Abstract
INTRODUCTION
The aim of this systematic review is to describe the use of cadavers in postgraduate surgical training, to determine the effect of cadaveric training sessions on surgical trainees' technical skills performance and to determine how trainees perceive the use of cadaveric workshops as a training tool.
METHODS
An electronic literature search was performed, restricted to the English language, of MEDLINE®, Embase™, the Cumulative Index to Nursing and Allied Health Literature (CINAHL®), Centre for Agricultural Bioscience (CAB) Abstracts, the Educational Resources Information Center (ERIC™) database, the British Education Index, the Australian Education Index, the Cochrane Library and the Best Evidence in Medical Education website. Studies that were eligible for review included primary studies evaluating the use of human cadaveric surgical workshops for surgical skills training in postgraduate surgical trainees and those that included a formal assessment of skills performance or trainee satisfaction after the training session.
RESULTS
Eight studies were identified as satisfying the eligibility criteria. One study showed a benefit from cadaveric workshop training with regard to the ability of trainees to perform relatively simple emergency procedures and one showed weak evidence of a benefit in performing more complex surgical procedures. Three studies showed that trainees valued the experience of cadaveric training.
CONCLUSIONS
Evidence for the effectiveness of cadaveric workshops in surgical training is currently limited. In particular, there is little research into how these workshops improve the performance of surgical trainees during subsequent live surgery. However, both trainees and assessors hold them in high regard and feel they help to improve operative skills. Further research into the role of cadaveric workshops is required.
Keywords: Surgery, Education, Graduate
In his 2008 annual report, the Chief Medical Officer identified that simulation offers an important route to safer care for patients and recommended that simulation-based training should be fully integrated and funded within training programmes for clinicians at all stages.1 Kneebone and Aggarwal claimed that the strength of simulation is as an adjunct rather than an alternative to clinical experience.2 Various modalities of surgical simulation exist, such as computer or video simulation and models,3 but these are all compromised by the absence of normal anatomical relationships and tissue handling, particularly for surgery. Live animal tissue, which offers excellent handling fidelity and the live operative experience of dealing with bleeding, is used worldwide but is not currently permitted under UK law.4
Cadaveric workshops have been used widely in the US and elsewhere and appear to be popular with trainees.5,6 The introduction of the Human Tissue Act in 2004 enables surgeons in the UK to practise operative procedures on cadavers. The Royal College of Surgeons of England has established a cadaveric workshop, the Wolfson Surgical Skills Centre. However, with only 674 donations to British medical schools in 2005,7 the supply of cadavers is limited and storing them and providing surgical training facilities is costly. Therefore, when considering the advantages of using cadavers over other forms of simulation in surgical training, it is important to determine the circumstances in which cadaveric training will confer the greatest benefit so that resources can be used appropriately.
In a review of surgical training, Hamstra et al reported that several studies have shown that technical skills acquired on low fidelity models (ie bench models) could confer the same degree of benefit as training on a high fidelity model (ie cadavers) as it was found that the learning process was of primary importance rather than the physical substrate.8 This may certainly be true for surgical procedures such as suturing or endoscopic removal of a ureteric stone where a bench model can be constructed. However, bench model simulators may not be as advantageous for procedures where anatomy and tissue fidelity play a greater role, such as surgical exposures in limbs or complex visceral procedures. In this context it is important to assess whether the benefits of using cadaveric workshops for teaching surgical skills justifies the difficulty and expense incurred in providing them and also whether there are any circumstances in which cadaveric training may be of particular benefit.
The aim of this systematic review is to describe the use of cadavers in postgraduate surgical training, to determine the effect of cadaveric training sessions on surgical skill and to determine how trainees perceive the use of a cadaver as a training tool.
Methods
Three reviewers (JG, AWP, KH) independently performed a systematic medical literature search, limited to the English language, to identify primary studies that evaluated the use of cadavers in surgical training. The search was carried out using Ovid MEDLINE® (1950 to March Week 4 2010), Embase™ (1980 to March Week 4 2010), CINAHL® (1982 to March Week 4 2010), Centre for Agricultural Bioscience (CAB) Abstracts (1990 – March Week 4 2010), the ERIC™ data-base (1966 – March 2010), the British Education Index (1975 – March 2010), the Australian Education Index (1979 – March 2010), the Cochrane Library (searched in March 2010) and the Best Evidence in Medical Education website (http://www2.warwick.ac.uk/fac/med/beme/) (searched in March 2010). The following search terms were used: (cadaver*) and (education or postgraduate education or surgery*). Two reviewers (JG, AWP) also screened the bibliographies of all articles and abstracts and agreed on eligibility.
Eligibility criteria
Included in our review were studies describing human cadaveric workshops for training multiple postgraduate surgical trainees in basic or advanced surgical skills. The studies needed to have a clearly defined outcome measure to assess the efficacy of training (either on the cadaveric model or in the operating theatre) or either an objective assessment of the technical skill or a qualitative subjective questionnaire regarding the perception of cadavers as a training tool. Disagreements between the reviewers regarding eligibility were resolved with discussion.
The exclusion criteria were: studies on the use of cadavers in education other than for surgical training; studies on surgical simulators other than cadavers; studies using animals.
Data abstraction
Two reviewers (JG and AWP) extracted data from each primary study independently and in duplicate, and discussed the quality of the data and relevant findings.
Study characteristics
Among the studies eligible for review, there was considerable disparity between trial design, grade of trainee, complexity of skill being taught and assessed, outcome measures and conclusions. The trials were therefore separated into those that provided a formal assessment of technical skill on the cadaver after the session, those that provided a formal assessment of technical skill in the clinical setting after the cadaveric session and those that provided a qualitative subjective assessment by the trainee with regard to the use of a cadaver as a training tool.
Results
Figure 1 illustrates the flow of studies through our review. The search of MEDLINE® and Embase™ produced 38 studies, of which 8 satisfied the inclusion criteria. Of the remaining 30, 9 did not relate to surgical training (eg use of dissection in teaching undergraduate anatomy), 6 were on non-cadaveric simulators and 4 were on animals (live or cadaveric). In addition, three were reviews, two were on preservation techniques, two were reports on cadaveric workshops with no attempt to assess their efficacy, two were historical articles, one was a comment on another study and one was a single surgeon series. No other studies (apart from duplications of some of those already found) were identified from the other sources searched. Table 1 gives a summary of the results of the eight studies included in our review.
Figure 1.
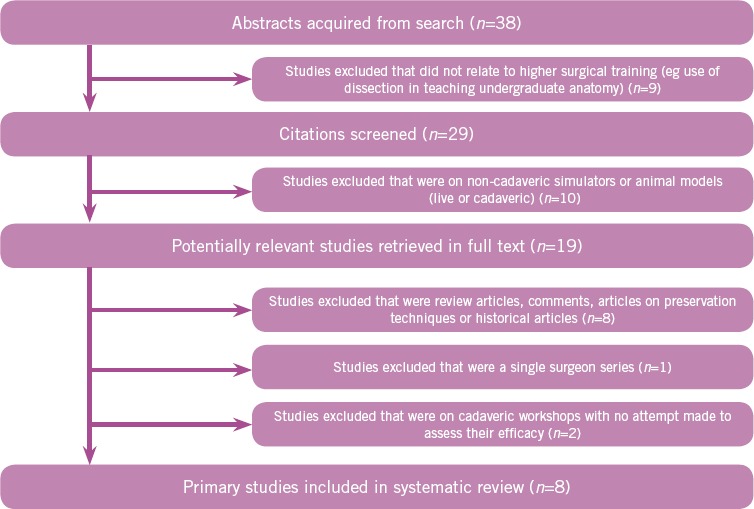
Flow of studies
Table 1.
Summary of results of studies evaluating efficacy of use of cadavers for surgical training
| Authors | No. of trainee surgeons in study | Methodology of study | Control group | Skills taught during session | Complexity of skill | Outcome measure | Assessment of clinical skill after workshop? | Grade of surgeons assessed |
|---|---|---|---|---|---|---|---|---|
| Studies that demonstrate objective assessment of trainees' performance on a cadaveric model after a cadaveric session | ||||||||
| Anastakis et al9 | 23 | Prospective, randomised crossover trial | Yes – compared text only (control group), bench model training, cadaver model training | Burr hole insertion, chest tube insertion, small bowel anastomosis, flexor tendon repair, K-wire fixation of a metacarpal fracture | Basic surgical skills | Detailed checklist with items orientated to the specific operative procedure at each station and a global rating scale of operative skill | No | PGY1 surgical residents |
| Bergeson et al10 | 3 | Observational study | No | Pedicle screw placement in spinal surgery | Advanced surgical skills | Observation of specimen post instrumentation, failure defined as critical violation | No | PGY1 & 3 surgical residents with no experience of freehand thoracic pedicle screw insertion |
| Rowland and Kleinert11 | 9 | Observational study | No | Endoscopic carpal tunnel release | Advanced surgical skills | Dissection of specimen after surgical procedure performed and extent of division of the transverse carpal ligament, neurovascular injury, osseous injury documented | No | Fellows in hand surgery |
| Studies that demonstrate transference of skill to the clinical setting after a cadaveric session | ||||||||
| Dunnington5 | 9 | Observational study | No | Sentinel node mapping and axillary lymph node dissection | Advanced surgical skills | Narrative comments from participants, feedback from faculty surgeons who witnessed trainee performance in the operating theatre | Yes | PGY2 & 3 surgical residents |
| Martin et al12 | 8 | Observational study | No | Chest tube insertion, endotracheal intubation, venous cutdown | Basic surgical skills | Competency-based approach, pass or fail judgement | Yes | PGY1 surgical residents |
| Studies that provide a qualitative subjective assessment of trainees' perceptions of the use of a cadaver as a training tool | ||||||||
| Giger et al13 | 33 | No | Advanced laparoscopic techniques in colon, vascular, hernia and bariatric surgery | Advanced surgical skills | Quality assessment subjective questionnaire completed by participants | No | 31 consultants and 2 senior residents, most of whom had performed fewer than 50 laparoscopic procedures prior to the course | |
| Supe et al6 | 32 | No | No | Cholecystectomy, appendicectomy, splenectomy, intestinal explorations, mesenteric lymph node biopsy and varicocoele vein occlusion | Advanced surgical skills | Subjective questionnaire to study the trainees' perceptions of training on a cadaver model | No | Surgeons with more than five years of practice |
| Reed et al16 | 45 | No | Basic vascular surgical anatomy and operating skills | Advanced surgical skills | Subjective questionnaire and evaluation | No | Second and third year surgical residents | |
PGY = postgraduate year
Studies that demonstrate objective assessment of trainees' performance on cadaveric model after cadaveric session
Anastakis et al published a prospective three-way crossover trial comparing cadaveric workshops, bench models and training by reading from a text.9 Twenty-three postgraduate year (PGY) 1 students were instructed on six surgical procedures in three groups. Each group learned two procedures (from a selection of burr hole insertion, chest tube insertion, small bowel anastomosis, abdominal wound closure, flexor tendon repair and K-wire fixation of a metacarpal fracture) using one of the teaching modalities. Assessment on a cadaver (procedure-specific checklist and a global rating scale) was carried out one week after the course. Both bench and cadaver training were found to be superior to text learning but they were not significantly different from each other. No assessment was made of how well those skills transferred to live patients.
Bergeson et al performed a study using cadaveric thoracic spine sections to evaluate the errors made when novice resident surgeons place thoracic pedicle screws and also to determine how many specimens need to be instrumented to assure an improvement in accuracy.10 A total of 297 pedicles were instrumented in 149 vertebrae. There was an overall technical error rate of 29%; 26% of these errors were critical (defined as a cortical breach of >2mm). The technical error rate decreased with the number of times the residents performed the procedure and with seniority of the resident. The authors of this study employed robust study methods, including direct observation and measurement, but it was compromised by small numbers (three candidates), no control group and no assessment of transfer of skills to the operating theatre.
Rowland and Kleinert evaluated a cadaveric workshop for endoscopic carpal tunnel release.11 Twelve fellows in hand surgery were given individualised instruction in the technique and then performed the surgery on cadavers. A surgeon who had not performed the procedure then dissected the specimen and assessed the adequacy of the carpal tunnel release and the number of operative errors. An incomplete release of the carpal tunnel was found in 9 of the 24 specimens and there were 4 complications. The numbers are too small to make any assessment of whether repetition of the procedure improved the completion rate and reduced the error rate. This study does, however, highlight the difficulties in using an endoscopic technique and also makes a case for practising this particular technique in the workshop before attempting it on a live patient.
Studies that demonstrate transference of skill to the clinical setting after a cadaveric session
Dunnington described a cadaveric workshop for teaching open sentinel lymph node mapping, excision and dissection using cadaver head and torso segments through T6 with radioactive cobalt discs implanted in the axilla.5 Nine PGY2 and PGY3 participants performed the sentinel lymph node excision and full dissection. The workshop was evaluated using a five-point Likert scale. The participants also commented on the authenticity of the cadaver model and valued the feedback from the faculty during the procedure. The faculty, who subsequently supervised participants in theatre, felt that the participants' approach to the axilla was technically better and more confident than residents who had not attended the workshop. However, as there was no control group it is possible that the trainees' performance could have improved as much from the pre-workshop preparation and detailed feedback from the faculty as from the cadaveric work itself.
Martin et al published a series in which eight PGY1 surgical residents in a level 1 trauma centre were assessed performing a chest tube insertion, endotracheal intubation and venous cutdown before and after training in a cadaveric workshop.12 The initial assessment was performed in the workshop and the trainees were required to demonstrate skill ‘mastery’ before returning to patient care. Subsequent assessments were made on the ward. The initial failure rate was high but it improved significantly at both subsequent assessments. The main criticism of this study is that residents could be expected to have sufficient exposure to these procedures to show improvement over time simply by doing their job. The use of a control group would also have improved the strength of the study.
Studies that provide a qualitative subjective assessment of trainees' perceptions of the use of a cadaver as a training tool
Giger et al used Thiel human cadavers for laparoscopy training in colon, vascular, hernia and bariatric surgery.13 Thiel cadavers are prepared using a technique that preserves the colour and consistency of cadaveric tissue.14,15 Data on participant satisfaction was collected on 6 courses that were run over 16 months. The majority of participants were consultants but most had performed fewer than 50 laparoscopic procedures prior to the course. The data revealed a high level of satisfaction with the courses in relation to their instructional content and also a high level of satisfaction with the Thiel human cadavers as simulators for live surgery. There was no attempt formally to assess the effectiveness of training with cadavers in improving skills in live operating. However, using Thiel cadavers is perhaps of value in that it draws attention to a method of preserving cadavers that is felt by experienced surgeons to mimic real conditions closely in vivo.
Supe et al published a survey of trainees' attitudes to using cadaveric workshops for training in laparoscopic techniques.6 The workshop employed the use of fresh cadavers to practise cholecystectomy, appendicectomy, splenectomy, intestinal explorations, mesenteric lymph node biopsy and varicocoele vein occlusion. The trainees' perception of the use of cadavers for training in these procedures was assessed using a questionnaire with a 5-point Likert scale. The parameters measured included understanding of surgical anatomy, understanding of laparoscopic technique and use of laparoscopic equipment. A total of 32 surgeons inexperienced in laparoscopic surgery participated in the study. All expressed satisfaction with the cadaver as a training model, 31 rating it as highly satisfactory. Supe et al commented that ‘the trainees thought it improved spatial perception of anatomy, and they perceived it as a valuable educational experience’ and ‘in the trainees' opinion, limitations of the model were the absence of active bleeding, the absence of breathing perception and limited hours of working as the cadavers tended to become malodorous after 6–8 hours’.
Reed et al published an account of their use of thawed fresh frozen cadavers for teaching vascular anatomy and surgical techniques.16 Second- and third-year residents in general surgery were invited to attend a four-hour session run by a vascular fellow. A dissection manual was also created and given to the trainees. Assessment consisted of an informal questionnaire issued by the organisers and a standard questionnaire issued by the general surgery programme director. These showed that this course met the trainees' expectations and that they felt it was of educational value. No assessment of the skills learnt or their transference to the operating room was made.
Discussion
Of the eight papers, only one12 made any attempt to relate skills learned in a cadaveric workshop to performance on live patients using objective, reproducible assessments. None showed any evidence that skills learnt by practising on cadavers improved performance in the operating theatre. This highlights the difficulty in designing and interpreting educational studies in postgraduates, particularly when patient care is involved in the assessment. Patient safety is of paramount concern and prior experience cannot be controlled. There are also many interventions being used simultaneously, each of which contributes to improving the learning experience for the student and obscuring the effect of any individual part.
Anastakis et al described cadaver models as ‘the gold standard for technical skills training’.9 This may reflect a widely held view that training on cadavers must be the gold standard as they most closely mimic the anatomy of live patients. The cadaver model does seem to have some value in allowing trainees to practise a procedure before performing it live and to make mistakes in a safe environment. Importantly, what this systematic review identifies is that trainees value the experience of training on cadavers and, although there is no strong evidence at this stage that training of cadaveric models transfers to the operating theatre, their use should be further explored. Attempts at surgical simulation in the past have been hindered by lack of fidelity and, as this problem can be overcome with this medium, cadaveric training may be of benefit for surgeons of all levels, from junior trainees to experienced surgeons learning new techniques.
Conclusions
Both trainees and assessors believe that cadaveric workshops are useful adjuncts when teaching operative skills. With the introduction of facilities that enable the use of cadavers for surgical training, further well designed studies can be carried out to confirm the proposed benefit, particularly on the transfer of these skills to the operating theatre. Moreover, it would be beneficial to determine which aspects of surgical training are likely to benefit from cadaver training and to preserve the valuable resource for these particular skills. Educational institutions have focused on improving the facilities and techniques required to run cadaveric training. Now they also need to address the evidence base required to establish that such workshops are truly effective.
References
- 1.Department of Health. 150 Years of the Annual Report of the Chief Medical Officer. London: DH; 2009. [Google Scholar]
- 2.Kneebone R, Aggarwal R. Surgical training using simulation. BMJ. 2009;338:b1001. doi: 10.1136/bmj.b1001. [DOI] [PubMed] [Google Scholar]
- 3.Sutherland LM, Middleton PF, Anthony A, et al. Surgical simulation: a systematic review. Ann Surg. 2006;243:291–300. doi: 10.1097/01.sla.0000200839.93965.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarker SK, Patel B. Simulation and surgical training. Int J Clin Pract. 2007;61:2120–2125. doi: 10.1111/j.1742-1241.2007.01435.x. [DOI] [PubMed] [Google Scholar]
- 5.Dunnington GL. A model for teaching sentinel lymph node mapping and excision and axillary lymph node dissection. J Am Coll Surg. 2003;197:119–121. doi: 10.1016/S1072-7515(03)00231-X. [DOI] [PubMed] [Google Scholar]
- 6.Supe A, Dalvi A, Prabhu R, et al. Cadaver as a model for laparoscopic training. Indian J Gastroenterol. 2005;24:111–113. [PubMed] [Google Scholar]
- 7. Research fuels grim trade in death. BBC News. http://news.bbc.co.uk/1/hi/health/7302468.stm (cited April 2011).
- 8.Hamstra SJ, Dubrowski A, Backstein D. Teaching technical skills to surgical residents: a survey of empirical research. Clin Orthop Relat Res. 2006;449:108–115. doi: 10.1097/01.blo.0000224058.09496.34. [DOI] [PubMed] [Google Scholar]
- 9.Anastakis DJ, Regehr G, Reznick RK, et al. Assessment of technical skills transfer from the bench training model to the human model. Am J Surg. 1999;177:167–170. doi: 10.1016/s0002-9610(98)00327-4. [DOI] [PubMed] [Google Scholar]
- 10.Bergeson RK, Schwend RM, DeLucia T, et al. How accurately do novice surgeons place thoracic pedicle screws with the free hand technique? Spine. 2008;33:E501–507. doi: 10.1097/BRS.0b013e31817b61af. [DOI] [PubMed] [Google Scholar]
- 11.Rowland EB, Kleinert JM. Endoscopic carpal-tunnel release in cadavera. An investigation of the results of twelve surgeons with this training model. J Bone Joint Surg Am. 1994;76:266–268. doi: 10.2106/00004623-199402000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Martin M, Vashisht B, Frezza E, et al. Competency-based instruction in critical invasive skills improves both resident performance and patient safety. Surgery. 1998;124:313–317. [PubMed] [Google Scholar]
- 13.Giger U, Frésard I, Häfliger A, et al. Laparoscopic training on Thiel human cadavers: a model to teach advanced laparoscopic procedures. Surg Endosc. 2008;22:901–906. doi: 10.1007/s00464-007-9502-7. [DOI] [PubMed] [Google Scholar]
- 14.Thiel W. The preservation of the whole corpse with natural colour. Ann Anat. 1992;174:185–195. [PubMed] [Google Scholar]
- 15.Groscurth P, Eggli P, Kapfhammer J, et al. Gross anatomy in the surgical curriculum in Switzerland: improved cadaver preservation, anatomical models, and course development. Anat Rec. 2001;265:254–256. doi: 10.1002/ar.10030. [DOI] [PubMed] [Google Scholar]
- 16.Reed AB, Crafton C, Giglia JS, Hutto JD. Back to basics: use of fresh cadavers in vascular surgery training. Surgery. 2009;146:757–762. doi: 10.1016/j.surg.2009.06.048. [DOI] [PubMed] [Google Scholar]


