Abstract
Context:
Jejunal diverticuli are rare and usually asymptomatic. More commonly, they are seen as incidental findings on CT images, enteroclysis, or during surgery. Complications such as bleeding, perforation, obstruction, malabsorption, diverticulitis, blind loop syndrome, volvulus, and intussusceptions may warrant surgical intervention.
Case report:
We report a case of 47-year old woman who had suffered from intestinal obstruction for 3 days. The symptoms did not improve after conservative treatment. An exploratory laparotomy found small bowel obstruction due to proximal jejunal diverticulum with an adhesion epiploic band. Strangulation of the jejunum resulted from the internal hernia caused by the band. The band was removed and the proximal jejunum segmentally resected. The postoperative course was uneventful.
Conclusion:
Although this phenomenon is rare, we should keep in mind that intestinal diverticulosis may induce intestinal obstructions of different kinds, repeat physical examinations and X-ray films are needed and enteroclysis studies or CT scan are helpful in diagnosis. Surgery is indicated for acute abdominal or repeated intestinal obstruction.
Keywords: Jejunal diverticula, gastrointestinal obstruction, jejunal resection
Introduction
The diverticulum of the small bowel may be congenital or acquired. The incidence varies from 0.2% to 1.3% in autopsy studies to 2.3% when assessed on enteroclysis[1]. The prevalence increases with age, peaking at the sixth and seventh decades[2]. 80% of diverticula occur in the jejunum, 15% in the ileum and 5% in both[3]. Small bowel motility disorders with increased intraluminal pressure are considered to be the main etiological factors for their development[1,2,4]. Although it is often asymptomatic, it can lead to severe complications including perforation, hemorrhage, enterolith formation, diverticulitis, and intestinal obstruction[5,6] and occur in 10%-30% of patients[7,8,9].
An adhesion band, arising from the base of the diverticulum, may be formed after repeated diverticulitis, and may cause strangulation of the intestine[1].
We report a case of a rare diverticulum of the jejunum with an epiploic adhesion band resulting in intestinal obstruction.
Case Report
A 47-year-old woman presented with a 3-day history of central colicky abdominal pain, abdominal distension and vomiting. She was treated with oral spasmolytic drugs without improvement. Medical history revealed no history of digestive bleeding. The patient underwent no surgical procedure in the past. Examination of her abdomen revealed tenderness and distension of the abdomen and no palpable mass. A 1cm uncomplicated umbilical hernia was present. Digital rectal examination was normal. Laboratory tests indicated an elevated white blood count (23500/mm3), normal serum sodium and potassium levels. A plain X-ray abdominal film showed distended small bowel loops and multiple gas fluid levels (Fig. 1). Computed tomography of the abdomen revealed multiple distended small-bowel loops distributed radially. The thickened small bowel wall and the congestive appearance of mesenteric fat were suggestive of a strangulated obstruction (Fig. 2).
Fig. 1.

X-ray abdominal film showed distended small bowel loops and multiple gas fluid levels.
Fig. 2.
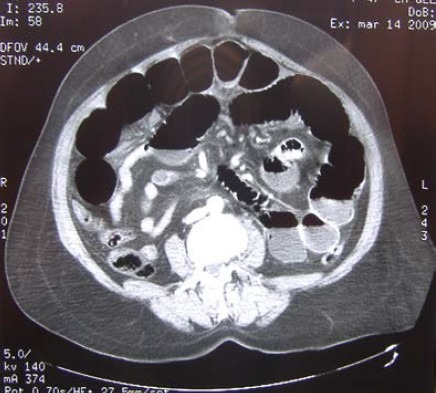
Computed tomography of the abdomen revealed multiple distended small-bowel loops distributed radially. The thickened small bowel wall and the congestive appearance of mesenteric fat were suggestive of a strangulated obstruction.
We decided that an emergent laparotomy was required after a brief and intensive resuscitation. Upon exploration, we found a moderate clear ascites and an epiploic adhesion band overriding the jejunum with ischemic changes in the proximal jejunum (Fig. 3). After surgical removal of the adhesion band we noted that it was connected to a 5cm long diverticulum arising from the mesentery side 20 cm distal to the ligament of Treitz (Fig. 4). A diverticulectomy without small bowel resection was performed because the swollen, purple intestines were well perfused after 20 min of observation and there was no suspect endoluminal tissue. An umbilical herniorraphy were also performed. Final pathology exam confirmed the jejunal diverticulum with no sign of malignancy. The patient had an uneventful post-operative course and was discharged 5 days after the procedure.
Fig. 3.
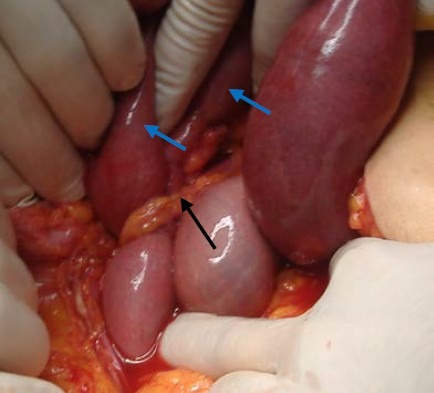
Adhesion band (black arrow) overriding the jejunum with ischemic changes in the proximal jejunum (blue arrow).
Fig. 4.

A 5cm long diverticulum arising from the mesentery side 20 cm distal to the ligament of Treitz.
Discussion
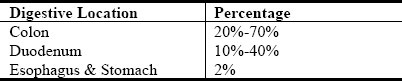
Jejunal diverticulum is a rare entity with an incidence rate ranging from 0.3% to1.3% in autopsy series and 2.3% in radiographic findings[3]. It was first described in 1794 by Sommering and later in 1807 by Sir Astley Cooper and is characterized by herniation of mucosa and submucosa through the muscular layer at the point where blood vessels penetrate the intestinal wall (false diverticula)[2,5]. This explains their typical location at the mesenteric side[2,3,10]. Diverticula are more frequent in jejunum (61%) than the other parts of the small bowel and it is attributed to the greater diameter of the penetrating jejunal artery[5]. Diverticuli are usually multiple[5,11], in contrast to the congenital Meckel's diverticulum and tend to be larger and higher in number in the proximal jejunum and smaller and fewer caudally[12]. Coexistent diverticuli are found in many other digestive localizations (Table 1)[7,14,15].
Table 1.
Percentage of coexistent diverticuli
The etiology is unclear; it is believed to develop as the result of abnormalities in peristalsis, intestinal dyskinesis, and high segmental intraluminal pressures[13]. The current hypothesis focuses on abnormalities in the smooth muscles or myenteric plexus[1,14]. Careful microscopic evaluation of jejunal specimens with diverticula has shown that these abnormalities are of three types[16]:
-
-
Fibrosis and decreased numbers of normal muscle cells, consistent with progressive systemic sclerosis;
-
-
Fibrosis and degenerated smooth muscle cells, suggestive of a visceral myopathy;
-
-
Neuronal and axonal degeneration indicative of visceral neuropathy.
Any of these abnormalities could lead to distorted smooth muscle contractions of the affected small bowel generating increased intraluminal pressure. Consequently, mucosa and submucosa would pass through the weakest mesenteric site in the bowel wall with penetration induced by paired blood vessels from the mesentery[1,14].
Jejunoileal diverticuli are commonly observed in patients aged 60-70 years[11], with a slight male preponderance[5].
Jejunoileal diverticuli are usually asymptomatic and are found incidentally. Most patients have chronic abdominal pain and a bloated sensation. If symptomatic, vague and chronic abdominal pain of varying severity, localized epigastrically or periumbilically with a bloating sensation after food intake is frequent and may be the earliest symptom[2,10,14]. Complications requiring surgical intervention occur in 8%-30% of patients[16]. Common acute complications include diverticulitis, hemorrhage, perforation and intestinal obstruction. Mechanical intestinal obstruction occurs in 2.3-4.6% of cases and may arise from enterolith formation, intussusception or volvulus[1,6,10]. In the latter situation the diverticulum acts as a pivot, especially where previous diverticulitis results in adhesive band formation arising from the mesodiverticulum[1,2]. Such adhesions may also cause obstruction by direct kinking of the bowel or by trapping another loop of bowel underneath[2] as it occurred in our case.
The diagnostic work up in symptomatic patients can start with plain abdominal X-ray film that could show distension of jejunal loops and gas-fluid levels into the diverticulum when it is giant. Barium enema study probably reveals the diverticulum as a contrast-filled out pouching, 0.5 to 10 cm long, that is located on the mesenteric border of the jejunum and has a junction-fold pattern. The enteroclysis and enteroscopy are the best imaging[11], however, their utility in emergency situations like in the presented case is limited. Computed tomography is helpful in complicated diverticula. It is reasonable to conclude that asymptomatic diverticula incidentally discovered on routine contrast studies or at laparotomy do not need resection[2,4]. However, other authors have suggested that surgical treatment is indicated for the incidental large diverticula with dilated hypertrophied bowel loops that represent a progressive form of the disease[17].
Treatment of acute complications of jejunoilelal diverticulum is mostly operative and non-specific. A higher complication rate is associated with jejunoileal diverticulosis and, as such, may justify less conservative approach to its management. Diagnostic laparoscopy is very useful in evaluating patients with a complicated course. It ensures an accurate diagnosis and avoids the risk of unnecessary laparotomy if not indicated[14]. Conclusive diagnosis in our patient was made by diagnostic laparotomy, resulting in prompt and appropriate surgical treatment.
It seems that the risk of occurrence of possible complication is higher in patients with multiple jejunal diverticula than in patients with solitary diverticulum. However, the recommended treatment for jejunal diverticulosis, often performed emergently, is intestinal resection and end-to-end anastomosis even in case of perforation or peridiverticular stenosis, in order to avoid further complications[4,5]. A simple diverticulectomy by wedge excision is most commonly used for symptomatic diverticulum or bleeding diverticulum. The diverticulum is simply excised, and the bowel is closed longitudinally or transversely, ensuring minimal luminal stenosis. In case of obstruction due to an enterolith, some authors suggest conservative management by performing the manual breakage of all stones, intradiverticular and blocking ones, pushing their fragments to the colon. If this is proved to be impossible or inappropriate, the stone is removed through an enterotomy which is made in a less edematous segment of proximal small bowel[6,10]. The outcome of operated jejunoileal diverticula is generally good. Mortality is influenced by patients’ age, nature of complications, and timeliness of intervention.
Conclusion
This is a new case of strangulation of the jejunum caused by a mesodiverticular band. The band may have formed during recurrent diverticulitis, because it arose from the mesodiverticulum. Although this phenomenon is rare, we should keep in mind that intestinal diverticulosis may induce intestinal obstructions of different kinds, repeat physical examinations and X-ray films are needed and enteroclysis studies or CT scan are helpful in diagnosis. Surgery is indicated for acute abdominal or repeated intestinal obstruction.
References
- 1.Lin CH, Hsieh HF, Yu CY, Yu JC, Chan DC, Chen TW, Chen PJ, Liu YC. Diverticulosis of the jejunum with intestinal obstruction: A case report. World J Gastroenterol. 2005;11(34):5416–5417. doi: 10.3748/wjg.v11.i34.5416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang A, McWhinnie DL, Sadler GP. An unusual cause of bowel obstruction. Postgrad Med J. 2000;76:183–185. doi: 10.1136/pmj.76.893.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kassahun WT, Fangmann J, Harms J, Bartels M, Hauss J. Complicated small-bowel diverticulosis: A case report and review of the literature. World J Gastroenterol. 2007;13(15):2240–2242. doi: 10.3748/wjg.v13.i15.2240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sagar J, Kumar V, Shah DK. Meckel's diverticulum: a systematic review. J R Soc Med. 2006;99(10):501–505. doi: 10.1258/jrsm.99.10.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kouraklis G, Glinavou A, Mantas D, Kouskos E, Karatzas G. Clinical Implications of Small Bowel Diverticula. IMAJ. 2002;4:431–433. [PubMed] [Google Scholar]
- 6.Hayee B, Khan HN, Al-Mishlab T, McPartlin JF. A case of enterolith small bowel obstruction and jejunal diverticulosis. World J Gastroenterol. 2003;9:883–884. doi: 10.3748/wjg.v9.i4.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilcox RD, Shatney CH. Surgical implications of jejunal diverticula. South Med J. 1988;81:1386–1391. doi: 10.1097/00007611-198811000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Akhrass R, Yaffe MB, Fischer C, Ponsky J, Shuck JM. Small-bowel diverticulosis: perceptions and reality. J Am Coll Surg. 1997;184:383–388. [PubMed] [Google Scholar]
- 9.Sibille A, Willocx R. Jejunal diverticulitis. Am J Gastroenterol. 1992;87:655–658. [PubMed] [Google Scholar]
- 10.Balducci G, Dente M, Cosenza G, Mercantini P, Salvi PF. Multiple giant diverticula of the foregut causing upper gastrointestinal obstruction. World J Gastroenterol. 2008;14(20):3259–3261. doi: 10.3748/wjg.14.3259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maršík L, Ferko A, Jaroš E, Jon B, Hadzi Nikolov D. Jejunoileal diverticula as a rare cause of acute abdomen. Report of three cases. Folia Gastroenterol Hepatol. 2006;4(2):56–60. [Google Scholar]
- 12.de Bree E, Grammatikakis J, Christodoulakis M, Tsiftsis D. The clinical significance of acquired jejunoileal diverticula. Am J Gastroenterol. 1998;93:2523–2528. doi: 10.1111/j.1572-0241.1998.00605.x. [DOI] [PubMed] [Google Scholar]
- 13.Krishnamurthy S, Kelly MM, Rohrmann CA, Schuffler MD. Jejunal diverticulosis. A heterogenous disorder caused by a variety of abnormalities of smooth muscle or myenteric plexus. Gastroenterology. 1983;85:538–547. [PubMed] [Google Scholar]
- 14.Kassahun WT, Fangmann J, Harms J, Bartels M, Hauss J. Complicated small-bowel diverticulosis: a case report and review of the literature. World J Gastroenterol. 2007;13:2240–2242. doi: 10.3748/wjg.v13.i15.2240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chow DC, Babaian M, Taubin HL. Jejunoileal diverticular. Gastroenterologist. 1997;5(1):78–84. [PubMed] [Google Scholar]
- 16.Wilcox RD, Shatney CH. Surgical significance of acquired ileal diverticulosis. Am Surg. 1990;56:222–225. [PubMed] [Google Scholar]
- 17.Chiu EJ, Shyr YM, Su CH, Wu CW, Lui WY. Diverticular disease of the small bowel. Hepatogastroenterology. 2000;47(31):181–184. [PubMed] [Google Scholar]


