Abstract
Objectives:
The aim of this study was to evaluate the efficiency of ozone alone and with a re-mineralizing solution following application on initial pit and fissure caries lesions in permanent molars.
Methods:
Forty children (9–12 years) having non-cavitated fissure caries lesions on bilateral 40 first permanent mandibular molar teeth were participated in the study. Patients were randomly allocated to 2 experimental groups consisting of 20 subjects. In the first group, ozone was applied once for 40 seconds to the assigned test teeth of each pair. In the second group, ozone was applied once for 40 seconds to the assigned test teeth of each pair with the use of re-mineralizing solution. Progression or improvement of the caries was assessed at baseline, immediately after treatment and at 1-,2-,3-, and 6 month follow-up by comparing the DIAGNOdent values, Clinical Severity Indexes, Oral Hygiene Scores. The results were analyzed statistically by using the Wilcoxon-Test for dependent samples in each group. When comparing different test groups (control and experimental groups) the Friedman S test followed by the Mann-Whitney U test was used.
Results:
A statistically significant difference was found between all of the control and experimental test lesions in each group (P<.001). However, there was no statistically significant difference between the ozone treated groups and those using the additional re-mineralizing solution (P>.001).
Conclusions:
Ozone treatment either alone or combined with a re-mineralizing solution was found to be effective for remineralization of initial fissure caries lesions.
Keywords: Ozone, Fissure caries, Preventive dentistry
INTRODUCTION
It is well known that dental caries is a multifactorial infectious disease caused by aciduric and acidogenic bacteria that is a major oral health problem affecting 60–90% of schoolchildren and also adults.1 Since the 19th century, the best practice in treating dental caries has been physical amputation of softened tissue from the tooth and replacement with some form of restorative materials. As we move into the 21st century, we have experienced significant improvement in equipment and technology. The ability to treat a carious lesion today without the need for amputation of the diseased tissue is one of the greatest achievements in dentistry.2
The caries process is a balance between demineralizing cariogenic challenges and neutralizing, remineralizing aspects, such as the salivary buffer capacity and minerals. It has been suggested that these processes are dynamic, and it is possible to modify the equilibrium towards remineralization with primary preventive strategies if the dental enamel surface is not lost.2,3
In recent years, ozone has been used for initial pit and fissure caries as an alternative management strategy within non-invasive interventions.4–6 Ozone is a gas that kills microorganisms quickly by oxidative degradation of the unsaturated fatty acids of the cell walls.7 Ozone can be applied in gas form or diluted in water, and both techniques show an effective reduction of cariogenic microorganisms in-vitro.8,9 Authors have suggested that ozone acts as a disinfectant with the unique feature of decomposing to a harmless, non-toxic, environmentally safe oxygen molecule.10,11 Recently an ozone-generating device HealOzone (Kavo, Biberach, Germany) has been developed and studied in dentistry. This device allows the application of high concentrations of gaseous ozone (2100±200 ppm at a flow rate of 615 ccs/min) to the tooth surface under controlled conditions.12 During the treatment, because of its molecular instability, ozone needs to be generated on-site, and it has a high oxidation potential. As a result of this property, bacteria in the lesion are destroyed as their cell membranes come into contact with the ozone. During this oxidative process glycoproteins, glycolipids, and other amino acids that protect the lesion are also affected. The dentin channels open, and the lesion is likely to remineralize before an established recolonization takes place. Furthermore, ozone also oxidizes pyruvic acid to acetate and CO2, and by the increased pH, makes remineralization possible.10,12
It has been proposed that tooth remineralization might be promoted with the assistance of salivary minerals and usable fluorides or remineralizing chemicals, resulting in a tooth surface that is more resistant to future acid attacks.13 On the other hand, it has not yet been investigated if an ozone application alone or combined with a mineral-rich solution might create different results in the remineralization of the carious lesions. The aim of this study was to evaluate the efficiency of an ozone delivery system alone, as well as combined with a re-mineralizing solution on initial pit and fissure caries lesions in permanent molars. During the treatment period the patients’ oral hygiene status was also evaluated.
MATERIAL AND METHODS
Forty children ranging between 9 and 12 years of age were included in the study. They had all been referred to the Gazi University, Faculty of Dentistry, Department of Pediatric Dentistry, which had laser fluorescence system (DIAGNOdent, Kavo, USA), which showed all having scores of 11–30 on 40 pairs of bilateral first permanent mandibular molar teeth. Ethical approval and informed consent were obtained from the Ankara University, Faculty of Dentistry.
At the beginning of the study, all participants were given adequate oral hygiene education consisting of a tooth brushing method (Modified Bass Technique), preventive dietary advice, instruction on the importance of oral health, and advice on using the given standard toothpastes (F- 1000 ppm, Colgate-Palmolive, UK) and toothbrushes (Colgate-Palmolive, UK) during the study period. The patients’ oral hygiene was assessed by recording the plaque, gingival status present on the distal surfaces and plaque accumulation on the occlusal surfaces of the examined molars within the study period.
Patients were randomly allocated to 2 test groups consisting of 20 subjects. For baseline clinical examinations, the patients’ oral hygiene was assessed as graded by Ekstrand et al14 (Table 1) by recording the distal and occlusal plaque and gingival status of each molar under examination. Then the Clinical Severity Index (CSI) and visual scoring were assessed for two contra-lateral molars as baseline reference values through use of a score system also developed by Ekstrand et al14 (Table 2). All patients were examined with an intro-oral camera (DPS, UK), with the video image displayed on a 40″ Sony screen. Where primary caries was detected, images of these teeth were captured into a video image storage system (Schick, USA). The system allows annotation of images, and this was used to locate the points used for DIAGNOdent assessment.
Table 1.
Oral hygiene status.
| Score | Status |
|---|---|
| Plaque Status (distal surface of examined molars) | |
| 0 | No plaque on probe |
| 1 | Thin plaque on probe |
| 2 | Thick plaque on probe |
| Gingival Status (distal of the molars under examination) | |
| 0 | No gingival examination |
| 1 | Gingival examination but no bleeding on probe |
| 2 | Gingival examination with bleeding on probe |
| Visible Plague Recording (occlusal surface of examined molars) | |
| 0 | No visible plaque |
| 1 | Visible plaque but difficult to recognize |
| 2 | Visible plaque easy to recognize |
Table 2.
Clinical severity index scores.
| Score | Description |
|---|---|
| 0 | No or slight change in enamel translucency after prolonged air dry (>5s) |
| *1 | Opacity (white) hardly visible on wet surface, but distinctly visible after air-drying (>5s) |
| *1a | Opacity (brown) hardly visible on wet surface, but distinctly visible after air-drying (>5s) |
| *2 | Opacity (white) distinctly visible without air-drying |
| *2a | Opacity (brown) distinctly visible without air-drying |
| 3 | Localized enamel breakdown in opaque/discolored enamel and/ grayish discoloration from the underlying dentin |
| 4 | Cavitation in opaque/discolored enamel exposing the dentin beneath |
Study criteria
In each group one molar was randomly assigned to receive ozone therapy or ozone appliance with a remineralizing solution, whereas the other molar of the pairs served as the corresponding untreated control. After the occlusal surfaces were cleaned with an airflow device (Prophyflex-3, Kavo, Germany), the measurements with the DIAGNOdent device were done after calibration of the device with a ceramic standard (Table 3).5 Readings for the assigned areas were assessed by two examiners for inter-examiner reproducibility and then re-examined after a week by the same examiners to assess intra-examiner reproducibility.
Table 3.
DIAGNOdent scores and possible clinical inferences.
| Score | Diagnodent value | Description |
|---|---|---|
| 0 | < 10 | Sound |
| *1 | 11–14 | Enamel caries in the outer half |
| *2 | 15–20 | Caries in enamel up to Dentino-enamel junction |
| *3 | 21–30 | Caries in enamel reaching to DEJ with some dentine demineralization |
| 4 | ≥ 31 | Deep dentinal caries |
Study criteria
In the first test group, only gaseous ozone was applied for 40 seconds to the assigned test teeth, whereas in the second test group after the application of gaseous ozone, a re-mineralizing solution (pH Balancer, CureOzone®, USA) was applied to the assigned test teeth and into the saliva according to the manufacturer’s directions. The treatment protocols were performed again at the recall visits (at months 1, 2, and 3 of the study period). Caries regression or improvement of each tooth pair was compared at baseline, immediately after treatment and in the 1-, 2-, 3-, and 6-month follow-up by using the laser-based DIAGNOdent values, CSI scores, and Oral Hygiene Status. For DIAGNOdent readings, declining values represent an improvement while increasing values represent deterioration of carious lesions.
According to the data, statistical analyses besides the inter- and intra-examiner reproducibility, were performed and calculated using Kappa statistics. Therefore, the DIAGNOdent values and CSI scores were used to compare the the ozone-only treatment with the ozone plus remineralizing treatment and with their control teeth, using the Wilcoxon-Test for dependent samples. For comparing the different test groups with each other, the Friedman test was followed by the Mann-Whitney test. (The level of significance was set at P<.001 or P<.002; Bonferroni correction was done when needed)
RESULTS
The gender, age, and past caries profile of the whole study population is given in Table 4.
Table 4.
Patients profile regarding number, gender, age, number of tooth, caries experience in the past (DMFS/defs/DMFT/deft).
| 1st Test group | 2nd Test group | |
|---|---|---|
| Number of patients | n=20 | n=20 |
| Girl | n=6 (% 30) | n=9 (% 45) |
| Boy | n=14 (% 70) | n=11 (% 55) |
| Age | 10.2±1.32 (9–12) | 10.3±1.09 (9–12) |
| Tooth number | n=40 | n=40 |
| DMFS | Mean= 3.80 (2.0–8.0) | Mean= 3.27 (2.0–10.0) |
| defs | Mean= 7.95 (0.0–26.0) | Mean= 10.8 (4.0–31.0) |
| DMFT | Mean= 3.70 (2.0–8.0) | Mean= 3.45 (2.0–4.0) |
| deft | Mean= 3.0 (0.0–6.0) | Mean= 4.05 (1.0–7.0) |
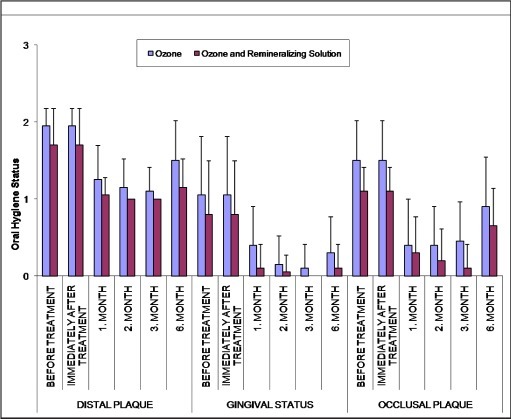
Oral hygiene status
Compared to the baseline, within 6 months’ time, statistically significant differences were observed for distal and occlusal plaque appearances as well as in the gingival examination for both test groups (P<.002). Furthermore, for all 3 parameters a regression was observed between the 3- and the 6- month examinations, but there were no significant differences (P>.002) (Figure 1).
Figure 1.
Changes of patients’ oral hygiene status over 6 months period.
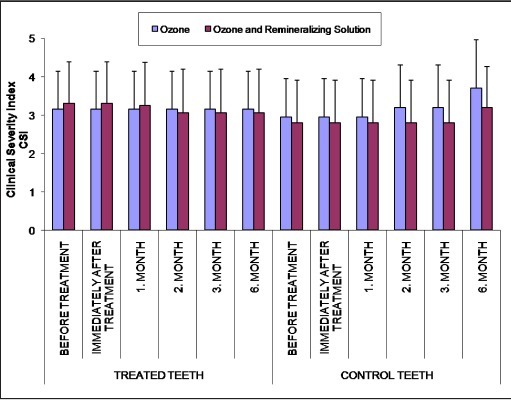
Clinical Severity Index (CSI)
For the ozone-treated group, the treated teeth revealed no significant differences between the baseline and the other examination periods of the study (P>.001). In the untreated control teeth of this group, a significant difference was found between the 6-month and the baseline examinations (P<.001); for the untreated control teeth, caries activation had occurred visually. For the ozone and remineralizing solution treated group, neither the teeth treated with ozone appliance along with remineralizing solution nor the untreated control teeth revealed statistically significant differences during the same period (Figure 2).
Figure 2.
Changes of CSI over 6 months period.
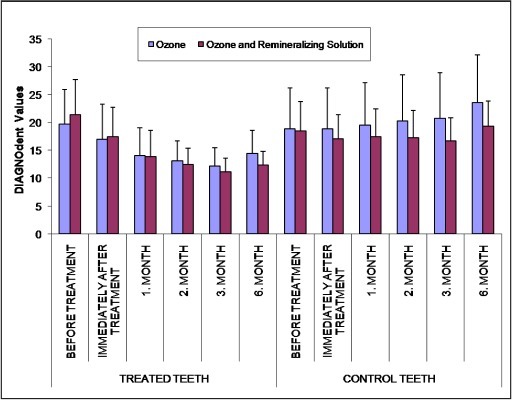
DIAGNOdent readings
For the ozone-treated group, the DIAGNOdent values of treated teeth decreased significantly compared to the baseline, whereas that of the untreated control teeth increased significantly (P<.001). For the group treated with ozone appliance with remineralizing solution, the DIAGNOdent values of treated teeth decreased significantly (P<.001), whereas the untreated control teeth revealed no significant difference between the baseline and 6-month examinations (P>.001) (Figure 3).
Figure 3.
Changes of DIAGNOdent readings over 6 months period.
In the ozone-treated group, 75% of treated teeth showed an improvement in remineralization, whereas 80% showed improvement in the ozone and remineralizing solution group. On the other hand for the control teeth, 80% of lesions in the ozone-treated group, and 30% of lesions in the other group showed an increase or progression according to the DIAGNOdent readings after the same period.
With regard to the repeatability of measurements from the laser fluorescence system DIAGNOdent, two examiners’ measurements were compared. The DIAGNOdent method revealed good intra-examiner reproducibility (Cohen’s K = 0.74 and 0.73, P<.001) as well as good inter-examiner reproducibility (Cohen’s K = 0.88 and 0.77, P<.001).
DISCUSSION
Prevention of disease has always been the most cost effective modality for any health care system. To avoid dental caries, since the 1960s the “preventive dentistry” or “non-invasive interventions” have seen some success. There is now strong scientific evidence that we can use the caries balance in treating caries as a disease for all ages.15 Furthermore, while the rate of dental caries has shown a significant decline in children and adolescents, fissure carious lesions in permanent molars still accounts for over 80% of total caries occurrences.5
The caries process can easily be explained as a balance between pathological factors (cariogenic bacteria, fermentable carbohydrates, salivary dysfunctions) and protective factors (salivary components and flow, existence of fluoride, antibacterial therapy).16–19 Featherstone et al20 indicated that reducing the pathological factors and enhancing the protective factors leads to reduction in risk and in caries. On the other hand, the management of dental caries is a complicated issue that is dependent on the stage at which caries is identified. Due to the potential reversibility of early lesions in their non-cavitated status, the idea of the treatment regime is that ozone diminishes the microflora in the lesion, oxidizes pyruvic acid to acetate and CO2, and thereby increases the pH to make remineralization of the demineralized tissue possible with the help of salivary minerals or usable remineralizing solutions.7
Yamayoshi and Tatsumi21 demonstrated that ozone was a strong oxidizer to the cell walls and the cytoplasmic membranes of microorganisms. Some of the available studies have assessed the antibacterial effects of ozone on oral microorganisms with results suggesting significant reductions in the number of planktonic microorganism cells in-vitro.11–24
Additionally, investigators have proposed that ozone alone may be sufficient to treat primary root caries or fissure caries due to its strong oxidizer potential.7,25 Baysan and Lynch26 have demonstrated that it is possible to remineralize primary root caries lesions (PRCLs) with the use of 10 or 20 seconds of ozonated water application. In addition, Hodson et al27 were in agreement with Baysan et al25 that ozone is effective for remineralization of initial fissure and root caries lesions.
The main purpose of applying ozone would be to kill viable microrganisms that remain in the carious lesions. Although traditional restorative work may eliminate the bacteria at the site of the restoration, the remainder of the mouth is left untouched, where caries continues unchecked and recolonization commences rapidly at the margins.3 However, Kramer et al28 revealed that etching and sealing can also reduce the number of microorganisms, but these procedures themselves reduced the viable microorganisms, in intact fissures and prepared fissures. Furthermore, Theilade et al29 found that some bacteria, such as Streptoccocus sanguis and Streptoccocus haemophilus, were reduced in number after treatment, while the main groups of cariostatic microorganisms that predominantly produce lactic acid, such as Streptoccocus mutans and Lactobacillus, were relatively unaffected. On the other hand, because ozone is a gas, it can penetrate and reach to the full depth of the fissure carious lesion and kill most of the microorganisms within 10 seconds.12 Again, Baysan et al4 stated that microorganisms in small, non-cavitated and less severe lesions showed greater reduction after the application of ozone; and their results related to the findings of Lynch,13 who reported that non-cavitated, small lesions had fewer cariogenic microorganisms than cavitated and large lesions. In the light of above studies participants having laser fluorescence system scores of between 11–30 on bilateral first permanent mandibular molar teeth and having fissure caries, were chosen for the study because the carious depth was limited to the enamel stage.
In the present study, contrary to other similar studies,5,25 the treatment and control lesions were designed to be the same individual and bilaterally because changes in treated lesions are not expected to occur regularly in different individuals and in different teeth. This paper suggests that remineralization in-vivo can be achieved with ozone when the correct oral conditions exist. This finding is related to the findings of other clinical studies about the remineralization of early carious lesions.12,27 Furthermore, no previous clinical study has evaluated the combined use of remineralizing solution and ozone therapy. Therefore, we considered the efficiency of gaseous ozone alone, as well as with ozone followed by a remineralizing solution. It is an interesting finding that neither test group revealed significant difference for the remineralization degrees of experimental teeth. Within the study period, for the 40-sec ozone application group, 90% of fissure carious lesions remineralized, whereas 95% remineralized in the second group. This finding is similar to the opinion of Featherstone15 that with good oral hygiene, saliva contains all the bio-available mineral components required for the remineralization process. In this study the only difference between the groups occurred for the control teeth. This result may be due to the monthly remineralizing solution application; the increased salivary buffer capacity may have had a protective effect on the control teeth of the second test group.
However, it was not possible to detect the CSI improvement or deterioration except for the control teeth in the first test group. The percentage of control teeth in which the CSI scores increased was significantly different for this group. The explanation may be that the only protective factor was oral hygiene, and within the study period the increased demineralization became clinically visible for this group.
Hogoson et al30 revealed that it is important to make the individual aware of his or her own power of maintaining good dental health without participation of the dental profession except for giving advice. Likewise, traditional oral hygiene motivation is the main thought in preventive dentistry. In this connection it is interesting to find that ozone application with regular oral hygiene education had an influence on oral hygiene motivation, and both of the groups showed improved oral hygiene status within the study period compared to the baseline. Similar to the study of Tan et al31 the current study noted that often recall visits and recurrent hygiene education are the most effective motivators in terms of oral hygiene.
It should be noted that with improved oral hygiene, repeated ozone applications in combination with additional remineralizing solution might serve to further improve the outcome of treatment described in the study. Therefore, further in-vivo and in-vitro studies are needed in which more standardized clinical situations are created.
CONCLUSIONS
Ozone application, either alone or with a remineralizing solution, is an effective method for caries reversal. Furthermore the present results have shown that remineralization in-vivo can be achieved through ozone therapy alone with the help of correct oral conditions. This painless preventive method can have an influence on remineralization through increased salivary mineral concentration.
REFERENCES
- 1.Müller P, Guggenheim B, Schmidlin PR. Efficacy of gasiform ozone and photodynamic therapy on a multispecies oral biofilm in vitro. Eur J Oral Sci. 2007;115:77–80. doi: 10.1111/j.1600-0722.2007.00418.x. [DOI] [PubMed] [Google Scholar]
- 2.Murdoch-Kinch CA. Minimal invasive dentistry. J Am Dent Assoc. 2003;134:87–95. doi: 10.14219/jada.archive.2003.0021. [DOI] [PubMed] [Google Scholar]
- 3.Featherstone JD. The science and practice of caries prevention. J Am Dent Assoc. 2000;131:887–899. doi: 10.14219/jada.archive.2000.0307. [DOI] [PubMed] [Google Scholar]
- 4.Baysan A, Lynch E. Effect of ozone on the oral microbiota and clinical severity of primary root caries. Am J Dent. 2004;17:56–60. [PubMed] [Google Scholar]
- 5.Huth KC, Paschos E, Brand K, Hickel R. Effect of ozone on non-cavitated fissure carious lesions in permanent molars. A controlled prospective clinical study. Am J Dent. 2005;18:223–228. [PubMed] [Google Scholar]
- 6.Nogales CG, Ferrari PH, Kantorovich EO, Lage-Marques JL. Ozone therapy in medicine and dentistry. J Contemp Dent Pract. 2008;9:75–84. [PubMed] [Google Scholar]
- 7.Dähnhardt JE, Jaeggi T, Lussi A. Treating open carious lesions in anxious children with ozone. A prospective controlled clinical study. Am J Dent. 2006;19:267–270. [PubMed] [Google Scholar]
- 8.Nagayoshi M, Kitamura C, Fukuizumi T, Nishihara T, Terashita M. Antimicrobial effect of ozonated water on bacteria invading dentinal tubules. J Endod. 2004;30:778–781. doi: 10.1097/00004770-200411000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Oizumi M, Suzuki T, Uchida M, Furuya J, Okamoto Y. In-vitro testing of a denture cleaning method using ozone. J Med Dent Sci. 1998;45:135–139. [PubMed] [Google Scholar]
- 10.Baysan A, Beighton D. Assessment of the ozone-mediated killing of bacteria in infected dentine associated with non-cavitated occlusal carious lesions. Caries Res. 2007;41:337–341. doi: 10.1159/000104790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Velano HE, do Nascimento LC, de Barros LM, Panzeri H. In vitro assessment of antibacterial activity of ozonized water against Staphylococcus aureus. Pesqui Odontol Bras. 2001;15:18–22. doi: 10.1590/s1517-74912001000100004. [DOI] [PubMed] [Google Scholar]
- 12.Baysan A, Whiley RA, Lynch E. Antimicrobial effect of a novel ozone- generating device on micro-organisms associated with primary root carious lesions in vitro. Caries Res. 2000;34:498–501. doi: 10.1159/000016630. [DOI] [PubMed] [Google Scholar]
- 13.Lynch E. Antimicrobial management of primary root carious lesions: a review. Gerodontology. 1996;13:118–129. doi: 10.1111/j.1741-2358.1996.tb00163.x. [DOI] [PubMed] [Google Scholar]
- 14.Ekstrand KR, Ricketts DNJ, Kidd EAM, Ovist V, Schou S. Detection, diagnosis, monitoring and logical treatment of occlusal caries in relation to lesion activity and severity: an in vivo examination with histological validation. Caries Res. 1998;32:247–254. doi: 10.1159/000016460. [DOI] [PubMed] [Google Scholar]
- 15.Featherstone JD. Caries prevention and reversal based on the caries balance. Pediatr Dent. 2006;28:128–132. discussion 192–198. [PubMed] [Google Scholar]
- 16.Loesche WJ. Role of Streptococcus mutans in human dental decay. Microbiol Rev. 1986;50:353–380. doi: 10.1128/mr.50.4.353-380.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.ten Cate JM, Featherstone JD. Mechanistic aspects of the interactions between fluoride and dental enamel. Crit Rev Oral Biol Med. 1991;2:283–296. doi: 10.1177/10454411910020030101. [DOI] [PubMed] [Google Scholar]
- 18.Lamkin MS, Oppenheim FG. Structural features of salivary function. Crit Rev Oral Biol Med. 1993;4:251–259. doi: 10.1177/10454411930040030101. [DOI] [PubMed] [Google Scholar]
- 19.Lynch H, Milgrom P. Xylitol and dental caries: an overview for clinicians. J Calif Dent Assoc. 2003;31:205–209. [PubMed] [Google Scholar]
- 20.Featherstone JD, Gansky SA, Hoover CI. A randomized clinical trial of caries management by risk assessment. Caries Res. 2005;39:295. doi: 10.1159/000337241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yamayoshi T, Tatsumi N. Microbicidal effects of ozone solution on methicillin-resistant Staphylococcus aureus. Drugs Exp Clin Res. 1993;19:59–64. [PubMed] [Google Scholar]
- 22.Hems RS, Gulabivala K, Ng YL, Ready D, Spratt DA. An in vitro evaluation of the ability of ozone to kill a strain of Enterococcus faecalis. Int Endod J. 2005;38:22–29. doi: 10.1111/j.1365-2591.2004.00891.x. [DOI] [PubMed] [Google Scholar]
- 23.Sechi LA, Lezcano I, Nunez N, Espim M, Duprè I, Pinna A, Molicotti P, Fadda G, Zanetti S. Antibacterial activity of ozonized sunflower oil (Oleozon) J Appl Microbiol. 2001;90:279–284. doi: 10.1046/j.1365-2672.2001.01235.x. [DOI] [PubMed] [Google Scholar]
- 24.Cardoso MG, de Oliveira LD, Koga-Ito CY, Jorge AO. Effectiveness of ozonated water on Candida albicans, Enterococcus faecalis, and endotoxins in root canals. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:e85–91. doi: 10.1016/j.tripleo.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 25.Baysan A, Lynch E. The use of ozone in dentistry and medicine. Part 2. Ozone and root caries. Prim Dent Care. 2006;13:37–41. doi: 10.1308/135576106775193897. [DOI] [PubMed] [Google Scholar]
- 26.Baysan A, Lynch E, Grootveld M. The use of ozone for the management of primary root carious lesions. Tissue preservation and caries treatment. Quintessence Book. 2001;3:49–67. [Google Scholar]
- 27.Hodson N, Dunne SM. Using ozone to treat dental caries. J Esthet Restor Dent. 2007;19:303–305. doi: 10.1111/j.1708-8240.2007.00127.x. [DOI] [PubMed] [Google Scholar]
- 28.Kramer PF, Zelante F, Simionato MR. The immediate and long-term effects of invasive and noninvasive pit and fissure sealing techniques on the microflora in occlusal fissures of human teeth. Pediatr Dent. 1993;15:108–112. [PubMed] [Google Scholar]
- 29.Theilade E, Fejerskov O, Migasena K, Prachyabrued W. Effect of fissure sealing on the microflora in occlusal fissures of human teeth. Arch Oral Biol. 1977;22:251–259. doi: 10.1016/0003-9969(77)90110-8. [DOI] [PubMed] [Google Scholar]
- 30.Hugoson A, Lundgren D, Asklöw B, Borgklint G. Effect of three different dental health preventive programmes on young adult individuals: a randomized, blinded, parallel group, controlled evaluation of oral hygiene behaviour on plaque and gingivitis. J Clin Periodontol. 2007;34:407–415. doi: 10.1111/j.1600-051X.2007.001069.x. [DOI] [PubMed] [Google Scholar]
- 31.Tan HH, Ruiter E, Verhey H. Effects of repeated dental health care education on gingival health, knowledge, attitude, behavior and perception. Community Dent Oral Epidemiol. 1981;9:15–21. doi: 10.1111/j.1600-0528.1981.tb01022.x. [DOI] [PubMed] [Google Scholar]