Abstract
This paper unpacks the slippery slope argument as it pertains to assisted death.
The assisted-death regimes of the Netherlands, Belgium, Luxembourg, Switzerland, and the states of Washington and Oregon are discussed and examined with respect to the slippery slope analytical rubric. In addition to providing a preliminary explanation of how the slippery slope argument has been academically defined and constructed, the paper examines assisted-death models from the perspective of considering what might exist at the top and at the bottom of the slippery slope. It also explores the nature and scope of safeguards implemented to avoid slippage, and shows that what lies at the top and bottom of the slippery slope may be different from jurisdiction to jurisdiction. After identifying some of the recent concerns that have arisen within each of the jurisdictions (concerns that might be viewed by some as evidence of slide), the paper concludes by making note of certain critical issues in the current assisted-death debate that merit deeper examination.
KEY WORDS: Slippery slope, euthanasia, pas, assisted suicide, assisted death, right to die, Netherlands, Belgium, Luxembourg, Canada
1. INTRODUCTION
While some might suggest that “it goes without saying” that the assisted-death debate is complex, it should nonetheless be said and furthermore bears repeating: the assisted-death discussion is inordinately complex. This state of complexity needs to be accepted and soberly reflected upon. There is no one simple solution or obvious panacea. There will be repercussions and consequences regardless of the legal path or paths taken. As put by Eugene Volokh, “[E]very decision changes the political, economic and psychological conditions under which future decisions are made” 1.
The first objective of this brief discussion is to explain some of the key features of the assisted-death schemes of the Netherlands, Belgium, Luxembourg, Switzerland, and the states of Washington and Oregon. The purpose of the explanation is to begin to identify the variations in the schemes. Taking note of those variations can assist in increasing the analytical accuracy of the application of the slippery slope rubric to the matter of assisted death.
The second objective of this discussion is to provide a succinct explanation of how the slippery slope argument has been academically defined and constructed. The primary purpose here is to provoke contemplation of the assisted-death schemes from the perspective of what might be understood to exist at the top and at the bottom of the slope, which in turn allows for a better understanding of the nature and scope of any safeguards implemented to avoid slippage. The paper then shows that what lies at the top and bottom of the slippery slope may be different from jurisdiction to jurisdiction.
The discussion goes on to identify some of the recent developments that have been asserted to be evidence of slide. Given that the present work is very much a first exploration, the discussion does not offer a slippery slope analysis of those particular developments, leaving the reader to form a personal opinion about whether slippage can indeed be perceived and to discern the potential value in the development of a more complex slippery slope analytic. The discussion concludes by making note of some of the critical issues in the current assisted-death debate that merit deeper examination.
2. AT THE TOP OF THE SLOPE: CURRENT ASSISTED-DEATH LAWS
2.1. Definitions
I use the term “assisted death” because it would be inaccurate to use the term “assisted dying” in the current Canadian debate. Not all jurisdictions being relied upon for experiential evidence to support or oppose assisted-death legalization restrict “euthanasia” (lethal injection upon the voluntary request of the patient)a or “physician-assisted suicide” (pas—the provision of a pharmaceutical prescription to the patient for self-administration) to “dying” individuals—namely, individuals in the terminal phase of an illness or whose illness is expected to end in death.
2.2. Netherlands, Belgium, and Luxembourg
The Netherlands, Belgium, and Luxembourg laws (respectively in force in the years 2002 2, 2002 3, and 2009 4)—the “Benelux laws”—all permit euthanasia or pas for somatic (physical) or non-somatic (non-physical—for example, psychiatric, mental, or emotional) suffering that is unbearable, lasting, and with no other reasonable solutionb. Thus, the key to euthanasia access in those jurisdictions aligns more with the concept of “suffering” (physical or non-physical) and less with the concept of “dying.” Put another way, dying, as we in Canada might understand the word in its strict physical sense, is not a prerequisite for access to euthanasia under any of the Benelux laws.
This is not to say that any form of suffering will suffice under the Benelux laws, because requisite suffering must be rooted in a medical conditionc. On the other hand, the requirement of suffering as a precondition to euthanasia has the potential for fairly broad interpretation because of additional factors that serve to qualify how the suffering requirement operates in practice:
“Unbearable” suffering is to be determined from the patient’s perspectived.
Suffering can arise as a result of a combination of medical conditions.
While there must be no other reasonable solution, it is always open to a patient to refuse medical treatment, and symptom relief is to be assessed from the patient’s perspective of what is reasonablee.
Suffering can be prospective or anticipatory—that is, it can include fear of future suffering related to personal deterioration, immobility, dependency, suffocation, loss of dignity, and so forth 9.
Future suffering can be addressed by the patient in an advance directivef.
Accordingly, euthanasia can legally be provided to individuals who anticipate unbearable suffering in the future and to patients who are unconscious (Netherlands, Belgium, and Luxembourg) or incompetent (Netherlands only), but who have made their wishes known in advance while still conscious and competentg. In other words, patient consciousness does not always have to coincide temporally with the provision of euthanasia nor does unbearable suffering always have to fully manifest.
For conscious patients, in addition to ensuring competency and voluntariness as part of the due care requirements, the treating physician must, under the Netherlands law, consult with at least one other independent physician who has seen the patient and provided an opinion on the patient’s suffering and their conviction that there is no other reasonable solutionh. The Belgian and Luxembourg laws also expressly mandate that the consulting physician be independent of both the treating physician and the patient, and be competent to give an opinion on the disorder in questioni. The Belgian law further imposes a third consultation for conscious patients “not expected to die in the near future”j—that is, patients with neurologic conditions such as quadriplegia or other conditions that can elicit fear of future suffering. In those situations, a second consulting physician (in addition to the treating physician and the first consulting physician) must examine the patient to ascertain voluntariness and the existence of persistent unbearable sufferingk. For unconscious patients who have requested euthanasia pursuant to an advance directive in Belgium and Luxembourg, the treating physician, before performing euthanasia, must consult another physician who is to confirm the irreversibility of the patient’s conditionl.
In the Netherlands, patients with a mental illness or disorder such as depression or dementia can also receive assistance as long as they are decisionally competent and have made a voluntary, well-considered request. In those situations, the physician is required to proceed with great caution, and in addition to the independent physician, should consult one or more experts, including a psychiatristm.
Under the Netherlands law, so long as parents or guardians have been involved in the decision process, minors between 16 and 18 years of age can direct assisted death; for minors between 12 and 16 years of age, the parent or guardian must agree with the decision for assisted deathn. Under the Belgian law, the patient must have reached the “age of majority” or be an “emancipated minor”o. Of the Benelux laws, only the Luxembourg law currently requires that a patient be an adultp.
It should be noted that, distinct from the Netherlands 2002 assisted-death law, the Netherlands also established a protocol for addressing the suffering of critically ill or disabled newborn infants. In 2005, the “Groningen Protocol” was adopted for national use by the Dutch Paediatrics Association, and the government soon after established a national review committee to advise prosecutorial authorities on these cases. Paediatricians may not be prosecuted for euthanasia performed on a newborn if reporting procedures are complied with and if certain criteria are met, including certainty of diagnosis and prognosis, parental consent, and confirmation of hopeless and unbearable suffering. Under the Groningen Protocol 11, the groups of infants for whom euthanasia might be considered are
infants with no chance of survival (will die soon after birth despite optimal care).
infants with a minimal chance of survival beyond the period of intensive treatment, and if they can survive, have an extremely poor prognosis and poor quality of life.
infants not dependent on intensive treatment, but with a hopeless prognosis in which a very poor quality of life is anticipated and is associated with sustained unbearable suffering in the judgment of the parents and medical experts.
Of the Benelux countries, the Netherlands was not only the first jurisdiction to pass assisted-death legislation, but also a jurisdiction with a lengthy history in the practice before it created express legislation. The legal concept was rooted in a professional conflict of duties: the physician’s duty to protect life versus the duty to relieve suffering. Out of that conflict emerged a defence that, in certain circumstances, a physician could be in a position of “overmacht” and, out of necessity, would have to choose a course of action. In those circumstances, euthanasia could be legally justified 12. Because of this underpinning, there is no distinction to be made between the physician choosing euthanasia or assisted suicide. Furthermore, the conflict-of-duties foundation anchors the perspective taken by the Netherlands that euthanasia is a “last resort” measure. The Dutch Medical Association (the knmg) recently and firmly reiterated that the assisted-death law in the Netherlands is established upon the medical conflict of duties and emphasizes that it is an “exceptional” medical procedure that will never become “standard”q.
Also significant is that the Netherlands law evolved from medical community participation; the laws of Belgium and Luxembourg did not. Despite being modeled on the Netherlands law, the assisted-death laws of Belgium and Luxembourg were largely advanced on a rights-based platform 13,14 and were met with degrees of resistance by the respective medical professional bodies in those countries 15,16. The Belgian Deontological Code was later changed to incorporate the legalization of euthanasia after the Belgian law passed in 2002, but the Code of Medical Ethics of Luxembourg’s Collège Médical has not yet been amended and continues to prohibit the practices of euthanasia and assisted suicide 17.
2.3. Oregon and Washington States
The Death with Dignity acts in the states of Oregon and Washington went into full force in the years 1997r and 2008 19 respectively. Evolving from a patient’s “right to die” discourse and legal historys, these American states have taken a different and narrower approach to regulating assisted death. Under the Oregon and Washington laws, only adult patients (18 years of age and older) who have been diagnosed with a terminal disease (incurable and irreversible disease that will produce death within 6 months) gain access to assisted death, and in that event, only pas—and not euthanasia—is permitted. In other words, in Oregon and Washington, persons with 6 or less months to live may request a prescription for lethal medication for purposes of self-administrationt. There is no requirement under either law for an assessment of suffering, nor is pas available for chronic or anticipatory suffering falling outside a 6-month terminal diagnosis.
Under the American laws, the prescribing physician must ensure that the patient is capable and is making a voluntary request. Additionally, the prescribing physician must refer the patient to a consulting physician for confirmation of diagnosis as well as for capacity and voluntarinessu. Although not required to be independent, the consulting physician must be qualified by specialty or experience to make a professional diagnosis and prognosis of the patient’s diseasev. If either the prescribing or the consulting physician believes that the patient suffers from depression or another psychiatric or psychological disorder causing impaired judgment, the patient must be referred for counselling, and no medication may be prescribed unless a determination in the negative is madew. As with the Code of Medical Ethics of Luxembourg’s Collège Médical the American Medical Association Code of Ethics continues to view pas as “fundamentally incompatible with the physician’s role as healer” 23.
2.4. Switzerland
Switzerland also allows only assisted suicide and not euthanasia. However, unlike the other jurisdictions discussed, Switzerland’s tolerance of assisted death arises from a very old penal code provision that punishes suicide assistance only if it is done for “selfish” reasons 24. Thus if it is done for “unselfish” reasons, assisted suicide is not a punishable offence. That provision has allowed the practice of assisted suicide to be developed by Swiss right-to-die organizations and furthermore does not technically restrict the practice to physicians nor impose any requirement that a particular illness or medical condition be present in the requesting individual. That said, the practice and scope of assisted suicide by Swiss right-to-die organizations is constrained and regulated through, among other things, internal guidelines of right-to-die organizations, formal agreements between organizations and local governmentsx, and the standardized use of lethal barbiturates, which, pursuant to Swiss narcotics laws, requires a medical prescription 26,27, thus triggering physician involvement.
Historically, pas has been discouraged by the Swiss Academy of Medical Sciences on the basis that assisted suicide is not part of a physician’s activities because it contradicts the aim of medicine. Academy guidelines do identify that, although there is no duty to assist suicide, a physician has a duty to take a patient’s wishes into account. Thus, while a physician is not obligated to assist, the physician who chooses to assist must confirm a terminal diagnosis (death within days or weeks), discuss alternatives, and confirm capacity and voluntariness. The final step must always be taken by the patient 28.
Participation by nonresidents of Switzerland, particularly by those without terminal illness, has prompted much international criticism of the Swiss scheme and in turn provoked heated debate and consideration by the Swiss state, either to ban organized assisted suicide altogether or to better regulate the practices of Swiss right-to-die organizations. In rejecting proposed reform options, the present minister of Justice has described the existing legislation as sufficient for addressing any abuses and has stated that the Swiss government will instead take measures to boost palliative care and suicide prevention, which are said to be aimed at “strengthening the right of self-determination to one’s dying day” 29.
2.5. Palliative Care
Palliative care measures have also been implemented in the jurisdictions that have proceeded with assisted-death legislation. Belgium and Luxembourg both passed palliative care laws establishing a right to palliative care simultaneously with their respective assisted-death laws 30,31. Oregon has not established a right to palliative care, but improvements to palliative care services have been observed and include improvements to physician training, pain management, and hospice referrals, as well as an increase in the number of deaths taking place at home 32,33. On the other hand, questions have been raised regarding the adequacy of health care coverage and access to medications 34.
2.6. Right to Refuse to Assist
Under all the laws so far discussed, there is no positive right to assisted death. Physicians have the right to refuse to provide assisted death.
3. DEFINING THE SLIPPERY SLOPE
When the foregoing details are viewed collectively, the following generalizations or observations about the assisted-death laws can be made:
There is no one accepted assisted-death model.
-
Although there is no positive right to assisted death, assisted death has been justified pursuant to a variety of concepts including
physician conflict of duties and necessity,
dignity,
relief of suffering,
autonomy, and
self-determination.
-
Through varied means, justifications, and logic, euthanasia and assisted suicide have been made available to individuals who
have terminal or non-terminal conditions,
have physical or nonphysical illnesses,
are conscious or unconscious,
have competence or incompetence, or
have reached or not reached adulthood.
Physicians and physician organizations are not unanimous in their support of assisted-death practice, and yet they are the members of the one profession advanced as the most appropriate to conduct the practice.
-
Palliative care and assisted death are analytically connected. Palliative care may have been expanded or improved by a state
to counter the effects of assisted-death legalization.
as part of an improved spectrum of patient care that includes assisted death.
in lieu of expanding assisted-death regulation.
Whether this list of observations provides an appropriate platform from which to begin to frame—or for that matter, to refute—a slippery slope argument to a large extent depends on what have been identified as point A (the top of the slope and the decision sought to be implemented) and point B (the bottom of the slope and the outcome sought to be avoided; Figure 1).
FIGURE 1.
The basic slippery slope.
If point A is to permit physicians to provide euthanasia at the voluntary request of patients who are suffering unbearably (which is essentially point A under the Benelux laws), then the identification of point B must be something other than the practice of euthanasia for non-terminal illness, because that is included in point A. In a slippery slope argument, B cannot equal A; rather, B is what potentially follows from the implementation of A. Thus, in this case, B might be identified as euthanasia for individuals who are non-voluntary (those who are unable to consent) or involuntary (those who do not consent). If B is identified in this manner, then safeguards can be put in place to ensure that the individual is capable, informed, and acting voluntarily when expressing the request to die.
However, point A in a subsequent jurisdiction might be to allow pas for voluntary and capable patients with terminal conditions—that is, expected to die within the near future (which is essentially point A under the Oregon and Washington state models). Point B might then be identified as including the practice of euthanasia and the practice of assisted suicide for non-terminal conditions in addition to involuntary and non-voluntary assisted death. This latter jurisdiction can benefit from the experiences of the previous jurisdiction, being able to model and more confidently rely on safeguards that have a proven record of being able to better ensure, for example, the competency and voluntariness of the patient.
What must still be addressed, however, are the safeguards required to prevent slippage toward euthanasia practice or expansion beyond terminal diagnosis, assuming that such extension continues to represent point B for the subsequent jurisdiction. Considerations here begin to descend into an analytical labyrinth, because the experiences of the jurisdiction proposed to be relied upon simultaneously reflect point B outcomes sought to be avoided. One principal question that this coincident position raises is whether certain elements of one scheme can be borrowed by the other without somehow setting up the conditions for the first to eventually play out in the second.
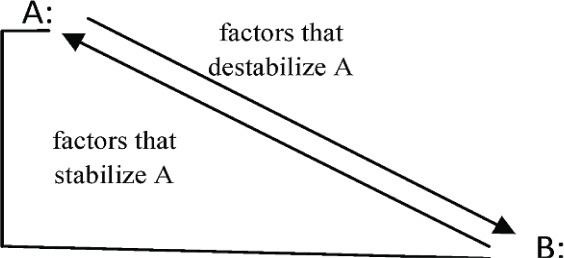
The nature of this inquiry remains of the slippery slope variety (“Will A lead to B?”), but is somewhat different from the first line of inquiry, which arguably works toward identifying positive factors that can prop up or stabilize a certain state of affairs (point A); this second line of inquiry seeks to identify factors that have the potential to topple or destabilize A, thus requiring a more thorough consideration of the various mechanisms that could cause a slide from A to B, as well as the likelihood of such a slide being set into motion (Figure 2).
FIGURE 2.
The mechanics of slide
Although a full analysis of the various theories for the mechanics and probability of a slide is beyond the scope of this brief discussion, a basic understanding of some of the ways in which the mechanics of the slippery slope have been academically organized can assist in gaining a better appreciation of the relevance and implications of the available empirical evidence as applied in arguments from either side of the assisted-death debate.
The slippery slope model most commonly discussed identifies two slopes. The first, the “logical” or “conceptual” slope “holds that we are logically committed to allow B once we have allowed A” 35—similar to a “floodgates” image perhaps, rather than a slope. The “psychological” or “empirical” slope holds that “the effect of accepting A will be that, as a result of psychological and social processes, we sooner or later will accept B” 35. Accordingly, if through logic or psychosocial processes A could lead to B, A should not be permitted. Or so the argument goes.
In the assisted-death debate, the logical slippery slope has been refuted on the basis that, if a logical distinction can be made between situations at the top and situations at the bottom, then the logical slope is not a valid argument against assisted death. The principles frequently asserted as being able to establish such a distinction are patient autonomy and free and informed consent. If access to assisted death is grounded on free and informed consent of the individual, for example, then there can be no slide from voluntary to involuntary death 36, assuming that involuntary death lies at position B.
The empirical or psychological slippery slope, which involves consideration of psychosocial processes, has also been described as a form of desensitization 37. Another common approach to defining the empirical slope has been to describe it by reference to how it differs from the logical slope. Under this approach, the empirical slope is defined as what people will “actually” think is permissible given the prior belief or activity, as opposed to the attitudes people might cultivate as a result of mental exercises in logical reasoning.
A major criticism of empirical slippery slope arguments is that, even when psychosocial arguments focus on probabilities and predictions for slippage, they are too often asserted as certainties 37. Additionally, proponents of assisted-death legalization argue that, as in the logical slippery slope, institutional safeguards can be made sufficient to avoid psychosocial slippage. Institutional safeguards here might include (for example) watchdog institutions and public education 38.
Eugene Volokh has taken a more analytically robust approach to the slippery slope model generally by concentrating on how the slope actually operates and identifying “mechanisms” that could potentially prompt a shift from A to B 39. According to Volokh, these mechanisms are gradual or sudden processes that involve, among other things, logical reasoning, judicial analysis, judicial decisions, and legislation 39. If applied in the assisted-death context, it can be observed that the logical slope or “logic mechanism” would be only one of several mechanisms that could potentially provoke a slide. It should be kept in mind that the task of identifying potential mechanisms of slide is a task distinct from the equally difficult task of evaluating the probability or likelihood of slide via the mechanisms identified.
One example of a slippage mechanism described by Volokh is what he calls the “equality slippery slope.” According to Volokh, the equality mechanism operates to include what is perceived to be the more extreme option (point B) along with the more moderate option (point A) on the basis that B is less discriminatory than A. An illustration of this mechanism in operation can be detected in a 2010 Swiss discussion concerning the possibility of increased regulation of organized assisted suicide. In that discussion, a provision that would make assisted suicide “the preserve of terminally ill patients” was described as “discriminatory and unlawful” 40.
A similar potential equality criticism (and thus potential mechanism of slide) could be made of the Oregon and Washington state laws: that is, that by restricting access to those with a terminal illness, the laws are discriminatory. Thus, contemplation of the American laws appears to indicate that something other than “voluntary and informed consent” will be required if a distinction between A (assisted death for terminal diagnosis) and B (assisted death for non-terminal diagnosis) is sought to be maintained in the future.
The overall point here is that, as a tool for analysis, the slippery slope paradigm in its current forms is academically and practically imperfect. The more theoretical versions of this model—that is, the ones that delineate somewhat clumsily between the logical and psychological slopes—do not satisfy lines of inquiry aimed at addressing the processes of sociopolitical change in society. More practical versions, such as those that might evolve from Volokh’s initial work on mechanisms and probabilities of slippage, offer more potential to respond to those kinds of inquiries, but such models have not yet been developed or fully explored with respect to the assisted-death controversy. Additionally, some might argue that pursuing such a detailed exercise may in any event become so overly complex as to make it irrelevant and inadequate for resolving the dilemma at hand.
Regardless, it is nonetheless necessary to understand the essence of the slippery slope argument to be able to tease out and appreciate the different strands of assisted-death argumentation. It also assists in pushing for a more precise articulation of the decision sought to be implemented (point A) and the outcomes sought to be avoided (point B), and thereby also challenges the processes through which decisions and outcomes are respectively ascertained and identified.
Thinking in terms of the slippery slope also draws attention to how A might be justified on a number of different grounds and that each of those grounds possesses greater or lesser potential to form the basis of arguments in support of B. Further, it demonstrates that even though the mechanisms chosen to stabilize A might be similar, it does not follow that A and B themselves are also similar between different jurisdictions, thus requiring, among other things, diligence with respect to the use and manipulation of data across jurisdictional lines.
Debate pursuant to a slippery slope framework may or may not presuppose the existence of A, but what is arguably more significant is its unrealized potential to stimulate broad discussion and to assist in finding areas of common accord.
4. CONVERSATIONS ABOUT THE BOTTOM
Against the foregoing, a few of the live issues that have been asserted, analyzed, or critiqued via the slippery slope lexicon are now briefly described. In the discussion, those issues are set out within their domestic context and are not critiqued from a cross- or inter-jurisdictional perspective with respect to the slippery slope.
4.1. The Netherlands
“Tired of life” (also known as “completed life” or “finished with life”) is a significant issue in the Netherlands and has been largely provoked by intense lobbying from a citizen’s action group, Uit Vrije Wil (“Of one’s own free will”) 41. According to the knmg, the issue of senior citizens (70 years of age or older) with a wish to end their lives is on the Dutch public and political agenda. The knmg has indicated that the “finished with life” initiative opens up a “second road to euthanasia and thereby undermines the existing Euthanasia law” 6. However, the knmg noted that “[i]t is hardly conceivable that physicians would not have a role when seniors voice a serious wish to die, even where this wish stems from the sense of having a completed life” 6. The knmg also described how physicians will be confronted, more than ever before, with fragile individuals of advanced age and multimorbidity (the latter of which significantly increases depression and, in turn, vulnerability), all of which can lead to unbearable and lasting suffering 6. According to the knmg, the sum of this “non-linear equation” and the complexity of what are usually “non-fatal afflictions” potentially create suffering sufficiently linked to the medical domain, thereby allowing a physician to act within the current law 6. Suffering with no medical basis will, however, continue to fall outside the scope and expertise of medicine and therefore outside the current euthanasia law. The knmg has nonetheless recommended a thorough and comprehensive analysis of this issue 42.
The 2010 report of the Dutch Regional Euthanasia Review Committees, tasked with reviewing notifications of assisted death under the Dutch law, noted a “sharp increase” of 19% in the number of notifications to 3136 in 2010 from 2636 in 2009. Starting in 2003, previous years demonstrated only a 10% increase in notifications from year to year 10. Some analysts attribute the increase to overall improved physician reporting, but the 2010 Review Committees report states that the cause of the continuing increase is “not known” 10. Evaluation of the rise is ongoing.
The Dutch 2010 report notes 2910 cases of euthanasia, 182 cases of assisted suicide, and 44 cases involving a combination of both [3136 cases total (2.3 per 1000 deaths)]. Cancer was the primary condition involved (2548 cases) 10. In 2010, the Review Committees reached conclusions on 2667 of the 3136 notifications, finding 9 cases in which physicians did not meet the due care criteria. Of those 9 cases, 5 related to the way in which euthanasia or assisted suicide was performed. In all notifications reviewed, it was found that suffering was connected with a recognized disease or disorder, with 2 notifications being connected with a mental illness or disorder 10. The Dutch 2010 report also emphasized the importance of a physician remaining with the patient or in the immediate vicinity until death, whether pursuant to euthanasia or pas 10.
4.2. Belgium
Belgium’s “tired of life” discussion has been ongoing since at least 2009, when a 93-year-old woman went on a hunger strike to hasten her own death after her request for euthanasia was refused. Her request was eventually granted 43. The “tired of life” discussion in the Belgian context similarly involves consideration of the physical forms of suffering arising out of age-related, but not necessarily fatal, medical conditions 7.
The Belgian Commission on the Control and Evaluation of the Law on Euthanasia reports an increase in reported assisted-death cases (euthanasia and pas), from 259 in 2002–2003 (0.2% of all deaths) to 924 in 2006–2007 (0.36% of all deaths) and to 1526 in 2008–2009 (0.7% of all deaths) 7. The increases are generally attributed to increased physician awareness of the law, but concerns about physician underreporting have also been raised, with a 2007 study finding that the incidence of euthanasia in 2007 was closer to 1.9% of all deaths 44.
A great preponderance of euthanasia deaths in Belgium are cancer-related (approximately 80%) 7. From 2008 to 2009, 36 cases of euthanasia (3% of the total) were performed on irreversibly unconscious patients on the basis of advance declarations. That number is slightly higher than those published in previous Commission reports 7. To date, no physician has been prosecuted under the Belgian law.
The issue of euthanasia for minors is a contested issue in Belgium 45–47. Bills contemplating an expansion of the law to include euthanasia for minors (in a manner somewhat similar to that provided for in the Netherlands) have been introduced in the Belgian legislature and senate since 2004y. Bills have also been introduced seeking to extend euthanasia to persons suffering from dementia pursuant to an advance declaration similar to the approach used in the Netherlandsz. Euthanasia by advance request under the Belgian law is currently available only to patients who are irreversibly unconscious 3. None of the bills related to minors or persons with dementia has been successful to date.
4.3. Luxembourg
The empirical information for Luxembourg is quite limited, with only 5 requests for euthanasia reported in 2009 and 2010 combined. All 5 cases involved cancer 48. By contrast, 681 end-of-life provisions were registered with the Luxembourg authority, with women being represented at 396 compared with 285 for men 48.
4.4. Switzerland
In March 2012, the Swiss authorities published the first official statistics on assisted suicide in Switzerland. According to the Federal Statistical Office, the number of Swiss residents who died from “assisted suicide” has “increased continuously” over the years 1998–2009. The Federal Statistical Office reported that, in 2009, approximately 300 assisted suicide deaths occurred [4.8 per 1000 deaths (0.48%)] compared with fewer than 50 deaths in 1998 49. For 2011, it has been independently reported that the right-to-die organization Exit assisted 416 deaths, up from approximately 348 deaths in 2010 50. The 2011 figure for nonresident deaths reported by the organization Dignitas was 149 51.
As described earlier, the Swiss state recently decided against introducing new regulatory measures; it is currently focusing its efforts on improving palliative care. However, discussions on assisted death are still ongoing. The matter of euthanasia is also part of that debate since the December 2010 acquittal of a physician who triggered a lethal drip based on the patient’s cue, a foot movement. The patient was suffering from amyotrophic lateral sclerosis (als) and had lost the ability to self-administer the medication because of a sudden deterioration in her condition. The court found that, in those circumstances, the doctor had a medical and moral duty to violate the law 52.
4.5. Oregon
The number of physician-assisted deaths under the 1994 Oregon law has gradually increased over the years to 71 during 2011 (22.5 of every 10,000 deaths) from 16 during 1998 (approximately 5 of every 10,000 deaths) 53. As of the end of 2011, a total of 935 end-of-life prescriptions had been written, and 596 patients had died from medication prescribed under the law 54. The most frequently cited end-of-life concerns in 2011 were loss of autonomy (88.7%), decreasing ability to participate in activities that make life enjoyable (90.1%), and loss of dignity (74.6%) 54. Concern over loss of autonomy and participation in enjoyable activities have both trended upward to 88.7% and 90.1% in 2011 from 75% and 69% in 1998 respectively 53–55. Inadequate pain control or concern about pain control are cited in 22.6% of the 596 total deaths to date 54.
Notwithstanding the overall trends between 1998 and 2011, from 2010 to 2011, concerns over loss of autonomy and lessened ability to participate in enjoyable activities both decreased: to 88.7% from 93.8% and to 90.1% from 93.8% respectively. Conversely, concern about burden on family, friends, or caregivers increased to 42.3% in 2011 from 26.2% in 2010. Inadequate pain control or concern about pain control also increased to 32.4% in 2011 from 15.4% in 2010 54,56.
Although most patients in 2011 were enrolled in hospice care at the time of death (96.7%), the number of prescribing physicians present at death trended downward to 8.5% in 2011 from the 1999 high of 48%. That finding has raised concern with respect to how complications arising upon ingestion of the lethal substance—such as regurgitation or otherwise failed ingestion—are addressed. Of the known cases, complications have been recorded in 3.7% of the 596 deaths under the Act thus far 54.
A further concern raised in Oregon is the possibility that, contrary to the Oregon law, patients with depression are receiving prescriptions for lethal medication. Suspicion has intensified because the number of requesting patients referred for psychiatric or psychological evaluation has continued to decline over time, to 1.5% in 2010 from 43.5% in 1999 55. A 2011 bill seeking to impose mandatory counselling for all individuals requesting a prescription for medication to end their lives died in committeeaa. That bill was considered by some proponents of assisted suicide to be an attempt to create barriers to “death with dignity” and designed to burden patients and physicians with needless procedures and paperwork 57.
During the years 1998–2010, patients with als have had the second highest rate of requests granted (8.0%) 54. That finding has led to some discussion about the ability of the Oregon assisted-death scheme to accommodate als patients, particularly when they have difficulty swallowing. To date, however, only oral medications have been prescribed under the legislation, and as already mentioned, physician presence at death has continued to trend downward, suggesting that the trend of prescribing oral medications will likely continue into the future. Unlike the Oregon law, the Washington law (discussed in more detail next) expressly defines “self-administer” as requiring ingestion of the medication. Cancer has consistently been the primary underlying condition for requests granted: 80.8% during 1998–2010 and 82.4% in 2011 54.
During the years 1998–2010, chronic lower respiratory disease was the underlying illness associated with the third-highest rate of requests granted (3.8%). However, in 2011, it had bypassed als to become the illness associated with the second-highest rate of requests granted at 7.4%; als ranked third, at 2.9% of requests granted 54.
4.6. Washington State
According to the Washington State Department of Health 2010 Death with Dignity Act Report, 87 people requested and received lethal doses of medication in 2010, and 72 individuals died (51 after ingestion, 15 without having ingested, 6 with ingestion status unknown). That number was slightly higher than in 2009, when 65 prescriptions and 63 deaths were reported 58.
As in Oregon, the primary end-of-life concerns of the 72 participants were recorded as loss of autonomy (90%), loss of ability to participate in enjoyable activities (87%), and loss of dignity (64%). Inadequate pain control or concern about pain control was a significantly lesser concern at 36%. Cancer was the primary underlying condition, accounting for 78% of deaths in 2010 and 79% of deaths in 2009. Neurodegenerative disease, including als was the second most common condition, accounting for 10% and 9% of deaths in 2010 and 2009 respectively. Psychological referrals declined to 3% in 2010 from 7% in 2009 58.
5. CONCLUDING COMMENTS
I hope that what has been conveyed by the foregoing discussion is an appreciation not only of how enormously complex assisted-death regulation is, but also of how experiential information from other jurisdictions can support advocacy on either side of the debate. Accordingly, depending on how experiential information is presented, it may not be very helpful in determining appropriate pathways forward, particularly as it concerns the identification of potential points A and their correlative points B on the slippery slope rubric.
On the other hand, I also hope to have conveyed a sense of how a slippery slope diagnostic can be used as a tool to provoke a robust and earnest discussion on point A possibilities which necessarily demands an equally comprehensive and open conversation on the matters that lurk at point B for all of a state’s citizens. These conversations are particularly relevant given that there is no single, obvious assisted-death template on which to model or rely, and that, among the current models, there does not appear to be any overall consensus on the description of point B.
Of additional significance is the need for sober thought, caution, clarity, and consistency in the identification and articulation of the potential legal grounds upon which assisted death (in whatever form) might be justified. The underlying justifications of assisted death are critical to securing boundaries or limits. As can be observed from the “tired of life” discussion in the Netherlands, justifications can later come to operate as mechanisms of stabilization or destabilization to earlier prescribed legal limits. Thus, a genuine debate over assisted death should also welcome and encourage dialogue that critiques the various pathways to legal reform and that examines the legislative, judicial, and political processes that have the potential to remove barriers between a proposal A and a possibility B.
A further issue in want of critical and comprehensive debate is that of the role of physicians. Although there is evidence to suggest that many physicians support assisted death, there is also evidence that not all professional medical bodies are in agreement on the matter. This professional disconnect requires further exploration, including, for example, ascertaining the scope and extent to which physicians may have formed their respective individual opinions on the basis of an appreciation of professional duties versus on the basis of personal political persuasion. From the Netherlands experience, it can be observed that assisted-death practice can indeed stem from an appreciation of professional duties to the patient; however, it remains that professional organizations in other jurisdictions continue to interpret otherwise, including the Canadian, British, Australian, and American medical associations 59–62. The ability of a given physician to refuse to participate in assisted death on the grounds of conscientious objection as a possible solution to the disconnect provides scarce insight into whether or how assisted death should be defined as a professional medical activity. And that stance will, in turn, carry additional consequences with respect to the scope and limits of future practices and health care policies.
To attempt to draw any conclusions with respect to the influence of palliative care on assisted death and vice versa would be, in the context of this discussion, a superficial exercise. It can, however, be asserted that palliative care and assisted death have numerous and varied intersections and that those intersections merit ongoing research and analysis. Further, while the relief of suffering appears to be the primary feature common to both palliative care and assisted death, it is readily observed based on the foregoing review that relief of suffering as a standalone principle does not assist in elucidating where the limits should lie. Even when relief of suffering is attached to the principles of free and informed consent, more is required in terms of how the scope and boundaries of assisted death are identified and maintained—the assisted-death laws of the states of Oregon and Washington serving as intriguing illustrations here.
In sum, when seeking pathways forward, although it is prudent to look to the experiences of other jurisdictions, it must also be kept in mind that such experiential evidence, while useful and profound, is not directly telling about whether or how to proceed in the matter of assisted-death reform.
6. ACKNOWLEDGMENTS
Thanks are owed to research assistant Keith Lenton, whose work was made possible through the generous support of the Centre on Aging, University of Manitoba, and to Dr. M. Michelle Gallant, Anne-Marie Brown rn mn, Dr. DeLloyd J. Guth, and the reviewers for their helpful comments.
Footnotes
In Western discussions, the term “euthanasia” is often qualified by the word “voluntary” as in “voluntary euthanasia” to identify the request and voluntariness of the individual. In European literature, the term “euthanasia” is widely understood to mean “termination of life upon request,” and thus from that perspective, use of the word “voluntary” before “euthanasia” is considered redundant.
Netherlands law 2, Art. 2.1.b, 2.1.d; Belgian law 3, Art. 3.1, 3.2; Luxembourg law 4, Art. 2.1, 2.2.
Dutch Medical Association 6, p. 20; Commission fédérale de contrôle et d’évaluation de l’application de la loi du 28 mai 2002 relative à l’euthanasie 7, p. 61; Ministry of Health and Ministry of Social Services, Luxembourg 8, p. 15.
Netherlands law 2, Art. 2.1.d; Commission fédérale de contrôle et d’évaluation de l’application de la loi du 28 mai 2002 relative à l’euthanasie 7, p. 61; Ministry of Health and Ministry of Social Services, Luxembourg 8, p. 15.
Netherlands law 2, Art. 2.1.e.
Belgian law 3, Art. 3.3.
Belgian law 3, Art. 3.3.1.
Regional Euthanasia Review Committees 10, p. 10-1.
Netherlands law 2, Art. 2.4.
Belgian law 3, Art. 3.1.
Luxembourg law 3, Art. 2.1.1.
knmg6, Preamble.
Oregon law 18, S. 127.800 to S. 127.89718.
See cases addressing the withdrawal or withholding of life support: In re Quinlan 20; Cruzan v Director, Missouri Department of Health 21. See also discussion on right-to-die organizations in Pratt 22, pp. 1029–32.
Oregon law 18, Art. 127.800 S. 1.01, Art. 127.800 S. 2.01; Washington law 19, S. 70.245.010 and S. 70.245.020.
See, for example, the Agreement on Organized Assisted Suicide 25.
S. 3-804/1, Proposition de loi modifiant la loi du 28 mai 2002 relative à l’euthanasie (July 7, 2004); Doc 51 2553/001, Proposition de Loi completant en ce qui concerne les mineurs, la loi du 28 mai 2002 relative à l’euthanasie (June 15, 2006); S. 4-920/1, Proposition de loi modifiant, en ce qui concerne les mineurs, l’article 3 de la loi du 28 mai 2002 relative à l’euthanasie (September 16, 2008); Doc 53 0496/001, Proposition de Loi completant en ce qui concerne les mineurs, la loi du 28 mai 2002 relative à l’euthanasie (October 28, 2010); Doc 5-179/1, Proposition de loi modifiant la loi du 28 mai 2002 relative à l’euthanasie, en ce qui concerne les mineurs âgés de quinze ans et plus; Doc 5-21/1, Proposition de loi modifiant la loi du 28 mai 2002 relative à l’euthanasie, en ce qui concerne les mineurs âgés de quinze ans et plus (August 16, 2010).
S. 4-676/1, Proposition de loi modifiant l’article 4 de la loi du 28 mai 2002 relative à l’euthanasie (April 8, 2008); Doc 53 0498/01, Proposition de loi modifiant la loi du 28 mai 2002 relative à l’euthanasie (October 28, 2010).
HR 2016, 76 Leg. (Or. 2011) [House Bill 2016, A Bill for an Act relating to the Oregon Death with Dignity Act; amending ORS 127.800, 127.815, 127.825, 127.855, and 127.865].
7. CONFLICT OF INTEREST DISCLOSURES
The author has no financial conflict of interest to declare.
8. REFERENCES
- 1.Harvard Law School. Home > Recent News and Spotlights > Eugene Volokh, of The Volokh Conspiracy, discusses slippery slope arguments [Web video] Cambridge, MA: The President and Fellows of Harvard College; 2011. [Available at: http://www.law.harvard.edu/news/2011/10/04_volokh-feldman-slippery-slope-arguments.html; cited April 20, 2012] [Google Scholar]
- 2.Netherlands. Termination of Life on Request and Assisted Suicide (Review Procedures) Act 2002. The Hague: Netherlands; 2002. [Available online at: http://www.eutanasia.ws/documentos/Leyes/Internacional/Holanda%20Ley%202002.pdf; cited April 20, 2012] [DOI] [PubMed] [Google Scholar]
- 3.The Belgian act on euthanasia of May, 28th 2002 [English translation] Ethical Perspect. 2002;9:182–8. doi: 10.2143/ep.9.2.503856. [Available online at: http://www.kuleuven.be/cbmer/viewpic.php?LAN=E&TABLE=DOCS&ID=23; cited April 20, 2012] [DOI] [PubMed] [Google Scholar]
- 4.Grand Duchy of Luxembourg . Memorial: Journal Officiel du Grand-Duché de Luxembourg. Recueil de legislation. Vol. 46. Luxembourg: Association momentanée Imprimerie Centrale/Victor Buck; 2009. Law of March 16, 2009, on euthanasia and assisted suicide [French] pp. 615–19. [Available online at: http://www.legilux.public.lu/leg/a/archives/2009/0046/a046.pdf#page=7; cited April 20, 2012] [Google Scholar]
- 5.Brongersma | Sutorius. Nederlandse Jurisprudentie 2003;167.
- 6.Dutch Medical Association (knmg) Position Paper: The Role of the Physician in the Voluntary Termination of Life. Utrecht, Netherlands: KNMG; 2011. [Dutch] [Download available at: http://www.knmg.nl/voluntary-termination-of-life; cited April 20, 2012] [Google Scholar]
- 7.Federal Commission on the Control and Evaluation of Euthanasia. Fourth Report to the Legislature (2008 and 2009) Brussels, Belgium: The Commission; 2010. Commission fédérale de contrôle et d’évaluation de l’application de la loi du 28 mai 2002 relative à l’euthanasie. [French] [Available online at: http://www.ieb-eib.org/nl/pdf/rapport-euthanasie.pdf; cited April 20, 2012] [Google Scholar]
- 8.Euthanasia and Assisted Suicide: Law of 16 March 2009. 25 Questions; 25 Answers. Luxembourg: Ministry of Health and Ministry of Social Services; 2010. [Available online at: http://www.sante.public.lu/publications/sante-fil-vie/fin-vie/euthanasie-assistance-suicide-25-questions-reponses/euthanasie-assistance-suicide-25-questions-reponses-en.pdf; cited April 20, 2012] [Google Scholar]
- 9.Public Prosecution Service, College of the Procurators-General . The Hague, Netherlands: Public Prosecution Service; 2003. Home > Organisation > Privacy > Policy Overview > Medical > Note Subsequent Decision on Euthanasia on Request (Euthanasia and Assisted Suicide) (2006A009) [Web page, Dutch] [Available at: http://www.om.nl/organisatie/beleidsregels/overzicht/medisch/@151338/aanwijzing/; cited April 20, 2012] [Google Scholar]
- 10.Regional Euthanasia Review Committees: Annual Report 2010. The Hague, Netherlands: The Regional Euthanasia Review Committees; 2011. [Available online at: http://www.rtde.eu/sites/default/files/JV%20RTE%202010%20ENGELS%20%28EU12.01%29_tcm52-30364-1.pdf; cited April 20, 2012] [Google Scholar]
- 11.Verhagen E, Sauer PJ. The Groningen protocol—euthanasia in severely ill newborns. N Engl J Med. 2005;352:959–62. doi: 10.1056/NEJMp058026. [DOI] [PubMed] [Google Scholar]
- 12.Schoonheim, Supreme Court, 27 November 1984. Nederlandse Jurisprudentie 1985;106.
- 13.Belgium. The Bridge to the Twenty-First Century—Coalition Agreement of July 7, 1999. Brussels, Belgium: Federal Government of Belgium; 1999. para 11. [Available online at: http://home.scarlet.be/~pin67548/Regeerakkoord.pdf; cited April 20, 2012] [Google Scholar]
- 14.Grand Duchy of Luxembourg. Proposition de loi sur le droit de mourir en dignité 1) Exposé des motifs 2) Texte de la proposition de loi 3) Commentaire des articles (J-2201-O-0277) 4909/00 (19 February 2002).
- 15.Deliens L, van der Wal G. The euthanasia law in Belgium and the Netherlands. Lancet. 2003;362:1239–40. doi: 10.1016/S0140-6736(03)14520-5. [“[N]o medical association supported the process in Belgium.”] [DOI] [PubMed] [Google Scholar]
- 16.College Medical of Luxembourg. Notice from the College Concerning the Proposed Law on the Right to Die in Dignity. Luxembourg: College Medical; 2002. [French] [Available online at: http://www.collegemedical.lu/opsmain/download/droitdemourirendignite.pdf; cited April 20, 2012] [Google Scholar]
- 17.Grand Duchy of Luxembourg. Memorial: Journal Officiel du Grand-Duché de Luxembourg. Recueil de legislation. Vol. 160. Luxembourg: Association momentanée Imprimerie Centrale/Victor Buck; 2005. Ministerial Order of 7 July 2005, approving the Code of Ethics of the medical and dental professions, issued by the College Medical [French]. Art. 40; p. 2761. [Available online at: http://www.legilux.public.lu/leg/a/archives/2005/0160/a160.pdf#page=2; cited April 20, 2012] [Google Scholar]
- 18.Oregon, Department of Human Services (dhs) Death with Dignity Act. Portland, OR: DHS; 2007. [Available online at: http://www.leg.state.or.us/ors/127.html; cited April 20, 2012] [Google Scholar]
- 19.Washington State. The Washington Death with Dignity Act. Olympia, WA: Washing State Legislature; 2009. RCW 70.245. [Available online at: http://apps.leg.wa.gov/RCW/default.aspx?cite=70.245; cited May 7, 2012] [Google Scholar]
- 20.In re Quinlan 355 A.2d 647 (NJ 1976).
- 21.Cruzan v Director, Missouri Department of Health, 497 U.S. 261(1990)
- 22.Pratt CA. Or L Rev. 1998. Efforts to legalize physician-assisted suicide in New York, Washington and Oregon: a contrast between judicial and initiative approaches—who should decide? pp. 1027–123. [Google Scholar]
- 23.American Medical Association (ama) Resources > Medical Ethics > AMA Code of Medical Ethics > Opinion 2.211 > Physician-Assisted Suicide [Web page] Chicago, IL: AMA; 1996. [Available at: http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion2211.page; cited April 20, 2012] [Google Scholar]
- 24.Switzerland. Swiss Penal Code [Swiss German] Berne: Switzerland; 2012. December 21, 1937 SR 757 (1938), Art. 115. [Translation available online at: http://www.admin.ch/ch/e/rs/3/311.0.en.pdf; cited April 20, 2012] [Google Scholar]
- 25.Ober staats anwalt schaft des Kantons Zurich (cz) and Exit Deutsch Schweiz (eds) Agreement on Organized Assisted Suicide [Swiss German] Zurich, Switzerland: CZ and EDS; 2009. [Available online at: http://www.sterbehilfedeutschland.de/sbgl/files/Medien/PDF%20neu/Vereinbarung%20Zuerich%20Brunner-Exit.pdf; cited April 20, 2012] [Google Scholar]
- 26.Switzerland. The Federal Law on Narcotic Drugs and Psychotropic Substances of October 3, 1951 (as at January 1, 2011) [Swiss French]. Art. 11-812.21. Berne: Switzerland; 2011. [Google Scholar]
- 27.Switzerland. The Federal Law of December 15, 2000, on Drugs and Medical Devices (Law on Therapeutic Products—LTP) (as at October 2010) [Swiss French]. Art. 26. Berne: Switzerland; 2011. [Google Scholar]
- 28.Swiss Academy of Medical Sciences (sams) Care of Patients in the End of Life. Basel, Switzerland: SAMS; 2004. p. 6. [Available for download at: http://www.samw.ch/en/Ethics/Guidelines/Currently-valid-guidelines.html; cited April 20, 2012] [Google Scholar]
- 29.Geiser U. Cabinet Rules Out New Suicide Legislation [Web article] Berne, Switzerland: Swiss Broadcasting Corporation, SwissInfo.ch; 2011. [Available at: http://www.swissinfo.ch/eng/swiss_news/Cabinet_rules_out_new_suicide_legislation_.html?cid=30575282; cited April 20, 2012] [Google Scholar]
- 30.Act of 14 June 2002 on Palliative Care [Belgian Dutch]. Belgisch Staatsblad 22.10.2002.
- 31.Grand Duchy of Luxembourg . Memorial: Journal Officiel du Grand-Duché de Luxembourg. Recueil de legislation. Vol. 46. Luxembourg: Association momentanée Imprimerie Centrale/Victor Buck; 2009. Law of March 16, 2009, on palliative care, advance directives, and end of life ... [French] pp. 610–14. [Available online at: http://www.legilux.public.lu/leg/a/archives/2009/0046/a046.pdf; cited April 20, 2012] [Google Scholar]
- 32.Steinbrook R. Physician-assisted death—from Oregon to Washington State. N Engl J Med. 2008;359:2513–15. doi: 10.1056/NEJMp0809394. [DOI] [PubMed] [Google Scholar]
- 33.Quill TE. Legal regulation of physician-assisted death—the latest report cards. N Engl J Med. 2007;356:1911–13. doi: 10.1056/NEJMp078061. [DOI] [PubMed] [Google Scholar]
- 34.Page AR. What’s the cost of living in Oregon these days? A fresh look at the need for judicial protections in the Death with Dignity Act. Reg U Law Rev. 2009;22:233–57. [Google Scholar]
- 35.van der Burg W. The slippery slope argument. Ethics. 1991;102:42–65. [PubMed] [Google Scholar]
- 36.Downie JG. Toronto, ON: University of Toronto Press; 2004. Dying Justice: A Case for Decriminalizing Euthanasia and Assisted Suicide in Canada. [Google Scholar]
- 37.Den Hartogh G. The slippery slope argument. In: Kuhse H, Singer P, editors. Companion to Bioethics. Malden, MA: Wiley–Blackwell; 2009. pp. 321–32. [DOI] [Google Scholar]
- 38.Schuklenk U, van Delden JJM, Downie J, McLean S, Upshur R, Weinstock D. The Royal Society of Canada Expert Panel: End-of-Life Decision Making. Ottawa, ON: Royal Society of Canada; p. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Volokh E. The mechanisms of the slippery slope. Harv L Rev. 2003;116:1026–137. doi: 10.2307/1342743. [DOI] [Google Scholar]
- 40.Switzerland, Federal Department of Justice and Police (fdjp) Specific Regulations for Organised Assisted Suicide in Switzerland [press release] Berne, Switzerland: FDJP; 2010. [Available online at: http://www.ejpd.admin.ch/content/ejpd/en/home/dokumentation/mi/2010/2010-09-17.html; cited April 20, 2012] [Google Scholar]
- 41.Sutorius E, Peters J, Daniels S. Proof of a Law [Web page, Dutch] The Hague, Netherlands: Uit Vrije Wil; n.d. [Available at: http://sparta.projectie.com/~uitvrije/index.php?id=1006; cited April 20, 2012] [Google Scholar]
- 42.Dutch Medical Association (knmg) KNMG Calls for Research on Older People with a Wish to Die [Web page, Dutch] Utrecht, Netherlands: KNMG; 2012. [Available at: http://knmg.artsennet.nl/Nieuws/Nieuwsarchief/Nieuwsbericht-1/KNMG-roept-op-tot-onderzoek-naar-ouderen-met-stervenswens.htm; cited April 20, 2012] [Google Scholar]
- 43.Expatica.com. Amsterdam, Netherlands: Expatica Communications; 2009. Home > News > Belgian News > 93-Year-Old Belgian Woman on Hunger Strike [Web page] [Available at: http://www.expatica.com/be/news/local_news/93_year_old-Belgian-woman-on-hunger-strike_50901.html; cited April 20, 2012] [Google Scholar]
- 44.Smets T, Bilsen J, Cohen J, Rurup ML, Mortier F, Deliens L. Reporting of euthanasia in medical practice in Flanders, Belgium: cross sectional analysis of reported and unreported cases. BMJ. 2010;341:c5174. doi: 10.1136/bmj.c5174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cohen–Almagor R. Belgian euthanasia law: a critical analysis. J Med Ethics. 2009;35:436–9. doi: 10.1136/jme.2008.026799. [DOI] [PubMed] [Google Scholar]
- 46.Vermeersch E. The Belgian law on euthanasia. The historical and ethical background. Acta Chir Belg. 2002;102:394–7. doi: 10.1080/00015458.2002.11679341. [DOI] [PubMed] [Google Scholar]
- 47.Pousset G, Mortier F, Bilsen J, Cohen J, Deliens L. Attitudes and practices of physicians regarding physician-assisted dying in minors. Arch Dis Child. 2011;96:948–53. doi: 10.1136/adc.2009.182139. [DOI] [PubMed] [Google Scholar]
- 48.First Report to the Chamber of Deputies: 2009 and 2010. Brussels, Belgium: The Commission; 2011. Commission nationale de contrôle et d’evaluation de la Loi du 16 mars 2009 sur l’euthanasie et l’assistance au suicide. [French] [Available online at: http://www.sante.public.lu/publications/sante-fil-vie/fin-vie/premier-rapport-loi-16-mars-2009/premier-rapport-loi-16-mars-2009.pdf; cited April 20, 2012] [Google Scholar]
- 49.Switzerland, Federal Department of Home Affairs, Federal Statistical Office (fso) FSO News. Neuchâtel, Switzerland: FSO; 2012. Cause of death statistics 2009; assisted suicide and suicide in Switzerland. [Available for download at: http://www.bfs.admin.ch/bfs/portal/en/index/news/publikationen.html?publicationID=4732; cited April 20, 2012] [Google Scholar]
- 50.Douez S.Assisted Suicide Numbers Up in 2011 [Web article] Berne, Switzerland: Swiss Broadcasting Corporation, SwissInfo.ch; 2012[Available at: http://www.swissinfo.ch/eng/swiss_news/Assisted_suicide_numbers_up_in_2011.html?cid=32154940; cited April 20, 2012]2931614 [Google Scholar]
- 51.Dignitas: To Live with Dignity, To Die with Dignity. Accompanied Suicides of Members of Dignitas, by Year and Country of Residency. Forch, Switzerland: Dignitas; 2011. [Swiss German] [Available online at: http://www.dignitas.ch/images/stories/pdf/statistik-ftb-jahr-wohnsitz-1998-2011.pdf; cited April 20, 2012] [Google Scholar]
- 52.Switzerland, Neuchâtel, District Court. Dossier: POL.2010.19. Distinction between assisted suicide and murder at the victim’s request. Extenuating circumstances exist [French]. Neuchâtel, Switzerland: District Court; 2010. [Available online at: http://jurisprudence.ne.ch/scripts/omnisapi.dll?OmnisPlatform=WINDOWS&WebServerUrl=jurisprudence.ne.ch&WebServerScript=/scripts/omnisapi.dll&OmnisLibrary=JURISWEB&OmnisClass=rtFindinfoWebHtmlService&OmnisServer=JURISWEB,localhost:7000&Parametername=NEWEB&Schema=NE_WEB&Source=&Aufruf=getMarkupDocument&cSprache=FRE&nF30_KEY=4942&nTrefferzeile=1&Template=search_result_document.html; cited April 20, 2012]
- 53.Oregon, Department of Human Services, Oregon Health Division, Center for Disease Prevention and Epidemiology . Oregon’s Death with Dignity Act: The Second Year’s Experience. Portland, OR: Oregon Health Division; 1999. [Available online at: http://public.health.oregon.gov/ProviderPartnerResources/EvaluationResearch/DeathwithDignityAct/Documents/year2.pdf; cited April 20, 2012] [Google Scholar]
- 54.Oregon, Public Health Division (phd) Oregon’s Death with Dignity Act—2011. Portland, OR: PHD; 2011. [Available online at: http://public.health.oregon.gov/ProviderPartnerResources/EvaluationResearch/DeathwithDignityAct/Documents/year14.pdf; cited April 20, 2012] [Google Scholar]
- 55.Oregon, Health Authority, Public Health Division (phd) Oregon’s Death with Dignity Act: thirteen years. CD Summary. 2011;60:1. [Available online at: http://public.health.oregon.gov/DiseasesConditions/CommunicableDisease/CDSummaryNewsletter/Documents/2011/ohd6006.pdf; cited April 20, 2012] [Google Scholar]
- 56.Oregon, Public Health Division (phd) Portland, OR: PHD; 2010. Oregon’s Death with Dignity Act—2010. [Available online at: http://public.health.oregon.gov/ProviderPartnerResources/EvaluationResearch/DeathwithDignityAct/Documents/year13.pdf; cited April 20, 2012] [Google Scholar]
- 57.Compassion and Choices of Oregon. Supporters of Death with Dignity Hail Failure of HB2016 [Web page] Portland, OR: Compassion and Choices of Oregon; 2011. [Available online at: http://blog.compassionandchoices.org/?p=1407; cited April 20, 2012] [Google Scholar]
- 58.Washington, Department of Health (doh) Washington State Department of Health 2010 Death with Dignity Act Report. Olympia, WA: DOH; 2010. [Available online at: http://www.doh.wa.gov/dwda/forms/DWDA.2010.pdf; cited April 20, 2012] [Google Scholar]
- 59.Canadian Medical Association (cma) CMA Policy: Euthanasia and Assisted Suicide (Update 2007) Ottawa, ON: CMA; p. 2007. [Google Scholar]
- 60.British Medical Association (bma) Ethics Department. End-of-Life Decisions: Views of the BMA. London, U.K.: BMA; 2009. pp. 4–6. [Google Scholar]
- 61.Australian Medical Association (ama) AMA Position Statement: Position Statement on the Role of the Medical Practitioner in End of Life Care. Canberra, Australia: AMA; 2007. p. 6. [Available for download at: http://ama.com.au/node/2803; cited April 20, 2012] [Google Scholar]
- 62.American Medical Association (ama) Resources > Medical Ethics > AMA Code of Medical Ethics [Web page]. Sect. 2.21, Sect. 2.211. Chicago, IL: AMA; n.d. [Available at: http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics.page; cited April 20, 2012] [Google Scholar]