Abstract
INTRODUCTION
Patients' understanding of their medical problems is essential to allow them to make competent decisions, comply with treatment and enable recovery. We investigated Patients' understanding of orthopaedic terms to identify those words surgeons should make the most effort to explain.
METHODS
This questionnaire-based study recruited patients attending the orthopaedic clinics. Qualitative and quantitative data were collected using free text boxes for the Patients' written definitions and multiple choice questions (MCQs).
RESULTS
A total of 133 patients took part. Of these, 74% identified English as their first language. ‘Broken bone’ was correctly defined by 71% of respondents whereas ‘fractured bone’ was only correctly defined by 33%. ‘Sprain’ was correctly defined by 17% of respondents, with 29% being almost correct, 25% wrong and 29% unsure. In the MCQs, 51% of respondents answered correctly for ‘fracture’, 55% for ‘arthroscopy’, 46% for ‘meniscus’, 35% for ‘tendon’ and 23% for ‘ligament’. ‘Sprained’ caused confusion, with only 11% of patients answering correctly. Speaking English as a second language was a significant predictive factor for patients who had difficulty with definitions. There was no significant variation among different age groups.
CONCLUSIONS
Care should be taken by surgeons when using basic and common orthopaedic terminology in order to avoid misunderstanding. Educating patients in clinic is a routine part of practice.
Keywords: Orthopaedics, Communication, Health literacy, Patient education
Patients' understanding of their medical problems is integral to their ability to make competent decisions, comply with treatment and enable recovery. When using medical terminology, clear communication is crucial. We noted that common terms used in orthopaedic clinic consultations with patients were often being misunderstood. Musculoskeletal consultations often require the use of specialist terms that can be confusing to patients. We aimed to investigate Patients' understanding of these terms to identify those that patients found most confusing and that doctors should therefore make the most effort to explain.
Methods
This questionnaire-based study recruited consecutive patients above 15 years of age who attended the fracture and orthopaedic clinics at an inner city district general hospital in August 2010. Participants completed a questionnaire while waiting for their appointment. The age group of the patient and his or her perceived fluency in the English language were noted and those who did not speak English as a first language were identified.
Knowledge of common orthopaedic words was assessed using both qualitative and quantitative methods as questions were split into two sections. The first section asked participants to provide written definitions of the terms ‘fracture’, ‘broken bone’, ‘sprain’ and ‘strain’ in free text boxes. Our definitions were derived from a medical dictionary. Responses were coded as being ‘correct’, ‘almost correct’, ‘wrong or did not know’ and ‘gave no response’ (Table 1). The second section had six multiple choice questions (MCQs) asking patients to identify the correct definition of the terms ‘fracture’, ‘sprain’, ‘ligament’, ‘tendon’, ‘meniscus’ and ‘arthroscopy’ from five options.
Table 1.
Coding of free text definitions
| Correct | Almost correct | Wrong | No answer | |
|---|---|---|---|---|
| Fracture | Bone is broken into more than one piece | ‘Less severe than broken bone’; cracked/chipped/displaced/not completely broken | Damaged/bruised/dislocated/mention of soft tissue rather than bone damage/ other answer | Ticked box to say they did not know; no response |
| Broken bone | Bone is broken/fractured/snapped into more than one piece | ‘More severe than fracture’; properly broken/broken all the way through | Damaged/bruised/dislocated/mention of soft tissue rather than bone damage/ other answer | Ticked box to say they did not know; no response |
| Strain | Injury/stretch to muscle (need muscle in definition) | Injury to ligament/tendon | Bone/limb/joint problem/ no anatomy identified | Ticked box to say they did not know; no response |
| Sprain | Injury/stretch of ligament (need ligament in definition) | Injury to muscle/joint/tendon | Damage to bone/no anatomy included/answer related to swelling or amount of pain rather than injury itself | Ticked box to say they did not know; no response |
Patients were asked to answer the questionnaire alone without the aid of an interpreter although participants who had difficulty reading questions or writing answers (due to either physical disability or poor literacy skills in English) were able to ask friends or family to read out the questions and transcribe responses for them. The data were entered on an Excel® spreadsheet. Results were analysed using a chi-square test.
Results
Overall, 150 patients were recruited for the study and 133 patients agreed to participate. There was an even spread of patients in each age group category (age 15–30, 31–40, 41–50, 51–60 and over 60 years). Of those surveyed, 74% (98/133) identified themselves as having English as a first language and 88% (117/133) considered themselves to be fluent in English.
‘Broken bone’ was defined correctly in the free text section by 71% (94/133) of respondents, with 4% (5/133) of respondents being almost correct, 5% (6/133) being wrong, 16% (21/133) leaving no answer and 5% (7/133) who did not know. However, ‘fractured bone’ was defined correctly by only 33% (44/133), with 32% (43/133) of respondents defining it as a less severe injury than a broken bone and the remaining 35% (46/133) giving an answer that was either wrong or indicated that they did not know. ‘Sprain’ was correctly defined by 17% (23/133) of respondents', with 29% (38/133) being almost correct, 25% (33/133) being wrong and 29% (39/133) saying they did not know. The results for ‘strain’ were 39% (52/133), 12% (16/133), 24% (32/133) and 25% (33/133) respectively. There was a lot of confusion and crossover between the meanings of sprain and strain among patients (Fig 1).
Figure 1.
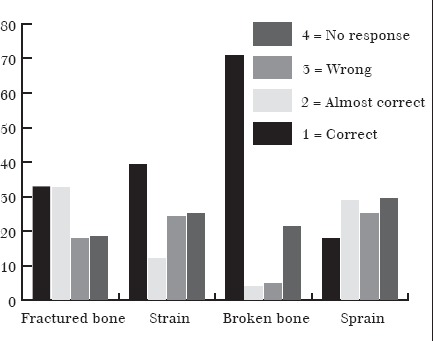
Responses to free text questions
In the MCQs, 51% (68/133) of respondents knew that a fracture meant that the bone was broken while 20% (26/133) believed it meant the bone was bruised and 6% (8/133) understood that a fracture meant the muscles had become detached from the bone. The meaning of arthroscopy was correctly identified by 55% (73/133), while 14% (18/133) believed an arthroscopy to be an x-ray of the knee. A torn meniscus was correctly identified correctly by 46% (61/133) as damage to the cartilage in the knee while 12% (16/133) believed it meant a torn muscle in the knee and 27% (36/13) were unsure of the meaning.
Uncertainty between the terms ‘tendon’ and ‘ligament’ was common. Of those surveyed, 35% (46/133) knew that a tendon joined muscle to bone but 16% (21/133) believed it joined bone to bone. Similarly, 23% (31/133) chose the correct definition for ligament while 40% (53/133) confused it with the definition for a tendon. ‘Sprained’ caused the most confusion with only 11% (14/133) answering correctly and 55% (73/133) choosing the answer ‘twisted’ (Fig 2).
Figure 2.
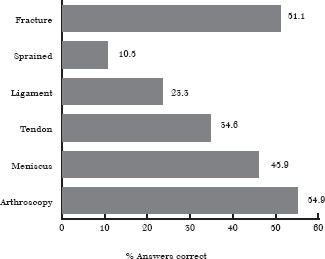
Responses to multiple choice questions
Speaking English as a second language was a statistically significant predictive factor for patients who had difficulty with definitions. In the free text questions, 81% (79/98) of native speakers gave a correct definition of the term ‘broken bone’ compared with 43% (15/35) of those for whom English was not a first language (p=0.023). Similarly, 47% (46/98) of those with English as a first language correctly defined ‘strain’ compared with 17% (6/35) (p=0.0154). In the MCQs, 41% (40/98) and 28% (27/98) of native speakers chose the correct definition of ‘tendon’ and ‘ligament’ respectively compared with 17% (6/35) and 11% (4/35) of people who did not speak English as a first language (p=0.041; p=0.089) (Fig 3). Of the patients who did not speak English as a first language, none had requested a hospital translator to be present. Some had brought an English-speaking relative with them to help with translation.
Figure 3.

Comparison of number of correct answers between patients for whom English is their first language and those for whom it is not
Using the chi-square test, there was no significant difference in the knowledge of orthopaedic terms between different age groups.
Discussion
Effective doctor–patient communication is directly related to increased patient satisfaction, better patient compliance with treatment and improved clinical outcomes.1 It has been suggested that effective communication in surgery can reduce postoperative complications and analgesic requirements, resulting in earlier discharge.2 Nonetheless, there is overwhelming evidence that communication between doctors and patients in all specialties is frequently overburdened by scientific jargon and complex medical phrases resulting in confusion and misunderstanding by the patient.3
Studies have shown that patients have poor understanding of medical terms used by doctors in various specialties. For example, in a study in an emergency department many patients were unable to match words such as haemorrhage and bleeding, heart attack and myocardial infarction.4 A gynaecological study found that only 68% of patients attending clinic for a ‘Pap smear’ knew what it was.5 Similarly, research done in general medicine and dermatology shows poor health literacy for commonly used words such as ‘arthritis’, ‘palpitations’, ‘the stomach’ and ‘the kidneys’.6 However, few studies have investigated orthopaedic terms.
Poor health literacy exists today despite improvements in health education, a growing media focus on health-related topics and increased access to the internet. Understanding of common medical terminology among patients has been shown to be very variable.7 Many patients do not know the location of key body organs, even those in which their medical problem is located.8 To compound this, studies show that doctors wrongly overestimate Patients' knowledge in as many as 41% of consultations; this has been shown to be true of both medical and surgical disciplines.2,9,10 Reduced levels of attention associated with illness and stress during a consultation only adds to Patients' poor understanding.
Our study demonstrates widespread misunderstanding of the most basic orthopaedic terms. Most patients have only a moderate grasp of meaning. A fractured bone was commonly seen to be a less severe form of injury than a broken bone. ‘Sprain’ and ‘strain’ were completely confused. We suggest that use of these terms is always clarified by a definition. Patients who did not speak English as a first language had the most difficulty; special attention should therefore be paid to this group of patients to avoid misunderstanding and poor patient outcomes. A greater use of interpreters is encouraged. Written information that patients can take home in a variety of languages may be helpful.
Patients who did not have English as a first language and had no translation assistance may have been disadvantaged in answering questions. Further study of this group with a hospital interpreter present would determine if translation assistance would change our findings. However, the aim of the study was to reflect the situation facing clinicians in a busy orthopaedic or fracture clinic when interpreters are not always requested or are unavailable.
The challenge of providing effective communication becomes ever greater with limited face-to-face consultation time in clinics, a wide variety of patients from different educational, socioeconomic and cultural backgrounds, and a proportion with limited English language skills. Furthermore, many individuals are embarrassed and will try to hide their limited knowledge, making it difficult for doctors to detect if a patient understands. Assumption of patient knowledge is one of the biggest barriers for successful communication. Williams et al designed a six-step guide for enhancing understanding and empowering patients to participate in healthcare; they suggest limiting information, using lay language and pictures to explain concepts, repeating instructions and applying a ‘teach back’ approach.11 As it is difficult to anticipate Patients' health literacy levels, doctors should use this approach and assume patients know less than they actually do to ensure the greatest possible level of patient understanding.
Conclusions
Our study shows that care should be taken when using basic and common orthopaedic terminology to avoid patient misunderstanding. Educational initiatives, either verbal or written, are needed to improve Patients' understanding of their diagnosis and to prevent confusion about their treatment. Clinicians should explain terms and assess patient understanding. Educating patients in clinic is a routine part of practice.
References
- 1.Williams N, Ogden J. The impact of matching the patient's vocabulary: a randomized control trial. Fam Pract. 2004;21:630–635. doi: 10.1093/fampra/cmh610. [DOI] [PubMed] [Google Scholar]
- 2.Richards J, McDonald P. Doctor–patient communication in surgery. J R Soc Med. 1985;78:922–924. doi: 10.1177/014107688507801109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gibbs RD, Gibbs PH, Henrich J. Patient understanding of commonly used medical vocabulary. J Fam Pract. 1987;25:176–178. [PubMed] [Google Scholar]
- 4.Lerner EB, Jehle DV, Janicke DM, Moscati RM. Medical communication: do our patients understand? Am J Emerg Med. 2000;18:764–766. doi: 10.1053/ajem.2000.18040. [DOI] [PubMed] [Google Scholar]
- 5.Blake DR, Weber BM, Fletcher KE. Adolescent and young adult women's misunderstanding of the term Pap smear. Arch Pediatr Adolesc Med. 2004;158:966–970. doi: 10.1001/archpedi.158.10.966. [DOI] [PubMed] [Google Scholar]
- 6.Boyle CM. Difference between Patients' and doctors' interpretation of some common medical terms. Br Med J. 1970;2:286–289. doi: 10.1136/bmj.2.5704.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thompson CL, Pledger LM. Doctor–patient communication: is patient knowledge of medical terminology improving? Health Commun. 1993;5:89–97. [Google Scholar]
- 8.Weinman J, Yusuf G, Berks R, et al. How accurate is Patients' anatomical knowledge: a cross-sectional, questionnaire study of six patient groups and a general public sample. BMC Fam Pract. 2009;10:43. doi: 10.1186/1471-2296-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hadlow J, Pitts M. The understanding of common health terms by doctors, nurses and patients. Soc Sci Med. 1991;32:193–196. doi: 10.1016/0277-9536(91)90059-l. [DOI] [PubMed] [Google Scholar]
- 10.Kelly PA, Haidet P. Physician overestimation of patient literacy: a potential source of health care disparities. Patient Educ Couns. 2007;66:119–122. doi: 10.1016/j.pec.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Williams MV, Davis T, Parker RM, Weiss BD. The role of health literacy in patient–physician communication. Fam Med. 2002;34:383–389. [PubMed] [Google Scholar]


