Abstract
Objective:
A 14-year multiwave panel design was used to examine relationships between longitudinal alcohol-consumption patterns, especially persistent moderate use, and change in health-related quality of life among middle-aged and older adults.
Method:
A nationally representative sample of 5,404 community-dwelling Canadians ages 50 and older at baseline (1994/1995) was obtained from the longitudinal National Population Health Survey. Alcohol-consumption patterns were developed based on the quantity and frequency of use in the 12 months before the interview. Health-related quality of life was assessed with the Health Utilities Index Mark 3 (HUI3). Latent growth curve modeling was used to estimate the change in HUI3 for each alcohol pattern after adjusting for covariates measured at baseline.
Results:
Most participants showed stable alcohol-consumption patterns over 6 years. Persistent nonusers, persistent former users, those decreasing their consumption levels, and those with unstable patterns (i.e., U shaped and inverted U shaped) had lower HUI3 scores at baseline compared with persistent moderate drinkers. A more rapid decline in HUI3 scores than that observed for persistent moderate users was seen only in those with decreasing consumption (p < .001). In a subgroup identified as consistently healthy before follow-up, longitudinal drinking patterns were associated with initial HUI3 scores but not rates of change.
Conclusions:
Persistent moderate drinkers had higher initial levels of health-related quality of life than persistent nonusers, persistent former users, decreasing users, U-shaped users, and inverted U-shaped users. However, rates of decline over time were similar for all groups except those decreasing their consumption, who had a greater decline in their level of health-related quality of life than persistent moderate users.
The numbers and proportions of older adults are rapidly increasing in industrialized countries (Christensen et al., 2009). Most persons older than age 50 consume alcohol, as do large numbers of people over age 65 (e.g., Blazer and Wu, 2009). There are, however, inconsistent public health messages for alcohol use in older age groups. For example, the U.S. National Institute on Alcohol Abuse and Alcoholism (NIAAA) suggests that two or more standard drinks (i.e., more than 27.4 g of ethanol) per day (on average) put men older than 65 at risk for adverse health effects of alcohol (Moos et al., 2010; NIAAA, 2007). Similarly, in the United Kingdom, the Royal College of Psychiatrists recently recommended that the long-held “sensible limits” (i.e., 21 units or 168 g of ethanol for men and 14 units or 112 g of ethanol for women a week) should be reduced to a maximum of 1.5 units or 12 g of alcohol per day for all people 65 and older (Royal College of Psychiatrists, 2011). The U.S. Department of Agriculture (2010) defined one or two standard drinks per day for men as moderate drinking with no adjustment for older age. Moreover, the Department of Agriculture concluded that “an average daily intake of one to two drinks per day is associated with the lowest all cause mortality and a low risk of diabetes and coronary heart disease among middle-aged and older adults” (p. 5). Interestingly, several countries, including Canada (Butt et al., 2011), lack age-specific low-risk drinking guidelines. Indeed, a recent review of alcohol guidelines within and across countries demonstrates wide variation in recommendations for low-risk drinking (Latino-Martel et al., 2011).
Epidemiological studies generally indicate that alcohol consumption starts to decline in middle age (Platt et al., 2010). A meta-analysis of longitudinal U.S. studies found that average alcohol quantity significantly declined with age in older men but not in older women (Fillmore et al., 1991). Increasing morbidity with age may explain in part the decline in alcohol use (Shaper, 2011).
Importantly, numerous studies show that alcohol in excess is harmful to health (Giesbrecht et al., 2011; Latino-Martel et al., 2011; World Health Organization, 2010) but potentially beneficial in moderation (Byles et al., 2006; Kaplan et al., 2008; Ronksley et al., 2011; Stahre et al., 2006). Indeed, several studies using baseline alcohol-consumption levels point to an association between moderate consumption and better health-related quality of life (HRQL) (Kraemer et al., 2005; Østbye et al., 2002; Powers and Young, 2008), functional status (Chen and Hardy, 2009; Karlamangla et al., 2009), cognitive health (Lang et al., 2007), subjective well-being (Lang et al., 2007), mental health (Lang et al., 2007), and self-rated health (Turvey et al., 2006), as well as absence of chronic illness (Beulens et al., 2005; Bulpitt, 2005; Djoussé et al., 2007; Mukamal et al., 2008; Yin et al., 2007) and lower mortality risk (Emberson et al., 2005; Holahan et al., 2010; Sorock et al., 2006). However, although alcohol consumption in moderation may have beneficial effects regarding cardiovascular disease, it is associated with elevated risks for several cancers including those of the oral cavity, pharynx, larynx, esophagus, and liver (Latino-Martel et al., 2011; Rehm et al., 2010).
At least some of the confusion around the association between alcohol consumption and health stems from drinking levels being measured exclusively at one point in time. Recent investigations highlight the importance of assessing longitudinal alcohol-consumption patterns rather than basing consumption on data from one time point (Gee et al., 2007; Molander et al., 2010; Platt et al., 2010; Shaw et al., 2011). These studies show that about half of older adults remain in their respective alcohol-consumption patterns (i.e., abstinence, moderate, and heavy use), whereas the other half move between categories. For example, Platt et al. (2010) found that 21% of adults age 50 and older were steady drinkers, 29% were abstainers, 30% were sporadic drinkers, and 18% decreased, whereas 2% increased their consumption over a 14-year period. There remains little knowledge of the dynamics of alcohol consumption and its relationship to change in health.
Another source of confusion in the literature is the role of health status in alcohol consumption. A decline in health may prompt individuals to reduce their drinking behavior and thus exaggerate the health benefits of continued consumption. Studies have shown that former drinkers are in poorer health—with many being high risk drinkers at one time—compared with current drinkers or lifetime abstainers (Bond et al., 2004; Ferreira and Weems, 2008; Heuberger, 2009). Karlamangla et al. (2009) suggested that controlling for health status at baseline might alter conclusions regarding the relationship over time between alcohol and health. Furthermore, the strength of evidence on alcohol and health has been questioned, as several studies failed to control adequately for biases, such as combining former drinkers and lifetime abstainers, which is likely to inflate estimates of benefits among those who drink small amounts (Chikritzhs et al., 2009; Fillmore et al., 2007; Naimi et al., 2005).
In addition, most past work has used narrowly focused outcomes, such as cognitive function (Bond et al., 2004) or diabetes (Beulens et al., 2005). With few exceptions (Chen and Hardy, 2009), studies generally have not considered the broader effects of alcohol on health or well-being. Yet such investigations are invaluable because the impacts of alcohol can be compared with those of other drugs (or foods) and with health-related behaviors (such as smoking or physical activity).
In light of these concerns and to address the issue of declines in health status leading to reductions in alcohol consumption, the primary aim of this study was to explore the relationship between longitudinal patterns of alcohol use (especially “persistent moderate use”) and changes in HRQL among middle-aged and older adults. The study sought to assess the effect of alcohol intake patterns on HRQL over a 14-year follow-up period using the Canadian National Population Health Survey (NPHS) (Statistics Canada, 2010), which includes extensive measures of drinking behavior and health collected biennially. The objectives were to (a) estimate the prevalence of drinking patterns from mid- to later life; (b) assess the association between persistent moderate drinking patterns and HRQL; and (c) among individuals in consistently good health before follow-up, examine the association between persistent moderate alcohol consumption and trajectories of HRQL.
Method
Data source
Data for this study were derived from the 1994/1995 to 2008/2009 NPHS (Statistics Canada, 2010). The longitudinal NPHS consisted of 17,276 members of private households in 1994/1995 ages 12 and older from all provinces, with the exclusion of individuals on Indian Reserves, Canadian Forces Bases, and some remote areas in Québec and Ontario (Swain et al., 1999).
In the initial cycle of the NPHS (i.e., 1994/1995), the sample was created by first selecting households and then within each household choosing one member age 12 and older to be the longitudinal respondent. The NPHS is based on a complex design, with stratification and multiple stages of selection and unequal probabilities of selection of respondents (Tambay and Catlin, 1995). The NPHS response rate at baseline was 83.6%. Panel members who died or who moved to health care institutions remain in the longitudinal sample. Sample size decreased slightly over time because of nonresponse, refusal, and inability to locate the subject. The main cause of attrition was refusal to participate. Despite the attrition, the longitudinal sample remains representative of the 1994/1995 Canadian general population. The cumulative attrition rate (36.4% at the last cycle in 2006/2007) is based on those who completed the questionnaire in all cycles and includes panel members who died.
In Cycle 1, 75% of the interviews with the longitudinal respondents were conducted in person and the remainder by telephone. Starting with Cycle 2, 95% of the interviews were conducted using computer-assisted telephone interviewing and the remainder in person. All interviewers were hired and trained by Statistics Canada. Alcohol data collected in person were very similar to those obtained via telephone (St-Pierre and Beland, 2004). The present study focuses on 5,404 participants who were 50 years old and older at baseline.
Measures
Cross-sectional alcohol-consumption categories.
The NPHS alcohol measures correspond to the Dawson and Room (2000) summary of recommendations and are compatible with suggestions in the World Health Organization (2000) report International Guide for Monitoring Alcohol. Respondents were categorized at each cycle according to a classification scheme based on the quantity and frequency of alcohol use in the 12 months before the interview.
Alcohol categories were chosen and adapted following Molander et al. (2010), Powers and Young (2008), and Lin et al. (2011). Many studies define moderate and heavy alcohol use with average daily consumption based on the weekly or monthly number of drinks (e.g., Lang et al., 2007; Østbye et al., 2002; Powers and Young 2008; Shaw et al., 2011). The NPHS provides a more precise set of questions regarding the number of drinks on each day of the week. Thus, we used the total number of drinks per week and the maximum number of drinks per day to define moderate and heavy drinkers. Using this scheme, moderate drinkers were defined as those having 1–14 drinks per week with no more than 3 on any day for women and no more than 4 on any day for men. More than 85% of moderate drinkers had 7 or fewer drinks per week. Heavy drinkers were those who had more than 14 drinks per week or more than 3 or 4 on any day for women and men, respectively. The average number of drinks per week among heavy drinkers was 18. Given that meeting either of two criteria would classify the respondent as a heavy drinker, it is noteworthy that among those in this drinking group, we found that 50% of the cases would have averaged 14 drinks or fewer per week but were also having more than 3 or 4 drinks on any day for women and men, respectively, on at least one day during the week. This group might have been classified as moderate drinkers in other studies. The other alcohol categories included lifelong abstainers (never), former drinkers (no drinks in the past 12 months), and infrequent drinkers (<1 drink per week).
Longitudinal alcohol-consumption patterns.
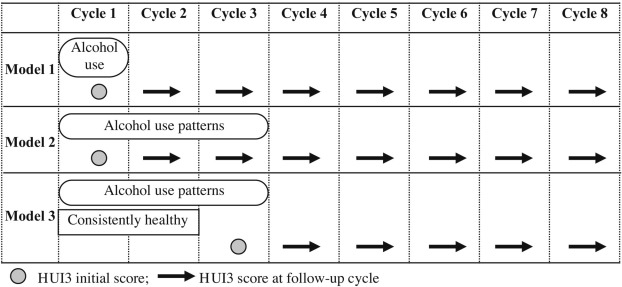
Longitudinal alcohol patterns were based on the change, if any, in consumption over three cycles (6 years) to obtain the maximum number of patterns possible (see Sensitivity analyses on p. 587). Several alcohol use patterns were established. Stable consumption includes participants who remained in their alcohol-consumption category for 6 years (i.e., persistent nondrinker, persistent former drinker, persistent infrequent drinker, persistent moderate drinker, and persistent heavy drinker). Unstable patterns were those who decreased, increased, or had a U-shaped or an inverted U-shaped drinking pattern. Although we do not account for the drinking fluctuation within the persistent moderate and heavy drinking categories, the change in the total amount of drinks from Cycle 1 to Cycle 2 and from Cycle 2 to Cycle 3 averaged less than one drink for each of these two patterns. The few illogical alcohol-consumption patterns (e.g., a drinker in one cycle reported never having consumed alcohol in a later cycle) were adjusted with the Fellegi–Holt principle (Fellegi and Holt, 1976). The conceptual framework and analytic timeline are graphically depicted in Figure 1.
Figure 1.
Conceptual and analytic framework. HUI3 = Health Utilities Index Mark 3.
Consistently healthy group.
Participants defined as “consistently healthy” were those who reported no health care professional diagnoses of heart disease, cancer, stroke, or diabetes for the first two cycles (Figure 1). These conditions were chosen because they may lead to changes in health behavior, such as reduced alcohol use (Chiuve et al., 2006; Khaw et al., 2008; Morley and Flaherty, 2002; Zanjani et al., 2006). In addition, consistently healthy participants had to report being in good to excellent health in the first two cycles (response options for self-rated health were excellent, very good, good, fair, or poor). See Sensitivity analyses below regarding the use of two versus three cycles of consistently good health. Cycle 3 (1998/1999) was used as the baseline for this analysis (Figure 1).
Control variables.
The control variables included baseline age, gender, education (<high school vs. ≥high school), household income (<Can. $15,000 vs. ≥Can. $15,000), marital status (married vs. not married), smoking (current/occasional smoker, former smoker vs. never smoker), potentially life-threatening illnesses (high blood pressure, diabetes, heart disease, cancer, and/or stroke) (Ferraro and Farmer, 1999), other chronic illness (allergies, asthma, arthritis/rheumatism, back problems, migraine, chronic bronchitis, sinusitis, epilepsy, stomach/intestinal ulcers, urinary incontinence, Alzheimer's/dementia, cataracts, glaucoma, and/or other), body mass index, physical activity, and a nonspecific psychological distress measure (Kessler et al., 2002). Physical activity was assessed with a continuous measure of energy expenditure (kcal/kg/day), which was based on the frequency and duration of 20 leisure-time activities (e.g., walking for exercise, yoga) over the previous 3 months (Statistic Canada, 2010). Nonspecific psychological distress was measured with six items on a 5-point Likert scale, ranging from all of the time (4) to none of the time (0). The participants indicated the frequency in the past month that they felt “so sad that nothing could cheer you up,” “nervous,” “restless or fidgety,” “hopeless,” “worthless,” or that “everything was an effort” (Kessler et al., 2002).
Outcome variable.
HRQL was ascertained with the widely used Health Utilities Index Mark 3 (HUI3; Feeny et al., 2002). The HUI3 includes a health-status description system based on eight dimensions or attributes of health: vision, hearing, speech, ambulation, dexterity, emotion, cognition, and pain/discomfort. There are five or six levels per attribute, ranging from no problem through severe disability.
Overall, HUI3 scores range from -.36 (highest possible level of disability across all attributes) to 1.00 (perfect health). The negative scores for HUI3 indicate health states viewed as being worse than dead. Those who died during the course of the study were assigned an HUI3 score of 0 at the cycle of their death and censored thereafter. There is substantial evidence on the construct validity of HUI3 in population health and clinical studies, including studies of people with chronic conditions that are associated with alcohol consumption (liver disease, type 2 diabetes, dementia, impaired mental health, and heart disease) (Asakawa et al., 2008; Bondini et al., 2007; Feeny et al., 2009, 2012; Fisk et al., 2005; Garster et al., 2009; Grootendorst et al., 2000; Jones et al., 2005; Kavirajan et al., 2009; Maddigan et al., 2004, 2006; Marra et al., 2005; Revicki et al., 2008; Wilkins, 2006; Younossi et al., 2001), and the scoring procedures can be found elsewhere (Feeny et al., 2002, 2004). Differences (or changes) of .03 or more in the overall HUI3 score are important clinically (Drummond, 2001; Grootendorst et al., 2000; Horsman et al., 2003). Ranges of overall HUI3 scores that correspond to no, mild, moderate, and severe disability are described elsewhere (Feeny et al., 2004; Feng et al., 2009).
Statistical analysis
Following the assessment of patterns of alcohol consumption, latent growth curve modeling was then used to estimate the change in HUI3 for each pattern after adjusting for covariates measured at baseline, which were centered on their respective means. In this approach, the outcome variable is each person's HRQL at each available cycle. It is assumed that the average person's HRQL declines linearly over the follow-up period. Participants’ baseline alcoholconsumption category and their alcohol use pattern, respectively, are used to predict the intercept and the slope of the line relating HRQL to cycle of follow-up (after adjustment for covariates). The models estimate means and variances for intercept and slope, respectively. The mean of the intercept represents the population's predicted baseline value of HRQL. The mean of the slope is the prediction of the rate at which HRQL declines over time as people are aging. Variances are estimated recognizing that responses are “nested” within people. Variance estimates, which incorporate the complex sampling procedure, measure the extent to which intercepts and slopes, respectively, differ among participants. Chief interest lies in statistical significance (and clinical importance) of model coefficients connecting baseline alcohol-consumption category and longitudinal alcohol use pattern, respectively, to the intercept and slope. Coefficients pertaining to the intercept reflect the influence of alcohol consumption on baseline HRQL. Conversely, coefficients pertaining to slope reflect the influence of alcohol consumption on change over time in HRQL. In effect, the coefficients pertaining to slope reflect group by time interactions.
Three models were tested. The first model (“baseline category predictor”) assessed the effect of baseline alcohol category on the intercept (baseline average) and slope (change over time) of HUI3 over the 14 years, adjusting for the covariates. The second model (“pattern predictor”) estimated the effect of the alcohol use patterns on the change in HUI3 over the 14 years. The third model (“consistently healthy group”) tested the effects of the alcohol use patterns on the intercept and slope of HUI3 over the 10 years of follow-up among those who were in the consistently healthy group. In all models, moderate consumption (or persistent moderate pattern) was used as the reference group. All analyses were weighted. The balanced repeated replication method in Mplus (Muthén and Muthén, 1998–2010) was used to adjust for the complex sampling design. Bootstrap weights provided by Statistics Canada were used. Following Bollen and Long (1993), goodness of fit was measured by the root mean square error of approximation.
Results
Of the 5,404 participants ages 50 and older, only 3% were missing alcohol information at baseline. Fifty-four percent of participants were women. The majority of the sample were aged 50 to 64 (55%), were married (70%), were in middle to higher income brackets (80%), and had at least a high school education (56%) (Table 1). More than one third had a life-threatening chronic health problem, nearly half reported other chronic illnesses, and 37% reported being a current or occasional smoker at Cycle 1.
Table 1.
Characteristics of participants 50 years of age and older
| Variable | n (%) or M(SE) |
| Male, n (%) | 2,322 (45.9) |
| ≥65 years, n (%) | 2,740 (44.5) |
| Married,n(%) | 3,140(69.6) |
| Education, n (%) | |
| <High school | 2,585 (44.2) |
| ≥High school | 2,801 (55.8) |
| Income,a,bn (%) | |
| Lower household income (<$ 15,000) | 1,415 (2.2) |
| Middle-higher household income (≥$ 15,000) | 3,689(79.8) |
| Health status | |
| Presence of life-threatening chronic conditions, n (%) | 2,056 (35.9) |
| Presence of other, n (%) chronic conditions, n (%) | 2,724 (47.5) |
| Former smoker, n (%) | 2,147(41.1) |
| Current/occasional smoker, n (%) | 1,960 (37.4) |
| Physical activity (kcal/kg/day), M (SE) | 1.4 (0.03) |
| Body mass index (kg/m2), M (SE) | 26.0 (0.08) |
| Nonspecific psychological distress (range: 0-24), M (SE) | 2.9 (0.06) |
Monetary values are in Canadian dollars;
based on one to two persons living in the household.
At baseline, 13% were categorized in cross-section as abstainers, 18% as former, 30% as infrequent, 32% as moderate, and 7% as heavy drinkers. Table 2 shows the patterns of alcohol use over 6 years. Most participants remained in their respective alcohol categories for over 6 years. Many of the fluctuations occurred in adjacent categories. Most who changed category reported a decrease in alcohol consumption. For example, 26% of moderates became infrequent users, and 36% of heavy drinkers became moderate users. Overall, 31% of older adults decreased their consumption over the 6-year period, 16% increased (mostly from infrequent to moderate), and 11% maintained a moderate level. The remainder had other longitudinal patterns (Table 2).
Table 2.
Alcohol patterns over 6 years
| Variable | n | % | HUI3 at baseline, M |
| Persistent nonuser | 382 | 6.1 | .78 |
| Persistent former user | 486 | 7.6 | .74 |
| Persistent infrequent user | 377 | 6.9 | .86 |
| Persistent moderate user | 518 | 11.4 | .89 |
| Persistent heavy user | 72 | 1.6 | .86 |
| Decreasing user | 1,773 | 31.4 | .78 |
| Increasing user | 810 | 15.8 | .84 |
| U-shaped user | 473 | 10.2 | .80 |
| Inverted U-shaped user | 476 | 9.2 | .79 |
Note: HUI3 = Health Utilities Index Mark 3.
The means of the HUI3 scores at baseline in Models 1 and 2 were .83 (Tables 3 and 4), suggesting the presence of mild disability. In Models 1 and 2, HUI3 scores decreased on average by .05 per 2-year period, which is expected in an aging cohort. Variances of intercept and slope were statistically significant, suggesting between-person differences in baseline HUI3 scores and in rates of change.
Table 3.
Influence of baseline alcohol categories on health-related quality of life over time
| Model descriptor | Model1 |
| Baseline predictor | |
| Follow-up years | 1994–2008 |
| n | 5,404 |
| Variable | Estimates |
| Effect of alcohol on HUI3 at initial follow-up | |
| Lifetime abstainer | −.044*** |
| Former drinker | −.053*** |
| Infrequent drinker | −.008 |
| Moderate drinker | Referent |
| Heavy drinker | −.003 |
| Effect of alcohol on HUI3 rate of change | |
| Lifetime abstainer | −.011** |
| Former drinker | −.009* |
| Infrequent drinker | −.006* |
| Moderate drinker | Referent |
| Heavy drinker | −.009 |
| HUI3 at initial follow-up | .83*** |
| HUI3 score rate of change | −.048*** |
| Variance of HUI3 at initial follow-up | .022*** |
| Variance of HUI3 rate of change | .002*** |
| RMSEA | .048 |
Notes: Models were adjusted for age, gender, marital status, education, household income, smoking, chronic illness, body mass index, physical activities, and nonspecific psychological distress. HUI3 = Health Utilities Index Mark 3; RMSEA = root mean square error of approximation.
p < .05;
p < .01;
p < .001
Table 4.
Influence of 6-year alcohol patterns on health-related quality of life over time among all participants and those in consistently good health
| Model descriptor | Model 2 | Model 3 |
| Pattern predictor | Consistently healthy group | |
| Follow-up years | 1998–2008 | 1994–2008 |
| n | 5,404 | 2,645 |
| Variable | Estimates | Estimates |
| Effect of alcohol on HUI3 at initial follow-up | ||
| Persistent nonuser | −.059** | −.065** |
| Persistent former user | −.078*** | −.023 |
| Persistent infrequent user | −.020 | −.034* |
| Persistent moderate user | Referent | Referent |
| Persistent heavy user | −.012 | −.051 |
| Decreasing user | −.108*** | −.085*** |
| Increasing user | −.014 | −.011 |
| U-shaped user | −.051** | −.027 |
| Inverted U-shaped user | −.069*** | −.066*** |
| Effect of alcohol on HUI3 rate of change | ||
| Persistent nonuser | −.006 | −.001 |
| Persistent former user | −.007 | −.009 |
| Persistent infrequent user | −.005 | .003 |
| Persistent moderate user | Referent | Referent |
| Persistent heavy user | −.016 | −.021 |
| Decreasing user | −.025*** | −.003 |
| Increasing user | −.006 | −.008 |
| U-shaped user | .001 | −.001 |
| Inverted U-shaped user | −.008 | .000 |
| HUI3 at initial follow-up | .828*** | .864*** |
| HUI3 score rate of change | −.051*** | −.046*** |
| Variance of HUI3 at initial follow-up | .021*** | .020*** |
| Variance of HUI3 rate of change | .002*** | .003*** |
| RMSEA | .048 | .038 |
Notes: Models were adjusted for age, gender, marital status, education, household income, smoking, chronic illness, body mass index, physical activities, and nonspecific psychological distress. HUI3 score = Health Utilities Index Mark 3; RMSEA = root mean square error of approximation.
p < .05;
p < .01;
p < .001.
Model 1 assessed the impact of baseline alcohol category on the slope and the intercept of HUI3 scores after adjusting for covariates. Lifetime abstainers and former drinkers had lower HUI3 scores at baseline than moderate drinkers. Lifetime abstainers, former drinkers, and infrequent drinkers experienced a greater decline in HUI3 compared with moderate drinkers. The model fit the data well. Namely, the root mean square error of approximation was .048 which, given the large sample size, is considered by MacCallum et al. (1996) to be indicative of close fit.
Models 2 and 3 are presented in Table 4. Model 2 shows the effect of alcohol patterns on HUI3 over time. Persistent nonusers, persistent former users, those decreasing their consumption levels, and those with unstable patterns (i.e., U shaped and inverted U shaped) had lower HUI3 scores at baseline compared with persistent moderates. Only those with decreasing consumption levels had a greater decline in their HUI3 scores than persistent moderate users. Model fit was good and not notably different from that of Model 1.
Model 3 (Table 4) tested the effect of alcohol-consumption patterns on HUI3 among those who reported being in consistently good health. As expected, these participants had high HUI3 scores at the start of their follow-up. Alcohol patterns only affected baseline HUI3 scores and not the rates of change. Specifically, persistent nonusers, persistent infrequent users, those who reduced their consumption levels, and those with an inverted U-shaped pattern of use had lower HUI3 scores at baseline. On the other hand, trajectories of HRQL over time for these participants could not be distinguished from those of the persistent moderate users. Model fit was also good.
Sensitivity analyses
Sensitivity analyses tested whether using alcohol patterns over 4 or 6 years or being in consistent good health for 4 or 6 years would affect results. Because results were similar, a block of 6 years was chosen to describe the alcohol patterns, and a block of 4 years was used for the consistently healthy comparison group. Because HUI3 can itself reflect chronic illness, additional analyses compared models with and without chronic conditions. The relationship between alcohol and HUI3, however, was not altered (data not shown) in these analyses. Moreover, models were run including and excluding decedents. The results without the decedents showed a weakened relationship between alcohol and HUI3 (data not shown). This is not surprising because removing the decedents raises the overall HRQL level of the sample and can produce overly optimistic heath profiles (Orpana et al., 2009).
Discussion
This project is the first nationally representative longitudinal study of Canadians to examine relationships between patterns of alcohol consumption and trajectories of HRQL in middle age to older adulthood, including those who were relatively healthy at baseline. The findings suggest that alcohol-consumption patterns are associated with HRQL, but the rate of decline in HRQL is similar for all drinking patterns except for persons who decreased their consumption. In general, the alcohol patterns did not predict decline in HRQL but were associated with the initial level of HRQL. Moderate alcohol use did not have a measurable deleterious effect on change in HRQL over time. Indeed, if anything, continued moderate consumption during middle and later life may have been beneficial. On the other hand, the present findings offer no support for initiating moderate alcohol consumption in later life to achieve positive health.
The study's longitudinal design is important because impaired health is associated with reduction in drinking or with infrequent drinking (Liang and Chikritzhs, 2011) such that causality and reverse causality are difficult to disentangle (Shaper, 2011). Specifically, there is evidence (e.g., Liang and Chikritzhs, 2011) that health status declines lead to reductions in alcohol consumption. As expected, then, former drinkers in the present study had lower baseline HRQL scores than moderate drinkers, who were both statistically significant and quantitatively important clinically. Even among the consistently healthy subgroup, the former drinkers had lower HRQL at start of follow-up (but these differences were neither statistically significant nor clinically important). Similarly, it was also expected (Liang and Chikritzhs, 2011) that participants with decreasing alcoholconsumption patterns would have low baseline HRQL. Persons with decreasing alcohol consumption showed accelerated decline in HRQL during follow-up. These results are consistent with the idea that declines in health trigger reductions in consumption of alcohol (Liang and Chikritzhs, 2011).
The long duration of the study allowed for assessment of consistent good health for a period of at least 4 years. Consequently, it was possible to identify individuals highly likely to be in good health at the start of follow-up. Even among those in consistently good health, moderate drinkers reported better HRQL at the start of their follow-up than did nondrinkers, infrequent drinkers, and heavy drinkers. There was, however, no relationship between alcohol-consumption patterns and rate of decline in HRQL during the healthy group's follow-up. In other words, the age-related decline in moderate drinkers’ HRQL (Orpana et al., 2009) over the study period looked no different than that of respondents in other drinking categories, including abstainers. Among these relatively healthy participants, variations in HRQL trajectories from middle age through older adulthood did not appear to be affected by alcohol-consumption patterns that may have been established at a younger age.
Several limitations should be kept in mind when interpreting the findings. First, the cumulative attrition rate over the eight cycles was 36.4% (mostly because of refusal to participate). Second, alcohol intake and health status measures were self-reported with potential reporting biases (e.g., underreporting alcohol intake because of social desirability). There may also be recall bias if some participants were not able to accurately remember their alcohol intake (e.g., how many drinks on each day of the previous week). Third, the survey did not collect information on the size of or on the absolute alcohol level within each drink. Similarly, there were no data regarding the type of beverage consumed (i.e., beer, wine, or distilled spirits). Fourth, healthy participants were those who reported no health care professional diagnoses of heart disease, cancer, stroke, and/or diabetes (first two cycles) and being consistently in good to excellent self-reported health. Data on other chronic conditions, which may be related to alcohol use, were not available in the NPHS.
Despite these limitations, the strengths of this study lie in the prospective population-based design, large sample, high participation rate, and long follow-up period of the NPHS. Of note, the biennial nature of the survey captured transient changes in drinking (a problem found in other studies with long follow-up periods—see Molander et al., 2010). Furthermore, the study examined an important demographic subgroup that has often been overlooked when examining alcohol use throughout the life course.
It also needs to be appreciated that the study began some 2 decades ago; therefore, participants represent cohorts born in the middle of the last century. Therefore, some prevalence data may seem anomalous by current standards. For example, the percentage of current or former smokers was much greater than would be found today. However, a comparison of estimates for persons age 50 years and older, obtained from the 1994 U.S. National Survey on Drug Use and Health (U.S. Department of Health and Human Services, 2008) and the 1994 Canadian NPHS, showed that the rates of current and former smokers (77% and 78%, respectively) and lifetime alcohol abstinence (11% and 13%, respectively) were virtually identical. It is important to note that the National Survey on Drug Use and Health and NPHS used comparable smoking behavior and alcohol-consumption questions.
In summary, this study found that alcohol consumption (regardless of quantity and frequency) is generally not associated with accelerated decline in HRQL among older adults. These findings have important public policy implications regarding current efforts to modify established drinking guideline recommendations for older people (Shaper, 2011). Effective public health measures require detailed understanding of the alcohol and health burden over the life course. Specifically, future longitudinal research involving younger populations is needed to understand relationships between alcohol-consumption patterns early in life and health status on entering middle age.
Acknowledgments
The authors gratefully acknowledge the help of Margaret King and Claude Nadeau with this article.
Footnotes
This research was supported by National Institute on Aging Grant AG33796.
References
- Asakawa K, Rolfson D, Senthilselvan A, Feeny D, Johnson JA. Health Utilities Index Mark 3 showed valid in Alzheimer disease, arthritis, and cataracts. Journal of Clinical Epidemiology. 2008;61:733–739. doi: 10.1016/j.jclinepi.2007.09.007. [DOI] [PubMed] [Google Scholar]
- Beulens JWJ, Stolk RP, van der Schouw YT, Grobbee DE, Hendriks HFJ, Bots ML. Alcohol consumption and risk of type 2 diabetes among older women. Diabetes Care. 2005;28:2933–2938. doi: 10.2337/diacare.28.12.2933. [DOI] [PubMed] [Google Scholar]
- Blazer DG, Wu LT. The epidemiology of at-risk and binge drinking among middle-aged and elderly community adults: National Survey on Drug Use and Health. American Journal of Psychiatry. 2009;166:1162–1169. doi: 10.1176/appi.ajp.2009.09010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA, Long SJ. Testing structural equation models. Newbury Park, CA: Sage; 1993. [Google Scholar]
- Bond GE, Burr R, McCurry SM, Rice MM, Borenstein AR, Kukull WA, Larson EB. Alcohol, gender, and cognitive performance: a longitudinal study comparing older Japanese and non- Hispanic white Americans. Journal of Aging and Health. 2004;16:615–664. doi: 10.1177/0898264304268587. [DOI] [PubMed] [Google Scholar]
- Bondini S, Kallman J, Dan A, Younoszai Z, Ramsey L, Nader F, Younossi ZM. Health-related quality of life in patients with chronic hepatitis B. Liver International. 2007;27:1119–1125. doi: 10.1111/j.1478-3231.2007.01558.x. [DOI] [PubMed] [Google Scholar]
- Bulpitt CJ. How many alcoholic drinks might benefit an older person with hypertension? Journal of Hypertension. 2005;23:1947–1951. doi: 10.1097/01.hjh.0000184408.97385.bb. [DOI] [PubMed] [Google Scholar]
- Butt P, Beirness D, Gliksman L, Paradis C, Stockwell T. Alcohol and health in Canada: A summary of evidence and guidelines for low risk drinking. Ottawa, Ontario: Canadian Centre on Substance Abuse; 2011. [Google Scholar]
- Byles J, Young A, Furuya H, Parkinson LA. A drink to healthy aging: The association between older women's use of alcohol and their health-related quality of life. Journal of the American Geriatrics Society. 2006;54:1341–1347. doi: 10.1111/j.1532-5415.2006.00837.x. [DOI] [PubMed] [Google Scholar]
- Chen LY, Hardy CL. Alcohol consumption and health status in older adults: A longitudinal analysis. Journal of Aging and Health. 2009;21:824–847. doi: 10.1177/0898264309340688. [DOI] [PubMed] [Google Scholar]
- Chikritzhs T, Fillmore K, Stockwell T. A healthy dose of scepticism: Four good reasons to think again about protective effects of alcohol on coronary heart disease. Drug and Alcohol Review. 2009;28:441–444. doi: 10.1111/j.1465-3362.2009.00052.x. [DOI] [PubMed] [Google Scholar]
- Chiuve SE, McCullough ML, Sacks FM, Rimm EB. Healthy lifestyle factors in the primary prevention of coronary heart disease among men: Benefits among users and nonusers of lipid-lowering and antihypertensive medications. Circulation. 2006;114:160–167. doi: 10.1161/CIRCULATIONAHA.106.621417. [DOI] [PubMed] [Google Scholar]
- Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: The challenges ahead. The Lancet. 2009;374:1196–1208. doi: 10.1016/S0140-6736(09)61460-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Room R. Towards agreement on ways to measure and report drinking patterns and alcohol-related problems in adult general population surveys: The Skarpö conference overview. Journal of Substance Abuse. 2000;12:1–21. doi: 10.1016/s0899-3289(00)00037-7. [DOI] [PubMed] [Google Scholar]
- Djoussé L, Biggs ML, Mukamal KJ, Siscovick DS. Alcohol consumption and type 2 diabetes among older adults: The Cardiovascular Health Study. Obesity. 2007;15:1758–1765. doi: 10.1038/oby.2007.209. [DOI] [PubMed] [Google Scholar]
- Drummond M. Introducing economic and quality of life measurements into clinical studies. Annals of Medicine. 2001;33:344–349. doi: 10.3109/07853890109002088. [DOI] [PubMed] [Google Scholar]
- Emberson JR, Shaper AG, Wannamethee SG, Morris RW, Whincup PH. Alcohol intake in middle age and risk of cardiovascular disease and mortality: Accounting for intake variation over time. American Journal of Epidemiology. 2005;161:856–863. doi: 10.1093/aje/kwi111. [DOI] [PubMed] [Google Scholar]
- Feeny D, Furlong W, Saigal S, Sun J. Comparing directly measured standard gamble scores to HUI2 and HUI3 utility scores: Group- and individual-level comparisons. Social Science & Medicine. 2004;58:799–809. doi: 10.1016/s0277-9536(03)00254-5. [DOI] [PubMed] [Google Scholar]
- Feeny D, Furlong W, Torrance GW, Goldsmith CH, Zhu Z, DePauw S, Boyle M. Multiattribute and single-attribute utility functions for the Health Utilities Index Mark 3 system. Medical Care. 2002;40:113–128. doi: 10.1097/00005650-200202000-00006. [DOI] [PubMed] [Google Scholar]
- Feeny D, Huguet N, McFarland BH, Kaplan MS. The construct validity of the Health Utilities Index Mark 3 in assessing mental health in population health surveys. Quality of Life Research. 2009;18:519–526. doi: 10.1007/s11136-009-9457-3. Erratum in: 2009. Quality of Life Research, 18, 667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeny D, Spritzer K, Hays RD, Liu H, Ganiats TG, Kaplan RM, Fryback DG. Agreement about identifying patients who change over time: Cautionary results in cataract and heart failure patients. Medical Decision Making. 2012;32:273–286. doi: 10.1177/0272989X11418671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fellegi IP, Holt D. A systematic approach to automatic edit and imputation. Journal of the American Statistical Association. 1976;71:17–35. [Google Scholar]
- Feng Y, Bernier J, McIntosh C, Orpana H. Validation of disability categories derived from Health Utilities Index Mark 3 scores. Health Reports. 2009;20:43–45. [PubMed] [Google Scholar]
- Ferraro KF, Farmer MM. Utility of health data from social surveys: Is there a gold standard for measuring morbidity? American Sociological Review. 1999;64:303–315. [Google Scholar]
- Ferreira MP, Weems MK. Alcohol consumption by aging adults in the United States: Health benefits and detriments. Journal of the American Dietetic Association. 2008;108:1668–1676. doi: 10.1016/j.jada.2008.07.011. [DOI] [PubMed] [Google Scholar]
- Fillmore KM, Hartka E, Johnstone BM, Leino EV, Motoyoshi M, Temple MT. A meta-analysis of life course variation in drinking. British Journal of Addiction. 1991;86:1221–1268. doi: 10.1111/j.1360-0443.1991.tb01702.x. [DOI] [PubMed] [Google Scholar]
- Fillmore KM, Stockwell T, Chikritzhs T, Bostrom A, Kerr W. Moderate alcohol use and reduced mortality risk: Systematic error in prospective studies and new hypotheses. Annals of Epidemiology. 2007;17:S16–S23. doi: 10.1016/j.annepidem.2007.01.005. [DOI] [PubMed] [Google Scholar]
- Fisk JD, Brown MG, Sketris IS, Metz LM, Murray TJ, Stadnyk KJ. A comparison of health utility measures for the evaluation of multiple sclerosis treatments. Journal of Neurology, Neurosurgery, and Psychiatry. 2005;76:58–63. doi: 10.1136/jnnp.2003.017897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garster NC, Palta M, Sweitzer NK, Kaplan RM, Fryback DG. Measuring health-related quality of life in population-based studies of coronary heart disease: Comparing six generic indexes and a disease-specific proxy score. Quality of Life Research. 2009;18:1239–1247. doi: 10.1007/s11136-009-9533-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Liang J, Bennett J, Krause B, Kobayashi E, Fukaya T, Sugihara Y. Trajectories of alcohol consumption among older Japanese followed from 1987–1999. Research on Aging. 2007;29:323–347. [Google Scholar]
- Giesbrecht N, Stockwell T, Kendall P, Strang R, Thomas G. Alcohol in Canada: Reducing the toll through focused interventions and public health policies. Canadian Medical Association Journal. 2011;183:450–455. doi: 10.1503/cmaj.100825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grootendorst P, Feeny DH, Furlong W. Health Utilities Index Mark 3: Evidence of construct validity for stroke and arthritis in a population health survey. Medical Care. 2000;38:290–299. doi: 10.1097/00005650-200003000-00006. [DOI] [PubMed] [Google Scholar]
- Heuberger RA. Alcohol and the older adult: A comprehensive review. Journal of Nutrition for the Elderly. 2009;28:203–235. doi: 10.1080/01639360903140106. [DOI] [PubMed] [Google Scholar]
- Holahan CJ, Schutte KK, Brennan PL, Holahan CK, Moos BS, Moos RH. Late-life alcohol consumption and 20-year mortality. Alcoholism: Clinical and Experimental Research. 2010;34:1961–1971. doi: 10.1111/j.1530-0277.2010.01286.x. [DOI] [PubMed] [Google Scholar]
- Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index (HUI): Concepts, measurement properties and applications. Health and Quality of Life Outcomes, 1. 2003:54. doi: 10.1186/1477-7525-1-54. Retrieved from http:// www.hqlo.com/content/1/1/54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CA, Feeny D, Eng K. Test-retest reliability of health utilities index scores: Evidence from hip fracture. International Journal of Technology Assessment in Health Care. 2005;21:393–398. doi: 10.1017/s0266462305050518. [DOI] [PubMed] [Google Scholar]
- Kaplan MS, Huguet N, Orpana H, Feeny D, McFarland BH, Ross N. Prevalence and factors associated with thriving in older adulthood: A 10-year population-based study. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2008;63:1097–1104. doi: 10.1093/gerona/63.10.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlamangla AS, Sarkisian CA, Kado DM, Dedes H, Liao DH, Kim S, Moore AA. Light to moderate alcohol consumption and disability: Variable benefits by health status. American Journal of Epidemiology. 2009;169:96–104. doi: 10.1093/aje/kwn294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavirajan H, Hays RD, Vassar S, Vickrey BG. Responsiveness and construct validity of the health utilities index in patients with dementia. Medical Care. 2009;47:651–661. doi: 10.1097/MLR.0b013e31819241b9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand S-LT, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Khaw K-T, Wareham N, Bingham S, Welch A, Luben R, Day N. Combined impact of health behaviours and mortality in men and women: The EPIC-Norfolk Prospective Population study. PLoS Medicine. 2008;5 doi: 10.1371/journal.pmed.0050012. e12. Erratum in: 2008. PLoS Medicine, 5, e7. Retrieved from http://www.plosmedicine.org/article/info:doi/1.1371/journal.pmed.0050070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer KL, Roberts MS, Horton NJ, Palfai T, Samet JH, Freedner N, Saitz R. Health utility ratings for a spectrum of alcohol-related health states. Medical Care. 2005;43:541–55. doi: 10.1097/01.mlr.0000163644.97251.14. [DOI] [PubMed] [Google Scholar]
- Lang I, Wallace RB, Huppert FA, Melzer D. Moderate alcohol consumption in older adults is associated with better cognition and well-being than abstinence. Age and Ageing. 2007;36:256–261. doi: 10.1093/ageing/afm001. [DOI] [PubMed] [Google Scholar]
- Latino-Martel P, Arwidson P, Ancellin R, Druesne-Pecollo N, Hercberg S, Le Quellec-Nathan M, Maraninchi D. Alcohol consumption and cancer risk: Revisiting guidelines for sensible drinking. Canadian Medical Association Journal. 2011;183:1861–1865. doi: 10.1503/cmaj.110363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang W, Chikritzhs T. Reduction in alcohol consumption and health status. Addiction. 2011;106:75–81. doi: 10.1111/j.1360-0443.2010.03164.x. [DOI] [PubMed] [Google Scholar]
- Lin JC, Guerrieri JG, Moore AA. Drinking patterns and the development of functional limitations in older adults: longitudinal analyses of the health and retirement survey. Journal of Aging and Health. 2011;23:806–821. doi: 10.1177/0898264310397541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1:130–149. [Google Scholar]
- Maddigan SL, Feeny DH, Johnson JA the DOVE Investigators. Construct validity of the RAND-12 and Health Utilities Index Mark 2 and 3 in type 2 diabetes. Quality of Life Research. 2004;13:435–448. doi: 10.1023/B:QURE.0000018497.06539.8f. [DOI] [PubMed] [Google Scholar]
- Maddigan SL, Feeny DH, Majumdar SR, Farris KB, Johnson JA. Health Utilities Index Mark 3 demonstrated construct validity in a population-based sample with type 2 diabetes. Journal of Clinical Epidemiology. 2006;59:472–477. doi: 10.1016/j.jclinepi.2005.09.010. [DOI] [PubMed] [Google Scholar]
- Marra CA, Rashidi AA, Guh D, Kopec JA, Abrahamowicz M, Esdaile JM, Anis AH. Are indirect utility measures reliable and responsive in rheumatoid arthritis patients? Quality of Life Research. 2005;14:1333–1344. doi: 10.1007/s11136-004-6012-0. [DOI] [PubMed] [Google Scholar]
- Molander RC, Yonker JA, Krahn DD. Age-related changes in drinking patterns from mid- to older age: Results from the Wisconsin longitudinal study. Alcoholism: Clinical and Experimental Research. 2010;34:1182–1192. doi: 10.1111/j.1530-0277.2010.01195.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, Brennan PL, Schutte KK, Moos BS. Older adults’ health and late-life drinking patterns: A 20-year perspective. Aging & Mental Health. 2010;14:33–43. doi: 10.1080/13607860902918264. [DOI] [PubMed] [Google Scholar]
- Morley JE, Flaherty JH. It's never too late: Health promotion and illness prevention in older persons. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2002;57:M338–M342. doi: 10.1093/gerona/57.6.m338. [DOI] [PubMed] [Google Scholar]
- Mukamal KJ, Kennedy M, Cushman M, Kuller LH, Newman AB, Polak J, Siscovick DS. Alcohol consumption and lower extremity arterial disease among older adults: The cardiovascular health study. American Journal of Epidemiology. 2008;167:34–41. doi: 10.1093/aje/kwm274. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. 6th ed. Los Angeles, CA: Authors; 1998–2010. [Google Scholar]
- Naimi TS, Brown DW, Brewer RD, Giles WH, Mensah G, Serdula MK, Stroup DF. Cardiovascular risk factors and confounders among nondrinking and moderate-drinking U.S. adults. American Journal of Preventive Medicine. 2005;28:369–373. doi: 10.1016/j.amepre.2005.01.011. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: A clinician's guide, updated 2005 edition. Bethesda, MD: Author; 2007. Retrieved from http://pubs.niaaa.nih.gov/publications/ practitioner/cliniciansguide2005/clinicians_guide.htm. [Google Scholar]
- Orpana HM, Ross N, Feeny D, McFarland B, Bernier J, Kaplan MS. The natural history of health-related quality of life: A 10- year cohort study. Health Reports. 2009;20:29–35. [PubMed] [Google Scholar]
- Østbye T, Taylor DH, Jr, Krause KM, Van Scoyoc L. The role of smoking and other modifiable lifestyle risk factors in maintaining and restoring lower body mobility in middle-aged and older Americans: Results from the HRS and AHEAD. Journal of the American Geriatrics Society. 2002;50:691–699. doi: 10.1046/j.1532-5415.2002.50164.x. [DOI] [PubMed] [Google Scholar]
- Platt A, Sloan FA, Costanzo P. Alcohol-consumption trajectories and associated characteristics among adults older than age 5. Journal of Studies on Alcohol and Drugs. 2010;71:169–179. doi: 10.15288/jsad.2010.71.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers JR, Young AF. Longitudinal analysis of alcohol consumption and health of middle-aged women in Australia. Addiction. 2008;103:424–432. doi: 10.1111/j.1360-0443.2007.02101.x. [DOI] [PubMed] [Google Scholar]
- Rehm J, Baliunas D, Borges GLG, Graham K, Irving H, Kehoe T, Taylor B. The relation between different dimensions of alcohol consumption and burden of disease: An overview. Addiction. 2010;105:817–843. doi: 10.1111/j.1360-0443.2010.02899.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Revicki DA, Brandenburg N, Matza L, Hornbrook MC, Feeny D. Health-related quality of life and utilities in primary-care patients with generalized anxiety disorder. Quality of Life Research. 2008;17:1285–1294. doi: 10.1007/s11136-008-9406-6. [DOI] [PubMed] [Google Scholar]
- Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: A systematic review and meta-analysis. BMJ. 2011;342:d671. doi: 10.1136/bmj.d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royal College of Psychiatrists. Our invisible addicts: First report of the older persons’ substance misuse working group of the Royal College of Psychiatrists (College Report CR165) London, England: Author; June 2011. Retrieved from http://www.rcpsych.ac.uk/files/pdfversion/ CR165.pdf. [Google Scholar]
- Shaper AG. Alcohol consumption decreases with the development of disease. Addiction. 2011;106:1023–1025. doi: 10.1111/j.1360-0443.2011.03372.x. [DOI] [PubMed] [Google Scholar]
- Shaw BA, Krause N, Liang J, McGeever K. Age differences in long-term patterns of change in alcohol consumption among aging adults. Journal of Aging and Health. 2011;23:207–227. doi: 10.1177/0898264310381276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorock GS, Chen LH, Gonzalgo SR, Baker SP. Alcoholdrinking history and fatal injury in older adults. Alcohol. 2006;40:193–199. doi: 10.1016/j.alcohol.2007.01.002. [DOI] [PubMed] [Google Scholar]
- St-Pierre M, Béland Y. Proceedings of the American Statistical Association Meeting, Survey Research Methods. Toronto, Canada: American Statistical Association; 2004, August. Mode effects in the Canadian Community Health Survey: A comparison of CAPI and CATI. [Google Scholar]
- Stahre M, Naimi T, Brewer R, Holt J. Measuring average alcohol consumption: The impact of including binge drinks in quantityfrequency calculations. Addiction. 2006;101:1711–1718. doi: 10.1111/j.1360-0443.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- Statistics Canada. National Population Health Survey–Household component–Longitudinal. 2010 Retrieved from http://www23.statcan.gc.ca:81/imdb/p2SV.pl?Function=getSurvey&SDDS=3225&lang=en& db=imdb&adm=8&dis=2. [Google Scholar]
- Swain L, Catlin G, Beaudet MP. The National Population Health Survey—Its longitudinal nature. Health Reports (Statistics Canada, Catalogue 82-003) 1999;10:69–82. Retrieved from http://www. statcan.gc.ca/pub/82-003-x/1998004/article/4511-eng.pdf. [PubMed] [Google Scholar]
- Tambay J-L, Catlin G. Sample design of the National Population Health Survey. Health Reports (Statistics Canada, Catalogue 82-003) 1995;7:29–38. [PubMed] [Google Scholar]
- Turvey CL, Schultz SK, Klein DM. Alcohol use and health outcomes in the oldest old. Substance Abuse Treatment, Prevention, and Policy. 2006;1(8) doi: 10.1186/1747-597X-1-8. Retrieved from http://www.substanceabusepolicy.com/ content/1/1/8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Agriculture. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans. 2010, June;201 Retrieved from http://www.cnpp.usda.gov/dgas2010-dgacreport.htm. [Google Scholar]
- U.S. Department of Health and Human Services (Substance Abuse and Mental Health Services Administration, Office of Applied Studies) National Household Survey on Drug Abuse, 1994.ICPSR06949- v1. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 2008-10-28; 2008. doi:10.3886/ICPSR06949. [Google Scholar]
- Wilkins K. Predictors of death in seniors. Health Reports, 16, Supplement. 2006:57–67. [PubMed] [Google Scholar]
- World Health Organization. International guide for monitoring alcohol consumption and related harm. Geneva, Switzerland: Author; 2000. Retrieved from http://whqlibdoc.who.int/hq/2000/who_msd_msb_00.4.pdf. [Google Scholar]
- World Health Organization. Global strategy to reduce harmful use of alcohol. 2010 doi: 10.2471/BLT.19.241737. Retrieved from http://www.who.int/substance_abuse/activities/ globalstrategy/en/index.html. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin R, Li H, Wu J, Lin W, Yang D, Pan S, Long X. Effects of alcohol consumption and other lifestyle behaviors on blood pressure for the middle-aged and elderly in the Guangxi Hei Yi Zhuang and Han populations. Alcohol. 2007;41:541–555. doi: 10.1016/j.alcohol.2007.09.002. [DOI] [PubMed] [Google Scholar]
- Younossi ZM, Boparai N, McCormick M, Price LL, Guyatt G. Assessment of utilities and health-related quality of life in patients with chronic liver disease. American Journal of Gastroenterology. 2001;96:579–583. doi: 10.1111/j.1572-0241.2001.03537.x. [DOI] [PubMed] [Google Scholar]
- Zanjani FA, Schaie KW, Willis SL. Age group and health status effects on health behavior change. Behavioral Medicine. 2006;32:36–46. doi: 10.3200/BMED.32.2.36-46. [DOI] [PubMed] [Google Scholar]