ethnic minorities and Whites. Overall, Black and Hispanic respondents were younger than White respondents (Mage = 44, 38, and 48 years, respectively, p < .001), had higher unemployment rates (8%, 7%, and 3%, respectively, p < .001), and were less likely to have had any postsecondary education (57%, 42%, and 72%, respectively, p < .001) (demographic data not shown in Table 1).
Table 1.
Variable means, prevalence (prev.) rates, and correlations, with comparisons across racial/ethnic group and poverty status
| Variable | M or prev. | SD | Racial stigma | Unfair treatmt. | Depress. sympt. | Heavy drink. | Alcohol depend. |
| Overall sample (n = 4,080) | |||||||
| Racial stigma | 1.93 | 0.83 | 1.0 | .24*** | .16*** | .02 | .08*** |
| Unfair treatmt. | 1.94 | 0.99 | .37*** | .07*** | .12*** | ||
| Depress. sympt. | 1.33 | 0.49 | .12*** | .22*** | |||
| Heavy drink. | 0.98 | 1.32 | .36*** | ||||
| Alcohol depend. | 4.3% | – | |||||
| White drinkers (n = 2,810) | |||||||
| Racial stigma | 1.68*** | 0.70 | 1.0 | .15*** | .11*** | .01 | .06*** |
| Unfair treatmt. | 1.86*** | 0.91 | .36*** | .07*** | .13*** | ||
| Depress. sympt. | 1.30*** | 0.46 | .12*** | .21*** | |||
| Heavy drink. | 0.98 | 1.31 | .36*** | ||||
| Alcohol depend. | 2.9%*** | – | |||||
| Black drinkers (n = 504) | |||||||
| Racial stigma | 2.70 | 0.83 | 1.0 | .23*** | .05 | .02 | .02 |
| Unfair treatmt. | 2.26 | 1.12 | .35*** | .05 | .13** | ||
| Depress. sympt. | 1.42 | 0.55 | .12*** | .24*** | |||
| Heavy drink. | 0.97 | 1.39 | .36*** | ||||
| Alcohol depend. | 5.9% | – | |||||
| Hispanic drinkers (n = 766) | |||||||
| Racial stigma | 2.23 | 0.84 | 1.0 | .28*** | .22*** | .02 | .04 |
| Unfair treatmt. | 2.00 | 1.07 | .36*** | .09** | .07* | ||
| Depress. sympt. | 1.39 | 0.54 | .13*** | .22*** | |||
| Heavy drink. | 1.01 | 1.31 | .41*** | ||||
| Alcohol depend. | 7.9% | – | |||||
| Non-poor drinkers (n = 3,103) | |||||||
| Racial stigma | 1.92*** | 0.83 | 1.0 | .26*** | .17*** | -.01 | .08*** |
| Unfair treatmt. | 1.90*** | 0.95 | .34*** | .05* | .10*** | ||
| Depress. sympt. | 1.31*** | 0.47 | .09*** | .19*** | |||
| Heavy drink. | 0.96*** | 1.28 | .33*** | ||||
| Alcohol depend. | 3.5%*** | – | |||||
| Poor drinkers (n = 470) | |||||||
| Racial stigma | 2.11 | 0.86 | 1.0 | .18*** | .10* | .07 | .11* |
| Unfair treatmt. | 2.20 | 1.17 | .41*** | .08 | .18*** | ||
| Depress. sympt. | 1.50 | 0.62 | .20*** | .27*** | |||
| Heavy drink. | 1.32 | 1.62 | .43*** | ||||
| Alcohol depend. | 10.1% | – | |||||
Notes: Significance levels attached to means and prev. rates for White drinkers reference comparisons with Black and Hispanic drinkers; significance levels attached to means and prev. rates for non-poor drinkers (income at or above the federal poverty level) reference comparisons with poor drinkers (income below poverty level). Treatmt. = treatment; depress. sympt. = depressive symptoms; drink.= drinking; depend. = dependence.
p < .05;
p < .01.
p < .001.
Testing the hypothesized model: Pathways between social adversity and alcohol problems
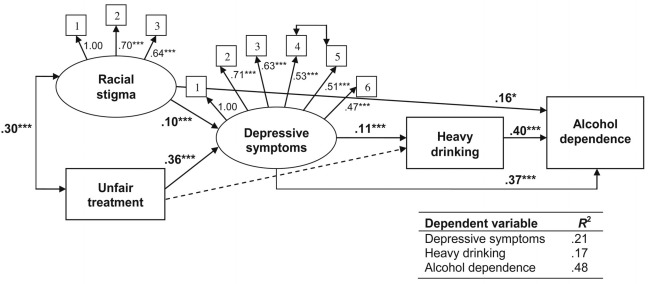
Figure 1 shows the final model developed using the full sample. The model had good fit and explained 48% of the variance in alcohol dependence, as well as substantial variance in depressive symptoms and heavy drinking (see goodness-of-fit indicators and R2 values). The measurement model revealed that the two racial stigma items loaded well with the first item and were retained. For depressive symptoms, two of the eight candidate items (i.e., “I felt hopeful about the future” and “My sleep was restless”) produced low loadings and, hence, were dropped. The remaining CES-D items all loaded well (Figure 1).
Figure 1.
The overall model in the full sample. Model χ2 = 136.0 (46, n = 3,525),p < .001; comparative fit index = .94; Tucker–Lewis index = .97; root mean square error of approximation = .024. Model shows standardized parameter estimates and controls for sex, age, poverty level, employment status, and education in predicting depressive symptoms, heavy drinking, and alcohol dependence (nonsignificant covariates removed). Dashed line (----) represents a tested, but nonsignificant, path. For racial stigma, 1 = stereotypes about my race or ethnic group have affected me personally, 2 = my race or ethnic group influences how people act with me, and 3 = many people have a problem with viewing my racial or ethnic group as equal. For depressive symptoms, 1 = I felt depressed, 2 = I felt sad, 3 = I felt lonely, 4 = I enjoyed life (reverse coded), 5 = I was happy (reverse coded), and 6 = I was bothered by things that don’t usually bother me. *p <.05; ***p < .001.
Consistent with this study’s first hypothesis, the structural model indicated that both racial stigma and unfair treatment were positively related to depressive symptoms (Figure 1; βs = .10 and .36, respectively,p < .001). Depressive symptoms were, in turn, positively associated with heavier drinking (β = .11, p < .001), which strongly predicted alcohol dependence (β = .40, p < .001). Depressive symptoms were also associated with alcohol dependence independent of heavy drinking (β = .37, p < .001). Notably, formal tests of mediation conducted using Mplus showed significant indirect pathways from racial stigma to alcohol dependence via depressive symptoms (β = .04, p < .001) and, likewise, from unfair treatment to dependence via depressive symptoms (β = .14, p < .001). A parallel test also showed a significant indirect pathway from depressive symptoms to alcohol dependence via heavy drinking (β = .06, p < .001). Based on modification indices, the final model specified shared error variance between two indicators of depressive symptoms (i.e., “I enjoyed life” and “I was happy,” both reverse coded; Figure 1), which is likely a function of the positive wording of these items. The model also included pathways between education and racial stigma and between poverty level and unfair treatment.
Differential vulnerability to stress and alcohol problems: Are Blacks and Hispanics more vulnerable than Whites?
Multiple group analyses were conducted to assess differences in the measurement and structural models across Blacks and Whites (first) and Hispanics and Whites (second). Results revealed that the measurement model was largely equivalent across race/ethnicity. None of the item loadings differed by race/ethnicity when evaluated against our adjusted criterion levels (see Methods), except for one racial stigma item (“Many people have a problem viewing my race or ethnic group as equal”). That item yielded significantly higher loadings for both Blacks (β = .75, p < .001) and Hispanics (β = .78, p < .001) than Whites (β = .44, p < .001). This suggests that, among Blacks and Hispanics, the perception that others treat one differently on the basis of race/ethnicity is closely associated with the belief that others view one’s racial/ethnic group as unequal, whereas this is less true among Whites. In general, most variables in a multiple group analysis should demonstrate loading invariance so that meaningful comparisons can be made across groups. However, partial measurement invariance may not pose a problem if the majority of item loadings are equivalent (Muthén and Asparouhov, 2002). In this case, we feel the substantive contribution of this item to the measurement of racial stigma outweighs the interpretational ambiguity that retaining the item introduces. Also, because the differences in item loadings were minor, measurement invariance should not dramatically alter the ability to compare results for racial stigma across racial/ethnic groups. Accordingly, the structural model was specified with fixed loadings for all indicators except the one racial stigma item noted above, which was free to vary across groups. Chi-square difference tests for structural pathways revealed that only one structural pathway varied significantly between the racial/ethnic groups (ps < .05): The relationship between racial stigma and unfair treatment was stronger among both Blacks (β = .29, p < .001) and Hispanics (β = .36,p < .001) than Whites (β = .23, p < .001). We found no significant racial/ethnic differences in the associations between social adversity and depressive symptoms, and depressive symptoms and alcohol outcomes.
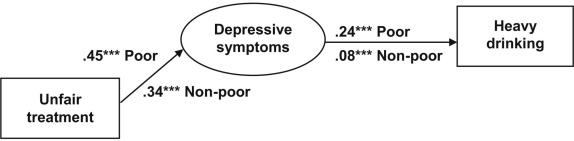
Are the poor more vulnerable than the non-poor to stress and alcohol problems?
Our second multiple group analysis examined differences in vulnerability between the poor and non-poor. Chi-square difference tests showed no major differences in the measurement model across the two groups when evaluated against our adjusted criterion levels (see Method). However, tests of the structural model revealed two significant differences. Specifically, the association between unfair treatment and depressive symptoms was stronger (p < .05) among the poor (β = .45, p < .001) compared with the non-poor (β = .34, p < .001). Likewise, the relationship between depressive symptoms and heavy drinking was stronger (p < .01) among the poor (β = .24, p < .001) versus non-poor (β = .08, p < .001) (Figure 2).
Figure 2.
Differences in vulnerability between poor and non-poor respondents. Non-poor (at or above federal poverty level): Model χ2 = 111.9 (39, n = 3,063), p < .001; comparative fit index (CFI) = .94; Tucker-Lewis index (TLI) = .97; root mean square error of approximation (RMSEA) = .025. Poor (below federal poverty level): Model χ2 = 53.05 (40, n = 462),p = .08; CFI = .94; TLI = .96; RMSEA = .027. Model shows standardized parameter estimates and controls for sex, age, employment status, and education in predicting depressive symptoms, heavy drinking, and alcohol dependence (nonsignificant covariates removed). ***p <.001.
Discussion
This study aims to extend a growing body of research on social adversity and alcohol problems by linking social adversity more directly to the problem of alcohol-related health disparities. Recognizing differential exposure and vulnerability as important theoretical mechanisms underlying health disparities, we investigated the understudied question of whether socially disadvantaged groups (racial/ethnic minorities and the poor) are more vulnerable to the effects of social adversity on psychological stress, and the effects of stress on heavy drinking and alcohol problems.
Confirming our first hypothesis, racial stigma and unfair treatment were related to alcohol dependence through pathways involving depressive symptoms and heavy drinking. The overall model predicting alcohol problems had excellent fit. These findings underscore the important role of stress in health risk behaviors associated with experiences of social adversity.
The study results also support our second (exploratory) hypothesis that racial/ethnic minorities and Whites are similar in their vulnerability to the effects of social adversity and stress, although we found much greater exposure to social adversity and slightly greater depressive symptoms among minorities than Whites. This corroborates the results of some prior research, including our own (e.g., Borrell et al., 2007; Lloyd and Turner, 2008), but deviates from others, as discussed earlier (e.g., Cooper et al., 1992, 1995; Peirce et al., 1994). Note that because existing research on this question is sparse, and studies lack comparability in terms of the types of stressors and alcohol outcomes investigated, additional work is needed to confirm and better understand the lack of racial/ethnic differences in this study. Our study findings raise questions about the experiences of Whites. In what contexts do they perceive that they are racially stigmatized, and on what basis do they feel they are treated unfairly? Unfair treatment may be attributed to various social status categories (e.g., race, SES, gender) and personal characteristics (e.g., criminal history, religious affiliation) (Stuber et al., 2003).
Future research is also needed to understand what factors might mitigate the harmful effects of social adversity experienced by Blacks and Hispanics and thus help to explain why they do not appear to be affected more severely than Whites. Some have speculated that Blacks’ and Hispanics’ more frequent and earlier exposure to social adversity might foster the development of certain coping strategies that Whites have not acquired because of the latter group’s relatively limited experience with unfair treatment and racial stigma (Schulz et al., 2000). For example, early, parental socialization of Black children to racial bias has been shown to lead to more positive coping with racism (Brown and Tylka, 2011; Fischer and Shaw, 1999; Hughes, 2003). Another possibility is that African American and Hispanic populations might be buffered by religiosity and the social support of minority and faith-based communities (West, 1994). Of note, the tendency toward conservative drinking norms in some faith communities, particularly Black churches, might be a significant factor countering the effects of stress on heavy drinking and alcohol problems among Blacks (Herd, 1996).
In support of our third (exploratory) hypothesis, we found evidence that the poor (vs. non-poor) are more vulnerable to the adverse effects of unfair treatment on depressive symptoms and the effects of depressive symptoms on heavy drinking. Indeed, there was a twofold greater association of depressive symptoms with heavy drinking among the poor. These findings are in keeping with those of Dawson and colleagues (2005), who showed that poverty exacerbates the effects of job-related stressors on drinking frequency and alcohol consumption among past-year drinkers. They are also in line with our prior finding that poverty intensifies the effects of unfair treatment and racial stigma on drinking outcomes, particularly among Hispanics (Zemore et al., 2011).
These amplifying effects of poverty might reflect fewer or weaker coping resources among the poor. At least one study has shown that social support, which typically exerts protective effects on health, does not ameliorate the effects of stressors and stress on problem drinking among low-income women (Mulia et al., 2008a). Another potential explanation concerns the environmental conditions in which poor people live. As noted earlier, alcohol outlets are more concentrated in economically deprived areas, and alcohol outlet density is associated with heavier consumption (Kavanagh et al., 2011; Scribner et al., 2000). In the context of constrained coping resources, the greater availability and heavy promotion of alcohol in poor neighborhoods could foster the heavy use of alcohol by low-income drinkers as a way to reduce stress.
The current study has several strengths. These include the analysis of data from a nationally representative sample of drinkers; a conceptual model of pathways linking social adversity to stress to heavy drinking and alcohol problems, thus permitting analysis of differential vulnerability at various points in the pathway; and rigorous testing for differential effects using multiple group analysis.
Several caveats and limitations deserve mention, however. First, the estimated differences between poor and non-poor drinkers are likely to be conservative in this study because the “non-poor” sample includes both affluent and near-poor respondents. Second, because the measure of unfair treatment does not specify attribution, the implications for targeted intervention are limited. Additionally, our stress measure captures only one aspect of stress—depressive symptoms—and was based on six items of the CES-D, which has been correlated with other psychological states. Future studies would benefit from more specific and stronger measures of unfair treatment and mental health. Third, there was insufficient power to conduct multiple group analyses of racial/ethnic differences at specific levels of SES. This is an important agenda for future research. Fourth, the observed associations of unfair treatment with heavy drinking and alcohol dependence could, potentially, reflect personality risk factors not studied here and warranting consideration. Finally, the study’s cross-sectional design does not allow us to assess temporal ordering, and therefore the relationships described here could reflect reverse or bidirectional causality. To address the possibility of reciprocal causation, we tested an alternative model adding the reverse pathway from alcohol dependence to depressive symptoms, which was nonsignificant (p = .15). Although this argues against reciprocal causation, longitudinal data are needed. Notably, longitudinal studies previously have shown that experiences of racial bias can affect subsequent levels of psychological stress (Brown et al., 2000) and that both racial bias and adverse emotional responses can affect the subsequent use of substances (Gibbons et al., 2010).
Despite these limitations, this study contributes important, new information on the theoretical mechanisms by which chronic social stressors may contribute to racial and socio-economic disparities in alcohol problems. Our study results suggest that differential exposure, rather than vulnerability, to unfair treatment, racial stigma, and psychological stress may be the more important factor in racial disparities in alcohol problems. This implies that efforts to reduce racial/ ethnic minorities’ greater exposure to these social adversities (e.g., through antidiscrimination policies and initiatives to foster racial diversity and integration) might help to mitigate stress, heavy drinking, and alcohol problems in these populations and thereby reduce alcohol-related racial disparities.
Our study findings have somewhat different implications for how we address socioeconomic disparities in alcohol problems. The commonly observed inverse, SES gradient in harmful drinking patterns has been attributed to low-SES groups’ greater exposure to chronic, material stressors (Droomers et al., 1999). Our study results do not contradict this but suggest that differences in vulnerability to social adversity and stress are also relevant. Together, these studies imply that dual efforts are needed to address both differential exposure and vulnerability, such as income-support policies and community development interventions targeted to low-SES persons and high-poverty areas, as well as interventions to prevent unhealthy coping behaviors. The latter could include structural interventions to reduce alcohol outlets and alcohol advertising in poor neighborhoods, as well as public media campaigns and counseling interventions. Ultimately, multilevel and multipronged interventions are likely to be our best hope in addressing the problems of chronic stress and unhealthy behaviors that contribute to health disparities.
Acknowledgments
The authors gratefully acknowledge the thoughtful comments and suggestions of two anonymous reviewers, which helped to strengthen this article considerably. They also thank Drs. Katherine J. Karriker-Jaffe, Jason Bond, and Tammy Tam for helpful discussions of structural equation modeling and multiple group analysis implemented in Mplus.
Footnotes
This study was supported by National Institute on Alcohol Abuse and Alcoholism Grants R21AA015397, R21AA015972, R01AA020474, and P50AA05595.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. Series B (Methodological) 1995;57:289–300. [Google Scholar]
- Bennett GG, Wolin KY, Robinson EL, Fowler S, Edwards CL. Perceived racial/ethnic harassment and tobacco use among African American young adults. American Journal of Public Health. 2005;95:238–240. doi: 10.2105/AJPH.2004.037812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluthenthal RN, Cohen DA, Farley TA, Scribner R, Beighley C, Schonlau M, Robinson PL. Alcohol availability and neighborhood characteristics in Los Angeles, California and southern Louisiana. Journal of Urban Health. 2008;85:191–205. doi: 10.1007/s11524-008-9255-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrell LN, Jacobs DR, Jr, Williams DR, Pletcher MJ, Houston TK, Kiefe CI. Self-reported racial discrimination and substance use in the coronary artery risk development in adults study. American Journal of Epidemiology. 2007;166:1068–1079. doi: 10.1093/aje/kwm180. [DOI] [PubMed] [Google Scholar]
- Brown DL, Tylka TL. Racial discrimination and resilience in African American young adults: Examining racial socialization as a moderator. Journal of Black Psychology. 2011;37:259–285. [Google Scholar]
- Brown TN, Williams DR, Jackson JS, Neighbors HW, Torres M, Sellers SL, Brown KT. “Being black and feeling blue”: The mental health consequences of racial discrimination. Race and Society. 2000;2:117–131. [Google Scholar]
- Caetano R, Tam TW. Prevalence and correlates of DSM-IV and ICD-10 alcohol dependence: 1990 US National Alcohol Survey. Alcohol and Alcoholism. 1995;30:177–186. [PubMed] [Google Scholar]
- Cardarelli R, Cardarelli KM, Fulda KG, Espinoza A, Cage C, VishwanathaCarroll J. Self-reported racial discrimination, response to unfair treatment, and coronary calcification in asymptomatic adults—the North Texas Healthy Heart study. BMC Public Health, 10(1) 2010;285 doi: 10.1186/1471-2458-10-285. Retrieved from http://www.biomedcentral. com/1471-2458/10/285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chae DH, Takeuchi DT, Barbeau EM, Bennett GG, Lindsey J, Krieger N. Unfair treatment, racial/ethnic discrimination, ethnic identification, and smoking among Asian Americans in the National Latino and Asian American Study. American Journal of Public Health. 2008a;98:485–492. doi: 10.2105/AJPH.2006.102012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chae DH, Takeuchi DT, Barbeau EM, Bennett GG, Lindsey JC, Stoddard AM, Krieger N. Alcohol disorders among Asian Americans: Associations with unfair treatment, racial/ethnic discrimination, and ethnic identification (the National Latino and Asian Americans Study, 2002–2003) Journal of Epidemiology and Community Health. 2008b;62:973–979. doi: 10.1136/jech.2007.066811. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology. 1995;69:990–1005. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Frone MR, Mudar P. Stress and alcohol use: Moderating effects of gender, coping, and alcohol expectancies. Journal of Abnormal Psychology. 1992;101:139–152. doi: 10.1037//0021-843x.101.1.139. [DOI] [PubMed] [Google Scholar]
- Cribbie RA. Multiplicity control in structural equation modeling. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14:98–112. [Google Scholar]
- Curtin R, Presser S, Singer E. Changes in telephone survey nonresponse over the past quarter century. Public Opinion Quarterly. 2005;69:87–98. [Google Scholar]
- Dawson DA, Grant BF, Ruan WJ. The association between stress and drinking: Modifying effects of gender and vulnerability. Alcohol and Alcoholism. 2005;40:453–460. doi: 10.1093/alcalc/agh176. [DOI] [PubMed] [Google Scholar]
- Diderichsen F, Evans T, Whitehead M. The social basis of disparities in health. In: Evans T, Whitehead M, Diderichsen F, Bhuiya A, Wirth M, editors. Challenging inequities in health:.From ethics to action. New York, NY: Oxford University Press; 2001. pp. 12–23. [Google Scholar]
- Droomers M, Schrijvers CTM, Stronks K, van de Mheen D, Mackenbach JP. Educational differences in excessive alcohol consumption: The role of psychosocial and material stressors. Preventive Medicine. 1999;29:1–10. doi: 10.1006/pmed.1999.0496. [DOI] [PubMed] [Google Scholar]
- Egerter S, Braveman P, Barclay C. How social factors shape health: The role of stress. Robert Wood Johnson Foundation Issue Brief Series: Exploring the Social Determinants of Health—Stress and Health. 2011 Retrieved from. http://www.rwjf.org/files/research/sdohstressandhealthissuebrief2011324.pdf. [Google Scholar]
- Fischer A R, Shaw CM. African Americans’ mental health and perceptions of racist discrimination: The moderating effects of racial socialization experiences and self-esteem. Journal of Counseling Psychology. 1999;46:395–407. [Google Scholar]
- Folkman S. The case for positive emotions in the stress process. Anxiety, Stress, and Coping. 2008;21:3–14. doi: 10.1080/10615800701740457. [DOI] [PubMed] [Google Scholar]
- Folkman S, Moskowitz JT. Coping: Pitfalls and promise. Annual Review of Psychology. 2004;55:745–774. doi: 10.1146/annurev.psych.55.090902.141456. [DOI] [PubMed] [Google Scholar]
- Gee G C, Delva J, Takeuchi D T. Relationships between self-reported unfair treatment and prescription medication use, illicit drug use, and alcohol dependence among Filipino Americans. American Journal of Public Health. 2007;97:933–940. doi: 10.2105/AJPH.2005.075739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons F X, Etcheverry P E, Stock M L, Gerrard M, Weng C-Y, Kiviniemi M, O’Hara R E. Exploring the link between racial discrimination and substance use: What mediates? What buffers? Journal of Personality and Social Psychology. 2010;99:785–801. doi: 10.1037/a0019880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B F. Prevalence and correlates of alcohol use and DSM-IV alcohol dependence in the United States: Results of the National Longitudinal Alcohol Epidemiologic Survey. Journal of Studies on Alcohol. 1997;58:464–473. doi: 10.15288/jsa.1997.58.464. [DOI] [PubMed] [Google Scholar]
- Green S B, Babyak M A. Control of type I errors with multiple tests of constraints in structural equation modeling. Multivariate Behavioral Research. 1997;32:39–51. doi: 10.1207/s15327906mbr3201_2. [DOI] [PubMed] [Google Scholar]
- Greenfield T K. Ways of measuring drinking patterns and the difference they make: Experience with graduated frequencies. Journal of Substance Abuse. 2000;12:33–49. doi: 10.1016/s0899-3289(00)00039-0. [DOI] [PubMed] [Google Scholar]
- Greenfield T K, Kerr W C. Alcohol measurement methodology in epidemiology: Recent advances and opportunities. Addiction. 2008;103:1082–1099. doi: 10.1111/j.1360-0443.2008.02197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield T K, Midanik L T, Rogers J D. Effects of telephone versus face-to-face interview modes on reports of alcohol consumption. Addiction. 2000;95:277–284. doi: 10.1046/j.1360-0443.2000.95227714.x. [DOI] [PubMed] [Google Scholar]
- Greenfield TK, Nayak MB, Bond J, Ye Y, Midanik LT. Maximum quantity consumed and alcohol-related problems: Assessing the most alcohol drunk with two measures. Alcoholism: Clinical and Experimental Research. 2006;30:1576–1582. doi: 10.1111/j.1530-0277.2006.00189.x. [DOI] [PubMed] [Google Scholar]
- Groves RM. Nonresponse rates and nonresponse bias in household surveys. Public Opinion Quarterly. 2006;70:646–675. [Google Scholar]
- Hatch SL. Conceptualizing and identifying cumulative adversity and protective resources: Implications for understanding health inequalities. The Journals of Gerontology: Series B, Psychological Sciences and Social Sciences. 2005;60:S130–S134. doi: 10.1093/geronb/60.special_issue_2.s130. [DOI] [PubMed] [Google Scholar]
- Herd D. The influence of religious affiliation on sociocultural predictors of drinking among Black and White Americans. Substance Use & Misuse. 1996;31:35–63. doi: 10.3109/10826089609045797. [DOI] [PubMed] [Google Scholar]
- Herd DA. The effects of parental influences and respondents’ norms and attitudes on black and white adult drinking patterns. Journal of Substance Abuse. 1994;6:137–154. doi: 10.1016/s0899-3289(94)90169-4. [DOI] [PubMed] [Google Scholar]
- Hilton J. Race and ethnicity in fatal motor vehicle traffic crashes 1999–2004 (NHTSA Technical Report No. DOT HS 809 956) Washington, DC: National Center for Statistics and Analysis; 2006. National Highway Traffic and Safety Administration. Retrieved from http://www-nrd.nhtsa.dot.gov/Pubs/809956.PDF. [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covari-ance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Huckle T, Huakau J, Sweetsur P, Huisman O, Casswell S. Density of alcohol outlets and teenage drinking: Living in an alcogenic environment is associated with higher consumption in a metropolitan setting. Addiction. 2008;103:1614–1621. doi: 10.1111/j.1360-0443.2008.02318.x. [DOI] [PubMed] [Google Scholar]
- Hughes D. Correlates of African American and Latino parents’ messages to children about ethnicity and race: A comparative study of racial socialization. American Journal of Community Psychology. 2003;31:15–33. doi: 10.1023/a:1023066418688. [DOI] [PubMed] [Google Scholar]
- Kavanagh AM, Kelly MT, Krnjacki L, Thornton L, Jolley D, Subramanian SV, Bentley RJ. Access to alcohol outlets and harmful alcohol consumption: A multi-level study in Melbourne, Australia. Addiction. 2011;106:1772–1779. doi: 10.1111/j.1360-0443.2011.03510.x. [DOI] [PubMed] [Google Scholar]
- Keeter S, Kennedy C, Dimock M, Best J, Craighill P. Gauging the impact of growing nonresponse on estimates from a national RDD telephone survey. Public Opinion Quarterly. 2006;70:759–779. [Google Scholar]
- Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior. 1999;40:208–230. [PubMed] [Google Scholar]
- Keyes KM, Barnes DM, Bates LM. Stress, coping, and depression: Testing a new hypothesis in a prospectively studied general population sample of U.S.-born whites and blacks. Social Science and Medicine. 2011;72:650–659. doi: 10.1016/j.socscimed.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS. From psychological stress to the emotions: A history of changing outlooks. Annual Review of Psychology. 1993;44:1–22. doi: 10.1146/annurev.ps.44.020193.000245. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal and coping. New York, NY: Springer; 1984. [Google Scholar]
- Lewis TT, Everson-Rose SA, Powell LH, Matthews KA, Brown C, Karavolos K, Wesley D. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: The SWAN Heart Study. Psychosomatic Medicine. 2006;68:362–368. doi: 10.1097/01.psy.0000221360.94700.16. [DOI] [PubMed] [Google Scholar]
- Lindenberg CS, Strickland O, Solorzano R, Galvis C, Dreher M, Darrow VC. Correlates of alcohol and drug use among low-income Hispanic immigrant childbearing women living in the U.S.A. International Journal of Nursing Studies. 1999;36:3–11. doi: 10.1016/s0020-7489(98)00046-7. [DOI] [PubMed] [Google Scholar]
- Lloyd DA, Turner RJ. Cumulative lifetime adversities and alcohol dependence in adolescence and young adulthood. Drug and Alcohol Dependence. 2008;93:217–226. doi: 10.1016/j.drugalcdep.2007.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JK, Tuch SA, Roman PM. Problem drinking patterns among African Americans: The impacts of reports of discrimination, perceptions of prejudice, and “risky” coping strategies. Journal of Health and Social Behavior. 2003;44:408–425. [PubMed] [Google Scholar]
- Meyer I H, Schwartz S, Frost DM. Social patterning of stress and coping: Does disadvantaged social statuses confer more stress and fewer coping resources? Social Science & Medicine. 2008;67:368–379. doi: 10.1016/j.socscimed.2008.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midanik LT. Drunkenness, feeling the effects and 5+ measures. Addiction. 1999;94:887–897. doi: 10.1046/j.1360-0443.1999.94688711.x. [DOI] [PubMed] [Google Scholar]
- Midanik LT, Greenfield TK. Defining ‘current drinkers’ in national surveys: Results of the 2000 National Alcohol Survey. Addiction. 2003a;98:517–522. doi: 10.1046/j.1360-0443.2003.00344.x. [DOI] [PubMed] [Google Scholar]
- Midanik LT, Greenfield TK. Telephone versus in-person interviews for alcohol use: Results of the 2000 National Alcohol Survey. Drug and Alcohol Dependence. 2003b;72:209–214. doi: 10.1016/s0376-8716(03)00204-7. [DOI] [PubMed] [Google Scholar]
- Mulia N, Schmidt L, Bond J, Jacobs L, Korcha R. Stress, social support and problem drinking among women in poverty. Addiction. 2008a;103:1283–1293. doi: 10.1111/j.1360-0443.2008.02234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulia N, Ye Y, Greenfield TK, Zemore SE. Disparities in alcohol-related problems among white, black, and Hispanic Americans. Alcoholism: Clinical and Experimental Research. 2009;33:654–662. doi: 10.1111/j.1530-0277.2008.00880.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulia N, Ye Y, Zemore SE, Greenfield TK. Social disadvantage, stress, and alcohol use among black, Hispanic, and white Americans: Findings from the 2005 U.S. National Alcohol Survey. Journal of Studies on Alcohol and Drugs. 2008b;69:824–833. doi: 10.15288/jsad.2008.69.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B, Asparouhov T. Latent variable analysis with categorical outcomes: Multiple-group and growth modeling in Mplus. 2002 Mplus Web Notes: No. 4, Version 5, December 9, 2002. Retrieved from http://www.statmodel.com/download/webnotes/catNGLong.pdf. [Google Scholar]
- Muthén LK, Muthén B. Los Angeles, CA: Authors; 2011. Mplus user’s guide, Version 6. [Google Scholar]
- Muthén LK, Muthén BO. Los Angeles, CA: Authors; 2009. Mplus user’s guide, Version 5.21. [Google Scholar]
- Paradies Y. A systematic review of empirical research on self-reported racism and health. International Journal of Epidemiology. 2006;35:888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. Journal of Health and Social Behavior. 1981;22:337–356. [PubMed] [Google Scholar]
- Peirce RS, Frone MR, Russell M, Cooper ML. Relationship of financial strain and psychosocial resources to alcohol use and abuse: The mediating role of negative affect and drinking motives. Journal of Health and Social Behavior. 1994;35:291–308. [PubMed] [Google Scholar]
- Pérez DJ, Fortuna L, Alegría M. Prevalence and correlates of everyday discrimination among U.S. Latinos. Journal of Community Psychology. 2008;36:421–433. doi: 10.1002/jcop.20221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinel EC. Stigma consciousness: The psychological legacy of social stereotypes. Journal of Personality and Social Psychology. 1999;76:114–128. doi: 10.1037//0022-3514.76.1.114. [DOI] [PubMed] [Google Scholar]
- Pollack CE, Cubbin C, Ahn D, Winkleby M. Neighbourhood deprivation and alcohol consumption: Does the availability of alcohol play a role? International Journal of Epidemiology. 2005;34:772–780. doi: 10.1093/ije/dyi026. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale:A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Schulz A, Williams D, Israel B, Becker A, Parker E, James SA, Jackson J. Unfair treatment, neighborhood effects, and mental health in the Detroit metropolitan area. Journal of Health and Social Behavior. 2000;41:314–332. [PubMed] [Google Scholar]
- Scribner RA, Cohen DA, Fisher W. Evidence of a structural effect for alcohol outlet density: A multilevel analysis. Alcoholism: Clinical and Experimental Research. 2000;24:188–195. [PubMed] [Google Scholar]
- Stuber J, Galea S, Ahern J, Blaney S, Fuller C. The association between multiple domains of discrimination and self-assessed health: A multilevel analysis of Latinos and blacks in four low-income New York City neighborhoods. Health Services Research. 2003;38:1735–1760. doi: 10.1111/j.1475-6773.2003.00200.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoits PA. Stress, coping, and social support processes: Where are we? What next? Journal of Health and Social Behavior. 1995;35:53–79. [PubMed] [Google Scholar]
- Troxel WM, Matthews KA, Bromberger JT, Sutton-Tyrrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychology. 2003;22:300–309. doi: 10.1037/0278-6133.22.3.300. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Avison WR. Status variations in stress exposure: Implications for the interpretation of research on race, socioeconomic status, and gender. Journal of Health and Social Behavior. 2003;44:488–505. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Washington, DC: Author; 2005. The 2004 HHS poverty guidelines: One version of the [U.S.] federal poverty measure. Retrieved from http://aspe.hhs.gov/ poverty/04poverty.shtml. [Google Scholar]
- West C P. Race matters. New York, NY: Vintage Books; 1994. [Google Scholar]
- Williams DR, Lavizzo-Mourey R, Warren RC. The concept of race and health status in America. Public Health Reports. 1994;109:26–41. [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: Findings from community studies. American Journal of Public Health. 2003;93:200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Williams-Morris R. Racism and mental health: The African American experience. Ethnicity & Health. 2000;5:243–268. doi: 10.1080/713667453. [DOI] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Yen IH, Ragland DR, Greiner BA, Fisher JM. Racial discrimination and alcohol-related behavior in urban transit operators:Findings from the San Francisco Muni Health and Safety Study. Public Health Reports. 1999;114:448–458. doi: 10.1093/phr/114.5.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon Y-H, Yi H-Y. Liver cirrhosis mortality in the United States, 1970–2004[Surveillance Report #79] Arlington, VA: National Institute on Alcohol Abuse and Alcoholism; 2007. [PMC free article] [PubMed] [Google Scholar]
- Zemore SE, Karriker-Jaffe KJ, Keithly S, Mulia N. Racial prejudice and unfair treatment: Interactive effects with poverty and foreign nativity on problem drinking. Journal of Studies on Alcohol and Drugs. 2011;72:361–370. doi: 10.15288/jsad.2011.72.361. [DOI] [PMC free article] [PubMed] [Google Scholar]