Abstract
Background:
Globally, suicide is the third leading cause of mortality among persons aged 15-44 years. However in Jamaica it is not among the leading cause of mortality; but its importance cannot be ignored because of this fact.
Aims:
This study seeks to 1) update the prevalence of suicide in Jamaica, 2) make comparisons with international data, 3) provide an understanding of age-sex composition of those who are committing suicides, and 4) provide public health practitioners with valuable information which will be used to inform policy decisions.
Materials and Methods:
Secondary data published by the Jamaica Constabulary Force was used for this study. Data were summarized using percentages and associations were examined by Kruskal-Wallis or Analysis of Variance.
Results:
The suicide rate averaged 2.26 per 100,000 over the last six years. In 2006, the suicide rate for males was 9 times higher than that of females. The group of 65-74 age, among the male population, recorded the highest suicide rate (11.3 per 100,000) and the 5-14 age group recorded the lowest (0.3 per 100,000). The highest rate for the female population (3.4 per 100,000) was recorded in the 65-74 age group. The 30-39 age group showed an overall higher rate of suicide over the study period, this was followed by the 40-49 age group.
Conclusions:
Jamaica's suicide rate is among the lowest in the world and in spite of this, there is a need to formulate a suicide policy for the nation in particular males and young adults.
Keywords: Self-injurious behaviour, suicide, suicide rate, cultural programmes, prevention programme, public health, Jamaica
Introduction
Jamaica is a developing country in the Caribbean with a population of 2,682,120 – 1,132,646 males and 1,360,474 females (estimated for 2007). It has a total land area of 10,991 km2, 14 parishes and those parishes are classified into 3 geographical planes (Cornwall, Middlesex and Surrey) (Figs. 1A, 1B). The Western side of the island is Cornwall, and this covers parishes such as Westmoreland, Hanover, St. James and St. Elizabeth. Middlesex on the other hand covers the middle section, with parishes such as Clarendon, Manchester, and St. Catherine. Surrey covers the Eastern regions with parishes such as Kingston, St. Thomas and Portland. Another classification is cities (urban areas) which constitute 27.3% of the population, peri-urban 30.2% and rural areas, 42.5% in 2007.
Fig. 1A.

Map of Jamaica by parish classification
Fig. 1B.
Map of Jamaica by 3 main classification: Cornwall, Middlesex and Surrey
Statistics from the Planning Institute of Jamaica and the Statistical Institute of Jamaica[1], for 2007, revealed that 30.7% were children (ages 0 to 14 years), 60.1% working age people (15 to 64 years) and 9.2% ages 65+ years. Furthermore, the mean consumption for male was $JA.176, 071 ($US1.00 = $JA.80.47) compared to $JA.152, 324 for females. Ten percent of the population was in poverty (6.2% urban; 4% semi-urban; 15.3% rural); 15.5% reported at least one health condition (17.8% females and 13.1% of males; 8.7% asthma; 12% diabetes mellitus; 22.4% hypertension and 8.8% arthritis. Another important statistical finding was that 66% of those who reported that they were ill sought medical care, with 33.9% stating that they were unable to afford and utilize medical care.
The number of people not seeking medical care includes some who are suffering from psychiatric disorders. A recently conducted study by Bourne and Beckford[2] revealed that there was a negative correlation between self-reported illness and medical care-seeking behaviour as well as seeking medical care and unemployment; a positive association between self-reported illness and unemployment and within the context that self-reported illness, for 2007, rose by 27% (to 15.5%) over the previous year. With inflation having increased by 194% over the same period, this would have some negative influence on health status of people. Another interesting issue that lies beneath the numbers is the psychological issue of how to live with this reality. The challenge of inflation not only includes the upward movement in prices, but the psychological component of survivability. Embedded in the increased self-reported illnesses of Jamaicans over the same time when inflation exponentially increased are some people who are suffering from psychiatric disorders, and who would be unable to afford it.
Suicide therefore becomes an escape route for many people who are unable to address the challenges of cost of living, social exclusion, problems in social relationships, financial burdens; challenges of illnesses, socio-cultural stressors and psychological challenges. In an earlier study, Hickling[3] opined that for some native Caribbean nationals, the Caribbean is a region that people should emigrate from as it is a milieu of poverty. This speaks to the psychological challenge of living in the Caribbean in particular Jamaica, and offers some socio-cultural explanation for psychiatric disorders.[4] Pottinger and colleagues[4] found that poor relationships in children and adolescents (ages 6 to 18 years) with their primary caregiver were significantly correlated with suicidal behaviour as well as experiencing abuse. Hicking's work[3] on Jamaicans revealed that 2.09 per 10,000 Jamaicans had schizophrenia, 2.2 per 1000 in Trinidad and 2.92 per 1000 in Barbados.
The aims of this study are to 1) update the prevalence of the suicide rate in Jamaica (2002-2006), 2) make comparisons with international data, 3) provide an understanding of age-sex composition of those who are committing suicides, and 4) provide public health practitioners with valuable information which can be used to formulate more policy decisions
Materials and Methods
Ethical approval was granted by the Institutional Review Board.
Jamaica is divided into nineteen police geographical divisions. Each division reports suicides within the region on a monthly basis to the Statistics Department of the Jamaica Constabulary Force. The database for suicide and other crimes are maintained within this department. In 1998, The Jamaica Constabulary Force established a formal and reliable system for recording suicides in Jamaica. Suicide cases are determined by police investigation and results of the post mortem examination. The number of completed suicides reported to the police between 2002 and 2006 were extracted from The Statistics Department of the Jamaica Constabulary Force by a trained researcher with written consent. These figures are the official statistics for the country, and are used by the government, the Statistical institute of Jamaica, the Planning Institute of Jamaica and all other agencies.
The suicide rate by gender, overall suicide rate and suicide rate by age groups were determined. The denominator used for population was based on the official population data reported by the Statistical Institute of Jamaica over the period under study. Test of associations were Kruskal-Wallis and Analysis of Variance (ANOVA) at the 95% confidence interval (i.e. 5% level of significance).
Results
Figure 2 showed the total suicide rate and the suicide rate by gender from 2002 to 2006. The total suicide rate followed a wavelike pattern over the period. The maximum 2.7 per 100,000 was recorded in 2003 and the minimum of 2.0 per 100,000 in 2006.
Fig. 2.
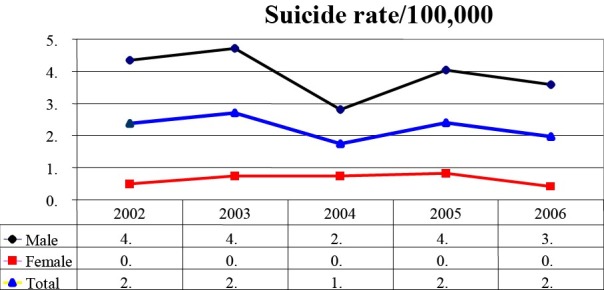
Suicide rate by sex and population, 2002-2006
The suicide rate by gender showed similar trends. The suicide rate for males was higher than that of females over the period under study. Among males, the suicide rate ranged between 2.8 and 4.7 with the highest reported in 2003 and the lowest in 2004. Among females, the highest suicide rate recorded in 2006 was 0.4 and in 2005, the highest rate was 0.8. Although, in 2006, total suicide rate was 2.0 per 100,000, the disparity between the numbers of cases committed by males to females was at its highest over the 5-year period (i.e. 9 times more males committed suicide compared to females). In 2002, 8.6 times more males committed suicide compared to females and the figure fell to 6.7 times in 2003 and 4.0 times the following year and increased to 5.0 times in 2005.
The group of 65-74 age among the male population recorded the highest suicide rate (11.3 per 100,000) and the 5-14 age group recorded the lowest (0.3 per 100,000). The highest rate for the female population (3.4 per 100,000) was recorded in the 65-74 age group. Analysis of Variance yielded a P < 0.025 level of significance indicating that there is a difference in the mean results between the groups. The Kruskal-Wallis also indicated a significant difference between the mean results from the group but at a higher level (P < 0.001).
There is no statistical difference in age-sex suicide rates across the years in the study period. The 30-39 age group showed an overall higher rate of suicide over the study period, this was followed by the 40-49 age groups. This was highly significant using Analysis of Variance, P = 0.025. The Kruskal-Wallis test was significant, P < 0.001. About 62.3% persons in the 5-44 years age group completed suicide and 37.7% of persons in the 45 and older age group completed suicide. Table 1
Table 1.
Suicide rate by age, sex and population, 2002-2006

Discussion
The suicide rates were determined between 2002 and 2006, a period when data collection by the police was relatively reliable. The suicide rate in Jamaica showed a wavelike pattern ranging between 1.8 in 2000 and 2.7 in 2003 per 100,000. Similar patterns were also recorded for the suicide rates by gender. This finding contrasts with the steady increase in suicide rates reported by WHO globally since 1950. The WHO opined that, for 2000, suicide rates for the world was 16 per 100,000 - one death every 40 seconds - in 1998 it was estimated that globally, suicide represents 1.8% of the total burden of disease[5], and that this is among the leading cause of mortality of people age 15-44 years. These results indicate that Jamaica falls among countries with the lowest suicide rates. The WHO reports that countries with suicide rates lower than Jamaica's were those such as Honduras which had no proper recording machinery in place; Guatemala and Jordan which had no current data and Dominican Republic, St. Kitts and Nevis which were labelled as islands paradise.
Suicide is an indicator of a psychiatric disorder, and so it is vital in providing information on a populace life coping mechanism (or the lack thereof). Hovanesian and colleagues[6] argued that coping approaches and defence mechanisms are linked to suicide, attempted suicide, and that past attempted suicidal behaviour is a good indicator of future suicide cases. Embedded in those arguments are issues of depression, which predate suicide. Lowe and Gibson[7], using data on adolescences, found that socio-cultural events such as under-achievement; poor lifestyle choice, and continued illness in adulthood are significantly correlated with depression, and that there is an increased probability of suicide when those events are occurring in the individual's life. Suicide; is it a silent killer?
Suicide accounts for 1.4% of the global disease burden indicating its public health relevance[8–10]. Suicide was the eleventh leading cause of mortality in 2004 in the United States of America and the third leading cause of death among persons 15–44 globally[8,9,11,12]. The World Health Organization (WHO) estimates that by 2020, approximately 1.53 million persons will die from suicide; recent trends indicate that there is an increase in suicide rates among young people[9].
Countries in Eastern Europe are among those reporting the highest suicide rates –Lithuania, 42 per 100,000; Russia, 38 per 100,000; Belarus, 35 per 100,000 and Ukraine, 26 per 100,000. Several European countries fall within the medium range – Belgium, 21 per 100,000; Finland, 20 per 100,000; Switzerland, 18 per 100,000 and Austria, 18 per 100,000 and Japan, 23.8 per 100,000[8,9,13].
In Latin America, several countries report suicide rates within the lower range, for example, Costa Rica has a rate of 6.9 per 100,000. A number of Muslim countries also record low suicide rates, for example, Kuwait's rate is 0.1 per 100,000[8].
Data from the Caribbean reveals that Trinidad and Tobago demonstrates the highest suicide rate of 12.8 per 100,000 in that country[8]; a previous study by Nehall[13] reported a suicide rate of 13.6 per 100,000 in Trinidad. The suicide rates for St. Vincent and Puerto Rico are 7.7 and 6.2 per 100,000 respectively.[9,14] Mahy[15] reported an age- corrected prevalence rate of 6.5 per 100,000 and 12 per 100,000 in the Bahamas.
In Jamaica, in a study based on a retrospective review of death certificates and a review of post-mortem records of sudden deaths in hospitals, Burke[14] reported the age-corrected incidence suicide rate of 1.4 per 100,000 (15+) over the period 1975-1976. No suicide case was reported in the less than 15 age group. Irons -Morgan[16] reported a prevalence rate of 2.85 per 100,000 in a psychopathological autopsy done in Jamaica.
The determination of suicide rates is associated with many methodological challenges. Firstly, under reporting is common, as suicide is associated with high levels of silence, stigma and shame worldwide[17]. Secondly, there is marked variation in the methodology for data collection. In many countries, data are collected by the police who often do not have a well-developed data collection system and, in other jurisdictions; suicide data are based on information sourced from death certificates and are often misreported and erroneous. Prior to 1996, the only report on incidence of suicide in Jamaica was the study by Burke[14]; official suicide reports by the government were based on police statistics which were not reliable or standardised. Hitherto, it was difficult to determine accurate suicide rates and to conduct reliable trend analysis. In spite of Burke's findings, there is no other institution or methodology that can be used to modify the official police statistics on suicide; however they were used despite of this limitation.
Depression and substance abuse are related with more than 90% of all cases of suicide, and the reality that this is associated with sociocultural and socioeconomic conditions, explains the disproportionate rate of suicides being committed by males. Males have a greater propensity to smoke, abuse drugs and thereby account for more cases of suicide than females. The suicide rates for men were higher than those for women in Jamaica with a male: female ratio ranging from 4:1 to 9:1. The higher suicide rate in men is consistent with global suicide patterns[5], the only exception being reports from rural China in which suicide rates for females were higher than that of males.
Suicide, therefore, is a male phenomenon, which is also the case in Jamaica. According to WHO, suicide is rampant in Asia, which globally accounted for 60% of all the cases, with China and Japan accounting for 40% of the cases[5]. This should come as no surprise as those two nations accounted for more than two-thirds of the world's population.
Suicidal behaviour[18] of males therefore is embedded in the cultural background of suppressing weakness, avoidance of exhibiting pain, low medical care-seeking behaviour and speaking about pain, disappointment, challenges and other sociocultural happenings are woman like. Chevannes[19] in seeking to explain the cultural dynamics of men's behaviour showed that boys are culturalized not to display weakness, cry, show emotions, suppress their feelings, and this justifies the reason for them seeking medical care based on severity. This is atypical to Jamaica as Ali and de Muynck[20] found that the males would seek medical care based on severity of illnesses and financial situation. Another finding was that they referred to the use of home remedies. The reason being that mild ailment is not severe enough to barr them from physical functioning, which mean that they are okay; and so some morbidity are not for-hospital, which was so in the case of the Nairobi slums[21]. Therefore, like the cases in Pakistan and Nairobi, the Jamaican men are equally not reporting illness and seeking health-care substantially because of their socialization. This is inextricably linked to the macho culture with which they are grown; as substantiated by Chevannes who posited that they should suppress response to pain. The point of view is similarly delineated in the works of Ali and Muynck and Taff and Chepngeno. With men having a deep culturalized tendency to store and internalize pain, weakness, disappointment, frustration and other negative psychological conditions. . The greater proportionality of them committing suicides can be rationalized.
Jamaica's suicide rate by age and gender has fluctuated with no specific pattern. Statistical analysis revealed that there are no significant differences between the years of the study (2002-2006) and at present, no explanation is available to explain the trend. While there was no observed trend in the suicide rate by age and gender during the study period, the year 2003 was noted to have the highest suicide rate by gender and age. In Jamaica, 62.3 % of suicides were committed by those between 5 and 44 years old and 37.7 % in the 45 and older age group. This is consistent with the global age Department of the Jamaica Constabulary Force distribution of age-sex suicide rates. The WHO data reveal that in 2000, 44% of suicides were committed by those 5-44 years old and 56% by those 45 years and older. This study concurs with another which showed that there is a significant statistical difference between age, sex and suicide cases[13,18,22,23].
The suicide rates provided us with some insights into the psychological state of those who commit the act or attempt this act. Suicide is a psychiatric disorder, suggesting that attempted or successfully executed cases offer an explanation into the negative psychological state of these people. Suicide victims therefore would not have been enjoying life or would not be experiencing any moderate-to-high degree of happiness at the time of the happening. Studies have revealed that there was a direct significant statistical correlation between positive moods and/or emotions and subjective wellbeing[24]. This suggests those who are experiencing negative affective psychological disorders (or conditions) will have a lowered health status. Hence, depression, anxiety, neuroticism and pessimism are seen as measures of the negative psychological conditions that affect subjective wellbeing.[25–27] From Evans and colleague[25], Harris et al.[26] and Kashdon's monographs[27], negative psychological conditions affect subjective wellbeing in an indirect manner (i.e. guilt, fear, anger, disgust); suggesting that suicide victims were experiencing lowered psychological wellbeing and by extension health status than non-suicide victims.
Jamaica is one of the countries that does not have a suicide policy. Many public health issues that are on the forefront of discussion and policy formulations are owing to 1) the requirements of international institutions such as World Health Organization (WHO), Pan American Health Organization (PAHO) and International Conventions, 2) outbreak of diseases, 3) disaster and disaster management, 4) moderate-to-high incidence or prevalence. With the suicide rate being as low as they are in Jamaica there is nothing alarming about the aggregate figures which may explain the reluctance in the formulation of a suicide policy. In spite of this reality, one of the critical measures that can be implemented in the reduction of suicide among Jamaicans in particular males is early detection of depression.
In summary, with suicide rates between 1.8 and 2.7, Jamaica's suicide rates are among the lowest in the world. However, suicide is a preventable public health problem. The WHO has made a call for a coordinated and intensified global action to address this global problem. Greater efforts must be directed towards strengthening the data collection system on suicide worldwide in order to ensure that consistent and reliable data are available to facilitate policy, planning and programme development.
Despite the low suicide rates in Jamaica, disproportionately more men are committing the act each year (in 2006, 9 times more males than females) and this must be addressed. Interestingly the suicide rate in 2006 was the last in the 5 year review period (2002-2006) and the disparity between the rate for male and female was the widest, with 2004 representing the least disparity (4 times more males than females). With predominately less males than females seeking medical care and more so for psychiatric disorders because of the cultural undertones, suicide is a silent killer for males who are undergoing severe negative psychological trauma. The only age group in which suicide was higher for females than males was 5-14 years (in 2002, 2004 and 2005), indicating the psychological challenges faced by males in Jamaica and how their silence is helping to explain those internal conflicts.
Acton and Zodda[28] summarized challenges of silence when they wrote that “expressed emotion is detrimental to the patient's recovery; it has a high correlation with relapse to many psychiatric disorders” Hence, a sustained effort must be directed towards devising and implementing culturally appropriate programmes to facilitate the early detection of substance abuse, mental disorders and a health literacy programme geared towards health and sex-disparity. Finally, the development of empirically based prevention and treatment programmes is critical to achieving a sustainable reduction in suicide.
Acknowledgement
The authors would like to extend their deep appreciation to Ms. Neva South-Bourne for sourcing aspects of the literature and making herself available for critique of the final manuscript.
References
- 1.Jamaica Survey of Living conditions, 2007. Kingston: 2008. Planning Institute of Jamaica, Statistical Institute of Jamaica. [Google Scholar]
- 2.Bourne PA, Beckford OW. Paper presented at the 34th annual conference, Caribbean Studies Association Conference June 1-5. Hilton Kingston, Jamaica: 2009. Unemployment, Illness and Health Seeking Behaviour in Jamaica. [Google Scholar]
- 3.Hickling FW. The epidemiology of schizophrenia and other common mental health disorders in the English-speaking Caribbean. Rev Panam Salud Publica. 2005;18(4-5):256–262. doi: 10.1590/s1020-49892005000900005. [DOI] [PubMed] [Google Scholar]
- 4.Pottinger AM, Milbourn PE, Leiba J. Suicidal behaviour and risk factors in children and adolescents in Jamaica. West Indian Med J. 2003;52(2):127–30. [PubMed] [Google Scholar]
- 5.Suicide Prevention. Washington DC: World Health Organization; 2009. WHO. [Google Scholar]
- 6.Hovanesian S, Isakov I, Cervellione KL. Defense mechanisms and suicide risk in major depression. Arch Suicide Res. 2009;13(1):74–86. doi: 10.1080/13811110802572171. [DOI] [PubMed] [Google Scholar]
- 7.Lowe GA, Gibson RC. Depression in adolescence: new developments. West Indian Med J. 2005;54(6):387–91. doi: 10.1590/s0043-31442005000600009. [DOI] [PubMed] [Google Scholar]
- 8.Figures and Facts about Suicide. Geneva: WHO; 1999. World Health Organization, (WHO) [Google Scholar]
- 9.Abel WD, Martin JS. Suicide: a preventable public health problem. West Indian Med J. 2008;57(2):387–91. [PubMed] [Google Scholar]
- 10.Murray CJL, Lopez AD. The Global Burden of Diseases. Vol. 1. Boston: Harvard School of Public Health; 2004. [Google Scholar]
- 11.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS) [Google Scholar]
- 12.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J of Methods in Psychiatric Research. 2006;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nehall J. An analysis of psychiatric inpatient admission for a defined geographic catchment area over a 1 year period. West Indian Med J. 1991;40:15–21. [PubMed] [Google Scholar]
- 14.Burke AW. Suicide in Jamaica. The West Indian Med. J. 1985;34(1):48–53. [PubMed] [Google Scholar]
- 15.Mahy G. Suicide in Jamaica. Int Rev Psychiatry. 1995;5(2/3):261–269. [Google Scholar]
- 16.Irons-Morgan M. Master in Public Health Thesis. Kingston: University of the West Indies (Mona); 1999. Suicide rate in Jamaica in 1998 and the prevalence of mental disorders and stressful life events in suicide victims in Kingston, St. Andrew and St. Catherine in 1998. [Google Scholar]
- 17.Burgess P, Pirkis J, Jolley D, Whiteford H, Saxena H. Do nations’ mental health policies, programs and legislation influence their suicide rates? An ecological study of 100 countries. Australian and New Zealand J of Psychiatry. 2004;38:933–939. doi: 10.1080/j.1440-1614.2004.01484.x. [DOI] [PubMed] [Google Scholar]
- 18.Nock MK, Borges G, Bromet E, Cha CB, Kessler RC, Lee S. Suicide and Suicidal behavior. Epidemiologic Review. 2008 doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chevannes B. Learning to be a man: Culture, socialization and gender identity in five Caribbean communities. Kingston, Jamaica: The University of the West Indies Press; 2001. [Google Scholar]
- 20.Ali M, de Muynck A. Illness incidence and health seeking behaviour among street children in Pawalpindi and Islamabad, Pakistan – qualitative study. Child: Care, Health and Development. 2005;31:525–32. doi: 10.1111/j.1365-2214.2005.00545.x. [DOI] [PubMed] [Google Scholar]
- 21.Taff N, Chepngeno G. Determinants of health care seeking for children illnesses in Nairobi slums. Tropical Medicine and International Health. 2005;10:240–45. doi: 10.1111/j.1365-3156.2004.01381.x. [DOI] [PubMed] [Google Scholar]
- 22.Rodriquea-Pulido F, Sierra A, Doreste J, Gracia R, Gonzalez-Rivera JL. Suicide in the Canary Islands: standardized epidemiological study by age, sex, and marital status. Soc Pyschiatry and Psychiatric Epidemiology. 1992;27(2):69–74. doi: 10.1007/BF00788508. [DOI] [PubMed] [Google Scholar]
- 23.Rezaeian M. Age and sex suicide rates in the Eastern Mediterranean Region based on global burden disease estimates for 2000. Eastern Mediterranean Health J. 2007;13(4) [PubMed] [Google Scholar]
- 24.Leung BW, Moneta GB, McBride-Chang C. Think positively and feel positively: Optimism and life satisfaction in late life. International Journal of Aging and human development. 2005;61:335–365. doi: 10.2190/FQTB-EBAJ-H9WP-LMYA. [DOI] [PubMed] [Google Scholar]
- 25.Evans CC, Sherer M, Nick TG, Nakase R, Yablon S. Early impaired self-awareness, depression, and subjective wellbeing following traumatic brain injury. J of Head Traua Rehabilitation. 2005;20:488–500. doi: 10.1097/00001199-200511000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Harris PR, Lightsey OR., Jr Constructive thinking as a mediator of the relationship between extraversion, neuroticism, and subjective wellbeing. European J of Personality. 2005;19:409–426. [Google Scholar]
- 27.Kashdan TB. The assessment of subjective wellbeing (issues raised by the Oxford Happiness Questionnaire) Personality and Individual Differences. 2004;36:1225–1232. [Google Scholar]
- 28.Acton GS, Zodda JJ. Classification of psychopathology: Goals and methods in an empirical approach. Theory of Psychology. 2005;15:373–399. [Google Scholar]


