Abstract
Objective
To compare the costs of two spinal implants—hook and hybrid constructs and pedicle screw constructs—in posterior spinal fusion for adolescent idiopathic scoliosis (AIS) as they relate to intraoperative deformity correction.
Study design and method
This retrospective study examined 50 patients with AIS who were treated with posterior spinal fusion using segmental hook-hybrid constructs (23) or pedicle screws (27). Radiographic parameters measured on immediate preoperative and initial standing postoperative scoliosis films were the coronal Cobb angles of the upper thoracic, middle thoracic, lumbar, and instrumented curves; global coronal and sagittal balance; thoracic kyphosis; lumbar lordosis; and type and number of implants used. Current implant cost data were obtained from three major spinal implant manufacturers to determine the total cost of the constructs, cost per degree of correction, cost per level fused, and cost per degree of correction of the major curve.
Results
After surgery, the average percentage of correction for the middle thoracic curve or major curve was 57 % in the hook-hybrid group compared to 73 % in the pedicle screw group (P < 0.001). The average amount of correction of the major curve was 31.1° in the hook-hybrid group compared to 42.7° in the pedicle screw group (P < 0.001). The average number of fused levels was 10.7 in the hook-hybrid group compared to 12.2 in the pedicle screw group (P < 0.001). The average number of implants was 14.8 in the hook-hybrid group compared to 23.3 in the pedicle screw group (P < 0.001). The average total cost of implants was $11,248 in the hook-hybrid group compared to $22,826 in the pedicle screw group (P < 0.001), and the average cost per fused level was $1,058 in the hook-hybrid group compared to $1,878 in the pedicle screw group (P < 0.001). The average cost per degree of correction of the major curve was $415 in the hook-hybrid group compared to $559 in the pedicle screw group (P = 0.0014). The global coronal balance, global sagittal balance, thoracic kyphosis, and lumbar lordosis did not differ significantly between the two groups.
Conclusion
Pedicle screw instrumentation was shown to be more expensive overall, per fused level, and per degree of correction. Also, more implants were used and more levels were fused in the pedicle screw group than in the hook-hybrid group. Pedicle screws showed a statistically significantly greater percentage of correction of the major curve. Physicians must evaluate each patient individually and determine if the increased percentage of correction warrants the increased cost for pedicle screw constructs.
Keywords: Scoliosis, Cost, Pedicle screw, Spinal fusion, Implant
Introduction
The surgical treatment of adolescent idiopathic scoliosis (AIS) is expensive and involves costs from various sources, including medical imaging, inpatient hospital expenses, operating room fees, and professional fees, among others. Charges can range from $100,000 to $150,000 per case [1]. One significant contributor to the cost of the surgical treatment of AIS is the spinal instrumentation used for deformity correction and stabilization, constituting as much as 29 % of the entire cost of treatment [2, 3]. Spinal implant constructs have evolved over the past few decades from in situ fusion and cast stabilization, to nonsegmental rods, to segmental wire fixation, to segmental hook fixation, to segmental screw fixation. Each advancement has brought increases in the costs of the constructs. With increased focus on healthcare reform and healthcare costs, it is important to determine whether increased cost provides an increased clinical benefit to the patient.
Excellent clinical and radiographic improvements have been documented with the use of pedicle screws in lumbar curves, and this approach has been widely adopted by surgeons [2, 4, 5]. Over the past decade, the use of pedicle screws has also spread cephalad and has become more widespread in the thoracic spine; however, the results have been conflicting as to whether thoracic pedicle screws offer significant clinical and radiographic improvements over segmental constructs [6–10].
The goal of this retrospective study was to investigate the cost of implants in patients treated with pedicle screw constructs or hook-hybrid constructs and to compare the costs against radiographic measures of deformity correction. This study focused on an assessment of deformity correction between immediate preoperative and immediate postoperative standing scoliosis radiographs. Endpoints included curve correction in the coronal and sagittal planes, total cost of constructs, cost per level fused, and cost per degree of correction.
Methods
Study patients
After Institutional Review Board approval was obtained, a retrospective review identified 50 patients with AIS who were treated with posterior spinal fusion with hook-hybrid constructs (23) or segmental pedicle screws (27) (Fig. 1). The patient lists were generated using CPT codes for segmental instrumentation of the spine. Two patient lists were generated, each representing a consecutive cohort. The first hook-hybrid cohort involved surgical procedures performed between 1996 and 2000 by two of the authors (B.L.F. and W.C.W.). Patients in the pedicle screw cohort were treated in 2008 and 2009 by three of the authors (W.C.W., J.R.S., and D.M.K.). In the hook-hybrid group, 24 patients were identified; one was excluded because of incomplete radiographs, leaving 23 for inclusion in the study. In the pedicle screw group, 33 patients were identified; six were excluded because of incomplete radiographs, leaving 27 for inclusion in the study. The decision to use pedicle screw constructs rather than hook-hybrid constructs was based on the surgeons’ preferred treatment at the time of the surgery. Children with congenital or neurogenic scoliosis and children with AIS who had anterior procedures were excluded from the analysis, as were patients with incomplete radiographic data. Many of these procedures were done before the widespread use of the Lenke classification of AIS, and bending films, although obtained, were no longer available in our older patient cohort. Therefore, formal classification using that system was not possible; however, all children had middle thoracic major curves. Instrumentation into the upper thoracic curve and lumber curve was variable among patients and treating surgeons, and could not be controlled for with this retrospective study design. The patient age at the time of surgery, race, and gender were similar in both groups (Table 1).
Fig. 1.
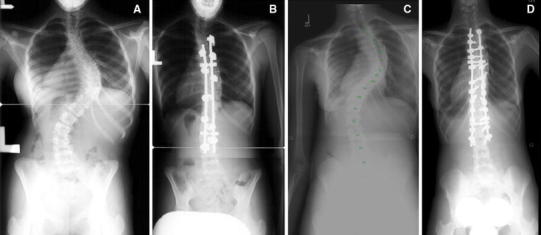
Preoperative and postoperative radiographs of curves treated with a hook construct (a, b) and with a pedicle screw construct (c, d). Initial and corrected curve magnitudes were similar (hook construct, 70° corrected to 23°; screw construct, 70° corrected to 17°). The hook construct (b) cost averaged $10,934.28 and the pedicle screw construct (d) cost averaged $26,341.32
Table 1.
Demographic data
| Hook-hybrid group | Screw group | P-value | |
|---|---|---|---|
| Average age at surgery (years) | 14.3 | 13.9 | 0.46 |
| Sex | |||
| Male | 1 | 6 | 0.09 |
| Female | 22 | 21 | 0.50 |
| Race | |||
| Caucasian | 15 | 13 | 0.41 |
| African American | 8 | 14 | 0.37 |
Construct was defined as all the implants used for deformity correction and stabilization, which included rods, screws, hooks, and crosslinks. Wires and cables were not used in any of the studied procedures. Of the 23 hook-hybrid constructs, seven used pedicle screws as a base, with an average of 3.4 screws used in the lower segments. Occasionally (8 of 27 procedures), one or more hooks were used at the uppermost level in the pedicle screw group.
Cost analysis
For cost analysis, we obtained price lists from our hospital for three separate manufacturers of spinal implants and then averaged the cost of each type of implant. We limited the analysis to stainless steel implants in order to keep the metal cost uniform. Although modern pedicle screw constructs tend to be titanium, we chose to limit our data to stainless steel so as to remove the type of metal as a variable and create more uniformity in the cost data. The costs of all implants were considered in terms of today’s cost in order to eliminate the change in cost over time as a confounding factor.
Radiographic analysis
Posteroanterior and lateral standing radiographs were used to evaluate the sagittal and coronal planes. The immediate preoperative and the initial standing postoperative radiographs were reviewed. The initial standing postoperative radiograph was obtained at 2–6 weeks postoperatively and was chosen to most accurately reflect the deformity correction achieved at the time of surgery. Measurements for the hook-hybrid construct group were made manually using 36-in-long cassette coronal and lateral radiographs, and measurements for the pedicle screw group were made using Carestream PACS digital software (Carestream Health, Inc., Rochester, NY). Radiographic analysis included Cobb angle measurements of the major (middle thoracic), upper thoracic, lumbar, and instrumented curves. Global coronal balance was measured as the distance from the center sacral vertical line to the C7 plumbline.
On the lateral radiographs, global sagittal balance was measured as the distance from the C7 plumbline to the posterior superior corner of the sacrum. If the C7 plumbline fell posterior to the posterior superior corner of the sacrum, the global sagittal balance was negative. If the C7 plumbline fell anterior to the posterior superior corner of the sacrum, the sagittal balance was positive. Thoracic kyphosis was measured from the upper endplate of T1 to the lower endplate of T12. Lumbar lordosis was measured from the upper endplate of T12 to the lower endplate of L5. The percentage of correction was calculated by the following formula [11]:
Results
Radiographic characteristics
The radiographic results are shown in Table 2. The mean preoperative Cobb angle of the major curve was 54.1° in the hook-hybrid group and 58.7° in the screw group. The mean postoperative Cobb angles were 23.0° and 16.0°, respectively. The absolute correction was 31.1° for the hook-hybrid group and 42.7° for the screw group (P < 0.001). The percentage of correction was 56.9 % for the hook-hybrid group and 73.0 % for the screw group (P < 0.0001).
Table 2.
Radiographic characteristics
| Hook-hybrid group | Screw group | P-value* | |
|---|---|---|---|
| Mean | Mean | ||
| Global balance | |||
| Preoperative (mm) | 18.4 | 19.5 | 0.7658 |
| Postoperative (mm) | 11.6 | 18.9 | 0.0572 |
| Major curve Cobb angle (°) | |||
| Preoperative | 54.1 | 58.7 | 0.0922 |
| Postoperative | 23.0 | 16.0 | 0.0007 |
| Absolute correction | 31.1 | 42.7 | <0.0001 |
| % correction | 56.9 | 73.0 | <0.0001 |
| Upper thoracic curve (°) | |||
| Preoperative | 25.3 | 27.8 | 0.4769 |
| Postoperative | 17.2 | 13.0 | 0.1149 |
| Absolute correction | 8.1 | 14.8 | 0.0082 |
| % correction | 27.8 | 50.0 | 0.0164 |
| Lumbar curve (°) | |||
| Preoperative | 33.8 | 35.5 | 0.6293 |
| Postoperative | 11.3 | 10.5 | 0.7214 |
| Absolute correction | 22.5 | 25.0 | 0.3465 |
| % correction | 68.0 | 73.0 | 0.3254 |
| Instrumented curve (°) | |||
| Preoperative | 32.0 | 23.1 | 0.0513 |
| Postoperative | 16.0 | 9.0 | 0.0023 |
| Absolute correction | 16.0 | 14.1 | 0.6309 |
| % correction | 34.7 | 44.8 | 0.5833 |
* Statistically significant if P < 0.05
The mean preoperative upper thoracic Cobb angle was 25.3° in the hook-hybrid group and 27.8° in the screw group, compared to postoperative upper thoracic Cobb angles of 17.2° and 13.0°, respectively. The absolute correction of the upper thoracic curve was 8.1° in the hook-hybrid group and 14.8° in the screw group (P = 0.008). The mean upper thoracic curve percentage of correction was 27.8 % in the hook-hybrid group and 50.0 % in the screw group (P = 0.016).
The mean preoperative lumbar Cobb angle was 33.8° in the hook-hybrid group and 35.5° in the screw group compared with mean postoperative lumbar Cobb angles of 11.3° and 10.5°, respectively. The mean lumbar curve percentage of correction was 68.0 % in the hook-hybrid group and 73.0 % in the screw group (P = 0.33).
The mean instrumented curve percentage of correction was 34.7 % in the hook-hybrid group and 44.8 % in the screw group (P = 0.58). No statistically significant difference in the global coronal balance was seen between the two groups.
No statistically significant difference existed between the hook-hybrid and screw groups for global sagittal balance, thoracic kyphosis angle, or lumbar lordosis angle (Table 3).
Table 3.
Sagittal plane measurements
| Hook-hybrid group | Screw group | P-value | |
|---|---|---|---|
| Mean | Mean | ||
| Global balance | |||
| Preoperative (mm) | −36.9 | −46.3 | 0.5472 |
| Postoperative (mm) | −16.7 | −32.5 | 0.5016 |
| Thoracic kyphosis angle (°) | |||
| Preoperative | 29.3 | 32.4 | 0.6880 |
| Postoperative | 26.0 | 32.2 | 0.2706 |
| Lumbar lordosis angle (°) | |||
| Preoperative | 52.4 | 49.0 | 0.3888 |
| Postoperative | 42.6 | 41.4 | 0.7072 |
Lowest instrumented vertebra (LIV) data were collected for both groups. The LIV in the hook-hybrid group averaged L2.29 and in the pedicle screw group, it averaged L2.93; the most common LIV in both groups was L3. On average, the pedicle screw group LIV was statistically more caudal by almost one vertebral level.
Cost characteristics
The screw group had a greater total cost of constructs, cost per fused level, and cost per degree of correction of the major curve than the hook-hybrid group (Table 4). The average total cost of constructs was $11,248 in the hook-hybrid group and $22,826 in the screw group (P < 0.001). The average cost per fused level (total construct cost/number of fused levels) was $1,058 in the hook-hybrid group and $1,878 in the screw group (P < 0.001). The average cost per degree of correction (total construct cost/number of degrees of correction of the major curve) was $415 in the hook-hybrid group and $559 in the screw group (P = 0.0141).
Table 4.
Cost characteristics
| Hook-hybrid group | Screw group | P value* | |
|---|---|---|---|
| Number of levels fused | 10.7 | 12.9 | <0.0001 |
| Number of hooks | 9.4 | 0.2 | n/a |
| Number of pedicle screws | 0.7 | 19.1 | n/a |
| Number of crosslinks | 2 | 2 | n/a |
| Number of rods | 2 | 2 | n/a |
| Total number of construct elements | 14.8 | 23.3 | <0.0001 |
| Total cost of constructs | $11,247.55 | $22,825.73 | <0.0001 |
| Cost per fused level | $1,057.92 | $1,877.56 | <0.0001 |
| Cost per degree of correction of the major curve | $415.28 | $559.21 | 0.0141 |
The screw group also had a greater number of levels fused (12.9) than the hook-hybrid group (10.7), and the screw group used 19.1 fixation points compared to 9.4 fixation points in the hook-hybrid group. The total number of construct elements in the screw group was 23.3 compared to 14.8 in the hook-hybrid group (P < 0.0001).
Cost data from the three major spinal implant manufacturers utilized most often at our facility were used in calculating the cost of constructs (Table 5). The average cost for each of the implants was calculated by averaging the cost for the different sizes of stainless steel implants from each of the companies. These costs were generated from a current pricing list (2010) provided by the implant manufacturers and likely represent a regional cost variation. Based on these cost figures, a screw is 30.1 % more expensive than a hook.
Table 5.
Average cost of various implants from three spinal implant manufacturers
| Implant | Company 1 | Company 2 | Company 3 | Average |
|---|---|---|---|---|
| Stainless steel screw | $1,404.28 | $777.19 | $875.00 | $1,018.82 |
| Stainless steel hook | $1,039.37 | $494.97 | $800.00 | $778.11 |
| Stainless steel crosslink | $1,439.03 | $891.48 | $1,200.00 | $1,176.84 |
| Stainless steel rod | $410.38 | $287.88 | $501.00 | $399.75 |
Discussion
The debate about the use of thoracic pedicle screws and hooks has persisted since the mid-1990s. The debate has focused mainly on a few principal issues: biomechanics, safety and complications, three-dimensional deformity correction, improvement in clinical outcomes, and cost. Although these factors and many others are involved in determining a good clinical outcome for AIS surgery, this review focused on intraoperative deformity correction. Specifically, a comparison was made between the current cost of hook-hybrid constructs and pedicle screw constructs in relation to intraoperative deformity correction
The radiographic measurements in this study are comparable to those previously reported (Table 6) [12–17]. Major curve correction in the coronal plane was 73 % in the screw group and 56.9 % in the hook group. There were no significant differences in the sagittal plane measurements between the two groups.
Table 6.
Comparisons of hook and pedicle screw constructs
| Study | No. of patients | Construct(s) | Major curve correction |
|---|---|---|---|
| Suk et al. [16] | 78 | 31 hooks only | 57 % |
| 24 pedicle screws in hook pattern | 67 % | ||
| 23 segmental pedicle screws | 72 % | ||
| Liljenqvist et al. [13] | 99 | 50 hooks only | 52 % |
| 49 pedicle screws + hooks/all pedicle screws | 56 % | ||
| Kim et al. [12] | 52 | 26 hook constructs | 52 % |
| 26 pedicle screws | 76 % | ||
| Storer et al. [15] | 25 | 15 hooks | 68 % |
| 10 screws | 70 % | ||
| Lowenstein et al. [14] | 34 | 17 hook-hybrid constructs | 63 % |
| 17 pedicle screws | 73 % | ||
| Vora et al. [17] | 72 | 24 hooks only | Not given |
| 23 hook-hybrid constructs | 63 % | ||
| 25 pedicle screws | 72 % | ||
| Current study | 50 | 23 hook-hybrid constructs | 57 % |
| 27 pedicle screws | 73 % |
Although the two groups in this study were similar in terms of the curve magnitude of the upper thoracic, middle thoracic, and lumber curves (see Table 2), inadequate radiographic data existed to correctly classify each curve. Nevertheless, there was a trend toward longer fusions in the pedicle screw group and an LIV almost one level more caudal in the pedicle screw group. The exact cause of this change over time is unclear. To control for the added length of fusion in the pedicle screw group, the cost data are expressed in terms of the cost per level and the cost per degree of correction (see Table 4).
The main focus of this study was to evaluate the added cost of the pedicle screws in relation to the radiographic measurements of curve deformity correction. The total cost of the construct ($22,825.73), cost per level fused ($1,877.56), and cost per degree of correction ($559.21) were significantly higher in the pedicle screw group than in the hook-hybrid group (being $11,247.55, $1,057.92, and $415.28, respectively). The total cost of the construct, cost per level fused, and cost per degree of correction were 102.9, 77.4, and 34.7 % higher in the screw group, respectively.
Much of the increased cost was due to the added cost of an individual pedicle screw ($1,018.82) compared to a hook ($778.11). The other significant factors in the increased cost in the screw group were the increased number of fused levels and the increased number of screws used at each level. In the screw group, an average of 19.1 screws were used, compared to 9.4 hooks, and 12.9 levels were fused, compared to 10.7 levels in the hook-hybrid group. This indicates a trend toward longer constructs with an emphasis on more points of fixation. It remains unclear if more implants and more levels are necessary in order to achieve additional correction. Nevertheless, this trend toward an increase in the number of fixation points has certainly added to the rising cost of spinal instrumentation constructs. In order to more easily compare these costs, we have chosen to calculate the cost per level and the cost per degree of correction. Although 28 % more correction was achieved over the major curve in the screw group, the cost per degree of correction in the screw group was 35 % higher.
The debate over “how much correction is enough correction?” will likely continue, and further research will be needed so as to determine the optimal amount of deformity correction in order to achieve a good, long-term outcome. It is still not known if additional points of fixation offered by all pedicle screw constructs are necessary to achieve good correction. Long-term followup of two similar AIS groups (with different constructs) will be needed in order to determine if the improved deformity correction obtained with pedicle screws translates into improved long-term clinical outcomes. As this debate continues, cost will certainly be an important factor in the discussion. Expressing cost in terms of “cost per degree of correction” may improve the ability to compare deformity correction in terms of cost.
In conclusion, thoracic pedicle screws appear to offer greater correction of major AIS curves compared to hook constructs, but at a significantly greater cost. Currently, it is not known if this improvement in the major curve correction provides significant clinical benefit to the patient to warrant the increased cost of implants.
References
- 1.Daffner SD, Beimesch CF, Wang JC. Geographic and demographic variability of cost and surgical treatment of idiopathic scoliosis. Spine. 2010;35:1165–1169. doi: 10.1097/BRS.0b013e3181d88e78. [DOI] [PubMed] [Google Scholar]
- 2.Hamill CL, Lenke LG, Bridwell KH, et al. The use of pedicle screw fixation to improve correction in the lumbar spine of patients with idiopathic scoliosis. Is it warranted? Spine. 1996;21:1241–1249. doi: 10.1097/00007632-199605150-00020. [DOI] [PubMed] [Google Scholar]
- 3.Kamerlink JR, Quirno M, Auerbach JD, et al. Hospital cost analysis of adolescent idiopathic scoliosis correction surgery in 125 consecutive cases. J Bone Joint Surg Am. 2010;92:1097–1104. doi: 10.2106/JBJS.I.00879. [DOI] [PubMed] [Google Scholar]
- 4.Barr SJ, Schuette AM, Emans JB. Lumbar pedicle screws versus hooks. Results in double major curves in adolescent idiopathic scoliosis. Spine. 1997;22:1369–1379. doi: 10.1097/00007632-199706150-00016. [DOI] [PubMed] [Google Scholar]
- 5.Gaines RW., Jr The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am. 2000;82:1458–1476. doi: 10.2106/00004623-200010000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Delorme S, Labelle H, Aubin CE, et al. Intraoperative comparison of two instrumentation techniques for the correction of adolescent idiopathic scoliosis. Rod rotation and translation. Spine. 1999;24:2011–2018. doi: 10.1097/00007632-199910010-00009. [DOI] [PubMed] [Google Scholar]
- 7.Halm H, Niemeyer T, Link T, et al. Segmental pedicle screw instrumentation in idiopathic thoracolumbar and lumbar scoliosis. Eur Spine J. 2000;9:191–197. doi: 10.1007/s005860000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liljenqvist UR, Halm HF, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine. 1997;22:2239–2245. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- 9.Suk SI, Lee CK, Kim WJ, et al. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. [PubMed] [Google Scholar]
- 10.Yamagata M, Kitahara H, Minami S, et al. Mechanical stability of the pedicle screw fixation systems for the lumbar spine. Spine. 1992;17(3 Suppl):S51–S54. doi: 10.1097/00007632-199203001-00011. [DOI] [PubMed] [Google Scholar]
- 11.O’Brien MF, Kuklo TR, Blanke KM, Lenke LG, editors. Radiographic measurement manual: Spinal Deformity Study Group. Memphis, TN: Medtronic Sofamor Danek; 2004. [Google Scholar]
- 12.Kim YJ, Lenke LG, Bridwell KH, et al. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine. 2004;29:333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 13.Liljenqvist UR, Lepsien U, Hackenberg L, et al. Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J. 2002;11:336–343. doi: 10.1007/s00586-002-0415-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lowenstein JE, Matsumoto H, Vitale MG, et al. Coronal and sagittal plane correction in adolescent idiopathic scoliosis: a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine. 2007;32:448–452. doi: 10.1097/01.brs.0000255030.78293.fd. [DOI] [PubMed] [Google Scholar]
- 15.Storer SK, Vitale MG, Hyman JE, et al. Correction of adolescent idiopathic scoliosis using thoracic pedicle screw fixation versus hook constructs. J Pediatr Orthop. 2005;25:415–419. doi: 10.1097/01.mph.0000165134.38120.87. [DOI] [PubMed] [Google Scholar]
- 16.Suk SI, Kim WJ, Lee SM, et al. Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine. 2001;26:2049–2057. doi: 10.1097/00007632-200109150-00022. [DOI] [PubMed] [Google Scholar]
- 17.Vora V, Crawford A, Babekhir N, et al. A pedicle screw construct gives an enhanced posterior correction of adolescent idiopathic scoliosis when compared with other constructs: myth or reality. Spine. 2007;32:1869–1874. doi: 10.1097/BRS.0b013e318108b912. [DOI] [PubMed] [Google Scholar]


