Abstract
Background:
Developing countries such as Jamaica suffer increasingly from high levels of public health problems related to chronic diseases.
Aims:
To examine the physical health status and use a model to determine the significant predictors of poor health status of Jamaicans who reported being diagnosed with a chronic non-communicable disease.
Methods and Materials:
The current study extracted a sub-sample of 714 people from a larger nationally representative cross-sectional survey of 6,783 Jamaicans. A self-administered questionnaire was used to collect the data from the sample. Statistical analysis was performed using chi-square to investigate non-metric variables, and logistic regression to determine predictors of poor health status.
Results:
Approximately one-quarter 25.3%) of the sample reported that they had poor health status. Thirty-three percent of the sample indicated unspecified chronic diseases: 7.8% arthritis, 28.9% hypertension, 17.2% diabetes mellitus and 13.3% asthma. Asthma affected 47.2% of children and 23.2% of young adults. S ignificant predictors of poor health status of Jamaicans who reported being diagnosed with chronic diseases were: age of respondents, area of residence and inability to work.
Conclusion:
Majority of the respondents in the sample had good health, and adults with poor health status were more likely to report having hypertension followed by diabetes mellitus and arthritis, while asthma was the most prevalent among children. Improvement in chronic disease control and health status can be achieved with improved patient education on the importance of compliance, access to more effective medication and development of support groups among chronic disease patients.
Keywords: Chronic disease, diabetes, hypertension, self-rated health status, health conditions, Jamaica
Introduction
The rapidly increasing burden of chronic diseases is a key determinant of global public health. In 2001, chronic diseases contributed to approximately 60% of the 56.5 million total reported deaths in the world and approximately 46% of the global burden of disease. The proportion of the burden of non-communicable diseases is expected to increase to 57% by 2020[1].
In five out of the six regions of the World Health Organization (WHO), deaths caused by chronic diseases dominate the mortality statistics[2] and there is evidence that 79% of deaths attributable to chronic diseases are occurring in developing countries, such as those in the Caribbean, predominantly in middle-aged men[2]. Most Caribbean countries have experienced a health transition, with decreases in fertility and mortality rates and changing disease patterns. Leading up to the mid-1990s, the mortality pattern changed from deaths being mainly due to communicable diseases to them being mainly due to non-communicable diseases[3,4]. More recently, these countries have additionally observed the re-emergence of ‘old’ communicable diseases and the emergence of new communicable diseases, along with an increasing prominence of non-communicable diseases. Furthermore, with 15-20% and 20-25% of the adult population in English and Dutch-speaking Caribbean countries having diabetes and hypertension respectively, these non-communicable diseases account for the single largest expenditure in national drug budgets[5].
Jamaica has undergone a significant demographic transition in the last 5 decades[6,7]. Some features of this transition include the increase in the median age of the population from 17 years to 25 years between 1970 and 2000, the doubling of the proportion of persons older than 60 years old to over 10%, and the increase in life expectancy at birth from less than 50 years in 1950 to greater than 70 years in 2000[8]. As a result, the main causes of illness and death in Jamaica and many other Caribbean islands and regions at a similar state of development are the chronic non-communicable diseases[9]. There is an increased prevalence of diet-related chronic non-communicable diseases, such as cardio-vascular diseases, diabetes and obesity. Wilks, et al.[10], reporting on a survey of body mass index in an urban population, found that 30.7% of the men were overweight (7.2% were obese) and 64.7% of the women were overweight (31.5% obese). In this same study, it was found that hypertension had a prevalence of 19.1% among the males and 28.2% among the females, while the prevalence of diabetes was 8.9% and 15.3% among the males and females respectively[10].
Chronic diseases such as heart disease, cancer and diabetes negatively affect the general health status and quality of life of individuals[11], and there is an absence in the literature of studies looking at the health status of persons in the Caribbean with chronic non-communicable diseases. It is against this background that this study was undertaken. This study was designed to explore any association between chronic non-communicable disease and health status. The aim of the study was to examine the self-reported health status of Jamaicans in rural, peri-urban and urban areas of residence. A model is used to predict the social determinants of poor health status of Jamaicans who reported at least one chronic non-communicable disease.
Patients and Methods
The current study extracted a subsample of 714 people who answered the question of having sought medical care in the last 4-weeks from a larger nationally representative cross-sectional survey of 6,783 Jamaicans (Jamaica Survey of Living Conditions, 2007)[12]. The survey was drawn using stratified random sampling. This design was a two-stage stratified random sampling design where there was a Primary Sampling Unit (PSU) and a selection of dwellings from the primary units. The PSU is an Enumeration District (ED), which constitutes a minimum of 100 residents in rural areas and 150 in urban areas. An ED is an independent geographic unit that shares a common boundary.
This study made use of the Jamaica Survey of Living Conditions (JSLC) 2007[12], which was conducted by the Statistical Institute of Jamaica (STATIN) and the Planning Institute of Jamaica (PIOJ) between May and August 2007. The researchers chose this survey based on the fact that it is the latest survey on the national population and that that it has data on self-reported health status of Jamaicans. Self-administered questionnaires were used to collect the data, and these were then stored and analyzed using SPSS for Windows 16.0 (SPSS Inc; Chicago, IL, USA). The questionnaire was modeled in the World Bank's Living Standards Measurement Study (LSMS) household survey. The questionnaire covered areas such as socio-demographic, economic and health variables. The non-response rate for the survey was 26.2%.
Descriptive statistics such as mean, standard deviation (SD), frequency and percentage were used to analyze the socio-demographic characteristics of the sample. Chi-square was used to examine the association between non-metric variables, and an Analysis of Variance (ANOVA) was used to test the relationships between metric and non-dichotomous categorical variables. Logistic regression examined the relationship between the dependent variable and some predisposed independent (explanatory) variables; because the dependent variable was a binary one (self-reported health status is 1 if the respondent reported poor health status and 0 if otherwise).
The results were presented using unstandardized B-coefficients, Wald statistics, odds ratio and confidence interval (95% CI). The predictive power of the model was tested using the Omnibus Test of Model and Hosmer & Lemeshow[13], which was used to examine goodness of fit of the model. The correlation matrix was examined in order to ascertain whether autocorrelation (or multicollinearity) existed between variables. Based on Cohen & Holliday[14], correlation can be low (weak) – from 0 to 0.39; moderate – 0.4-0.69, and strong – 0.7-1.0. This was used to exclude (or allow) a variable in the model. Wald statistics were used to determine the magnitude (or contribution) of each statistically significant variable in comparison with the others, and the Odds Ratio (OR) was used to interpret each significant variable.
Multivariate regression framework[15] was utilized to assess the relative importance of various demographic, socio-economic characteristics, physical environment and psychological characteristics in determining the reported health status of Jamaicans; this has also been employed outside of Jamaica[16,17]. Having identified the determinants of health status from previous studies, using logistic regression techniques, final models were built for Jamaicans as well as for each of the geographical sub-regions (rural, peri-urban and urban areas of residence) and sex of respondents using only those predictors that independently predict the outcome. A p-value of 0.05 was used to for all tests of significance.
Model
The use of multivariate analysis in the study of health and subjective wellbeing (i.e., self-reported health or happiness) is well established[18] and this is equally the case in Jamaica and Barbados[19,20]. The use of this approach is better than bivariate analyses as many variables can be tested simultaneously for their impact (if any) on a dependent variable. The current study examined the social determinants of self-reported health status of Jamaicans (Equation 1). Equation 1 was again tested and decomposed by (i) sex of respondents and (ii) area of residence in order to ascertain those social predictors of each sub-group.
Ht= f(Ai, Gi, HHi, ARi, It Ji, 1nC, InDi, EDi, MRi, Si, HIi, 1nY, CRi, MCt, SAi, Ti εi) [1]
where Ht (i.e., self-rated current health status in time t) is a function of age of respondents, Ai; sex of individual i, Gi; household head of individual i, HHi; area of residence, ARi; current self-reported illness of individual i, I t ; injuries received in the last 4 weeks by individual i, Ji; logged consumption per person per household member, lnC; logged duration of time that individual i was unable to carry out normal activities, lnDi; education level of individual i, EDi; marital status of person i, MRi; social class of person i, Si; health insurance coverage of person i, HIi; logged income, lnY; crowding of individual i, CRi; medical expenditure of individual i in time period t, MC t ; social assistance of individual i, SAi; length of time living in current household by individual i, Ti; and an error term (i.e., residual error).
The final model that was derived from the general Equation[1] can be used to predict health status of Jamaicans (Equation[2])[2].
Ht=f(Ai, ARi, InDUt, εi)
Variables that were investigated include age, self-reported illness (diabetes mellitus, hypertension) and social class. Age group is a non-binary measure: children (under 15 years); young adults (15 to 30 years); other-aged adults (31 to 59 years); young elderly (60 to 74 years); old elderly (75 to 84 years) and oldest elderly (85 years and older).
Results
Demographic characteristics of sample
The sample constituted 714 respondents (36.7% men and 63.3% women) with a mean age of 49.15 years. The majority of the sample was never married (44.7%), 13.4% were widowed, 1.7% separated, 3.1% divorced and 37.1% married. Some 25.3% of the sample reported that they had poor health status, 31.9% indicated at least good and 42.8% indicated fair. Thirty-three percent of the sample indicated unspecified chronic illness: 7.8% arthritis, 28.9% hypertension, 17.2% diabetes mellitus and 13.3% asthma. Marginally more of the sample was in the upper class (41.6%), 19.7% in the middle class and 38.7% in the lower class (i.e., poor). The majority of the respondents were elderly (ages 60 years and older – 41.6%) compared to 33.6% other-aged adults, 9.7% young adults and 15.1% children. Interestingly, the mean number of persons per room was 4.07 (S.D. 2.63 persons) and in rural areas it was 4.38 (S.D. 2.75 persons) compared to 3.9 persons in other town areas (S.D. 2.41) and 3.6 persons in urban areas (S.D. 2.42) – F statistic 2, 711 = 6.642, p = 0.001.
Table 1 revealed that there is a statistical correlation between social class, self-evaluated health status, annual income and area of residence (p < 0.001). Just over 50% of the rural residents were in the lower class (i.e., poor) compared to 26.4% of other town residents and 18.0% of urban dwellers. With regards to self-evaluated health and area of residence, most of the residents reported fair health status: urban residents (46.5%); other town residents (50.8%) and rural residents (38.4%). On the other hand, 28.6% of rural residents indicated that they had good self-evaluated health status compared to 31.7% of other town residents and 38.5% of urban dwellers. The mean annual income of rural residents was US$5,873.08 compared to US$8,218.05 for other town residents and US$10,312.41 for urban residents. Most of the rural respondents were in the lower class (52.9%), while 26.4% of the other town residents were in the lower class and 18% of the urban dwellers were in the lower class.
Table 1.
Socio-demographic characteristics of sample
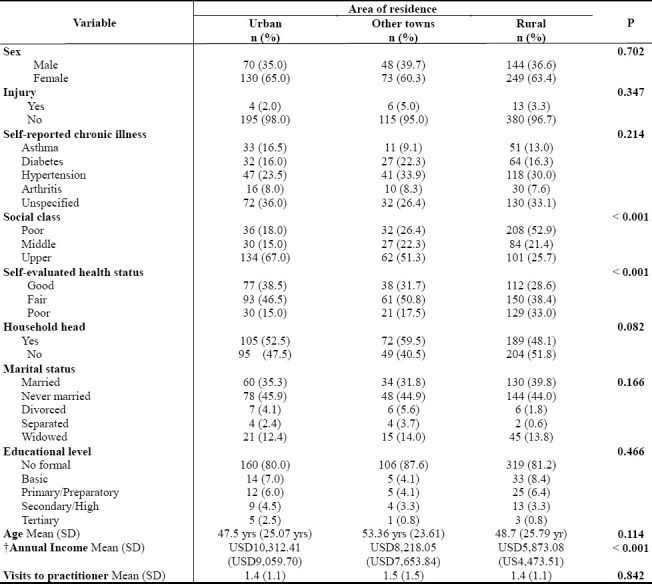
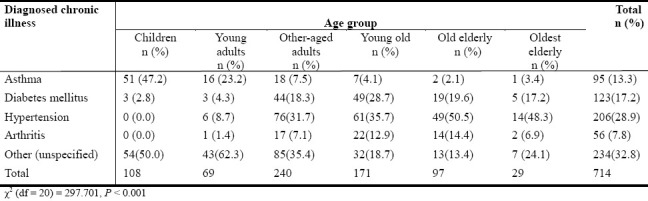
Table 2 revealed that there is a statistical correlation between diagnosed chronic diseases and age group [χ2 (DF = 20) = 297.701, p < 0.001, n = 714]. Asthma was primarily an illness for the younger ages and primarily affects children: 47.2% of children and 23.2% of young adults (Table 2).The findings revealed that as an individual aged, he/she was more likely to report being diagnosed with hypertension: 0% of children, 8.7% of young adults, 31.7% of other-aged adults, 35.7% of young old, 50.5% of old-elderly and 48.3% of oldest-elderly. Arthritis was more likely to affect older ages than young ages: 0% of children, 1.4% of young adults, 7.1% of other-aged adults, 12.9% of young-old, 14.4% of old-elderly and 6.9% of oldest-elderly. On the other hand, the findings also revealed that as an individual aged, he/she was more likely to be aware of the typology of chronic illness that he/she has than they were at young ages (i.e., under 31 years). Interestingly, 2.8% of children had diabetes compared to 4.3% of young adults, 18.3% of other-aged adults, 28.7% of young old, 19.6% of old-elderly and 17.2% of oldest-elderly.
Table 2.
Diagnosed chronic recurring illness by age group
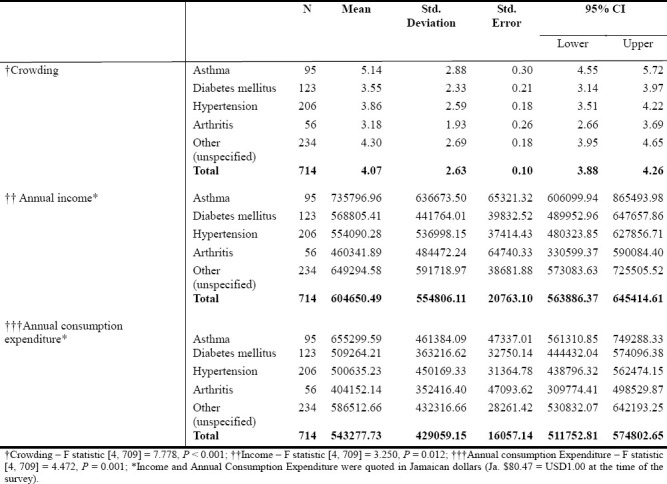
Based on Table 3, no statistical correlation was found between diagnosed chronic disease and social class [χ2 (DF = 8) = 13.882, p = 0.085, n = 714]. On the other hand, a statistical relationship was found between income, consumption, crowding and chronic disease (p < 0.5; Table 4). Furthermore, there is a similarity across the aforementioned variable as asthma was found to be associated with the most income, consumption and persons per room; and unspecified chronic disease was the second leading reported dysfunction. Diabetes mellitus was found to be the third leading reported chronic disease influencing people with more income and consumption. While hypertension was the third most reported chronic disease associated with crowding, it was the fourth most reported dysfunction associated with income and consumption expenditure.
Table 3.
Diagnosed chronic illness by social class
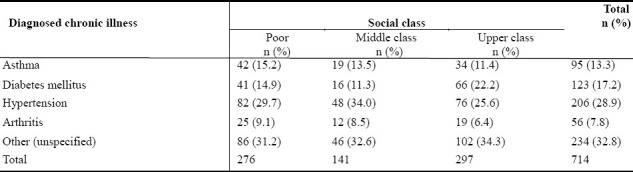
Table 4.
Crowding, income and annual consumption expenditure by diagnosed chronic disease
Multivariate analyses
Using logistic regression analyses, of the 17 variables that were tested for this study, only 3 emerged as statistically significant predictors of poor health status of Jamaicans who reported being diagnosed with chronic diseases (Table 5): age of respondents (OR = 1.029, 95% CI = 1.018 – 1. 040), area of residence (urban areas – OR = 0.352, 95% CI = 0.191 – 0.652; other towns – OR = 0.352, 95% CI = 0.173 – 0.744) and log duration unable to work (OR = 1.711, 95% CI = 1.280 – 2.271).
Table 5.
Logistic regression: Predictor of poor health status of patients who reported chronic disease
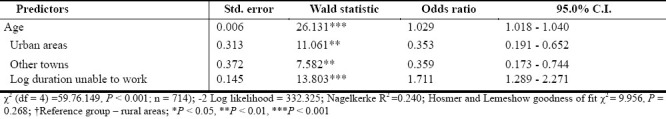
The model (Equation 2) had statistically significant predictive power [χ2 (4) =59.76.149, p < 0.001; Hosmer and Lemeshow goodness of fit χ2 = 9.956, p = 0.268] and correctly classified 74.4% of the sample (correctly classified 92.6% of those who were in poor health and 31.6% of those who were not in poor health). The logistic regression model can be written as: Log (probability of poor health status/probability of not reporting poor health status) = -0.704 + 0.028 (age) -1.041(urban residents) -1.041 (other towns) + 0.537 (log duration unable to work). Furthermore, the predictors accounted for 24% of the variability in poor health status (Table 5).
Discussion
There is an association between chronic disease and health status and the former has a significant negative impact on the physical aspects of health[21]. Self-reported health status has been widely used in censuses, surveys, and observational studies and there is evidence suggesting that self-reported health is an indicator of general health with good construct validity[22] and is a respectably powerful predictor of mortality risks[23], disability[24] and morbidity[25]. The results of this study showed that the majority of those sampled reported to be experiencing at least good or fair health, while approximately one-quarter indicated poor health. These results concur with those by other researchers from Dominica[26] and Trinidad[27].
The current study revealed that hypertension was the most common chronic disease among the respondents, followed by diabetes mellitus and arthritis. Hypertension was highest among the elderly, with the old-elderly recording the most among the elderly cohorts. In a study by Sargeant et al.[28], hypertension is more common among women and the elderly in Jamaica. Studies from developed countries have reported prevalence of raised blood pressure among the elderly to vary from 60% to 80%[29]. Hypertension is one of the most important treatable causes of morbidity and mortality and accounts for a large proportion of cardiovascular diseases in the elderly in Jamaica[28]. The age- and sex-adjusted prevalence in Jamaica is 24%[30] with somewhat higher levels in women than in men. The Jamaican Healthy Lifestyle Survey Report 2000[31] noted a prevalence of hypertension of 19.9% among males and 21.7% among females; prevalence increased with age in both rural and urban populations and in both sexes. Among persons known to be hypertensive, 42% were on treatment, and of this group, 37.7% had been able to lower and maintain their blood pressure at 140/90 or less. In the Caribbean and the USA, the higher prevalence of hypertension was associated with an increased prevalence of obesity, especially in women, and with greater intake of dietary sodium[32,33].
Diabetes mellitus is an important cause of morbidity and mortality in Jamaica and represents a significant burden on health services. Diabetes was the second leading cause of chronic disease in this study and was most prevalent among the young-old with just under one-third reporting that they have diabetes mellitus. The prevalence of diabetes mellitus is high in Jamaica and the Caribbean and many patients have poor metabolic control[34]. In Jamaica the prevalence of diabetes among persons 25-74 years old is estimated to be 12% to 16%[35–37], but of which a third is unrecognized[36,37]. There is also evidence that the diabetes prevalence has increased[38]. In the Jamaican Healthy Lifestyle Survey Report 2000[31], diabetes mellitus was found in 6.3% of males and 8.2% of females and there was a sharp increase with age. Awareness of diabetes mellitus among those classified as diabetic by the survey was 76.3%. Almost one-third of those classified as diabetic were not being treated, and 60% of those who reported being on medication did not have their condition under control. The average length of stay in hospitals was 8.3 days for diabetes mellitus in 2002, compared to 6.3 days for all conditions[31]. Diabetes mellitus accounts for about 10% of mortality in Jamaica[39] and is ranked fourth as the principal cause of death among Jamaicans during the period 1990 to 1994[40]. But the impact of diabetes mellitus on mortality is under-reported since the disease may contribute to mortality from such other conditions as cerebrovascular accidents and myocardial infarctions[41]. Furthermore, there is evidence that the high prevalence of diabetes in Jamaica is due to the low rates of awareness, treatment and control among patients with diabetes mellitus[34].
In the Caribbean, there has been growing concern at the apparent increase in asthma in children and young adults. In 2001, hospital morbidity patterns and primary care data indicated that respiratory illnesses dominated the list of childhood infirmities among children 0-14 years. For children aged 0-4 years, asthma was the major condition for which patients were seen in health facilities, a condition mainly attributable to the high incidence of tobacco smoke to which these children are exposed[42]. In this study, asthma was the predominant chronic disease affecting approximately one-half of the children and almost one-quarter of young adults. Asthma is an important public health issue in Jamaica. Exercise-induced asthma has been reported to occur in 20 percent of school age children[43]. In government hospitals in Jamaica, five percent of clinic visits are asthma related and 25 percent of respiratory admissions to hospital are due to asthma[44]. Barnes and colleagues[45] studied asthmatic children in Barbados where treatment was associated with use of inhalers, but no distinction between bronchodilators and corticosteroids was made[46]. Asthma is a significant cause of mortality in Jamaica, resulting in a death rate of approximately 5 per 100,000[47].
Studies conducted over the last three decades in Third World countries have confirmed that rheumatoid arthritis occurs throughout the world. Rheumatoid arthritis is a chronic systemic inflammatory disorder that may affect many tissues and organs but particularly the joints, often progressing to destruction of the particular cartilage and ankylosis of the joints[48,49]. Due to its physical, social and psychological burden, patients’ experience many difficulties in various aspects of their lives can contribute to their self-reported poor health. Rheumatoid arthritis is the third chronic illness among the respondents in the study. In India, the prevalence of rheumatoid arthritis (0.75%) is similar to that in the West[50]. The rarity of rheumatoid arthritis in rural Africa contrasts with the high prevalence of the disease in Jamaica, where over 2% of the adult population is affected[51]. In a study in Latin America, rheumatoid arthritis was the reason for seeking medical advice in 22% of rheumatology clinic patients[52]. Quality of life is significantly low in patients with rheumatoid arthritis, knee osteoarthritis and fibromyalgia syndrome, whose depression and/or anxiety scores are high[53]. Therefore, these patients should be managed using a multidisciplinary approach including psychiatric support.
In this study, just over one-third of the respondents indicated an unspecified chronic illness. The unspecified chronic diseases could be other chronic non-communicable diseases such as a malignant neoplasm or a chronic communicable disease. In Jamaica, cancers accounted for 15% of non-communicable diseases and 9% of total disease burden in 1990. Cancers of the breast and cervix are the most common neoplasms in women, with rates in 1991 of 22.6 and 19.2 per 1,000 population members, respectively. Prostate cancer was the number one form of cancer found in men[54]. In 2002, there were 3,769 public hospital discharge diagnoses (4% of total discharge diagnoses) for malignant neoplasms with an equal gender distribution. The types of neoplasms involved for males, in order of decreasing frequency, were: trachea, bronchus, and lungs; prostate; leukemia; and non-Hodgkin's lymphoma; representing 56% of all cancers. For females, the order was as follows: breast; cervix uteri; other malignant neoplasms of female genital organs; trachea, bronchus, and lungs; leukemia; and non-Hodgkin's lymphoma; together representing 56% of all cancers[55]. The unspecified chronic illness may include HIV/AIDS, a communicable disease, which has become a serious public health concern in Jamaica. The national incidence of AIDS in 2000 was 352 per 1,000,000 population members[56]. In addition, the unspecified chronic disease may include depression and there is evidence to suggest that depressive disorders frequently accompany other chronic medical diseases. The 2000 Lifestyle Survey found approximately 25 % depressive symptoms in the general population[31]. Anderson et al.[57] concluded that the presence of diabetes mellitus increases the risk of depression and studies have shown that in persons diagnosed with diabetes mellitus the prevalence of depression ranges from 6.1% - 60.7%[58].
The majority of the respondents resided in rural areas and just over one-half of these were in the lower class. The study found that there was an income differential between respondents in rural compared with urban areas of residence, with those in the rural areas having mean annual income of approximately two-thirds of their urban counterparts. Diabetes mellitus was found to be the third leading reported chronic disease influencing persons with greater income and consumption. While hypertension was the third most reported chronic disease associated with crowding, it was the fourth most reported dysfunction associated with income and consumption expenditure. According to Sobal and Stunkard[59], in developing societies there is a higher likelihood of obesity among men in higher socio-economic strata. These men are at increased risk of developing type 2 diabetes mellitus[60] which is increasing in the adult population. Most of the respondents in this study were female and single women constitute 45% of Jamaican heads of household[61]. In Jamaica, female-headed households are poorer than those headed by males and twice as likely to be unemployed. Male-headed households are smaller and have a per capita expenditure 10 times higher than female-headed households[62,63]. The 1999 data from STATIN show that individuals who live in rural areas, who are in the poorest quintile, and who are males are less likely to seek health care[64].
Conclusion
The general epidemiological shift from infectious to chronic non-communicable diseases in Jamaica puts the residents at risk. The majority of the respondents in the sample had good health. Adults with poor health status were more likely to report having hypertension followed by diabetes mellitus and arthritis, while asthma was the most prevalent among children. Poor health status was more prevalent among those of lower economic status in rural areas who reported the least annual income. Predictors of poor health status of Jamaicans who reported being diagnosed with a chronic disease were: age, area of residence, and inability to work (therefore being unemployed). Given the high prevalence and poor levels of control, hypertension and diabetes mellitus remain formidable issues for public health care in Jamaica and the Caribbean. Poverty, low education and poor access to health care in rural communities intensify the inertia to the lifestyle modifications that are necessary to bring about greater levels of control. We suggest that further improvement in chronic disease control can be achieved with improved patient education on the importance of compliance, access to more effective medication and development of support groups among patients with chronic disease(s).
References
- 1.The world health report 2002: reducing risks, promoting healthy life. Geneva: World Health Organization; 2002. World Health Organization (WHO) [Google Scholar]
- 2.World Health Organization. Geneva: World Health Organization; 2002. Diet, physical activity and health. [Google Scholar]
- 3.Figueroa JP. Health trends in Jamaica.Significant progress and a vision for the 21st century. West Indian Med J. 2001;50(Suppl 4):15–22. [PubMed] [Google Scholar]
- 4.Guilliford MC. Epidemiological transition in Trinidad and Tobago, West Indies 1953-1992. Int J Epidemiol. 1996;25:357–365. doi: 10.1093/ije/25.2.357. [DOI] [PubMed] [Google Scholar]
- 5.Caribbean Commission on Health and Development Report. 2004 [Google Scholar]
- 6.Forrester TE. Research into policy. Hypertension and diabetes mellitus in the Caribbean. West Indian Med J. 2003;52:164–169. [PubMed] [Google Scholar]
- 7.Wilks R, Bennett F, Forrester T, McFarlane-Anderson N. Chronic diseases: The new epidemic. West Indian Med J. 1998;47(Suppl 4):40–44. [PubMed] [Google Scholar]
- 8.Demographic Statistics 2001. Kingston: STATIN; 2002. Statistical Institute of Jamaica (STATIN) [Google Scholar]
- 9.Sargeant LA, Wilks RJ, Forrester TE. Chronic diseases-facing a public health challenge. West Indian Med J. 2001;50(Suppl 4):27–31. [PubMed] [Google Scholar]
- 10.Wilks R, Bennett F, Forrester T, McFarlane-Anderson N, Anderson SG, Kaufman JS, Rotimi C, Cooper RS, Cruickshank JK. Chronic disease: the new epidemic. West Indian Medical Journal. 1998;47(suppl 4):40. [PubMed] [Google Scholar]
- 11.Atlanta, Ga: Centers for Disease Control and Prevention; 2000. Measuring Healthy Days: Population assessment of health-related quality of life. [Google Scholar]
- 12.Jamaica Survey of Living Conditions 2007. Kingston: PIOJ, STATIN; 2008. Planning Institute of Jamaica and Statistical Institute of Jamaica (PIOJ & STATIN) [Google Scholar]
- 13.Homer D, Lemeshow S. Applied logistic regression. 2nd ed. New York: John Wiley & Sons Inc.; 2000. [Google Scholar]
- 14.Cohen L, Holliday M. Statistics for social sciences. London, England: Harper and Row; 1982. [Google Scholar]
- 15.Asnani MR, Reid ME, Ali SB, Lipps G, Williams-Green P. Quality of life in patients with sickle cell disease in Jamaica: Rural-urban differences. Rural and Remote Health. 2008;8(890):1–9. [PubMed] [Google Scholar]
- 16.Grossman M. The demand for health – A theoretical and empirical investigation. New York: National Bureau of Economic Research; 1972. [Google Scholar]
- 17.Hambleton IR, Clarke K, Broome HL, Fraser HS, Brathwaite F, Hennis AJ. Historical and current predictors of self-reported health status among elderly persons in Barbados. Rev Pan Salud Public. 2005;17(5-6):342–352. doi: 10.1590/s1020-49892005000500006. [DOI] [PubMed] [Google Scholar]
- 18.Smith JP, Kington R. Demographic and economic correlates of health in old age. Demography. 1997;34:159–170. [PubMed] [Google Scholar]
- 19.Hutchinson G, Simeon DT, Bain BC, Wyatt GE, Tucker MB, LeFranc E. Social and health determinants of wellbeing and life satisfaction in Jamaica. International Journal of Social Psychiatry. 2004;50:43–53. doi: 10.1177/0020764004040952. [DOI] [PubMed] [Google Scholar]
- 20.Bourne P. Using the biopsychosocial model to evaluate the wellbeing of the Jamaican elderly. West Indian Medical J. 2007;56(suppl 3):39–40. [Google Scholar]
- 21.Groothoff JW, Grootenhuis MA, Offringa M, Gruppen MP, Korevaar JC, Heymans HS. Quality of life in adults with end-stage renal disease since childhood is only partially impaired. Nephrol Dial Transplant. 2003;18:310–317. doi: 10.1093/ndt/18.2.310. [DOI] [PubMed] [Google Scholar]
- 22.Smith J. Measuring health and economic status of older adults in developing countries. Gerontologist. 1994;34:491–496. doi: 10.1093/geront/34.4.491. [DOI] [PubMed] [Google Scholar]
- 23.Idler EL, Benjamin Y. Self-rated health and mortality: A Review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- 24.Idler EL, Kasl S. Self-ratings of health: Do they also predict change in functional ability? Journal of Gerontology. 1995;50B(6):S344–S353. doi: 10.1093/geronb/50b.6.s344. [DOI] [PubMed] [Google Scholar]
- 25.Schechter S, Beatty P, Willis GB. Asking survey respondents about health status: Judgment and response issues. In: Schwarz N., Park D., Knauper B., Sudman S., editors. Cognition, Aging, and Self-Reports. Ann Arbor. Michigan: Taylor and Francis; 1998. [Google Scholar]
- 26.Luteijn B. Health status of the elderly in the Marigot Health District, Dominica ; 45(Suppl. West Indian Medical Journal. 1996;45(Suppl. 2):31. [PubMed] [Google Scholar]
- 27.Rawlins JM, Simeon DT, Ramdath DD, Chadee DD. The elderly in Trinidad: Health, social and economic status and issues of loneliness. West Indian Medical Journal. 2008;57:589–595. [PubMed] [Google Scholar]
- 28.Sargeant L, Boyne M, Bennett F, Forrester T, Cooper R, Wilks R. Impaired glucose regulation in adults in Jamaica: Who should have the oral glucose tolerance test? Pan American Journal of Public Health. 2004;16:35–42. doi: 10.1590/s1020-49892004000700005. [DOI] [PubMed] [Google Scholar]
- 29.Kalavathy MC, Thankappan KR, Sharma PS, Vasan RS. Prevalence, awareness, treatment and control of hypertension in an elderly community-based sample in Kerala, India. Natl Med J India. 2000;13:9–15. [PubMed] [Google Scholar]
- 30.Cooper R, Rotimi C, Ataman S, McGee D, Osotimehin B, Kadir S, Muna W, Kingue H, Fraser H, Forrester T, Bennett F, Wilks R. The prevalence of hypertension in seven populations of West African origin. Am J Public Health. 1997;7:160–168. doi: 10.2105/ajph.87.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Figueroa JP, Ward E, Walters C, Ashley DE, Wilks RJ. Jamaica Healthy Lifestyle Survey Report. 2000 [Google Scholar]
- 32.Ravallion M. Poverty comparisons. Chur, Switzerland: Harwood Academic Publishers; 1994. [Google Scholar]
- 33.Sadana R, Mathers CD, Lopez AD, Murray CJL, Iburg K. Comparative analyses of more than 50 household surveys on health status. Geneva: World Health Organization; 2000. [Google Scholar]
- 34.Wilks R, Sargeant L, Gulliford M, Reid M, Forrester T. Management of diabetes mellitus in three settings in Jamaica. Pan Am J Public Health. 2001;9:65–71. doi: 10.1590/s1020-49892001000200002. [DOI] [PubMed] [Google Scholar]
- 35.Wilks R, Bennett F, Forrester T, McFarlane-Anderson N, Anderson SG, Kaufman JS, Rotimi C, Cooper RS, Cruickshank JK. Diabetes in the Caribbean: Results of a population survey from Spanish Town, Jamaica.British Diabetic Association. Diabetic Medicine. 1999;16:875–883. doi: 10.1046/j.1464-5491.1999.00151.x. [DOI] [PubMed] [Google Scholar]
- 36.Ragoobirsingh D, Lewis-Fuller E, Morrison EY. The Jamaican Diabetes Survey. Diabetes Care. 1995;18(9):1277–1279. doi: 10.2337/diacare.18.9.1277. [DOI] [PubMed] [Google Scholar]
- 37.Cooper RS, Rotimi CN, Kaufman JS, Owoaje EE, Fraser H, Forrester T, Wilks R, Riste LK, Cruickshank JK. Prevalence of NIDDM among populations of the African diaspora. Diabetes Care. 1997;20(3):343–348. doi: 10.2337/diacare.20.3.343. [DOI] [PubMed] [Google Scholar]
- 38.Florey Cdu V, McDonald H, McDonald J, Miall WE. The prevalence of diabetes in a rural population of Jamaican adults. Int J Epidemiol. 1972;1(2):157–166. doi: 10.1093/ije/1.2.157. [DOI] [PubMed] [Google Scholar]
- 39.Demographic statistics 1995. Kingston, Jamaica: Statistical Institute; 1996. Statistical Institute of Jamaica. [Google Scholar]
- 40.Caribbean Regional Health Study. Washington, DC: Pan American Health Organization; 1996. Pan American Health Organization; pp. 21–22. [Google Scholar]
- 41.Alleyne SI, Cruickshank JK, Golding AL, Morrison EY. Mortality from diabetes mellitus in Jamaica. Bull Pan Am Health Organ. 1989;23(3):306–314. [PubMed] [Google Scholar]
- 42.Prendergast K, Ashley D. Report on the Results of the Global Youth Tobacco Survey in Jamaica – 2001. http://www.cdc.gov/tobacco/global/gyts/reports/paho/2001/ Jamaica.2001Paho01.htm .
- 43.Nichols DJ, Longsworth FG. Prevalence of exercise-induced asthma in schoolchildren in Kingston, St Andrew and St Catherine, Jamaica. West Indian Med J. 1995;44:16–19. [PubMed] [Google Scholar]
- 44.Ward E, Grant A. Epidemiological Profile of Selected Health Conditions and Selected Services in Jamaica. A Ten Year Review. 2002 [Google Scholar]
- 45.Barnes K C, Brenner R J, Helm R M, Howitt M E, Naidu R P, Roach T. The role of the house dust mite and other household pests in the incidence of allergy among Barbadian asthmatics. West Indian Med J. 1992;41(suppl 1):38. [Google Scholar]
- 46.Barnes K C, Naidu R P. Plenty children got wheeze these days: Lay knowledge, beliefs and stated behaviours related to asthma in Barbados. West Indian Med J. 1993;42(suppl 1):37. [Google Scholar]
- 47.Scott PW, Mullings RL. Bronchial asthma deaths in Jamaica. West Indian Med J. 1998;47:129–132. [PubMed] [Google Scholar]
- 48.Katz WA. Rheumatoid arthritis. In: Katz WA, editor. Diagnosis and Management of Rheumatic Diseases. Philadelphia: Lippincott; 1998. pp. 380–396. [Google Scholar]
- 49.Ravinder N, Feldmann MM. Rheumatoid arthritis. In: Maddison PJ, Isenberg DA, Woo P, Glass DN, editors. Oxford textbook of Rheumatology. Second Edition. New York: Oxford University Press; 1998. pp. 1004–1027. [Google Scholar]
- 50.Malaviya AW, Kapoor SK, Singh RR, Kumar A, Pande I. Prevalence of Rheumatoid arthritis in the adult Indian population. Rheumatology International. 1993;13(4):131–134. doi: 10.1007/BF00301258. [DOI] [PubMed] [Google Scholar]
- 51.Mijiyawa M. Epidemiology and Semiology of rheumatoid arthritis in third world countries. Rev Rhum Engl Ed. 1995;62(2):121–126. [PubMed] [Google Scholar]
- 52.Kerr G, Richards J, Harris E. Rheumatic disease in minority population. Medical Clinics of North America. 2005;89(4):829–868. doi: 10.1016/j.mcna.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 53.Ozcetin A, Ataoglus S, Kocer E, Yazici S, Yildiz O, Ataoglul A, Icmeli C. Effects of depression and anxiety on quality of life in patients with rheumatoid arthritis, knee osteoarthritis and fibromyalgia syndrome. West Indian Medical Journal. 2007;56(2):122–129. doi: 10.1590/s0043-31442007000200004. [DOI] [PubMed] [Google Scholar]
- 54.II. Jamaica. Washington D.C.: 1998. Pan American Health Organization. Health in the Americas. [Google Scholar]
- 55.Ministry of Health Annual Report 2002. Kingston: Ministry of Health; 2003. Jamaica, Ministry of Health. [Google Scholar]
- 56.Pan American Health Organization. Jamaica – Health situation analysis and trends summary. http://www.paho.org/English/DD/AIS/cp_388.htm .
- 57.Anderson R, Freedland KE, Clouse RE, Lustman PJ. The prevalence of co-morbid depression in adults with diabetes. Diabetes Care. 2001;24:1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 58.Friis R, Nanjundappa G. Diabetes, depression and employment status. Soc Sci Med. 1986;23:471–475. doi: 10.1016/0277-9536(86)90006-7. [DOI] [PubMed] [Google Scholar]
- 59.Sobal J, Stunkard AJ. Socioeconomic status and obesity: A review of the literature. Psychol Bull. 1989;105:260–275. doi: 10.1037/0033-2909.105.2.260. [DOI] [PubMed] [Google Scholar]
- 60.Astrup A, Finer N. Redefining Type 2 diabetes: Diabetes or obesity dependent diabetes. Obesity Reviews. 2001;1(2):57–59. doi: 10.1046/j.1467-789x.2000.00013.x. [DOI] [PubMed] [Google Scholar]
- 61.Dunn LL. Jamaica, : Situation of children in prostitution: A rapid assessment. International Labor Organization: International Program on the Elimination of Child Labor, Geneva, Switzerland; 2001. [Google Scholar]
- 62.Situation analysis on excluded children in Jamaica, 2006. Kingston: UNICEF; 2006. United Nation's Nation Children Fund (UNICEF) [Google Scholar]
- 63.A review of gender issues in the Dominican Republic, Haiti and Jamaica, 2002. Report No. 21866-LAC. Washington, DC: The World Bank; 2002. World Bank. [Google Scholar]
- 64.Jamaica Survey of Living Conditions: report. Kingston, Jamaica: The Statistical Institute of Jamaica; 1999. The Statistical Institute of Jamaica; pp. 45–47. [Google Scholar]


