Abstract
This study examined whether parent–youth dyads participating in the Strengthening Families Program 10–14 (SFP 10–14) would demonstrate greater postprogram family cohesion, communication, involvement, and supervision and if youth would report less alcohol, tobacco, and other drugs involvement in contrast to a comparison group. From 16 randomly selected schools, we recruited 167 parent–youth dyads: 86 from intervention and 81 from comparison schools. The intention-to-treat analysis found one significant change in family environment. Considering dose, it was found that among dyads receiving a full dose, all the outcomes were in the expected direction and effect sizes were moderate. Among dyads receiving a partial dose, 10 of 18 outcomes were in the direction opposite that expected. Youth participation in alcohol, tobacco, and other drugs was very low and did not differ postprogram. Although the expected outcomes were not realized, findings descriptive of dosage effects make a valuable contribution to the field. Study of factors that distinguish intervention completers from noncompleters is recommended.
Keywords: adolescence, parenting/families, community, experimental, quasi-experimental
The family is a crucial target for preventive interventions to achieve youth health and development and reduce risk of illness, injury, and death. Families are the primary vehicle of socialization. Families that function well are characterized by cohesion, communication, involvement, and supervision (Glasser & Glasser, 1966; Olson et al., 1983). The Substance Abuse and Mental Health Administration (SAMHSA) issued a call for proposals in 2000 for a third cohort of multi-site initiatives to test the efficacy of mentoring and family strengthening programs in reducing child and youth involvement in alcohol, tobacco, and other drugs (ATOD). This paper reports the outcomes of a family strengthening activity, The Strengthening Families Program for Parents and Youth ages 10–14 (SFP 10–14) at one site. In addition to examining the potential for ATOD prevention among the sample, we sought to understand a potential mechanism by which the SFP 10–14 may work, that is, promoting characteristics of the family environment, specifically: cohesion, communication, involvement, and supervision. Our site focused on families with children aged 9 to 11 in two Midwestern cities.
Youth Substance Use and Family Functioning Factors
Studies since the early 1990s, using limited samples, have documented that an alarming number of elementary school children have used ATOD (Bush & Iannotti, 1993; Finke, Chorpenning, French, Leese, & Siegel, 1996; Harrell, Bangdiwala, Deng, Webb, & Bradley, 1998; Long & Boik, 1993; Loveland-Cherry, Ross, & Kaufman, 1999). Data on elementary school aged–children’s ATOD participation is sparse because it is thought that ATOD use is not a problem (Morrongiello & Lasenby-Lessard, 2007) and that questioning children about ATOD may encourage the report of behavior whether it has occurred or not (Rodgers, Billy, & Udry, 1982) or expose children unnecessarily to ideas about ATOD (Rew, Horner, Riesch, & Cauvin, 2004).
More recently, Dowdell (2006) surveyed 106 seventh-graders in two parochial middle schools in southwest Philadelphia and found that 43% said they tried smoking, 40% of those began before age 11 and 69% of those who tried smoked at least one cigarette every day the past 30 days. Using data from the New Hampshire Teen Assessment Project Survey, DiNapoli (2009) documented that 28% of 3,775 adolescent girls reported they initiated tobacco use before they were 12 years old. A study of 737 North Carolina third-through fifth-graders reported by Jackson and Dickinson (2006) revealed that 168 (25%) admitted having smoked a whole cigarette.
Analyzing four national and seven statewide surveys of children’s alcohol use in the United States, Donovan (2007) conceptualized alcohol use as prevalence of ever having tasted alcohol, ever having more than a sip of alcohol, lifetime experience of more than a few sips of alcohol, use in the past year, past month, and past week. He reported substantial numbers of children have experience with alcohol with greatest rates of use increasing between Grades 5 and 6.
These data, from isolated small studies to large surveys, substantiate that strategies to reduce ATOD use need to be delivered prior to youth’s transition to middle school. The ages 9 to 11, corresponding with the last year of elementary school in the study location, were chosen in order to maximize the opportunity of reaching young adolescents when they remain amenable to parental and trustworthy adult influence.
Family functioning was conceptualized as family cohesion, communication, involvement, and supervision. Cohesion is defined as the emotional bonding, togetherness, and closeness family members have toward one another. Ideally, family members derive pleasure in their relationships from within and outside the family. Cohesion is associated with social competence among children and adolescents (Leidy, Guerra, & Toro, 2010) and resilience when families are faced with economic pressures (Behnke et al., 2008).
Communication is defined as the expression of ideas and feelings assertively but inoffensively and the reception of ideas expressed by others attentively and accurately (Robin, 1979). Clear messages, empathy, reflective listening, supportive statements, and effective problem solving characterize positive communication. It enables family members to share their changing needs, feelings, and preferences; ask for help; and bring up difficult topics. Incongruent, disqualifying, and nonsupportive messages; harsh criticism; poor problem-solving skills; and lack of empathy characterize negative communication. It minimizes the ability of family members to share feelings, address tough issues, or manage conflict. Good communication skills are crucial to family relationships and are associated with a host of child health and developmental outcomes such as reduced underage drinking (Fang, Schinke, & Cole, 2009) and tobacco smoking (Abroms, Simons-Morton, Haynie, & Chen, 2005; Harekeh, Scholte, de Vries, & Engels, 2005) to cite a few.
The concern and commitment members have toward the family is termed involvement. Valuing participation in family events, spending time together, doing activities regularly, and being drawn in to activities family members enjoy typify involvement. Family involvement is linked to reduced risky behavior (Fang et al., 2009; Fischer, Miles, Austin, Camargo, & Corditz, 2007; Gorman-Smith, Tolan, Zelli, & Huesmann, 1996).
Supervision is adult presence and interaction, sometimes referred to as monitoring, and is crucial to youth risk behavior prevention. It includes practices such as limiting access to weapons and substances (Blum et al., 2000); presence at key times such as before and after school and at bedtime (Resnick et al., 1997); establishing house rules, for example, disapproval of smoking, drinking, sexual involvement (Small & Luster, 1994); and providing structure such as curfew and established mealtimes (Jessor, Van Den Bos, Vanderryn, Costa, & Turbin, 1995; Forgatch & Patterson, 2010).
These indicators of family functioning are strong predictors of youth health risk behavior (Cleveland, Feinberg, Bontempo, & Greenberg, 2008) and are fundamental to SFP 10–14.
The SFP 10–14 was the product of a major revision of the 14-session Strengthening Families Program developed by Kumpfer, DeMarsh, and Child (1989). The SFP 10–14 is based on the Bio-psychosocial Vulnerability Model (Kumpfer, Trunnell, & Whiteside, 1990). According to this model, psychosocial risk variables interact with family stressors and are buffered by family coping skills and resources. Family variables also interact with community, school, and peer variables to influence youth substance use (Kumpfer, Molgaard, & Spoth, 1996). The SFP 10–14 is designed to reduce risk factors and build family capacity and coping skills to access and use resources within their school and community to achieve child socialization goals. The program was developed for families at all economic and educational levels and has been tested with both rural and urban populations. SFP 10–14 is a SAMHSA model program (http://www.nrepp.samhsa.gov/programf`ulldetails.asp?PROGRAM_ID=212). A universal intervention for a general population, it targets the reduction of family risk factors and the enhancement of family protective processes (Table 1). The curriculum, particularly strategies and actors, is updated routinely at Iowa State University Extension (http://www.extension.iastate.edu/sfp/).
Table 1.
Strengthening Families Program 10–14 Content
| Session | Parent | Youth | Family |
|---|---|---|---|
| 1 |
|
|
|
| 2 |
|
|
|
| 3 |
|
|
|
| 4 |
|
|
|
| 5 |
|
|
|
| 6 |
|
|
|
| 7 |
|
|
|
In three previous efficacy trials, when compared with nonparticipants, participants in SFP 10–14 demonstrated reductions in parent, family, and youth risk factors for substance use and later youth substance use in children of drug users (Kumpfer & DeMarsh, 1985), methamphetamine use (Spoth, Clair, Shin, & Redmond, 2006), and negative peer associations (Gottfredson et al., 2006). Cultural adaptations of the program have produced positive outcomes among African American samples (Aktan, Kumpfer, & Turner, 1996). Spoth, Shin, Guyll, Redmond, and Azevedo (2006) demonstrated that SFP 10–14 delayed alcohol initiation by 12.9 months among high-risk groups and by 14.7 months for low-risk groups determined 6 years after pretest assessment among rural, white, public school students.
The SFP 10–14 approach assumes a developmental perspective, with the family exerting relatively more influence on pre- and young adolescents than on older adolescents. For most families and youth, research has shown that the most vulnerable and stressful periods are transitions. When youth advance from elementary school to middle school or junior high, they often face challenges associated with physical, cognitive, and social changes, such as learning to get along with a wider group of peers (Rudolph, Lambert, Clark, & Kurlakowsky, 2001). It is at this stage, that youth are likely to encounter ATOD for the first time. A substantial body of literature supports a strong predictive relationship between ineffective family environments in early adolescence and problem behaviors, such as ATOD use, in later adolescence (Ackard, Neumark-Sztainer, Story, & Perry, 2006; Bullock & Dishion, 2007; DeVore & Ginsburg, 2005; Marsiglia, Kulis, Parsai, Villar, & Garcia, 2009; Watkins, Howard-Barr, Moore, & Werch, 2006)
Parents and youth alike anticipate change in their relationship and have demonstrated openness to strategies to assist them in making the transition (Riesch & Forsyth, 1992). Moreover, this age is immediately prior to increases in the prevalence of delinquent behavior, substance use, and sexual activity (Resnick et al., 1997). Late childhood is an ideal time to develop skills and habits that have lifelong consequences. At this age, youth are industrious and family continues to be central to their relationships. Just prior to the transition to middle school is the ideal time to implement a universal preventive intervention to delay substance use. Fifth grade marked the end of elementary school where this study was conducted. If SFP 10–14 is efficacious for improving the family environment characteristics, it may in turn be efficacious for preventing youth involvement in substance use.
The SAMHSA cohort initiative included seven family strengthening programs sites. Based on the Bio-psychosocial Vulnerability Model described earlier, family, community and school, and peer-related environments were assessed at all sites. Local sites were encouraged to study issues of interest to their community. We held several meetings of our community advisory boards. Community members were most distressed by what they perceived as adults failing to place high priority on family functioning. Strategies to enhance involvement with and monitoring youth and reduce harsh communication practices were requested. This input guided the selection of the SFP 10–14 among the array of SAMHSA model programs and the measures to evaluate the study outcomes. Our communities were interested in family environment and the youth ATOD outcomes.
The questions examined in this paper are as follows:
To what extent do youth and adults who participate in SFP 10–14 demonstrate an improved family environment as indicated by greater family cohesion, open communication, involvement, and supervision than youth and adults who did not participate when compared immediately (Post 1) and at 6 months (Post 2) after the intervention?
To what extent do youth who participate in SFP 10–14 report incidents of involvement with ATOD than youth who did not participate when compared immediately (Post 1) and at 6 months (Post 2) after the intervention.
Method
This study was part of a seven-site, national initiative to test the efficacy of SAMHSA model family strengthening programs to reduce child and youth involvement in ATOD. The study was conducted from April 2003 through December 2005.
Design
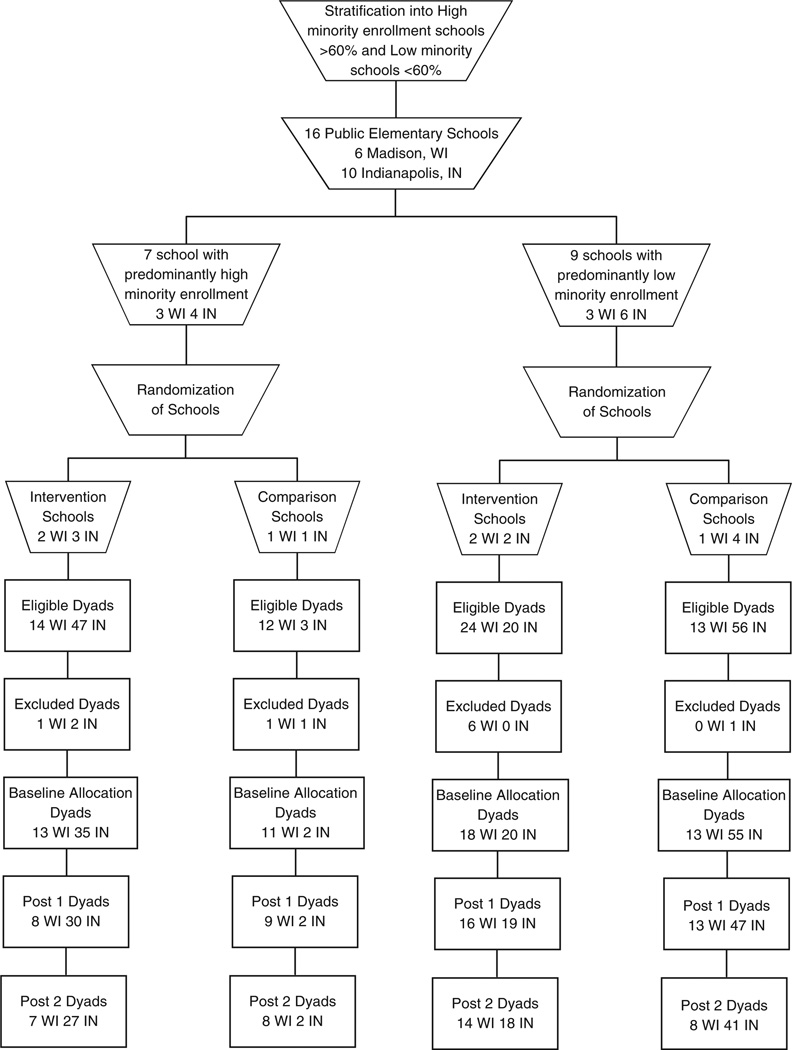
A two-group intervention and comparison condition with baseline (Time 1), Post 1 (Time 2), and Post 2 (Time 3) data collection periods design was implemented. Post 1 occurred immediately postintervention and Post 2 occurred 6 months after the intervention. All public elementary schools with a fifth grade in the two Midwestern cities, one midsized (Madison, Wisconsin) and the other a large urban area (Indianapolis, Indiana), were stratified by race as high (<60%) or low (>60%) to ensure representation among the groups. Sixty percent was chosen because it constituted high minority enrollment in Madison, Wisconsin. Schools were randomly assigned to the intervention or comparison conditions. Schools served only as a recruitment site for adult–youth dyads. See Figure 1 for a schema of school stratification, randomization, and adult–youth dyad participation.
Figure 1.
Consort diagram
Measures
The family environment was assessed through measures of family cohesion, open communication, involvement, and supervision as perceived by the youth and adult.
Family cohesion refers to the feelings of emotional closeness and bonding among family members. It was measured with the widely used cohesion subscale of the Family Adaptability and Cohesion Evaluation Scale III (Olson, 1994). The subscale has 10 items with response options of 1 (almost never) to 5 (almost always). With a potential minimum score of 20 and potential maximum score of 50, higher scores indicate higher perceived family cohesion. This item typifies the instrument: “Family members ask each other for help.” Alpha reliability coefficients in this sample were .70 for youth and .74 for adults.
Openness of communication is characterized by the adult and youth perceiving a climate for honest discussion with an expectation of being listened to and understood. It was measured with the widely used Parent Adolescent Communication Inventory (PACI), a 20-item instrument (Barnes & Olson, 1985) that participants choose from 5-point Likert-type responses of strongly disagree (1) to strongly agree (5). With a potential minimum score of 20 and a potential maximum score of 100, higher scores indicate greater perceived open communication. The PACI has a youth and a parent version, the difference being the target of the item—mother or father or youth. An example of an item is “When we are having a problem, I often give my child/mother/father the silent treatment.” Alpha coefficient reliabilities in this sample were .69 for parent to youth, .62 for youth to mother, and .77 for youth to father.
Family involvement is the concern and commitment members have toward the family. It was measured with the eight-item Family Involvement Scale adapted by the Evaluation Management Training (EMT) from the Effective Black Parenting Module–Family Strengthening (Alvy, 1996) under contract to the SAMHSA Center for Substance Abuse Prevention (CSAP) Mentoring and Family Strengthening cross-site study (2000). Adults and youth answered a 5-point scale from never (1) to always (5). Scores are created by taking the mean of the eight items, for a potential minimum score of 1 and a potential maximum score of 5, and higher scores indicate greater perceived family involvement. A sample item is, “My parents/child and I do things together at home.” Alpha coefficient reliabilities for this sample were .84 for youth and .80 for adults.
Family supervision is parents knowing where the youth is and being at home at key times of the day. It was measured with the four-item Family Supervision Scale from the CSAP National Youth Survey (Arthur, Hawkins, & Catalano, 1982). Adults and youth answered a 5-point scale from 1 for never to 5 for always. Scores are created by taking the mean of four items with a minimum potential score of 1 and a maximum potential score of 5, and higher scores indicate higher perceived supervision. “I/My parents want to know who my child is/I am with when he or she goes/I go out with friends” is an example of an item. Alpha coefficient reliabilities for this sample were .70 for youth and .85 for adults.
Children’s participation in health risk behaviors is involvement in risk behaviors as conceptualized by the Centers for Disease Control and Prevention Biennial Youth Risk Surveillance Survey, that is, unintentional injury, intentional injury, ATOD use, sexual involvement, and health practices. It was measured with the 21-item Children’s Health Risk Behavior Survey (Riesch et al., 2006). We chose this measure in addition to the CSAP Government Performance Required Accountability (GPRA) measures because the CHRBS included a logic tree to obtain further data if youth admitted to substance use and because it included data on a panel of health risk behaviors beyond ATOD, of interest to our community.
Procedures
Recruitment
Adults and youth were eligible for study participation if they spoke English, the youth was in the fifth grade, and the family intended to stay in the area for 8 months after enrollment. We reasoned from past studies that approximately 20% of invited families would respond. An average of 60 children was enrolled in the fifth grade at each public elementary school. To attain the 150 dyads expected as part of the SAMHSA contract, we needed to include a minimum of 13 schools. We randomly selected 17 schools from the high and low minority enrollment schools.
After approval from the institutional review boards at the collaborating universities and the public school systems in each city, the administration of each particular school was approached. In Madison, 7 schools were approached and in Indianapolis, 10 schools were approached. All approached schools agreed to serve as recruitment sites, except one in Indianapolis. Serving as a recruitment site for the study meant that invitational materials were sent home in school backpacks or U.S. mail to families with a child in the fifth grade. The materials included a letter from the school principal indicating his or her knowledge of the study and that the procedures had been approved by the school district’s research or evaluation committees, but questions should be directed toward the study team.
In Madison, 396 letters of invitation were sent; 66 parents indicated an interest in enrolling by telephone, return of a form to the school, or e-mail; 57 were eligible for the study; and 55 consented to participate, for an enrollment rate of 14%. In Indianapolis, 520 letters of invitation were sent; 148 parents responded as interested in enrolling by telephone, return of a form to the school, or e-mail; 140 were eligible for the study; and 112 consented to participate, for an enrollment rate of 22%. Of those eligible, reasons for not enrolling were lack of time or unwillingness to make the commitment to study procedures.
Data collection
All data were collected by interview at the families’ homes or other location of their choosing at three times (Baseline–Time 1, Post 1–Time 2, and Post 2–Time 3). Data collection points were chosen to assess immediate change within 1 month of program participation (Post 1) and lag effect at 6 months. We reasoned that 6 months would allow for program skill implementation and further development by the youth and was within the contract timeline.
Youth answered survey instruments using a personal digital assistant (PDA) programmed with Pendragon software (Bobula et al., 2004). Adults used a laptop computer. Visits lasted from 60 to 90 min.
Intervention implementation
Staff from the Madison and Indianapolis communities who were bachelor’s prepared or university students were hired and trained to facilitate the SFP 10–14. Trainers from the Iowa State University Extension conducted 2-day sessions on three separate occasions.
Youth and one parent attended the 7-week, 2-hr-per-week program together at community locations in the evenings or weekends in each city. Didactic content was presented by videotape, discussion sessions were timed, and the curriculum was detailed carefully in a manual that contained all the required handouts. Youth and parents or legal guardians were separated for the first of the 2 consecutive hours to work on goal-oriented, developmentally appropriate activities. The dyads were reunited in the second hour for family-oriented activities. The sessions were characterized by lively activities and interactions. Booster sessions were not offered because of the short 2-year duration of the contract.
The three-person teams of trained facilitators conducted 10 groups, 5 in Madison and 5 in Indianapolis. Group size included a minimum of 5 and a maximum of 12 dyads, with an average of 8 dyads attending. Most dyads in each group were from the same school or district region. A content checklist was used to assess implementation fidelity. According to analyses of the checklists, more than 90% of the content was consistently covered in the adult groups and 87% for the youth groups. Sessions also were observed by the project directors on a random basis. The structure provided by the manual, facilitator training, videotaped content, and timed discussions contributed to a high level of intervention fidelity in terms of content delivery.
Minimal contact comparison condition
Comparison group families participated only in the data collection procedures. No comparison families reported participation in another family skill building or parenting program.
Retention strategies
Families participating in both study conditions received three newsletters directed toward games, activities, and issues of interest to parents and children. The content of the newsletter was neutral on family environment and substance use. Cash or Wal-Mart gift cards were provided on completion of surveys: $10, $15, and $20 for youth and $20, $30, and $40 for adults at Times 1, 2, and 3, respectively.
Research staff telephoned and mailed reminders to adults to increase retention in both groups. Our community advisors and other investigators have implemented strategies to assist with retention in the intervention group. A meal was served as an on-time incentive immediately before the sessions began. Transportation through the use of vouchers and child care was available. All program sessions were delivered at the schools, community centers, churches, a mall, or clinics in the participant’s neighborhoods.
Data analyses
All data from the laptop computers and PDAs were converted to SPSS and other software packages for statistical analyses. The data were assessed for level and type of missingness, specifically for missing completely at random (MCAR; Little & Rubin, 1987). Using the BMDP8D routine (Dixon et al., 2009), assessment of the various t values and variance ratios for the three data collection periods (baseline, Post 1, and Post 2) indicated the data were MCAR.
Because this was a clustered randomized trial, the data included multilevel or hierarchically structured samples. Adult–youth dyads were clustered within each school. A two-level regression model was used (Rasbash, Charlton, Browne, Healy, & Cameron, 2009) with a dummy variable for treatment effects to avoid underestimating standard errors of regression coefficients from fitting a model that did not recognize clustering. Baseline measures were used as covariates in each analysis. The model for assessing change was a multilevel model for fixed-occasion repeated outcomes (Goldstein, 1995; Yang, Health, & Goldstein, 2000). The model was written as a two-level hierarchical structure, where outcome was a function of the intervention and other covariates. The intercepts were modeled as random variables. This provided variance–covariance matrices at the fixed-occasion level and the dyad level. Two variance–covariance matrices were estimated. These matrices provided both estimates of variance and covariance of the intervention effect at the fixed occasions, and across and between dyads.
A second series of two-level regression models were conducted to explore the issue of dosage effect of intervention on these outcome measures. A (k – 1) treatment dose variable dichotomized into high dose (dyads attending five or more sessions) and low dose (dyads attending four or fewer sessions), with the comparison group as reference, was replaced in the model. This approach provided two treatment variables instead of the single treatment dummy.
Results
Sample Description
One hundred sixty-seven adult–youth dyads were enrolled in the study. Of these, 55 were from Madison and 112 were from Indianapolis. More than half the adult–youth dyads were African American and another third were Euro-American. About half the sample reported an annual income that was below $25,000 annually and a third reported an income above $50,000 annually. Half the sample reported they received some form of public assistance. Adults were in their late thirties, female, tended to be educated beyond high school, employed, and married. The youth average age was 10.8 years (SD = 0.69) and half were male.
Analyses of demographic variables included exact two binomial unconditional tests (Chan & Zhang, 1999), unordered R × C exact tests (Lydersen, Pradham, Senchaudhuri, & Laake, 2005), and parametric mean contrasts. All exact tests were run in StatXact-8 Procs (2008). No differences in any of the characteristics were found between the intervention and comparison conditions (see Table 2).
Table 2.
Characteristics of the Sample
| Intervention Group |
Full-Dose Group |
Partial-Dose Group |
Comparison Group |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | n | % | n | % | n | % | n | % | Statistics α Error |
| Race of adult | χ2 = 2.709, df = 4, αea = 0.7422b | ||||||||
| African American | 47 | 55 | 20 | 49 | 27 | 60 | 45 | 56 | |
| Asian | 1 | 1 | – | – | 1 | 2 | 1 | 1 | |
| Alaska Native, Native American | 1 | 1 | – | – | 1 | 2 | – | – | |
| Hispanic | 4 | 5 | 1 | 2 | 3 | 7 | 1 | 1 | |
| Euro-American | 31 | 37 | 20 | 49 | 11 | 25 | 32 | 40 | |
| Missing | 1 | 1 | – | – | 1 | 1 | 2 | 2 | |
| Race of youth | χ2 = 3.142, df = 5, αe = .8180b | ||||||||
| African American | 48 | 56 | 20 | 49 | 28 | 62 | 44 | 54 | |
| Asian | 1 | 1 | – | – | – | – | 1 | 1 | |
| Alaska Native, Native American | 1 | 1 | 1 | 2 | – | – | – | – | |
| Hispanic | 3 | 4 | 1 | 2 | 2 | 4 | 1 | 1 | |
| Euro-American | 30 | 35 | 19 | 47 | 11 | 25 | 32 | 40 | |
| Other | 1 | 1 | – | – | 1 | 2 | 1 | 1 | |
| Missing | 3 | 3 | – | – | 3 | 7 | 2 | 3 | |
| Gender of adult | χ2 = 0.4017, df = 1, αe = .6207b | ||||||||
| Male | 8 | 9 | 10 | 12 | |||||
| Female | 78 | 91 | 71 | 88 | |||||
| Gender of youth | χ2 = 0.0487, df = 1, αe = .8774b | ||||||||
| Male | 45 | 51 | 21 | 51 | 24 | 53 | 41 | 50 | |
| Female | 41 | 47 | 20 | 49 | 21 | 47 | 40 | 50 | |
| Missing | 2 | 2 | – | – | – | – | – | – | |
| Receiving public assistance | χ2 = 1.272, df = 1, αe = .2792b | ||||||||
| Yes | 51 | 60 | 17 | 42 | 34 | 75 | 41 | 50 | χ2 = 0.914, df = 1, αe = .443c |
| No | 35 | 40 | 24 | 58 | 11 | 25 | 40 | 50 | χ2 = 7.467, df = 1, αe = .007d |
| Annual income | χ2 = 13.53, df = 10, αe = .1925b | ||||||||
| $0–5,000 | 4 | 5 | – | – | 4 | 9 | 1 | 1 | |
| $5,001–10,000 | 12 | 14 | 3 | 7 | 9 | 21 | 5 | 6 | |
| $10,001–15,000 | 7 | 8 | 3 | 7 | 4 | 9 | 10 | 12 | |
| $15,001–20,000 | 14 | 16 | 4 | 10 | 10 | 22 | 8 | 10 | |
| $20,001–25,000 | 7 | 8 | 2 | 5 | 5 | 11 | 9 | 11 | |
| $25,001–30,000 | 1 | 1 | – | – | 1 | 2 | 7 | 9 | |
| $30,001–35,000 | 7 | 8 | 5 | 12 | 2 | 4 | 7 | 9 | |
| $35,001–40,000 | 3 | 4 | 2 | 5 | 1 | 2 | 7 | 9 | |
| $40,001–45,000 | 1 | 1 | 1 | 2 | – | – | 2 | 3 | |
| $45,001–50,000 | 2 | 2 | 2 | 5 | – | – | 2 | 3 | |
| >$ 50,000 | 25 | 29 | 17 | 42 | 8 | 18 | 25 | 31 | |
| Missing | 3 | 4 | 2 | 5 | 1 | 2 | – | – | |
| Poverty index | χ2 = 10.89, df = 1, αe = .008b | ||||||||
| High | 34 | 41 | 9 | 23 | 25 | 57 | 54 | 67 | χ2 = 20.06, df = 1, αe = <.001c |
| Low | 49 | 59 | 30 | 77 | 19 | 43 | 27 | 33 | χ2 = 1.189, df = 1, αe = .332d |
| Education of adult | χ2 = 1.80, df = 6, αe= .9783b | ||||||||
| Grade school | 1 | 1 | 1 | 2 | – | – | – | – | |
| Some high school | 10 | 12 | 2 | 5 | 8 | 18 | 8 | 10 | |
| High school | 21 | 24 | 7 | 17 | 14 | 31 | 18 | 22 | |
| Some college | 17 | 20 | 5 | 12 | 12 | 27 | 14 | 17 | |
| College | 17 | 20 | 11 | 27 | 6 | 14 | 14 | 17 | |
| Trade or technical college | 4 | 5 | 2 | 5 | 2 | 4 | 6 | 7 | |
| Postcollege | 13 | 15 | 11 | 27 | 2 | 4 | 13 | 16 | |
| Missing | 3 | 4 | 2 | 5 | 1 | 2 | – | – | |
| Employment status | χ2 = 0.5645, df = 2, αe = .7703b | ||||||||
| Full-time | 39 | 45 | 20 | 48 | 19 | 42 | 41 | 51 | |
| Part-time | 17 | 20 | 8 | 20 | 9 | 20 | 18 | 22 | |
| Not employed | 27 | 31 | 11 | 27 | 16 | 36 | 22 | 27 | |
| Missing | 3 | 4 | 2 | 5 | 1 | 2 | – | – | |
| Adult partnered | χ2 = 3.490, df = 1, αe = .084b | ||||||||
| Yes | 33 | 40 | 22 | 56 | 11 | 25 | 44 | 54 | χ2 = 0.046, df = 1, αe = .847c |
| No | 50 | 60 | 17 | 44 | 33 | 75 | 37 | 46 | χ2 = 9.948, df = 1, αe = .002d |
| Adult age | t = −0.885, df = 165, αe = .3774 | ||||||||
| M | 38.7 | 39.9 | |||||||
| SD | 8.62 | 8.9 | |||||||
| Minimum | 21 | 26 | |||||||
| Maximum | 66 | 71 | |||||||
| Youth age | t = 0.281, df = 165, αe = .7791b | ||||||||
| M | 10.8 | 10.8 | |||||||
| SD | 0.68 | 0.70 | |||||||
| Minimum | 10 | 10 | |||||||
| Maximum | 12 | 13 | |||||||
Exact alpha error.
Intervention vs. comparison.
Full dose vs. comparison.
Partial dose vs. comparison.
Asymptotic alpha error.
Attrition and Attendance
Thirty-five families withdrew from the study from Baseline to Post 2 for an overall attrition rate of 21%. The Madison site lost 15 families (10 intervention and 5 comparison) and the Indianapolis site lost 20 families (10 intervention and 10 comparison). No significant differences among sociodemographic characteristics were found between those who completed the study and those who did not at each site.
Outcome Analyses
Research Question 1: Main outcome results
There are nine potential outcomes: youth perception of cohesion, parent perception of cohesion, youth perception of communication with mother, youth perception of communication with father, mother perception of communication with the youth, youth perception of family involvement, parent perception of family involvement, youth perception of family supervision, and adult perception of family supervision at Post 1 and at Post 2. There were too few fathers (eight at Post 1 and five at Post 2) responding to the measure of father perception of communication with the youth. This potential outcome, therefore, was dropped from analyses.
Unadjusted scores for the outcome measures are displayed in Table 3 for baseline, Post 1, and Post 2. The intention-to-treat analysis focused on the differences in the nine outcomes between the intervention and comparison conditions at Post 1 and Post 2 controlling for baseline levels. The results for the intention-to-treat analysis are displayed in Table 4, Model 1. Only adult perception of family supervision increased significantly at Post 1, but this finding was not stable to Post 2.
Table 3.
Unadjusted Means and Standard Deviation Scores for Study Variables at All Three Time Points for Intervention Participants Broken Down by Full- and Partial-Dosea and Comparison Group Participants
| Time 1: Baseline | Time 2: Post 1 | Time 3: Post 2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Intervention | Intervention | ||||||||||
| Variable | Control | All | Full Dose |
Partial Dose |
Control | All | Full Dose |
Partial Dose |
Control | All | Full Dose |
Partial Dose |
| Youth perception of family cohesion | ||||||||||||
| n | 81 | 83 | 39 | 44 | 67 | 70 | 37 | 33 | 63 | 50 | 30 | 20 |
| M | 37.59 | 37.76 | 38.69 | 36.93 | 36.71 | 38.61 | 39.80 | 37.28 | 38.54 | 39.56 | 41.01 | 37.39 |
| SD | 5.77 | 5.89 | 5.92 | 5.80 | 6.44 | 6.38 | 5.42 | 7.15 | 6.13 | 7.16 | 6.19 | 8.10 |
| Adult perception of family cohesion | ||||||||||||
| n | 81 | 83 | 38 | 45 | 68 | 73 | 38 | 35 | 46 | 45 | 26 | 19 |
| M | 39.85 | 39.73 | 40.5 | 39.19 | 39.79 | 39.55 | 40.76 | 38.23 | 38.91 | 40.38 | 40.5 | 40.2 |
| SD | 5.06 | 5.49 | 5.33 | 5.60 | 5.07 | 6.05 | 5.27 | 6.62 | 4.97 | 4.63 | 4.66 | 4.71 |
| Youth perception of openness of communication with mother | ||||||||||||
| n | 80 | 83 | 38 | 45 | 70 | 72 | 38 | 34 | 48 | 44 | 25 | 19 |
| M | 71.02 | 68.94 | 71.42 | 66.85 | 69.94 | 69.97 | 71.80 | 67.92 | 70.03 | 70.25 | 75.43 | 63.43 |
| SD | 12.62 | 13.36 | 15.81 | 10.62 | 16.03 | 12.21 | 12.14 | 12.13 | 14.94 | 17.61 | 15.65 | 18.10 |
| Youth perception of openness of communication with father | ||||||||||||
| n | 73 | 75 | 35 | 40 | 60 | 66 | 35 | 31 | 37 | 38 | 22 | 16 |
| M | 65.59 | 65.14 | 65.65 | 64.69 | 68.92 | 68.40 | 70.62 | 65.89 | 72.83 | 74.41 | 78.82 | 63.98 |
| SD | 15.04 | 14.76 | 18.26 | 11.05 | 16.58 | 14.53 | 14.58 | 14.30 | 13.64 | 16.74 | 13.19 | 18.61 |
| Mother perception of openness of communication with youth | ||||||||||||
| n | 71 | 76 | 35 | 41 | 60 | 65 | 34 | 31 | 41 | 40 | 23 | 17 |
| M | 75.08 | 73.68 | 76.06 | 71.66 | 72.92 | 75.48 | 77.26 | 73.52 | 73.32 | 76.60 | 79.74 | 72.35 |
| SD | 11.40 | 10.80 | 9.06 | 11.82 | 11.19 | 9.53 | 8.13 | 10.65 | 12.59 | 11.62 | 7.61 | 14.71 |
| Youth perception of involvement with the family | ||||||||||||
| n | 78 | 77 | 38 | 39 | 69 | 72 | 37 | 35 | 61 | 61 | 34 | 27 |
| M | 4.01 | 4.02 | 4.01 | 4.02 | 4.02 | 3.88 | 4.09 | 3.65 | 4.06 | 4.05 | 4.14 | 3.93 |
| SD | 0.69 | 0.72 | 0.67 | 0.78 | 0.81 | 0.89 | 0.74 | 0.98 | 0.83 | 0.83 | 0.78 | 0.89 |
| Adult perception of involvement with the family | ||||||||||||
| n | 74 | 76 | 37 | 39 | 70 | 70 | 36 | 34 | 61 | 63 | 35 | 28 |
| M | 4.01 | 4.02 | 3.96 | 4.13 | 4.08 | 4.15 | 4.09 | 4.20 | 4.04 | 4.11 | 4.06 | 4.17 |
| SD | 0.53 | 0.53 | 0.47 | 0.57 | 0.52 | 0.51 | 0.48 | 0.53 | 0.53 | 0.51 | 0.52 | 0.49 |
| Youth perception of family supervision | ||||||||||||
| n | 63 | 64 | 31 | 33 | 56 | 63 | 33 | 30 | 51 | 59 | 32 | 27 |
| M | 4.24 | 4.28 | 4.28 | 4.29 | 4.41 | 4.21 | 4.34 | 4.07 | 4.27 | 4.35 | 4.45 | 4.22 |
| SD | 0.69 | 0.78 | 0.72 | 0.85 | 0.76 | 0.78 | 0.72 | 0.84 | 0.90 | 0.78 | 0.57 | 0.97 |
| Adult perception of family supervision | ||||||||||||
| n | 74 | 76 | 37 | 39 | 70 | 70 | 36 | 34 | 61 | 63 | 35 | 28 |
| M | 4.76 | 4.82 | 4.83 | 4.80 | 4.72 | 4.84 | 4.82 | 4.85 | 4.71 | 4.74 | 4.76 | 4.71 |
| SD | 0.31 | 0.27 | 0.22 | 0.32 | 0.33 | 0.25 | 0.2 | 0.22 | 0.34 | 0.36 | 0.30 | 0.43 |
Participants were not randomized to full- and partial-dose conditions, analyses were conducted post hoc.
Table 4.
SFP 10–14 Effect Sizes With Covariates of Baseline Measure, Poverty Index, and Partner Status on Proximal Outcomes at Post 1 and Post 2 for Intervention, Full Dose, and Partial Dose Conditions Contrasted With the Comparison Group
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| Intervention vs. Comparison | Full Dose vs. Comparison | Partial Dose vs. Comparison | ||||
| Variable | Time 2 Post 1 | Time 3 Post 2 | Time 2 Post 1 | Time 3 Post 2 | Time 2 Post 1 | Time 3 Post 2 |
| Youth report of family cohesion Nowcy | 0.301 [−0.04, 0.64] | 0.049 [−0.32, 0.43] | 0.51* [0.095, 0.93] | 0.44* [0.001, 0.90] | 0.18 [−0.24, 0.60] | −0.36 [−0.86, 0.15] |
| Adult report of family cohesion Nowca | −0.12 [−0.46, 0.21] | 0.18 [−0.15, 0.51] | 0.002 [−0.40, 0.41] | 0.28 [−0.23, 0.78] | −0.15 [−0.56, 0.25] | 0.25 [−0.28, 0.79] |
| Youth report of openness of communication with mother Paciy_m | 0.18 [−0.15, 0.64] | 0.16 [−0.25, 0.57] | 0.18 [−0.22, 0.59] | 0.45 [−0.05, 0.96] | 0.17 [−0.24, 0.58] | −0.15 [−0.68, 0.38] |
| Youth report of openness of communication with father Paciy_f | 0.02 [−0.34, 0.38] | −0.14 [−0.61, 0.33] | 0.19 [−0.25, 0.63] | 0.31 [−0.25, 0.87] | −0.16 [−0.61, 0.29] | −0.67** [−1.29, −0.06] |
| Mother’s report of openness of communication with youth Pacim | −0.04 [−0.43, 0.37] | 0.10 [−0.29, 0.50] | 0.36 [−0.07, 0.79] | 0.19 [−0.33, 0.73] | 0.25 [−0.19, 0.69] | −0.05 [−0.62, 0.51] |
| Youth perception of involvement with the family Fminv_y | −0.27 [−0.61, 0.07] | −0.01 [−0.38, 0.35] | 0.04 [−0.38, 0.46] | 0.16 [−0.28, 0.60] | −0.48** [−0.92, −0.06] | −0.12 [−0.60, 0.35] |
| Parent perception of involvement with the family Fminv | 0.19 [−0.16, 0.54] | 0.11 [−0.26, 0.48] | 0.18 [−0.25, 0.59] | 0.15 [−0.2, −0.60] | 0.20 [−0.23, 0.64] | −0.12 [−0.60, 0.34] |
| Youth perception of family supervision Fsupv_y | −0.12 [−0.53, 0.28] | 0.28 [−0.15, 0.71] | 0.06 [−0.43, 0.54] | 0.35 [−0.17, 0.86] | −0.26 [−0.78, 0.25] | 0.29 [−0.25, 0.82] |
| Adult perception of family supervision Fsupv | 0.40* [0.05, 0.75] | 0.16 [−0.61, 0.07] | 0.55* [0.12, 0.98] | 0.25 [−0.20, 0.69] | 0.41 [−0.02, 0.85] | 0.07 [−0.4, 0.54] |
Note: Values are Cohen’s d [95% confidence interval]. Cohen’s d was calculated using: .
Significant change in expected direction.
Significant change in opposite than expected direction.
Research Question 1: Secondary outcome results
The second set of analyses, presented as Model 2 in Table 4, focused on dosage. This analysis was an exploratory, post hoc analysis. Full dose was defined as attendance at five of seven sessions. Twenty of 31 dyads in the intervention condition at the Madison site were full-dose attendees and 22 of the 55 dyads in intervention condition at the Indianapolis site were full-dose attendees.
The sociodemographic variables were reexamined for differences between the partial and full-dose conditions and the comparison condition. It was found that a higher proportion of participants in the partial dose condition received Public Assistance (χ2 = 7.467, df = 1, αe = 0.007) and reported a low income (χ2 = 21.46, df = 10, αe = 0.012) when contrasted with those in the comparison condition. A higher proportion of participants in the full-dose condition were partnered than in the comparison condition (χ2 = 9.948, df = 1, αe = 0.002). We reasoned that income and partner status could confound the intervention outcomes. Thus, we created two new variables to address income and partner status.
First, we pursued the widely accepted practice of examining poverty threshold, which takes into account not only income but number of children and adults in the home. The 2003 rates (www.census.gov/hhes/www/poverty/threshld/thresh03.html), consistent with the year data were collected, were used to determine poverty status. Participants were coded as in poverty or not. Second, we developed a partner status variable. Adults who reported they were married or living with a partner were considered partnered and adults who reported they were single, divorced, or widowed were considered not partnered.
Examining the full- and partial-dose conditions for poverty and partner status, it was found that dyads in the partial dose condition were more likely to meet the threshold for poverty than those in the full-dose condition (57% vs. 23%, p = 0.02) and less likely to be partnered than those in the full-dose condition (25% vs. 54%, p = 0.0002). Because of these findings, we used poverty status (yes vs. no) and partner status (partnered vs. not) as covariates in Model 2.
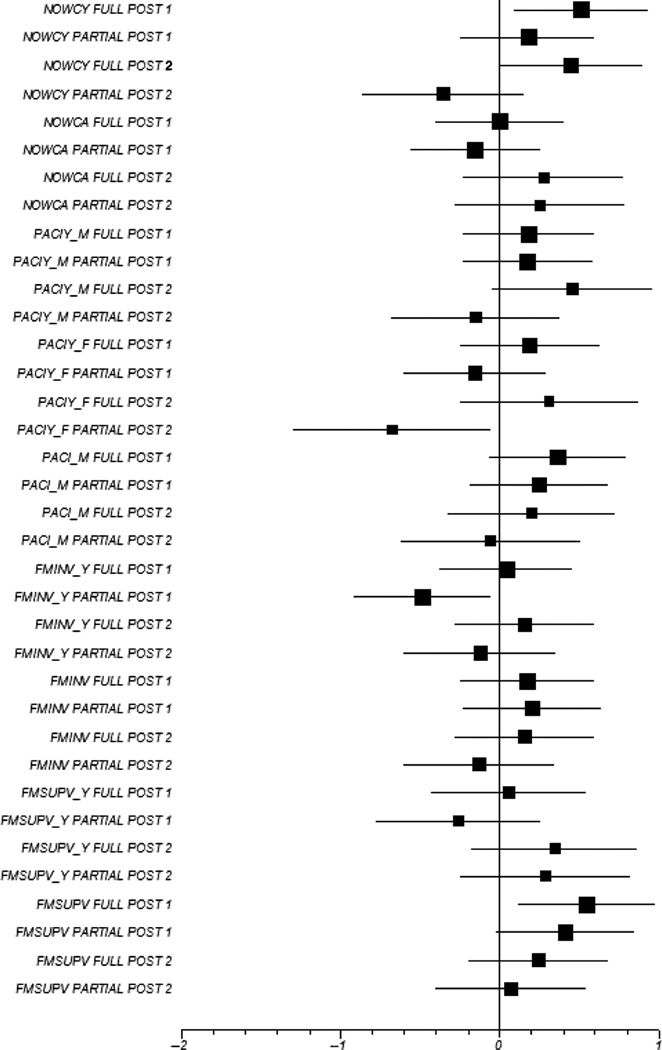
As displayed in Table 4, among dyads who received the full dose, there were three statistically significant findings. Youth perceived more cohesion at Post 1 and Post 2 than youth in the comparison condition, whereas adults perceived more supervision at Post 1 than adults in the comparison condition.
As displayed in Table 4, significant outcomes among youth who received a partial dose were in the direction opposite than expected, that is, youth who received a partial dose perceived their communication with their father as statistically significantly less open at Post 2 and their involvement in the family as statistically significantly less at Post 1 than youth in the comparison condition.
Effect size was computed as the difference between two groups (d dyad effect size), to determine if the magnitude of differences are of practical concern. In this study, the d dyad effect size consisted of variations over standardized mean difference assessed in the two-level regression models (Cohen, 1988). Both statistically significant and nonsignificant effect sizes from this study are reported. Our practice is in agreement with the position of Roberts and Henson (2003) that reporting of both provides information needed for replication or meta-analysis, a potentially valuable contribution to the field.
Of the nine outcomes repeatedly measured at Post 1 and Post 2 among adults and youth who received the full dose, all were in the expected direction. At Post 1 in the full-dose condition, there were three noteworthy effect sizes: youth report of family cohesion with an effect size of d = 0.51, adult perception of family supervision with an effect size of d = 0.55, and mother’s perception of open communication with the youth with an effect size of d = 0.36. These three particular effect sizes decreased at Post 2. Five of the nine outcomes with small effect sizes at Post 1 improved by Post 2, some to medium-size effect sizes. Only parent perception of involvement with the family showed no change in effect size (Table 4; Full dose vs. Comparison Groups).
Of the nine outcomes measured at Post 1 among adults and youth who received a partial dose, five outcomes were in the expected direction: youth perception of cohesion, youth perception of open communication with mother, mother’s perception of open communication with youth, adult perception of family involvement, and adult perception of family supervision. Four outcomes measured at Post 1 were in the opposite direction: adult perception of cohesion, youth perception of open communication with father, youth perception of family involvement, and youth perception of family supervision.
Of the nine outcomes measured at Post 2 among adults and youth who received a partial dose, three were in the expected direction: adult perception of cohesion, youth perception of family supervision, and adult perception of family supervision. Six outcomes were opposite the expected direction: youth perception of cohesion, youth perception of open communication with mother, youth perception of open communication with father, mother’s perception of open communication with youth, youth perception of family involvement, and mother’s perception of family involvement.
The effect sizes are displayed in Table 4 and Figure 2. In Figure 2, the size of the box represents the number of respondents for the measure.
Figure 2.
Effect sizes for outcomes of youth and adults in full- and partial-dose intervention groups at Post 1 and Post 2
Research Question Two
Youth participation in any of the ATOD behaviors was very low, did not provide sufficient numbers for modeling, and is displayed for Post 2 only in Table 5. Basic proportions were conducted using exact tests. No significant differences were documented in youth ATOD use over time or between the intervention and comparison conditions. The CSAP GPRA items also were analyzed, and included youth report of alcohol, tobacco, snuff, and illegal drugs in the past 30 days. The findings were nearly identical to the CHRBS findings.
Table 5.
Frequency, Exact Alpha, Absolute Proportional Differences, 95th Percentile Confidence Intervals for Youth Report of ATOD Use Postprogram for the Intervention and Comparison Groups
| Time 3: Post 2 | |||||||
|---|---|---|---|---|---|---|---|
| Variable | Intervention | Comparison | Exact Alpha |
Abs. Prop. Diff.a |
95% CI Pr.b | ||
| Substance | n | % | n | % | |||
| Smoked a cigarette, even one puff | 0.87 | 0.01 | −0.10, 0.12 | ||||
| No | 57 | 86.4 | 58 | 87.9 | |||
| Yes | 5 | 7.6 | 6 | 9.1 | |||
| Missingc | 1 | 1.5 | 2 | 3.0 | |||
| Smoked a whole cigarette | 0.86 | 0.09 | −0.45, 0.61 | ||||
| No | 4 | 6.1 | 4 | 6.1 | |||
| Yes | 2 | 3.0 | 3 | 4.5 | |||
| Missingc | 41 | 62.1 | 44 | 66.7 | |||
| Drank wine, beer, or liquor without parent permission | 1.00 | 0.00 | −0.07, 0.06 | ||||
| No | 61 | 92.4 | 63 | 95.5 | |||
| Yes | 1 | 1.5 | 1 | 1.5 | |||
| Missing | 1 | 1.5 | 2 | 3.0 | |||
| Chewed tobacco | 0.55 | 0.02 | −0.06, 0.13 | ||||
| No | 58 | 87.9 | 59 | 89.4 | |||
| Yes | 3 | 4.5 | 5 | 7.6 | |||
| Missing | 2 | 3.0 | 2 | 3.0 | |||
| Smoked marijuana | 0.65 | 0.01 | −0.09, 0.05 | ||||
| No | 59 | 89.4 | 63 | 95.5 | |||
| Yes | 2 | 3.0 | 1 | 1.5 | |||
| Missing | 2 | 3.0 | 2 | 3.0 | |||
| Used inhalants | – | 0.00 | – | ||||
| No | 62 | 93.9 | 64 | 97.0 | |||
| Yes | |||||||
| Missing | 1 | 1.5 | 2 | 3.0 | |||
Note: SFP = Strengthening Families Program; ATOD = alcohol, tobacco, and other drug.
Refers to Absolute Proportional difference
Refers to 95% CI proportional difference
The missing data are due to the item being changed from smoked a whole cigarette to smoked a cigarette even one puff after the study began. The latter question was more appropriate for the age group than the former question.
Discussion
The SFP 10–14 is a SAMHSA model program designed to reduce youth participation in substance use by building family capacity. Although our SAMHSA contract included a multitude of assessments, our communities were most interested in the family capacity variables of cohesion, communication, involvement, and supervision. Other than the finding that adults in the intervention group adults perceived better supervision at Post 1 than adults in the comparison group, no perceptions changed significantly postintervention. Taking into account a dose effect, parents and youth who participated in the full dose of the intervention demonstrated all nine outcomes in the expected direction, with youth report of family cohesion improving significantly at Post 1 with stability to Post 2. Three of the nine effect sizes at Post 1 were moderately large, and five others increased from Post 2 to Post 3. The range of effect sizes by Post 2 in the full-dose condition were d = 0.15 to d = 0.45, respectable effect sizes suggesting positive results.
A key finding of this study is the number of outcomes that were contrary to prediction among the partial-dose group. Youth perception of open communication with their mother and with their father and youth perception of family involvement were consistently opposite of the expected direction. In fact, most of the youth and adult outcomes were contrary to prediction in the partial-dose group.
Attrition from this study was 21%, below the 30% reported by Gottfredson et al. (2006) and similar to the 22% reported by Spoth, Clair, et al. (2006). Analyses indicated that attrition did not vary by condition, site, baseline measures, or demographic measures. It seems unlikely then that attrition from the study biased the results in any important way.
The findings that adults and youth who received a partial dose had many outcomes in the direction opposite of that expected leads to speculation about the factors that may contribute to the finding. These factors may include dyadic factors and study factors. Our thinking about the dyadic factors is discussed here. Study factors will be addressed under intervention fidelity.
Dyadic factors
Adult–youth dyads who completed SFP 10–14 may be compliant, a trait that may coincide with a positive family environment. If the motivation for participating in the study among parents was to improve family functioning, those already functioning well but who desire to be the best they can be have limited potential gains.
The youth at our site demonstrated very little ATOD behavior. Conforming behavior among these youth may have been the norm, raising little concern among parents. Although we intended to provide parents and youth with the skills and techniques to handle problems or decisions about future risk situations, the lack of being tested in these situations may make the content abstract rather than applied.
Adult–youth dyads who did not complete SFP 10–14 may have observed how a family could function and found the skills to move toward that goal unattainable or not valued. These families may have experienced a cognitive dissonance or effect in their families that was in contrast to the higher attending families.
The factors that prevent youth and adults from attending groups may be the same factors that contribute to less-than-optimal family environments. Poverty status and partner status provided some insight into this finding. Dyads who received the partial dose were more likely to be in the poverty and nonpartnered categories, suggesting that poverty and single parenthood contributed to the dyad’s ability to attend intervention sessions. Despite our efforts to present the content in a youth-friendly, fun format, some youth may not have wanted to attend. Although the finding of low attendance among low-income and single-parent families is not surprising, it is disappointing given the input we gathered and followed from our community advisors.
The dosage analyses were revealing, but the factors that account for the dyads’ outcomes beyond the poverty and partner status remain unconfirmed. The factors that motivated the intervention completers are similarly unconfirmed.
Theory
The entire Bio-psychosocial Vulnerability Model guided this study. It may be too broad to underpin the four bidirectional concepts chosen as indicative of the family environment: cohesion, communication, involvement, and supervision. A model that is specific to bidirectionality of family environment characteristics may need construction. If the Bio-psychosocial Vulnerability Model was too broad for application, it follows that the SFP 10–14 may take too broad an approach to strengthening the family environment.
Intervention fidelity
An important aspect of intervention fidelity is staff training. Prior to delivery of SFP 10–14, in-depth analysis of the content, competence of the interventionists, consistency of implementation, and strategies to handle a wide range of participants’ responses were accomplished. Interventionists were trained by staff who contributed to the adaptation of SFP 10–14 into the seven-session program from Extension Services at Iowa State University (Lee Molgaard). The staff adherence to intervention content was assessed through trained facilitators keeping with the manualized content.
The target for the intervention constitutes another important aspect of intervention fidelity. SFP 10–14 is targeted to entire families with children aged 10 to 14 years. In this study, only one parent, typically a mother, and one index child attended. Achieving family environment change is more likely if all family members receive the intervention. Although change was achieved in other studies focused on parent–teen relationships among youth–adult dyads (Anderson et al., 1999; Lederman, Chan, & Roberts-Gray, 2008; Riesch et al., 1993), it is considered difficult and not likely unless all family members are recipients of the intervention. In other studies that report positive results from the SFP 10–14, the program was delivered in schools, not community settings (Gottfredson et al., 2006; Spoth, Shin, et al., 2006).
Participant engagement and involvement, another aspect of intervention fidelity, was not formally measured. Although we observed lively sessions, it does not follow that youth and adults received the content as intended.
A portfolio of strengthening families’ curricula have been developed, tested, and culturally adapted for families of preschool, elementary, middle, and high school students (http://strengtheningfamiliesprogram.org/about.html#cultural). We chose the universal SFP 10–14 intervention. We reasoned that all families with children making the transition from elementary to middle school were at risk for substance use. Thus, our target was all families with fifth-grade youth.
Selecting the appropriate program for the appropriate population is an important aspect of intervention fidelity. Income level and partner status constitute potential moderators of program effect. To demonstrate program effect with the low-income and single-parent families in this study, we might have shown a greater effect if we had chosen the 14-session SFP 6–11 program that is targeted to higher risk families. The program we chose, SFP 10–14, is a concentrated 7-session adaptation of the content and format of the original 14-session program. With only 7 sessions to attend, low-income or single-parent families may have had a harder time receiving a high dosage than if they had had 14 sessions available to attend.
Ceiling effects
Many of the adult–youth dyads were functioning highly on the outcome variables at study intake. The unadjusted means, standard deviations, and minimum and maximum scores (see Table 3) demonstrated little variability. On all the measures, scores are in the upper third or higher, suggesting little potential for upward movement, indicating a probable ceiling effect.
Intervention power
In the everyday full lives of parents and youth, how powerful can seven weeks of assignments, role-playing, discussion, videos, and demonstration–return demonstration be? Changing 10 or more years of interaction patterns with a few hours of instruction is challenging, even if participants are highly motivated. In a study following parents and youth roughly 10 years after participation in a family communication skills training, all 33 youth and all 25 adults recontacted remembered participating. But when asked what would have helped them communicate more effectively during the youth’s early teen years, most of the suggestions were content from the intervention but apparently not attributed to the intervention (Riesch, Jackson, & Chanchong, 2003). To constitute memorable lessons, the content needs to be stunning. In addition, there is potentially a plethora of confounding variables that may interfere with change.
Nurses who practice in community settings, such as schools, often seek evidence-based programs for families. Nurses in school districts and public health agencies may consider training interdisciplinary staff in the universal SFP 10–14 or one of the SFP portfolio of effective programs. Regular availability of family strengthening programs at normal, developmental transitions for all families may be a major contribution to improve family functioning and the prevention of substance use among children and adolescents. Regular and expected availability and attendance may decrease the stigma associated with attending family strengthening or parenting programs.
Targeting families at risk, those in poverty for example, may be welcomed in communities and schools. The special challenges of single parenting may be addressed with a targeted program. In other words, the needs of the community of childrearing families should drive the program delivered.
Substance use is a constant challenge to adolescent health. There are numerous programs available but few involve the family as the SFP series does. Practitioners may be benefit from reviewing the Cochrane Collaboration documents (Faggiano et al., 2005; Foxcroft, Ireland, Lowe, & Breen, 2002) or the SAMHSA model program site for universal or targeted programs worthy of dissemination to school or community populations (http://www.nrepp.samhsa.gov/).
Nurse researchers need to know the mechanism by which interventions work. Without this knowledge, interventions are merely black boxes without theoretical or empirical grounding to explain the outcomes. The effect size analyses we conducted substantiate to a degree that full participation in SFP 10–14 indeed moves the family environment, namely cohesion, communication, involvement, and supervision in the expected direction.
Nurse researchers may wish to consider dosage when evaluating intervention efficacy and effectiveness. Intervention content and strategy is generally developed from theory, but dosage is rarely considered. Community-based interventions usually address convenience, participant burden, delivery mechanisms (face-to-face, web-based), and number of total sessions to convey content. It might behoove intervention developers to assign priority to content and strategies to achieve outcome. For example, does content build? Do some strategies address multiple levels of content and for that reason must be received by all participants? What is the minimum dose to achieve an outcome? How might dose interact with other factors such as individual, dyadic, or family characteristics or motivation? Analogous to pharmacological or physiological interventions, how is dose calculated for optimal effect?
Nurse researchers are challenged with determining methods to engage all members of families in interventions to strengthen family environments and functioning. The inclusion of adults with fathering responsibilities remains a particular challenge. Successful engagement of entire families, including both parents if there two parents, was achieved by Kumpfer, Alvarado, Tait, and Turner (2002) and Golan (2006). Kumpfer et al. held family fun evenings with a meal at schools. They enrolled 655 families in 12 schools with a population of 1,110 first-grade students for a 59% enrollment rate. Golan makes parent attendance at her Parent Agency Targeting Children’s Health program a requisite for medical and psychosocial treatment of child overweight. Approaching parenting androgynously is one suggestion to reduce perceptions that parenting is a feminine role (Golan, 2006).
Finally, the timing of interventions so that the content is especially relevant and available when the need for it arises needs additional study. To prevent behavior, it is generally agreed that evidence-based strategies should be introduced prior to the behavior. With children and adolescents, this timing is far from constant. Our delivery of the program in the fifth grade may have been too early for dyads to use the skills.
A major strength of the program, one that was welcomed in the communities and schools, was the inclusion of parents as active participants with their children. Several parents asked for more sessions, booster sessions, and more opportunities through their schools. Parents and youth who attended the SFP 10–14 were effusive in their praise of the content, delivery, group method, facilitators, and inclusion of parent and child together.
The handheld computer–assisted survey interview method of evaluation was highly rated by the youth and parents. It was perceived as fun and private by youth. This method may have contributed to the relative lack of missing data.
The Three Rs (representativeness, robustness, and replicability) were adhered to in the design and conduct of the study. Participants were representative of the communities they lived in. Staff members were similar racially, ethnically, and socioeconomically to the participants. The settings were community based. Robustness of delivery across subgroups, staff, and conditions was strong. Potential for replicability under different contexts is strong.
The sample size was powered for the large, cross-site study. Our site was one of seven across the nation. Subsequently, our analyses for a single site may be underpowered. The sample was followed for only a short time, 8 months after intake. Little change in youth development or acquisition of ATOD behaviors occurred to strain the techniques learned in SFP 10–14. Booster sessions, to refresh the content, are considered standard for the program. Their absence may have influenced results. The duration of the SAMHSA contract prohibited our ability to offer the sessions before contract conclusion. Finally, the dosage analyses were post hoc, possibly contributing to potential bias because the full and partial group assignment was nonrandom.
To our knowledge, this is the only independent study of SFP 10–14 not to replicate previous published outcomes. Although the expected outcomes from this randomized clinical trial were not realized, interesting findings descriptive of dosage effects, effect sizes, and covariates make a valuable contribution to the field. Without the 10 total sessions, seven sessions plus three boosters, the SFP 10–14 may be ineffective. On the other hand, considering that the booster sessions were not available and several other challenges to intervention fidelity occurred, that reasonably moderate effect sizes (d = 0.15 to 0.45) were attained among those who attended five of seven sessions suggests the SFP 10–14 to be a robust program to build family capacity.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research and/or authorship of this article: The work was supported by the Substance Abuse and Mental Health Services Administration (UD1 SPO-9460, Susan K. Riesch Project Director and Janie Canty-Mtichell Project Co-Director).
Footnotes
Declaration of Conflicting Interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
References
- Abroms L, Simons-Morton B, Haynie DL, Chen R. Psychosocial predictors of smoking trajectories during middle and high school. Addiction. 2005;100:852–861. doi: 10.1111/j.1360-0443.2005.01090.x. [DOI] [PubMed] [Google Scholar]
- Ackard M, Neumark-Sztainer D, Story M, Perry C. Parent–child connectedness and behavioral and emotional health among adolescents. American Journal of Preventive Medicine. 2006;30:59–66. doi: 10.1016/j.amepre.2005.09.013. [DOI] [PubMed] [Google Scholar]
- Aktan G, Kumpfer KL, Turner C. Effectiveness of a family skills training program for substance abuse prevention with inner city African American families. International Journal of the Addictions. 1996;31:158–175. doi: 10.3109/10826089609045805. [DOI] [PubMed] [Google Scholar]
- Alvy KT. Effective Black Parenting Program. Studio City, CA: Center for the Improvement of Child Caring; 1996. [Google Scholar]
- Anderson NLR, Koniak-Griffin D, Keenan CK, Uman G, Dugal BR, Casey C. Evaluating the outcomes of parent-child family life education. Scholarly Inquiry for Nursing Practice: An International Journal. 1999;13:211–238. [PubMed] [Google Scholar]
- Arthur MW, Hawkins D, Catalano RJ. Student survey of risk and protective factors. South Deerfield, MN: Channing & Bete; 1982. [Google Scholar]
- Barnes HL, Olson DH. Parent-adolescent communication and the Circumplex Model. Child Development. 1985;56:438–447. http://dx.doi.org/10.2307/1129732. [Google Scholar]
- Behnke AO, MacDermid SM, Coltrane SL, Parke RD, Duffy S, Widaman KF. Family cohesion in the lives of Mexican American and European American parents. Journal of Marriage and Family. 2008;70:1054–1059. [Google Scholar]
- Blum RW, Beuhring T, Shew ML, Bearinger LH, Sieving RE, Resnick MD. The effects of race/ethnicity, income, and family structure on adolescent risk behaviors. American Journal of Public Health. 2000;90:1879–1884. doi: 10.2105/ajph.90.12.1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobula JA, Anderson LS, Riesch SK, Canty-Mitchell J, Duncan A, Krueger HA, Angresano N. Enhancing survey data collection among children and parents: Use of handheld and laptop computers. CIN: Computers, Informatics and Nursing. 2004;22:255–265. doi: 10.1097/00024665-200409000-00004. [DOI] [PubMed] [Google Scholar]
- Bullock BM, Dishion TJ. Family processes and adolescent problem behavior: Integrating relationship narratives into understanding development and change. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:396–407. doi: 10.1097/chi.0b013e31802d0b27. [DOI] [PubMed] [Google Scholar]
- Bush P, Iannotti R. Alcohol, cigarette, and marijuana use among fourth grade school children in 1988/89 and 1990/91. American Journal of Public Health. 1993;83:111–114. doi: 10.2105/ajph.83.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan ISF, Zhang Z. Test based exact confidence intervals for the difference of two binomial proportions. Biometrics. 1999;55:1201–1209. doi: 10.1111/j.0006-341x.1999.01202.x. [DOI] [PubMed] [Google Scholar]
- Cleveland MJ, Feinberg ME, Bontempo DE, Greenberg MT. The role of risk and protective factors in substance use across adolescence. Journal of Adolescent Health. 2008;43:157–164. doi: 10.1016/j.jadohealth.2008.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analyses for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- DeVore ER, Ginsburg KR. The protective effects of good parenting on adolescents. Pediatrics. 2005;17:460–465. doi: 10.1097/01.mop.0000170514.27649.c9. [DOI] [PubMed] [Google Scholar]
- DiNapoli PP. Early initiation of tobacco use in adolescent girls: Key socio-structural influences. Applied Nursing Research. 2009;22:126–132. doi: 10.1016/j.apnr.2007.07.001. [DOI] [PubMed] [Google Scholar]
- Dixon WJ, Brown MB, Engelman L, Frane JW, Hill MA, Jennrich RI, Toporek JD. BMDP statistical software. Berkeley: University of California Press; 2009. [Google Scholar]
- Donovan JE. Really underage drinkers: The epidemiology of children’s alcohol use in the United States. Prevention Science. 2007;8:192–205. doi: 10.1007/s11121-007-0072-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowdell EB. Alcohol use, smoking, and feeling unsafe: Health risk behaviors of two urban seventh grade classes. Issues in Comprehensive Pediatric Nursing. 2006;29:157–171. doi: 10.1080/01460860600846925. [DOI] [PubMed] [Google Scholar]
- Faggiano F, Vigna-Taglianti F, Versino E, Zamborn A, Borraccino A, Lemma P. School-based prevention for illicit drugs’ use. Cochrane Database of Systematic Reviews. 2005;2 doi: 10.1002/14651858.CD003020.pub2. CD003020. [DOI] [PubMed] [Google Scholar]
- Fang L, Schinke SP, Cole KC. Underage drinking among young adolescent girls: The role of family processes. Psychology of Addictive Behaviors. 2009;23:708–714. doi: 10.1037/a0016681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finke LM, Chorpenning J, French B, Leese C, Siegel M. Drug and alcohol use of children in a rural community. Journal of School Nursing. 1996;12:22–25. doi: 10.1177/105984059601200203. [DOI] [PubMed] [Google Scholar]
- Fischer LB, Miles IW, Austin SB, Camargo CA, Jr, Corditz GA. Predictors of initiation of alcohol use among US adolescents: Findings from a prospective cohort study. Archives of Pediatrics and Adolescent Medicine. 2007;161:959–966. doi: 10.1001/archpedi.161.10.959. [DOI] [PubMed] [Google Scholar]
- Forgatch MS, Patterson GR. Parent Management Training–Oregon Model: An intervention for antisocial behavior in children and adolescents. In: Weisz J, Kazdin AE, editors. Evidence based psychotherapies for children and adolescents. 2nd ed. New York, NY: Guilford; 2010. pp. 157–178. [Google Scholar]
- Foxcroft D, Ireland D, Lowe G, Breen R. Primary prevention for alcohol misuse in young people. Cochrane Database of Systematic Reviews. 2002;3 doi: 10.1002/14651858.CD003024. CD003024. [DOI] [PubMed] [Google Scholar]
- Glasser P, Glasser L. Adequate family functioning. Psychiatric Research Report. 1966;20:8–17. [PubMed] [Google Scholar]
- Golan M. Parents as agents of change in childhood obesity—From research to practice. International Journal of Childhood Obesity. 2006;1:66–76. doi: 10.1080/17477160600644272. [DOI] [PubMed] [Google Scholar]
- Goldstein H. Multilevel statistical models. London, UK: Arnold; 1995. [Google Scholar]
- Gorman-Smith D, Tolan PH, Zelli A, Huesmann LR. The relation of family functioning to violence among inner-city minority youths. Journal of Family Psychology. 1996;10:115–129. [Google Scholar]
- Gottfredson D, Kumpfer K, Polizzi-Fox D, Wilson D, Puryear V, Beatty P, Vilmenay M. The Strengthening Washington D.C. Families project: A randomized effectiveness trial of family-based prevention. Prevention Science. 2006;7:57–74. doi: 10.1007/s11121-005-0017-y. [DOI] [PubMed] [Google Scholar]
- Harekeh Z, Scholte R, de Vries H, Engels C. Parental rules and communication: Their association with adolescent smoking. Society for the Study of Addiction. 2005;100:862–870. doi: 10.1111/j.1360-0443.2005.01067.x. [DOI] [PubMed] [Google Scholar]
- Harrell JS, Bangdiwala SI, Deng S, Webb JP, Bradley C. Smoking initiation in youth. Journal of Adolescent Health. 1998;23:271–279. doi: 10.1016/s1054-139x(98)00078-0. [DOI] [PubMed] [Google Scholar]
- Jackson C, Dickinson D. Enabling parents who smoke to prevent their children from initiating smoking: Results from a 3-year intervention evaluation. Archives of Pediatric and Adolescent Medicine. 2006;160:56–62. doi: 10.1001/archpedi.160.1.56. [DOI] [PubMed] [Google Scholar]
- Jessor R, Van Den Bos J, Vanderryn J, Costa FM, Turbin M. Protective factors in adolescent problem behavior: Moderator effects and developmental change. Developmental Psychology. 1995;31:923–933. [Google Scholar]
- Kumpfer KL, Alvarado R, Tait C, Turner C. Effectiveness of schoolbased family and children’s skills training for substance abuse prevention among 6–8 year old rural children. Psychology of Addictive Behaviors. 2002;16:S65–S71. doi: 10.1037/0893-164x.16.4s.s65. [DOI] [PubMed] [Google Scholar]
- Kumpfer KL, DeMarsh JP. Prevention of chemical dependency in children of alcohol and drug abusers. NIDA Notes. 1985;5:2–3. [Google Scholar]
- Kumpfer KL, DeMarsh JP, Child W. Strengthening families program: Children’s skills training curriculum manual, parenting training manual, children’s skill training manual, and family skills training manual (Prevention services to children of substance-abusing parents) Salt Lake City: University of Utah, Social Research Institute, Graduate School of Social Work; 1989. [Google Scholar]
- Kumpfer KL, Molgaard V, Spoth R. The strengthening families program for the prevention of delinquency and drug use. In: Peters RD, McMahon RJ, editors. Preventing childhood disorders, substance abuse, and delinquency. Thousand Oaks, CA: Sage; 1996. pp. 241–267. [Google Scholar]
- Kumpfer KL, Trunnell EP, Whiteside AO. The Bio-psychosocial Model: Application to the additions field. In: Engs RC, editor. Controversy in the addiction field. Dubuque, IA: Kendall/Hunt; 1990. pp. 55–66. [Google Scholar]
- Lederman RP, Chan W, Roberts-Gray C. Parent-Adolescent Relationship Education (PARE): Program delivery to reduce risks for adolescent pregnancy and STDs. Behavior Medicine. 2008;33:37–143. doi: 10.3200/BMED.33.4.137-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leidy MS, Guerra NG, Toro RI. Positive parenting, family cohesion, and child social competence among immigrant Latino families. Journal of Family Psychology. 2010;24:252–260. doi: 10.1037/a0019407. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. New York, NY: John Wiley; 1987. [Google Scholar]
- Long K, Boik R. Predicting alcohol use in rural children: A longitudinal study. Nursing Research. 1993;42:79–86. [PubMed] [Google Scholar]
- Loveland-Cherry CJ, Ross LT, Kaufman SR. Effects of a home-based family intervention on adolescent alcohol use and misuse. Journal of Studies on Alcohol, Supplement. 1999;13:94–102. doi: 10.15288/jsas.1999.s13.94. [DOI] [PubMed] [Google Scholar]
- Lydersen S, Pradham V, Senchaudhuri P, Laake P. Comparison of the exact tests for association unordered contingency tables using standard, mid-p, and randomized test versions. Journal of Statistical Computation and Simulation. 2005;75:447–458. [Google Scholar]
- Marsiglia F, Kulis S, Parsai M, Villar P, Garcia C. Cohesion and conflict: Family influences on adolescent alcohol use in immigrant Latino families. Journal of Ethnicity in Substance Abuse. 2009;8:400–412. doi: 10.1080/15332640903327526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrongiello BA, Lasenby-Lessard J. Psychological determinants of risk taking by children: An integrative model and implications for interventions. Injury Prevention. 2007;13:20–25. doi: 10.1136/ip.2005.011296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson DH. Commentary: Curvilinearity survives: The world is not flat. Family Process. 1994;33:471–478. doi: 10.1111/j.1545-5300.1994.00471.x. [DOI] [PubMed] [Google Scholar]
- Olson DH, McCubbin HI, Barnes H, Larsen A, Muxen M, Wilson M. Families: What makes them work? Beverly Hills, CA: Sage; 1983. [Google Scholar]
- Rasbash J, Charlton C, Browne WJ, Healy M, Cameron B. MLwiN (Version 2.1) [Computer software] Bristol, UK: University of Bristol, Centre for Multilevel Modeling; 2009. [Google Scholar]
- Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, Jones J, Udry R. Protecting adolescents from harm. Journal of the American Medical Association. 1997;278:823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- Rew L, Horner SD, Riesch L, Cauvin R. Computer-assisted survey interviewing of school-age children. Advances in Nursing Science. 2004;27:129–137. doi: 10.1097/00012272-200404000-00006. [DOI] [PubMed] [Google Scholar]
- Riesch SK, Anderson LS, Angresano N, Canty-Mitchell J, Johnson DL, Krainuwat K. Evaluating content validity and test-retest reliability of the children’s health risk behavior scale. Public Health Nursing. 2006;23:366–372. doi: 10.1111/j.1525-1446.2006.00574.x. [DOI] [PubMed] [Google Scholar]
- Riesch SK, Forsyth DM. Preparing to parent the adolescent: A theoretical overview. Journal of Child and Adolescent Psychiatric and Mental Health. 1992;5:32–40. doi: 10.1111/j.1744-6171.1992.tb00110.x. [DOI] [PubMed] [Google Scholar]
- Riesch SK, Jackson NM, Chanchong W. Communication approaches to parent-child conflict: Young adolescence to young adult. Journal of Pediatric Nursing. 2003;18:244–256. doi: 10.1016/s0882-5963(03)00083-6. [DOI] [PubMed] [Google Scholar]
- Riesch SK, Tosi CB, Thurston CA, Forsyth DM, Kuenning TMS, Kestly J. Effects of communication training on parents and young adolescents. Nursing Research. 1993;42:10–16. [PubMed] [Google Scholar]
- Roberts JK, Henson RK. Not all effects are created equal: A rejoinder to Sawilowsky. Journal of Modern Applied Statistical Methods. 2003;2:226–230. [Google Scholar]
- Robin AL. Problem-solving communication training: A behavioral approach to the treatment of parent-adolescent conflict. American Journal of Family Therapy. 1979;7:69–83. [Google Scholar]
- Rodgers JL, Billy JOG, Udry R. The recession of behaviors: Inconsistent responses in adolescent sexuality data. Social Science Research. 1982;11:280–296. [Google Scholar]
- Rudolph KD, Lambert SF, Clark AG, Kurlakowsky KD. Negotiating the transition to middle school: The role of self-regulatory processes. Child Development. 2001;72:929–946. doi: 10.1111/1467-8624.00325. [DOI] [PubMed] [Google Scholar]
- Small SA, Luster T. Adolescent sexual activity: An ecological, risk factor approach. Journal of Marriage and the Family. 1994;56:181–192. [Google Scholar]
- Spoth RL, Clair S, Shin C, Redmond C. Long-term effects of universal preventive interventions on methamphetamine use among adolescents. Archives of Pediatric and Adolescent Medicine. 2006;160:876–882. doi: 10.1001/archpedi.160.9.876. [DOI] [PubMed] [Google Scholar]
- Spoth RL, Shin C, Guyll M, Redmond C, Azevedo K. Universality of effects: An examination of long-term family intervention effects on substance use across risk-related subgroups. Prevention Science. 2006;7:209–224. doi: 10.1007/s11121-006-0036-3. [DOI] [PubMed] [Google Scholar]
- Watkins JA, Howard-Barr EM, Moore MJ, Werch CC. The mediating role of adolescent self-efficacy in the relationship between parent practices and adolescent substance use. Journal of Adolescent Health. 2006;38:448–450. doi: 10.1016/j.jadohealth.2005.04.002. [DOI] [PubMed] [Google Scholar]
- Yang M, Heath A, Goldstein H. Multilevel models for repeated binary outcomes: Attitudes and vote over the electoral cycle. Journal of Royal Statistical Society A. 2000;163:49–62. [Google Scholar]