Abstract
Purpose
In 2006, the American Society of Clinical Oncology established guidelines on fertility preservation in cancer patients, but recent data suggest that the guidelines are not widely followed. To identify the frequency of fertility discussions and the characteristics that influence the rate of discussion, we performed a retrospective chart review for patients less than 40 years of age with newly diagnosed colorectal cancer (crc).
Methods
Charts of patients aged 18–40 years with newly diagnosed crc presenting to the Juravinski Cancer Centre from 2000 to 2009 were reviewed for documentation of discussions regarding fertility risks with treatment and reproductive options available. The influences of sex, age, year of diagnosis, stage of cancer, and type of treatment on the frequency of discussions were explored.
Results
The review located 59 patients (mean age: 35 years) who met the criteria for inclusion. A fertility discussion was documented in 20 of those patients [33.9%; 95% confidence interval (ci): 22.1% to 47.4%]. In the multivariate analysis, the odds of fertility being addressed was higher for patients receiving radiation [odds ratio (or): 9.31; 95% ci: 2.49 to 34.77, p < 0.001) and lower by age (or: 0.86; 95% ci: 0.74 to 0.99; p = 0.040). Of patients less than 35 years of age undergoing radiation treatment, 85% had a documented fertility discussion. We observed no significant difference in the frequency of discussions after 2006, when the American Society of Clinical Oncology guidelines were published (31.4% for 2000–2006 vs. 37.5% for 2007–2009, p = 0.63).
Conclusions
Discussions about fertility risks associated with crc treatment occur infrequently among young adults with newly diagnosed crc. However, discussions occur more frequently in younger patients and in those undergoing radiation. Further investigations assessing barriers and physician attitudes to fertility risk discussion and reproductive options are planned.
Keywords: Fertility, colorectal cancer, supportive, practice
1. INTRODUCTION
Colorectal cancer (crc) is the third most common cancer among men and women, with approximately 150,000 new cases diagnosed each year in the United States 1. About 6% of cases occur in the first four decades of life, with 3% occurring in people between the ages of 20 and 40 years 1. The incidence of crc in 20- to 49-year-olds increased by 1.5% per year in men and 1.6% per year in women from 1992 to 2005, an increase driven predominantly by an increasing incidence of rectal cancer 2. Thus, issues of fertility and family planning can arise because of the effects of surgery, radiation, and chemotherapy on a patient’s reproductive health.
Although adjuvant chemotherapy with 5-fluorouracil alone may have little influence on fertility, it is unknown whether agents such as oxaliplatin and irinotecan cause gonadal failure 1. Moreover, there is an infertility risk associated with surgery for crc, based largely on data suggesting decreased fertility after pelvic surgery for conditions such as inflammatory bowel disease and polyposis syndromes 3. The use of radiation can also have negative fertility consequences, leading to premature ovarian failure in women and sterility in men 4.
During any discussion of treatment for crc, be it surgery, chemotherapy, or radiation, the physician has a responsibility to discuss potential side effects and toxicity. Fertility and family planning issues should therefore be discussed with any young adult before a treatment plan is decided on. The American Society of Clinical Oncology established guidelines on fertility preservation in patients of reproductive age diagnosed with cancer 5. However, one study in crc patients has investigated the frequency of fertility discussion, and it showed that, in a cohort of 13 women of childbearing age, fertility was addressed for only 2 6.
Given the paucity of literature on the subject, we decided to investigate the frequency of fertility discussions before treatment commencement for young adults with newly diagnosed crc at a tertiary care cancer centre. We further examined the influences of age, sex, treatment type, stage of disease, and year of diagnosis on the frequency of fertility discussions.
2. METHODS
A retrospective chart review located patients aged 20–40 years presenting to the Juravinski Cancer Centre from 2000 to 2009 with a new diagnosis of colorectal adenocarcinoma documented at the initial consultation. The Juravinski Cancer Centre is a regional cancer centre located in Hamilton, Ontario, Canada, with a catchment population of more than 1.7 million people. More than 7000 patients are referred to the centre each year by physicians in the region.
Eligible charts were identified through health records and were reviewed by one of the two primary investigators (AK, AM) for documentation indicating that a discussion about the fertility risks of treatment and potential reproductive options had occurred. If the discussion had occurred, then the chart was reviewed to identify whether follow-up with either an oncologist or a reproductive specialist to further discuss the issues had been offered. Demographic and treatment information, including age, sex, stage of cancer, and eventual treatment decisions were extracted from all charts. Patients with stage i or iia disease who were not offered any form of treatment were excluded. The chemotherapy regimens used were defined as “modern” if they contained either oxaliplatin or irinotecan in addition to 5-fluorouracil.
Descriptive statistics, such as mean, median, range, proportion, and frequency, were used to summarize the patient characteristics. Logistic regression was used to investigate factors prognostic for fertility discussion. Multivariate logistic models were constructed using forward stepwise selection. A p value of 0.05 or less was considered statistically significant, and all tests were two-sided. For selected outcomes, 95% exact confidence intervals (cis) were constructed.
3. RESULTS
Within the study period, 3218 patients were identified as presenting with crc. Of those 3218 patients, 70 (2%) met the age criteria. Upon further review, 11 patients were excluded: 9 had stage i or iia disease with no further treatment, 1 had a carcinoid tumour, and 1 had squamous cell pathology. Thus, 59 patients were included in the final analysis. The average age of patients was 34.6 years (range: 26–40 years). The group included 35 men [59.3%; average age: 35.2 years (range: 26–39 years)] and 24 women [average age: 33.6 years (range: 24–40 years)]. Table i summarizes the baseline characteristics of the patients.
TABLE I.
Characteristics of the patients included in the analysis
| Variable |
Group |
||
|---|---|---|---|
| Overall | Men | Women | |
| Patients (n) | 59 | 35 | 24 |
| Age (years) | |||
| Average | 34.6 | 35.2 | 33.6 |
| Range | 24–40 | 26–39 | 24–40 |
| Age [n (%)] | |||
| <35 | 25 (42.4) | 14 | 11 |
| ≥35 | 34 (57.6) | 21 | 13 |
| Year of diagnosis [n (%)] | |||
| Before 2006 | 31 (52.5) | 24 | 11 |
| 2006 onwarda | 28 (47.5) | 11 | 13 |
| Chemotherapy [n (%)] | |||
| 5-Fluorouracil | 23 (39.0) | 18 | 5 |
| Modern | 33 (55.9) | 16 | 17 |
| None | 3 (5.1) | 1 | 2 |
| Radiation [n (%)] | |||
| Yes | 24 (40.6) | 19 | 5 |
| No | 35 (59.4) | 16 | 19 |
| Clinical stage [n (%)] | |||
| iia | 8 (13.6) | 5 | 3 |
| iib | 1 (1.7) | 1 | 0 |
| iiia | 4 (6.8) | 3 | 1 |
| iiib | 13 (22.0) | 8 | 5 |
| iiic | 14 (23.7) | 10 | 4 |
| iv | 18 (30.1) | 8 | 10 |
| Unknown | 1 (1.7) | 1 | 0 |
Guidelines from the American Society for Clinical Oncology were published in 2006.
Approximately 95% of the patients received chemotherapy, with 33 patients (55.9%) receiving modern chemotherapy [for example, folfox (5-fluorouracil–leucovorin–oxaliplatin) or folfiri (5-f luorouracil–leucovorin–irinotecan)] and 23 patients receiving 5-fluorouracil alone. Three patients received no chemotherapy. Radiation therapy was given to 24 patients (40.7%), and 55 patients (93.2%) underwent surgery. Fertility was addressed in 20 patients (33.9%; 95% ci: 22.1% to 47.4%). Of those 20 patients, 2 lacked any documented fertility follow-up; for all 18 remaining patients, fertility follow-up, such as a referral to a fertility specialist or a discussion regarding the patient’s decision not to pursue fertility measures, was documented.
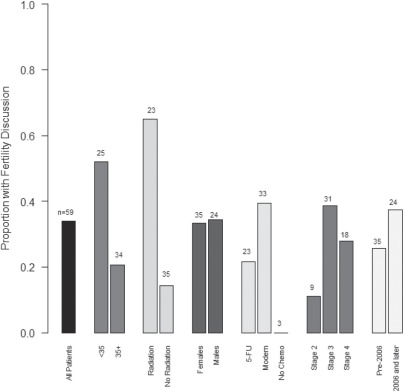
Table ii shows the results of the univariate logistic regression analysis of factors influencing fertility discussion. Figure 1 shows the proportion of patients, by influencing factor, who had a fertility discussion.
TABLE II.
Univariate analyses of prognostic factors for fertility being addressed
| Model variables | Odds ratio | 95%ci | p Value |
|---|---|---|---|
| Sex (women vs. men) | 0.96 | 0.32 to 2.88 | 0.94 |
| Age (per year) | 0.84 | 0.74 to 0.96 | 0.013 |
| Age (≥35 vs. <35) | 0.24 | 0.08 to 0.75 | 0.014 |
| Chemotherapy (M/other vs. 5fu) | 1.80 | 0.57 to 5.68 | 0.31 |
| Chemotherapy (M vs. 5fu) | 2.09 | 0.66 to 6.65 | 0.21 |
| Radiation (yes) | 10.00 | 2.85 to 35.13 | <0.001 |
| Clinical stage (ii vs. iv) | 1.30 | 0.23 to 7.32 | 0.74 |
| Clinical stage (iii vs. iv) | 1.64 | 0.47 to 5.79 | |
| Year of diagnosis (2006 onwardsa) | 1.31 | 0.44 to 3.90 | 0.63 |
American Society for Clinical Oncology guidelines were published in 2006.
M = modern (contained either oxaliplatin or irinotecan in addition to 5-fluorouracil); 5fu = 5-fluorouracil.
FIGURE 1.
Proportion of patients who had a fertility discussion. 5fu = 5-fluorouracil.
Age (p = 0.013) and radiation treatment (p < 0.001) were both statistically significant; the other factors evaluated showed no association with fertility discussion. As a secondary analysis, age was split into younger than 35 years of age and 35 years of age and older. Upon comparison, the results in the two age groups were similar, and therefore age was kept as a continuous outcome because of the increased statistical power available in that scenario. For every year of increase in age, the odds of fertility being discussed declined by 16% (odds ratio: 0.84; 95% ci: 0.74 to 0.96). The odds of fertility being addressed increased for patients undergoing radiation (odds ratio: 10.00; 95% ci: 2.85 to 35.13). The frequency of fertility discussion showed no significant difference after 2006, when the American Society of Clinical Oncology guidelines were published (31.4% for 2000–2006 vs. 37.5% for 2007–2009, p = 0.63).
In the multivariate analysis, radiation and age both entered the regression model. The interaction effect between those two variables was nonsignificant (p = 0.13), and no other variable was significant after adjustments for those two variables. Of the 13 patients younger than 35 who received radiation, 11 (84.6%) had fertility addressed. Only 2 of 12 patients (16.7%) who were younger than 35 years and who did not receive radiation had fertility addressed. Among patients older than 35, 4 of 11 receiving radiation (36.4%) and 3 of 23 not receiving radiation (13.0%) had a fertility discussion.
Fertility discussion rates were similar between the sexes, with discussions occurring with 12 of 35 men (34.3%; 95% ci: 19.1% to 52.2%) and 8 of 24 women (33.3%; 95% ci: 15.6% to 55.3%). Age was a statistically significant prognostic factor for fertility discussions among men (p = 0.016), with 8 of 14 men (57.1%; 95% ci: 28.9% to 82.3%) younger than 35 years of age having a fertility discussion, compared with only 4 of 21 men (19.0%; 95% ci: 5.5% to 41.9%) 35 years of age and older. Age did not attain statistical significance as a prognostic factor among women (p = 0.23). In clinic notes, 5 of 11 women (45.5%; 95% ci: 16.8% to 76.6%) younger than 35 were documented as having had a fertility discussion, compared with 3 of 13 women (23.1%; 95% ci: 6.0% to 61.0%) 35 years of age and older.
4. DISCUSSION
Treatment options for crc include surgery, radiation, and chemotherapy. These modalities are often used in combination. All three can significantly affect fertility.
The literature suggests that newly diagnosed cancer patients consider fertility preservation of utmost importance 7,8. Surveys have shown that cancer survivors identify infertility secondary to cancer treatment as a risk factor for increased emotional distress 8,9. One study in men suggested that banking sperm was a positive factor in coping emotionally with cancer, even if the sample was never used 8. It has been recommended by the President’s Cancer Panel in the United States that all cancer patients of reproductive age be informed about the possibility of treatment-related infertility 10. Options for fertility preservation should be discussed and referrals made to fertility specialists as required.
In our study, only 34% of patients between the ages of 20 and 40 referred for treatment of crc had a documented discussion regarding the fertility risks associated with treatment and the options available for fertility preservation. That rate is a similar to the rate seen in a previous study in a similar patient population, which showed a 20% rate of fertility discussion. Patients receiving radiation were more likely to be offered fertility options, likely because of the well-established and well-known risks of radiation on reproductive organs. Overall, fertility was better addressed in younger patients, but a statistically significant age effect was observed only among men. A smaller, nonsignificant, age effect was observed among women.
A weakness of the study is that a discussion about fertility may have occurred without being documented in the patient record. Thus, the 34% rate found may be an underestimate of the true rate. Moreover, patients may have indicated to the physician that they were not interested in fertility preservation or that they had previously undergone a hysterectomy or vasectomy, thus precluding the need for discussion. However, even such cases, the discussion should ideally be documented. Finally, in patients with whom the issue of fertility was raised, we were unable assess the comprehensiveness of the discussion, the level of patient satisfaction with the discussion, or whether the patient ultimately acted on the discussion by making a change in treatment or using a fertility preservation plan.
Barriers that have been identified to having a discussion about fertility risk and preservation include a lack of knowledge regarding the options available, a lack of time available to clinicians, or an emotional discomfort discussing the issue 11. Many physicians underestimate the importance of fertility to patients and believe that the financial costs of fertility preservation are high. In a study assessing sperm-banking, physicians overestimated the cost of the procedure, and only 7% of patients identified cost as a deterrent to sperm banking 12. Finally, patients with a poor prognosis are less likely to be referred for fertility preservation, although many patients with advanced cancer still desire such discussions 11.
5. CONCLUSIONS
Our study suggests that discussion about the fertility risks associated with crc treatment and the available preservation options occur infrequently among young adults with newly diagnosed crc. Discussions occur more frequently in younger patients and in patients undergoing radiation. To the best of our knowledge, our study is the largest cohort of young crc patients systematically evaluated with respect to fertility discussion. Our results accord with the only other published study exploring fertility risk discussions in young patients with crc. Given that fertility preservation options are available to patients and that, when accessed in a timely fashion, such options do not necessarily delay crc treatment, it is important that discussions about those options be conducted with all appropriate patients. Further investigations assessing barriers to fertility risk discussions and physician attitudes toward reproductive options are planned. In addition, the present study highlights the need to aggressively disseminate to health care professionals knowledge about the importance of fertility risk discussion.
6. CONFLICT OF INTEREST DISCLOSURES
None of the four authors has any financial conflict of interest to declare.
7. REFERENCES
- 1.Zbuk K, Sidebotham E, Bleyer A, La Quaglia MP. Colorectal cancer in young adults. Semin Oncol. 2009;36:439–50. doi: 10.1053/j.seminoncol.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Jemal A, Ward EM. Increase in incidence of colorectal cancer among young men and women in the United States. Cancer Epidemiol Biomarkers Prev. 2009;18:1695–8. doi: 10.1158/1055-9965.EPI-09-0186. [DOI] [PubMed] [Google Scholar]
- 3.Spanos CP, Mamopoulos A, Tsapas A, Syrakos T, Kiskinis D. Female fertility and colorectal cancer. Int J Colorectal Dis. 2008;23:735–43. doi: 10.1007/s00384-008-0483-3. [DOI] [PubMed] [Google Scholar]
- 4.Wallace WH, Thomson AB, Kelsey TW. The radiosensitivity of the human oocyte. Hum Reprod. 2003;18:117–21. doi: 10.1093/humrep/deg016. [DOI] [PubMed] [Google Scholar]
- 5.Lee SJ, Schover LR, Partridge AH, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24:2917–31. doi: 10.1200/JCO.2006.06.5888. [DOI] [PubMed] [Google Scholar]
- 6.Strong M, Peche W, Scaife C. Incidence of fertility counselling of women of child-bearing age before treatment for colorectal cancer. Am J Surg. 2007;194:765–7. doi: 10.1016/j.amjsurg.2007.08.031. [DOI] [PubMed] [Google Scholar]
- 7.Schover LR, Rybicki LA, Martin BA, Bringelsen KA. Having children after cancer: a pilot survey of survivors’ attitudes and experiences. Cancer. 1999;86:697–709. doi: 10.1002/(SICI)1097-0142(19990815)86:4<697::AID-CNCR20>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 8.Schover LR, Brey K, Lichtin A, Lipshultz LI, Jeha S. Knowledge and experience regarding cancer, infertility, and sperm banking in younger male survivors. J Clin Oncol. 2002;20:1880–9. doi: 10.1200/JCO.2002.07.175. [DOI] [PubMed] [Google Scholar]
- 9.Saito K, Suzuki K, Iwasaki A, Yumura Y, Kubota Y. Sperm cryopreservation before cancer chemotherapy helps in the emotional battle against cancer. Cancer. 2005;104:521–4. doi: 10.1002/cncr.21185. [DOI] [PubMed] [Google Scholar]
- 10.President’s Cancer Panel 2003/2004 Annual Report: Living Beyond Cancer: Finding a New Balance. Bethesda, MD: National Cancer Institute; 2004. pp. 1–87. [Google Scholar]
- 11.Schover LR, Brey K, Lichtin A, Lipshultz LI, Jeha S. Oncologists’ attitudes and practices regarding banking sperm before cancer t reatment. J Clin Oncol. 2002;20:1890–7. doi: 10.1200/JCO.2002.07.174. [DOI] [PubMed] [Google Scholar]
- 12.Wallace WH, Anderson RA, Irvine DS. Fertility preservation for young patients with cancer: who is at risk and what can be offered? Lancet Oncol. 2005;6:209–18. doi: 10.1016/S1470-2045(05)70092-9. [DOI] [PubMed] [Google Scholar]