Abstract
Study Objectives:
Many studies of adolescent insomnia use experience of insomnia-like symptoms to categorize “caseness.” This is likely to lead to inflated prevalence and may have important ramifications for the research using individual symptoms to operationalize insomnia. The aim of the present study was to contrast the occurrence of insomnia symptoms with cases of insomnia diagnosed using criteria from the fourth edition of the Diagnostic and Statistical Manual for Mental Disorders (DSM-IV) and the second edition of the International Classification of Sleep Disorders (ICSD-II) in a sample of Australian adolescents.
Methods:
Data were collected from 384 representative Australian adolescents aged 13-18 years old (59% male). During school hours, adolescents completed a comprehensive questionnaire battery targeting insomnia criteria and then completed a sleep diary for 7 days.
Results:
Insomnia symptoms were frequently reported by adolescents (e.g., 34.6% for frequent sleep-related daytime consequences). The proportion of adolescents meeting the diagnositc criteria for insomnia was much smaller: 10.9% of adolescents were classified as having General Insomnia using ICSD-II criteria, and 7.8% were classified as having Primary Insomnia according to DSM-IV criteria. ICSD-II Psychophysiological Insomnia was observed in 3.4% of adolescents. Insomnia diagnoses did not vary according to age, gender, school grade, or socioeconomic status. Using the ICSD-II criteria for General Insomnia resulted in a significantly higher number of insomnia diagnoses than did DSM-IV criteria for Primary Insomnia (p < 0.001) and ICSD-II Psychophysiological Insomnia (p < 0.001).
Conclusions:
These results reveal that approximately 3 adolescents in the average classroom of 30 are likely to meet the diagnostic criteria for insomnia, while many more will have insomnia symptoms. There were significant differences in prevalence rates, depending on how insomnia was operationalized.
Citation:
Authors. Insomnia and its symptoms in adolescents: comparing DSM-IV and ICSD-II diagnostic criteria. J Clin Sleep Med 2012;8(3):295-299.
Keywords: Insomnia disorders, insomnia symptoms, adolescents, DSM-IV, ICSD-II
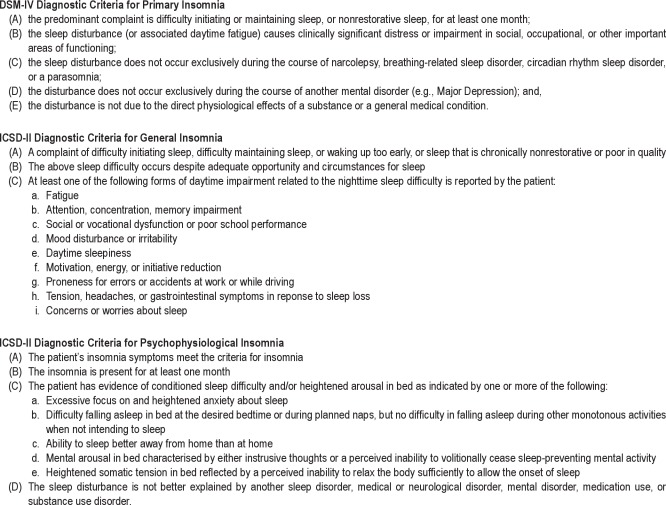
Insomnia can be colloquially known as sleep difficulties; however diagnostic classification systems provide more details about this debilitating disorder. Both the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV)1 and the second edition of the International Classification of Sleep Disorders (ICSD-II)2 describe insomnia in similar ways, but nevertheless subtle differences are apparent (see Appendix for diagnostic criteria). Both the DSM-IV's Primary Insomnia diagnosis1 and the ICSD-II's General Insomnia Disorder2 describe the sleep disturbance as difficulty initiating/maintaining sleep, waking too early, and/or non-restorative sleep.1,2 Both insomnia diagnoses require the sleep difficulty to be related to daytime impairment;1,2 however the the DSM-IV's Primary Insomnia diagnoses only provides a single example (i.e., fatigue),1 whereas the ICSD-II's General Insomnia diagnosis lists many more daytime impairments (e.g., memory impairment, poor school performance, etc.).2 General Insomnia also requires that there be adequate opportunity for sleep. Once these criteria are met, the ICSD-II also provides a more detailed insomnia diagnosis, Psychophysiological Insomnia, which assumes the criteria for General Insomnia are met.2 Both the DSM-IV's Primary Insomnia and the ICSD-II's Psychophysiological Insomnia state the nocturnal and associated diurnal symptoms are experienced for at least 1 month,1,2 and are stated to better explain the sleep disturbance than other sleep disorders, or sleeplessness arising from mental disorders, general medical conditions, and substance use.1,2 The ICSD-II's Psychophysiological Insomnia provides further clarity by stating that there must be evidence for conditioned sleep difficulty and/or heightened arousal in bed.2
BRIEF SUMMARY
Current Knowledge/Study Rationale: Previous rates of insomnia in adolescents range between 7-40%. The present study compares rates of insomnia symptoms and insomnia disorders using current diagnostic systems (i.e., DSM-IV and ICSD-II).
Study Impact: The findings highlight the importance of distinguishing between insomnia symptoms from insomnia disorders. Querying daytime impairments, heightened arousal, maladaptive conditioning, and the chronicity of symptoms in addition to sleep difficulties will provide more accurate estimates for the early detection and treatment of adolescent insomnia.
Estimates of the prevalence of “insomnia” have varied widely, from approximately 2% to 48% in adults,3 and from 7% to 40% in adolescents.4 Differences in the rate of insomnia are likely to occur due to the different ways that insomnia is conceptualized and measured. Less stringent classification of insomnia is likely to result in higher prevalence rates. Studies that have assessed adolescents' difficulties initiating/maintaining sleep or nonrestorative sleep over a 1-month period report rates of insomnia ranging between 12% and 17%.5,6 Other studies have used a shorter symptomatic timeframe, resulting in higher prevalence (e.g., 34% of adolescents met the criteria for insomnia over 2-week period),7 or have classified caseness according to the experiencing of one or more insomnia symptoms “often” or “always” (23.5%),8 again resulting in higher proportions of adolescents classified as having insomnia. These studies demonstrate that many adolescents experience insomnia symptoms; however, focusing on individual symptoms leads to inflated prevalence rates. In addition, many studies of adolescent insomnia do not assess unrefreshing or nonrestorative sleep—a Criterion A symptom in both ICSD-II2 and DSM-IV1 criteria. Thus, they do not provide a good indication of the proportion of adolescents who meet full diagnostic criteria for an insomnia disorder.9 This has potentially significant ramifications for studies examining the etiology or consequences of insomnia if there are important differences between individuals experiencing insomnia symptoms versus those who have an insomnia disorder.
Research using the DSM-IV to assess Primary Insomnia1 in adolescent samples suggests the rate of insomnia is more conservative (< 11%),4 with estimates ranging from 4% in European samples10 to 5% to 11% in North American samples.4,11 One novel study contrasted insomnia disorder prevalence using separate diagnostic systems. In a sample of 794 European adolescents aged 15-18 years, Ohayon and Roberts12 compared insomnia diagnostic criteria from the DSM-IV with the International Classification of Sleep Disorders, 1st edition (ICSD).13 They found 3.3% met criteria for DSM-IV Primary Insomnia, compared to only 1.9% with ICSD Psychophysiological Insomnia. In 2005, the second edition of the ICSD was released.2 In adults, the percentage identified with an insomnia disorder is higher using the DSM-IV criteria compared to the ICSD-II.14 To our knowledge, research has not examined rates of adolescent insomnia between the DSM-IV and the updated ICSD,2 nor are there comparisons of rates of insomnia symptoms compared to insomnia disorders. Thus, the aim of the present study is to compare the proportions of DSM-IV and ICSD-II diagnoses of insomnia with rates of insomnia symptoms in adolescents and to determine whether these different methods of assessment result in comparable rates of diagnosis.
METHOD
Participants and Procedures
Participants were 384 adolescents from 8 schools (7 co-educational and 1 single-sex boys school) in Adelaide, South Australia. Schools were selected from a stratified sample based on socioeconomic status. Adolescents were aged 13-18 years (M = 15.6, SD = 1.0, 59% male). The majority of adolescents (39.7%) consumed caffeinated beverages less than once per day, with 14.7% drinking a caffeinated beverage every day. In the past 2 weeks, the overwhelming majority (72.8%) did not drink alcohol, with only 8.9% reporting that they drank alcohol “more than once but not everyday.” Only 3 adolescents (< 1%) reported infrequently taking prescribed medication, and 5 (1.3%) reported taking over-the-counter herbal remedies for their sleep in the past 2 weeks. Seventy-seven percent of adolescents resided with 2 parents. The majority (71.5%) of participants came from families with 2 or 3 children, and most (86.3%) were born in Australia. Eighty percent of fathers and 30.4% of mothers were in fullltime paid employment; 82.7% of adolescents had their own bedroom. The study was promoted as a “health survey,” and the response rate was 84%. Informed consent was obtained from parents and adolescents. This study was approved by the Flinders University Social and Behavioral Research Ethics Committee and the Department of Education and Children's Services Ethics Committee. Adolescents completed questionnaires during school class time (see Measures) and maintained a record of their sleep patterns using a 7-day sleep diary. Data collection occurred from April 2008 to April 2010, during school terms, at least 2 weeks either side of school holidays, and not during daylight savings.
Measures
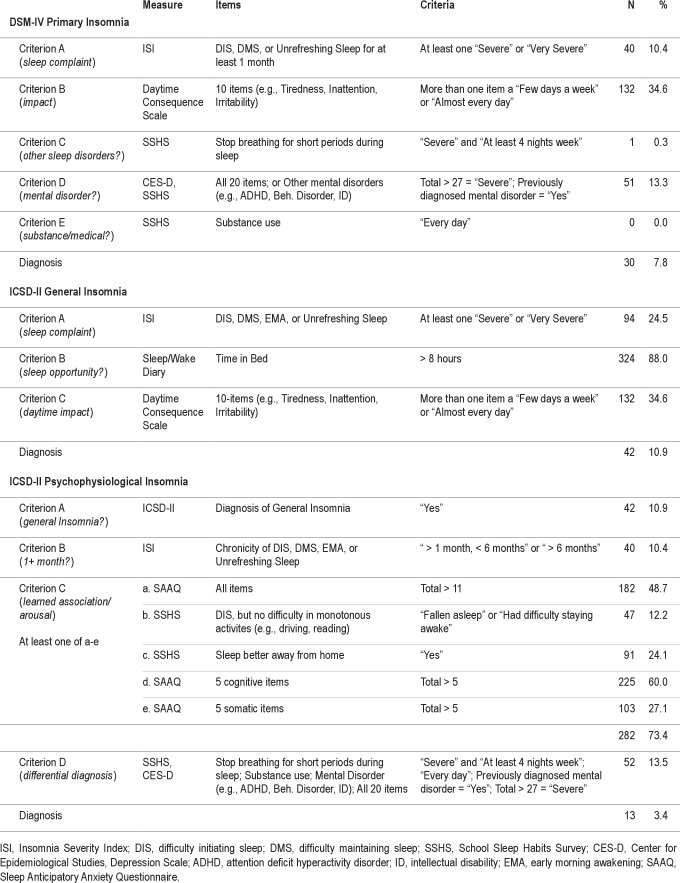
Table 1 outlines the measures, items, and scoring used to diagnose DSM-IV Primary Insomnia, and ICSD-II General Insomnia and Psychophysiological Insomnia. The Insomnia Severity Index (ISI)15 was used to assess adolescents' sleep complaints, such as difficulty initiating (DIS) or maintaining sleep (DMS). In line with diagnostic criteria, an added item examined unrefreshing sleep. Each item was rated on a 5-point Likert scale (ranging from 0 “not at all” to 4 “very severe”). Finally, adolescents were asked of the chronicity of their sleep complaint (e.g., “How long have you had difficulty falling asleep?”). The item assessing early morning awakening was drawn from the School Sleep Habits Survey.16 It asked participants “How often have you awakened too early in the morning and couldn't get back to sleep?” Responses ranged from 0 (“never”) to 4 (“every day/night”).
Table 1.
A 7-day sleep diary obtained a self-report measure of adolescents' sleeping patterns, providing mean sleep onset latency (SOL), bedtimes, and time in bed (TIB). Ninety-two percent of the sample provided complete school week sleep data. TIB > 8 h was considered “adequate opportunity for sleep” for Criterion B of ICSD-II General Insomnia. Sleep diary bedtimes were substantiated with adolescents phoning these in daily (78% compliance), as well as wrist actigraphy (Ambulatory Monitoring Inc., Ardsley, NY), with 75% compliance. Adolescents completed a 10-item daytime consequences of poor sleep scale based on General Insomnia Criterion C from the ICSD-II. Items included “I felt fatigued or exhausted” and “I lacked motivation or energy.” A 6-point scale was used, ranging from 0 (“don't know”) to 5 (“every day or almost every day”).
The Sleep Anticipatory Anxiety Questionnaire (SAAQ)17 examined heightened arousal in bed. The 10-item SAAQ measures pre-sleep anxiety, with somatic and cognitive anxiety subscales. A 4-point scale was used (0 = “strongly disagree” to 3 = “strongly agree”). For the present study, the total, cognitive, and somatic subscales scores were used to address Criterion C of ICSD-II Psychophysiological Insomnia.
The School Sleep Habits Survey (SSHS)16 was used to examine a number of other diagnostic criteria. The SSHS is a widely used questionnaire that comprises questions about sleep/wake behaviors, sleep hygiene (e.g., substance use), non-school activities (e.g., sport, part-time work), and socioeconomnic status, among others. Of interest to the present study were questions examining adolescents' trouble staying awake or falling asleep during monotonous activities (e.g., travelling in a car, at school), or whether they slept better away from home, which targeted ICSD-II Psychophysiological Insomnia criteria. The SSHS also asks questions about other sleep (e.g., breathing-related disorders) and medical conditions. Finally, adolescents completed the Center for Epidemiological Studies–Depression scale (CES-D)18 in class. Ninety-nine percent of adolescents completed the entire questionnaire battery.
RESULTS
As shown in Table 1, 7.8% of adolescents met DSM-IV criteria for Primary Insomnia and 10.9% met ICSD-II diagnostic criteria for General Insomnia (GI). McNemar χ2 analyses were used to test whether the proportion of adolescents meeting criteria for a diagnosis of insomnia was significantly different between the means of assessing insomnia. Considering the 2 diagnostic systems used, adolescents were significantly more likely to receive a diagnosis of insomnia when ICSD-II General Insomnia criteria were used as opposed to DSM-IV Primary Insomnia criteria, χ2(1) = 264.99, p < 0.001, Φ = 0.831. When applying the diagnostic criteria for ICSD-II Psychophysiological Insomnia (PPI), 3.4% of adolescents met these criteria. This is a significantly smaller proportion of adolescents meeting PPI criteria than met either ICSD-II General Insomnia criteria (10.9%), χ2(1) = 109.57, p < 0.001, Φ = 0.534, or the DSM-IV Primary Insomnia criteria (7.8%), χ2(1) = 158.78, p < 0.001, Φ = 0.643. Phi (Φ) values > 0.5 reveal that the effect size for all comparisons was large.
When examining insomnia symptoms, > 10% of adolescents had either difficulty initiating or maintaining sleep for ' 1 month or sleep that was nonrestorative for ≥ 1 month; 25% reported a sleep complaint of either difficulty initiating or maintaining sleep, early morning awakenings, or that their sleep was not refreshing regardless of time frame. A large proportion of adolescents (35%) reported their sleep impacted their daytime functioning. The majority (88%) of the 384 adolescents had adequate time and opportunity in bed (> 8 h).
Among the 10.9% of adolescents diagnosed with GI, nearly all had been experiencing their sleep complaint for at least one month. While only a small proportion of adolescents met the diagnositc criteria for PPI, nearly three-quarters (73%) of the entire sample demonstrated evidence of a conditioned sleep difficulty and/or heightened arousal in bed (Criterion C, a to e). Excessive focus on and heightened anxiety about sleep (49%) [a], including both cognitive arousal (60%) [d] and somatic arousal (27%) [e] were commonly reported. Nearly one-quarter of the 384 adolescents (24%) said they sleep better away from home than at home [c], and 12% reported difficulty falling asleep in bed but no difficulty during monotonous activites [b]. Fourteen percent were excluded due to a diagnosis of another disorder (Criterion D). In particular, 13% of the adolecents were identified at risk for Major Depression, according to the CES-D.
Finally, the demographics of adolescents with and without a diagnosis of insomnia were examined. Independent samples t-tests revealed no significant differences for age, grade, or SES (all p > 0.05), in predicting the diagnoses of Primary Insomnia, GI, or PPI. Similarly, no differences were found for gender when using χ2 analyses (all p > 0.05). Compared to adolescents without an insomnia diagnosis, depression scores were significantly higher for adolescents diagnosed with ICSD-II diagnoses (GI = p < 0.0001; PPI = p < 0.05), but not different from those with a DSM-IV Primary Insomnia diagnosis (p = 0.11). Finally, no significant differences were found for frequency of alcohol use between adolescents with and without an insomnia diagnosis (all p > 0.05).
DISCUSSION
The present study compared DSM-IV and ICSD-II insomnia diagnoses in a sample of Australian adolescents. Our results show 7.8% met DSM-IV diagnostic criteria for Primary Insomnia. This percentage lies within the range for previously reported rates of insomnia in adolescents from other countries, which vary between 3% to 11%.5,6 Similar to Ohayon and Roberts'12 comparative study using the first edition of the ICSD, our findings show that using DSM-IV insomnia criteria resulted in lower rates of diagnosis than the more recent ICSD-II criteria for General Insomnia. The inclusion of differential diagnosis criteria in the DSM-IV criteria is likely to account for much of this difference. With the forthcoming proposed additions to the DSM-V insomnia diagnosis,19 the greater specificity (i.e., insomnia present 3 times per week for ≥ 3 months) is likely to reduce the rate; however, allowing the insomnia disorder diagnosis despite a coexisting condition (i.e., depression) would likely increase the rate. For example, in the present study, > 13% of adolescents were excluded from a potential DSM-IV Primary Insomnia diagnosis due to the likely presence of an existing mental disorder. Inclusion of this group would raise the rate from 7.8% to 20.8%. Unfortunately, we did not collect data on the weekly frequency of insomnia, nor use a 3-month timeframe, thus we cannot provide a final estimate of the percentage of adolescents who would qualify for a DSM-V Insomnia Disorder diagnosis.
Of note, unlike Ohayon and Roberts,12 the present study found rates of insomnia approximately twice the size of theirs (i.e., DSM-IV: 7.8% vs. 3.3%; ICSD PPI: 3.4% vs. 1.9%). There may be several explanations for this difference. First, it has been a decade since Ohayon and Roberts' study. The proportion of adolescents with insomnia may be rising in line with increasing demands on adolescents' lives (e.g., study, part-time employment) and their increased use of technology,20,21 all of which increase arousal and impact their sleep. However, of all factors tested in the present study, it appears depression symptoms are more likely involved in the diagnosis of an insomnia disorder—at least the ICSD-II diagnoses. Second, rates of adolescent insomnia are likely to differ between countries,22 highlighting the need for studies across disparate countries and cultures. Third, Ohayon and Roberts12 used a telephone-based diagnostic assessment that may have excluded more adolescents than the survey and sleep diary used in the present study. In contrast, recent work has demonstrated the use of the Brief Insomnia Questionnaire (BIQ) to assess insomnia in adults was more likely to underdiagnose compared to clinician-led interviews.14 Use of the same protocol (i.e., BIQ vs. expert clinical interviews) to assess insomnia in adolescents would help qualify published prevalence rates and steer researchers towards preferred measurement tools. The use of close-ended questions with binary answers (yes or no) along with follow-up probe questions are likely to yield more accurate estimates compared to questionnaire items with multiple responses (i.e., moderate, severe, very severe), which require decisions about where to apply a cutoff answer. In the present study we used a more stringent cutoff for sleep difficulties (at least “severe”). This method produced a conservative estimate that 1-3 adolescents per class of 30 school students qualify for an insomnia disorder, nevertheless suggesting an important and prevalent public health concern.
The present study shows a reliance on measuring insomnia by symptoms only can lead to inflated rates. For instance, enquiring about difficulties initiating, maintaining, or unfreshing sleep resulted in a 24.5% rate, but when a 1-month timeframe was applied (as per the DSM-IV Primary Insomnia criteria), this decreased to 10.4%. These figures concur with those found in other studies focusing on insomnia symptoms (12%-34%)4–7 and highlight the need for comprehensive assessments of insomnia that include associated daytime symptoms, heightened arousal, and maladaptive conditioning. Possibly the most important questions to ask involves differential diagnosis. In the present study, the largest indicator that adolescents insomnia was likely not a primary disorder was from clinically elevated depression scores. Over 13% of adolescents were excluded from a potential DSM-IV insomnia diagnosis due to the likely presence of an existing mental disorder. Further investigations will be rewarding, such that accurately recognizing and diagnosing insomnia will help health professionals better diagnose and treat adolescent insomnia early to prevent its transition into early adulthood.
DISCLOSURE STATEMENT
This was not an industry supported study. The author has indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This work was conducted at the Flinders University of South Australia. The authors thank Jason Gill, Anna Johnston, Emma Currie, and Lisa-Marie Colton who assisted in data collection, and the school principals and adolescents who participated in this project. Funding was provided by an Australian Research Council Discovery Project Grant (#DP0881261).
Appendix A.
DSM-IV and ICSD-II Insomnia Diagnostic Criteria
REFERENCES
- 1.American Psychiatric Association. Diagnostic and Statistical manual of mental disorders, Fourth Edition (DSM-IV) Washington, DC: The American Psychiatric Association; 1994. [Google Scholar]
- 2.American Academy of Sleep Medicine. The International Classification of Sleep Disorders: diagnostic and coding manual. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 3.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 4.Johnson EO, Roth T, Schultz L, Breslau N. Epidemiology of DSM-IV insomnia in adolescents: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics. 2006;117:e247–56. doi: 10.1542/peds.2004-2629. [DOI] [PubMed] [Google Scholar]
- 5.Liu X, Uchiyama M, Okawa M, Kurita H. Prevalence and correlates of self-reported sleep problems among Chinese adolescents. Sleep. 2000;23:27–33. [PubMed] [Google Scholar]
- 6.Morrison DN, McGee R, Stanton WR. Sleep problems in adolescence. J Am Acad Child Adolesc Psychiatry. 1992;31:94–9. doi: 10.1097/00004583-199201000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Roberts RE, Roberts CR, Chen IG. Ethnocultural differences in sleep complaints among adolescents. J Nerv Mental Dis. 2000;188:222–9. doi: 10.1097/00005053-200004000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Kaneita Y, Ohida T, Osaki Y, et al. Insomnia among Japanese adolescents: a nationwide representative survey. Sleep. 2006;29:1543–50. doi: 10.1093/sleep/29.12.1543. [DOI] [PubMed] [Google Scholar]
- 9.Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29:1155–73. doi: 10.1093/sleep/29.9.1155. [DOI] [PubMed] [Google Scholar]
- 10.Ohayon MM, Roberts RE, Zulley J, Smirne S, Priest RG. Prevalence and patterns of problematic sleep among older adolescents. J Am Acad Child Adolesc Psychiatry. 2000;39:1549–56. doi: 10.1097/00004583-200012000-00019. [DOI] [PubMed] [Google Scholar]
- 11.Roberts RE, Roberts CR, Chan W. Persistence and change in symptoms of insomnia among adolescents. Sleep. 2008;31:177–84. doi: 10.1093/sleep/31.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ohayon MM, Roberts RE. Comparability of sleep disorder diagnoses using DSM-IV and ICSD classifications with adolescents. Sleep. 2001;24:920–5. doi: 10.1093/sleep/24.8.920. [DOI] [PubMed] [Google Scholar]
- 13.American Sleep Disorders Association. International classification of sleep disorders: diagnostic and coding manual. Rochester, MN: American Sleep Disorders Association; 1990. [Google Scholar]
- 14.Kessler RC, Coulouvrat C, Hajak G, et al. Reliability and validity of the brief insomnia questionnaire in the America Insomnia Survey. Sleep. 2010;33:1539–49. [PMC free article] [PubMed] [Google Scholar]
- 15.Morin CM. Insomnia: psychological assessment and management. New York: Guilford Press; 1993. [Google Scholar]
- 16.Wolfson AR, Carskadon MA, Acebo C, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26:213–6. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- 17.Bootzin RR, Shoham V, Kuo T. Sleep Anticipatory Anxiety Questionnaire: a measure of anxiety about sleep. Sleep Res. 1993;23:188. [Google Scholar]
- 18.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1997;1:385–401. [Google Scholar]
- 19.American Psychiatric Association. DSM-V Proposed Revision. Retrieved August 10, 2011, from http://www.dsm5.org/ProposedRevision/Pages/proposedrevision.aspx?rid=65.
- 20.Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: a review. Sleep Med. 2010;11:735–42. doi: 10.1016/j.sleep.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 21.National Sleep Foundation. 2011 Sleep in America Poll. Washington: National Sleep Foundation; 2011. [Google Scholar]
- 22.Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. 2010;12:110–8. doi: 10.1016/j.sleep.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 23.Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31:1351–6. [PMC free article] [PubMed] [Google Scholar]
- 24.Roberts RE, Roberts CR, Chen IG. Impact of insomnia on future functioning of adolescents. J Psychosom Res. 2002;53:561–9. doi: 10.1016/s0022-3999(02)00446-4. [DOI] [PubMed] [Google Scholar]