Abstract
Objective
To examine whether meta-cognitive psychological skills, acquired in MBCT are also present in patients receiving medication treatments for prevention of depressive relapse and whether these skills mediate MBCT's effectiveness.
Method
This study, embedded within a randomized efficacy trial of MBCT, was the first to examine changes in mindfulness and decentering during 6-8 months of antidepressant treatment and then during an 18 month maintenance phase where patients either discontinued medication and received MBCT, continued on antidepressants, or were switched to a placebo. A total of 84 patients (mean age 44, 58% female) were randomized to one of these three prevention conditions. In addition to symptom variables, changes in mindfulness, rumination and decentering were assessed during the phases of the study.
Results
Pharmacological treatment of acute depression was associated with reductions in Rumination and increased Wider Experiences. During the maintenance phase, only patients receiving MBCT showed significant increases in the ability to monitor and observe thoughts and feelings as measured by the Wider Experiences (p<.01) and Decentering (p<.01) subscales of the Experiences Questionnaire and Toronto Mindfulness Scale. In addition, changes in Wider Experiences (p<.05) and Curiosity (p<.01) predicted lower HRSD scores at 6 months follow up.
Conclusions
An increased capacity for decentering and curiousity may be fostered during MBCT, and underlie its effectiveness. With practice, patients can learn to counter habitual avoidance tendencies and to regulate dysphoric affect in ways that support recovery.
Keywords: MBCT, meditation, relapse prevention, depression, maintenance pharmacotherapy
Mindfulness Based Cognitive Therapy (MBCT) is an 8 week group treatment for prevention of relapse in unipolar depression that integrates elements of cognitive therapy for depression with the clinical application of mindfulness meditation (Segal, Williams, & Teasdale, 2002). Randomized trials of MBCT have reported consistent reductions in relapse rates on the order of 50% compared to usual care in remitted, nonmedicated depressed patients with multiple previous episodes of depression (Teasdale et al., 2000), or equivalent protection when compared to maintenance antidepressant treatment (Kuyken et al., 2008). The development of MBCT was informed by empirical studies showing that relapse was strongly associated with the reinstatement of automatic modes of cognitive processing, such as rumination and avoidance, that are characteristic of the depressed state. Following this account, patients in MBCT are taught to become more aware of, and to relate differently to potentially depressogenic thoughts, feelings, and bodily sensations.
Qualitative analyses of MBCT suggest that one characteristic of this new relationship to mental contents is the development of skills in decentering, allowing patients to observe their thoughts and feelings as temporary, objective events in the mind, instead of seeing them as being true or descriptive of self (Allen et al., 2009). Furthermore, although MBCT was designed to train these specific attentional skills as a response to mood-linked processing biases, it is not at all clear if these types of changes would be present in other treatments such as antidepressant medication. It may be that medication prevents relapse solely by altering somatic illness markers, but it is equally possible that reductions in depression resulting from any effective treatment would increase scores on meta-cognitive variables. To date, the question of treatment specificity remains unaddressed.
While the related literature on treatment mediation in MBCT indicates that changes in decentering, rumination, mindfulness, and compassion are important aspects of the process by which depression is prevented, it is unclear whether the changes are unique to MBCT. For example, Michalak et al. (2008) reported that higher post-treatment levels of mindfulness were associated with lower rates of relapse/recurrence over a 12 month follow up. Shahar and colleagues (2010) studied partially remitted depressed patients who were randomly assigned to either MBCT or a wait list control and found that the use of informal mindfulness practices and reductions in brooding independently accounted for the effects of MBCT on reducing depressive symptoms. These studies are less informative regarding treatment specificity because the former lacked a control group, while the latter did not examine prophylaxis. In a more comprehensive study, Kuyken et al., (2010) reported treatment specific increases in mindfulness and self-compassion for patients receiving MBCT compared to antidepressant medication (ADM). Most recently, Segal et al., (2010) studied patients who were initially treated with an antidepressant and were then randomized to either discontinue their medication in order to receive MBCT, continue taking their medication for 18 months, or were switched to placebo (PLA). They found that, compared to PLA, patients characterized by an unstable pattern of remission1 showed a 73% reduction in relapse risk when they received MBCT or ADM. Moreover, ADM and MBCT performed equivalently in the study (Segal et al., 2010).
The present study was embedded within this larger efficacy trial and took advantage of its 3-arm design to examine treatment specific changes in mindfulness and decentering, while considering their relation to symptom return. This is the first study to examine changes in these constructs during 6-8 months of ADM for acute depression and then during the maintenance phase, in MBCT, maintenance ADM and PLA conditions. This makes it possible to examine changes in decentering and mindfulness in treatments that rely on markedly different modes of action and over two distinct treatment phases. Kraemer's conceptual model for the analysis of treatment mediation in randomized trials was used to further examine these variables (Kraemer et al., 2008). As this is the first study to examine changes in decentering and mindfulness during pharmacotherapy for acute depression, we made no specific prediction about whether these variables would change during this study phase. We did predict, however, that MBCT would lead to increased decentering and mindfulness compared to maintenance ADM or PLA and that these changes would be related to depression outcomes following treatment.
Methods
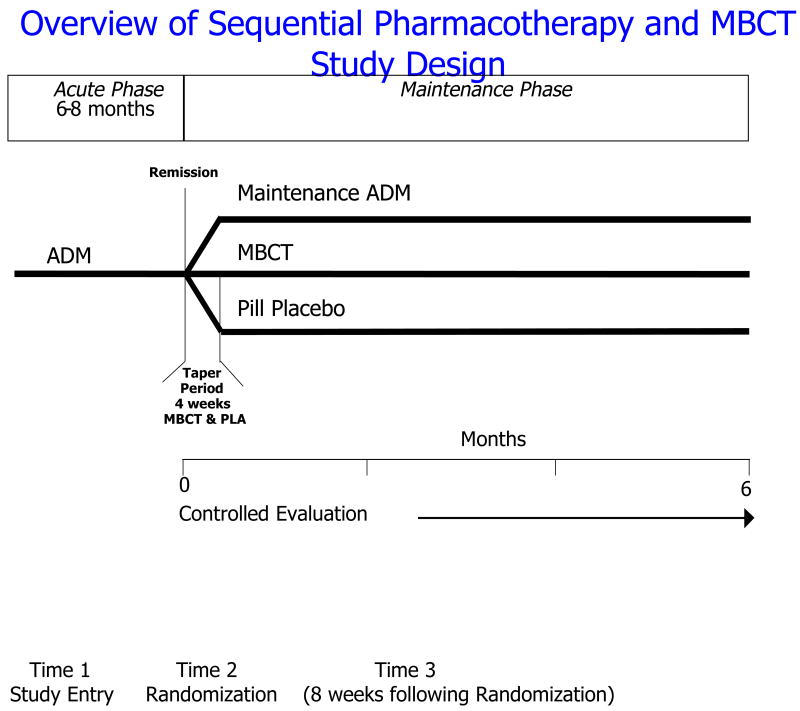
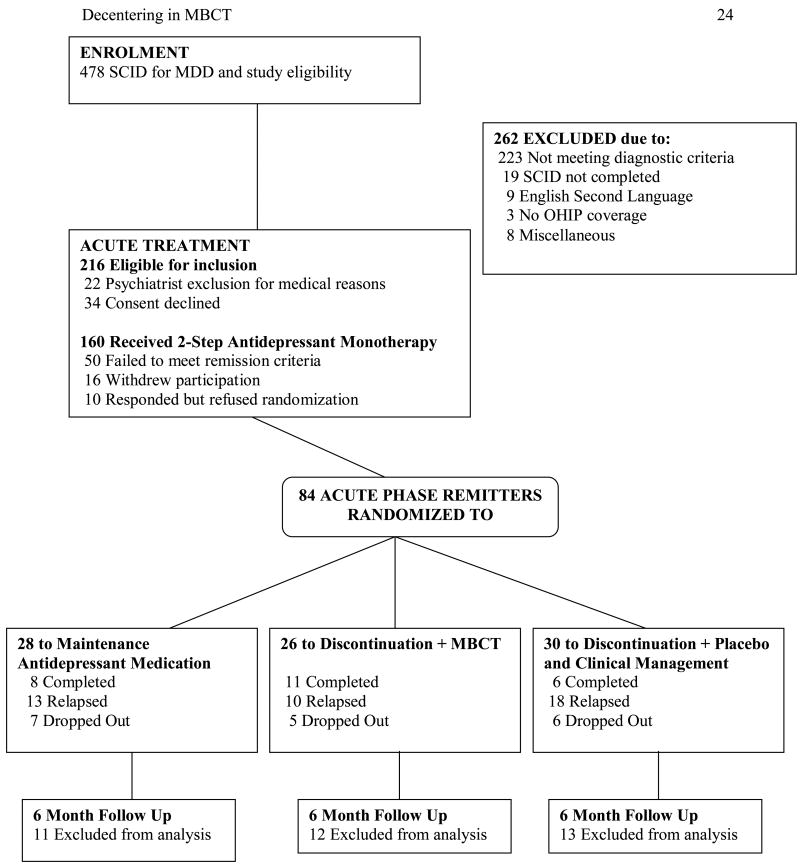
The study protocol was approved by IRBs at the Centre for Addiction and Mental Health (CAMH), Toronto and St. Joseph's Healthcare, Hamilton, was monitored by a DSMB and all participants provided written consent prior to any research activity. A total of 84 out of 160 (52.5%) participants who were treated with ADM achieved clinical remission and were assigned to one of the 3 study conditions (see Figures 1 and 2).
Figure 1.
Overall study design schematic and subject flow.
Figure 2. Study Flow of Patients from Screening to Analysis.
Participants and Study Flow
Inclusion criteria were a DSM-IV diagnosis of Major Depressive Disorder (MDD), a score of ≥ 16 on the Hamilton Depression Rating Scale (HRSD-17), two or more previous depressive episodes, and between 18 and 65 years in age.2 All patients were treated with a 2 step, standardized monotherapy algorithm designed to maximize the likelihood of treatment response; patients who failed to respond to initial treatment with an SSRI (citalopram or sertraline) were given the option of receiving an SNRI (venlafaxine or mirtazapine; Segal et al., 2010). All measures described in this study were administered at study enrolment (Time 1). Acute phase treatment was continued until the patient achieved clinical remission (defined as a 50% reduction in HRSD and HRSD ≤ 7 for 8 weeks) and was then extended for five months to ensure remission was sustained. Patients were then randomly assigned to one of the three study arms: maintenance antidepressant medication (ADM), medication taper plus MBCT, or medication taper plus placebo (PLA). At randomization, the symptom, decentering and mindfulness measures were repeated to assess change from entry (Time 2). Patients in MBCT attended 8 weekly 2 hour groups and a 6 hour retreat day in week 6. Details of the treatment protocol and fidelity are provided in Segal et al. (2010). All measures were repeated at 8 weeks in all arms of the study (Time 3) to coincide with the end of treatment for the 8 session MBCT. Symptom and relapse status were then assessed for a maximum of 18 months during the follow-up phase, and data collection ceased when participants relapsed because they were re-treated. Depressive symptoms were assessed using the HRSD score at 6 months after Time 3, as this provided a sufficient number of observations for analysis.
Outcome Measures
Hamilton Rating Scale for Depression
(HRSD; Hamilton, 1960). Patients were assessed on the 17-item HRSD by clinical evaluators blind to treatment allocation over the 6-8 month acute treatment and 18 month maintenance phase. The HRSD demonstrates high reliability and validity coefficients.
Mindfulness Skills: Toronto Mindfulness Scale
(TMS; Lau et al., 2006). This 10 item measure is completed after an instructional prime that asks respondents to engage in experiential awareness for 15 minutes. Participants are asked to indicate their level of agreement with items reflecting curiosity and decentering – the two TMS subscales. The curiosity scale contains items that reflect an attitude of approaching and investigating one's experience without judgment. The decentering scale contains items that reflect a shift away from identifying personally with thoughts and feelings to observing their movement in a wider field of awareness and accepting the experience as it is. The TMS has adequate internal consistency and validity; in our sample alpha was .89 for decentering and .83 for curiosity at Time 1.
Experiences Questionnaire
(EQ; Fresco et al. (2007). The EQ is a 20 item self-report scale designed to measure wider-experiences and rumination. The Wider Experiences scale (EQ-W) is defined as the ability to observe one's thoughts and feelings as temporary, objective events in the mind, as opposed to true reflections of the self. Items with a negative valence were included on the scale to form a Rumination scale (EQ-R), which is reverse scored. Fresco et al., (2007) have reported acceptable reliability and convergent and discriminant validity coefficients; in our sample, the alpha coefficient was .86 for EQ-R and .85 for EQ-W at Time 1.
Results
Participant Characteristics
Information on patient demographics is presented in Table 1. Patients had a mean age of 44 years (11.49) at study entry and 58% of the sample was female, with 20% self-identified as a member of an ethnic/racial minority group. At study randomization (Time 2), 84 remitted patients were assigned to the three treatment groups, 28 in ADM, 26 in MBCT, and 30 in PLA. At the six month time point data for 48 patients were available on all measures, 17 in the ADM, 14 in the MBCT, and 17 in the PLA group. There were no differences in baseline characteristics between the three prevention arms, the only exception being a greater percentage of Axis II comorbidity in MBCT (p<.05). Demographic and symptoms variables were also compared between participants who completed all follow-up assessments and those who did not; there were no significant differences between groups or in the proportion of missing data in each study arm.
Table 1. Baseline Characteristics of The Three Prevention Conditions.
| Variable | M-ADM (n=28) | MBCT (n=26) | PLA+Clin (n=30) |
|---|---|---|---|
| Gender: Female, % | 71.4 | 50.0 | 66.7 |
| White, % | 85.7 | 73.1 | 76.7 |
| Age, yrs | 45.8 ± 11.4 | 44.8 ± 9.4 | 41.9 ± 11.6 |
| Married/cohabitating, % | 36 | 39 | 40 |
| Employed, % | 79 | 77 | 62 |
| Age of first onset | 34.6 ± 12.7 | 28.78 ± 10 | 29.9 ± 11.3 |
| No. of prior episodes | 4.9 ± 2.6 | 4.5 ± 2.2 | 4.8 ± 2.1 |
| Duration of current episode in weeks | 80.7 ± 111.6 | 102.6 ± 92.2 | 67.8 ± 101.1 |
| Days in acute phase | 231.4 ± 59.7 | 228 ± 52.6 | 239.7 ± 34.2 |
| Days to reach remission | 80.1 ± 60 | 68.1 ± 51.9 | 90 ± 57.8 |
| Days in remission | 151.3 ± 31.7 | 160 ± 34.2 | 149.7 ± 44.5 |
| Hx of prior antidepressant, % | 61 | 54 | 52 |
| Hx psychiatric hospitalization, % | 7 | 4 | 10 |
| Any Axis I comorbidity, % | 39 | 35 | 27 |
| Hx substance abuse/dependence, % | 4 | 4 | 10 |
| Any Axis II comorbidity, % | 18 | 58 | 37* |
Note.
p < .05
Descriptive Data
Table 2 displays the intercorrelations3, means, and standard deviations for all measures. Generally, these correlations suggested that the EQ and TMS subscales correlated within themselves over the different time points and with one another, suggesting some overlap in these measures and consistency over time in these meta-cognitive variables. Participants with missing T3 data, including those who dropped out of the study or relapsed before 6 months, needed to be removed from this analysis. For three individuals, missing EQ data was estimated- data from week six of the maintenance phase was used to estimate the week eight observation.
Table 2. Descriptive Statistics and Correlations Among Measures.
| T1 HRSD | T2 HRSD | T3 HRSD | T1 EQ-R | T2 EQ-R | T3 EQ-R | T1 EQ-W | T2 EQ-W | T3 EQ-W | T1 TMS-C | T2 TMS-C | T3 TMS-C | T1 TMS-D | T2 TMS-D | T3 TMS-D | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T2 HRSD | .20 | ||||||||||||||
| T3 HRSD | -.07 | .02 | |||||||||||||
| T1 EQ-R | -.18 | -.04 | -.09 | ||||||||||||
| T2 EQ-R | -.03 | -.18 | -.18 | .44* | |||||||||||
| T3 EQ-R | -.08 | -.06 | -.20 | .60* | .70* | ||||||||||
| T1 EQ-W | .01 | .07 | -.20 | .20 | .23 | .42* | |||||||||
| T2 EQ-W | .07 | -.25 | -.07 | .23 | .36* | .30 | .20 | ||||||||
| T3 EQ-W | .12 | -.01 | .15 | .03 | .20 | .21 | .27 | .40* | |||||||
| T1 TMS-C | .29 | -.16 | .24 | -.20 | .24 | .09 | .26 | .48* | .21 | ||||||
| T2 TMS-C | .17 | -.02 | -.23 | -.08 | .03 | -.03 | .19 | .30 | .02 | .58* | |||||
| T3 TMS-C | .02 | .30 | .19 | -.19 | -.16 | -.23 | .08 | .01 | .23 | .01 | .44* | ||||
| T1 TMS-D | .27 | -.10 | .34* | .09 | .29 | .28 | .26 | .28 | .15 | .73* | .54* | -.24 | |||
| T2 TMS-D | .08 | -.15 | -.10 | -.03 | -.08 | -.05 | .12 | .22 | .21 | .45* | .58* | .13 | .52* | ||
| T3 TMS-D | .07 | .14 | -.13 | -.14 | -.10 | -.19 | -.12 | .04 | .31 | -.17 | .29 | .51* | .07 | .44* | |
| M | 19.10 | 2.79 | 4.29 | 16.05 | 18.61 | 18.64 | 25.53 | 34.10 | 33.57 | 9.97 | 11.18 | 11.30 | 11.18 | 13.79 | 14.84 |
| SD | 3.06 | 1.84 | 3.64 | 2.96 | 3.28 | 3.46 | 5.64 | 6.92 | 8.42 | 6.63 | 5.92 | 6.13 | 5.18 | 6.67 | 6.54 |
Note. T1 = Time 1 (Study Entry); T2 = Time 2 (Randomization); T3 = Time 3 (HRSD: 6 months following treatment; EQ or TMS: 8 weeks following randomization); EQ-R= Experiences Questionnaire, Rumination; EQ-W= Experiences Questionnaire, Wider Experiences; TMS-C= Toronto Mindfulness Scale, Curiosity; TMS-D = Toronto Mindfulness Scale, Decentering; HRSD= Hamilton Rating Scale for Depression.
p<.01.
Changes in EQ & TMS During Antidepressant Acute Treatment Phase (Time 1 to Time 2)
To examine change in the subscales of the EQ and TMS from Time 1 (study enrolment) to Time 2 (randomization), Table 3 compares the scores on the EQ, TMS and HRSD during the acute antidepressant treatment. Paired sample t-tests were used to examine whether these mean scores were significantly different. As expected, there were significant differences between the HRSD scores (t80 = 39.91, p<.001), d = 6.40 between study entry (M = 19.1, SD = 3.1) and randomization (M = 2.8, SD = 1.8). Similarly, significant differences were demonstrated for the EQ-R scores (t66 = -6.58, p<.001), d = -0.26 and EQ-W scores (t66 = -8.68, p<.001), d = -1.34. However, significant differences were not found for the TMS Curiosity and Decentering subscales. To examine whether the changes in EQ Rumination and Wider Experiences were attributable to change in depression, a hierarchical regression was conducted; the dependent variable used was the T2 HRSD (randomization). Predictors were entered in two blocks, T1 HRSD (intake) in the first block, residualized change in the EQ subscales (calculated from Time 1 (intake) to Time 2 (randomization)) in the second block. After controlling for change in depression scores, changes in the EQ subscales were no longer significant.
Table 3. Means (and Standard Deviations) of EQ, TMS and HRSD During Acute Phase Antidepressant Treatment (N=84).
| Variable | M (and SD) Time 1 (Study Entry) | M (and SD) Time 2 (Randomization) | Paired t-test | Cohen's d |
|---|---|---|---|---|
| EQ Rumination | 16.05 (2.96) | 18.61 (3.28) | t66 = -6.58*** | -0.26 |
| EQ Wider Experiences | 25.53 (5.64) | 34.10 (6.92) | t66 = -8.68*** | -1.34 |
| TMS Curiosity | 9.97 (6.63) | 11.18 (5.92) | t33 = -1.42 | -0.19 |
| TMS Decentering | 11.18 (5.18) | 13.79 (6.67) | t33 = -1.17 | -0.21 |
| HRSD | 19.1 (3.1) | 2.8 (1.8) | t80 = 39.91*** | 6.40 |
p < 0.001
Note. EQ= Experiences Questionnaire, TMS= Toronto Mindfulness Scale, HRSD= Hamilton Rating Scale for Depression. Effect sizes calculated using the following formula: Cohen's d = Mpre-Mpost/SDpooled; large effect size equals > 0.8; medium effect size equals > 0.5; small effect size equals > 0.2.
Changes in EQ & TMS During Maintenance Treatment (Time 2 to Time 3)
Treatment specific changes in EQ and TMS were examined across the three prevention conditions, Table 4 displays the means for each measure from randomization to 8 weeks post randomization (corresponding with the end of MBCT treatment). A one-way ANOVA examined standardized residualized change scores for the four subscales of the TMS and EQ, by treatment group. Results indicated that changes in both TMS-D (F (2,46) = 10.31; p <.01) and EQ-W (F(2,55) = 6.67; p <.01) differed significantly based on treatment group. Post-hoc Tukey's HSD tests indicated a significant increase in TMS Decentering and EQ Wider Experiences for participants in the MBCT condition at the .05 level of significance.
Table 4. Means (and Standard Deviations) of EQ and TMS in the Three Prevention Conditions at Randomization and 8 Weeks Later.
| Time 2 (Randomization) | Time 3 (8 weeks post randomization) | |
|---|---|---|
| Experiences Questionnaire - Rumination | ||
| Medication (N=17) | 19.12 (2.83) | 19.05 (3.36) |
| Placebo (N=15) | 19.53 (2.20) | 19.33 (2.66) |
| MBCT (N=15) | 17.40 (4.10) | 17.73 (3.91) |
| Experiences Questionnaire – Wider Experiences | ||
| Medication (N=17) | 34.82 (6.09) | 34.35 (5.80) |
| Placebo (N=15) | 34.92 (7.65) | 30.80 (8.86) |
| MBCT (N=15) | 32.25 (6.95) | 37.21 (7.83)* |
| Toronto Mindfulness Scale - Curiosity | ||
| Medication (N=14) | 13.33 (4.3) | 11.07 (4.5) |
| Placebo (N=15) | 11.61 (5.5) | 10.00 (7.1) |
| MBCT (N=18) | 9.93 (6.8) | 13.20 (7.0) |
| Toronto Mindfulness Scale - Decentering | ||
| Medication (N=14) | 16.73 (3.8) | 14.07 (5.4) |
| Placebo (N=15) | 12.44 (6.1) | 12.00 (6.8) |
| MBCT (N=18) | 13.53 (8.2) | 19.67 (5.2)* |
Note.
p < .05, one-way ANOVA on standardized residualized change scores for the four subscales of the TMS and EQ by treatment group followed by post-hoc Tukey's HSD tests.
Treatment Specific Changes in EQ and TMS and Prediction of Depressive Symptoms
Kraemer et al. (2008) propose a regression approach to mediation in which the treatment group, the candidate mediator, and the group by mediator interaction term are independent variables. In the current study, we examined treatment outcome by examining the change in depressive symptoms between the pre-treatment randomization session (T2 HRSD) and the six month follow-up (T3 HRSD) using hierarchical linear regression.4
To ensure that any mediation effects were present over and above the influence of depression severity, our regression models included T2 HRSD depression severity in the first step. Kraemer et al. (2008) emphasize the need for a treatment group variable to be coded as deviations from a central value (i.e., zero), and to center the mediator (i.e., zero) in order to reduce collinearity in interaction terms and to aid with interpretation; therefore, in our current analyses, the treatment group variable was recoded (-1, 0, 1) while potential mediators were computed as standardized residualized change scores, centered at zero.5
To determine whether changes in the mediator variables predicted depression symptom change, when controlling for known predictors, a series of regression equations were constructed.6 The dependent variable in these analyses was the HRSD score 6 months after randomization. We opted to use this time point because it allowed us to retain sufficient participants (see Figure 2). Our protocol required us to immediately re-treat any participant who relapsed during the maintenance phase which meant that they were censored for the purpose of further analyses. Predictors were entered in three blocks; HRSD score at randomization in the first block, treatment condition (MBCT, ADM, PLA) and residualized change in the mediator (T2 for the mediator was at randomization and T3 for the mediator was always 8 weeks later) in the second block. The third block contained two interaction terms, each involving the residualized change score with the three conditions dummy coded to represent a comparison of a) MBCT and ADM and b) active treatment (i.e., MBCT, ADM) versus placebo. Four regression equations for the EQ and TMS subscales were created. There were no significant predictors of 6 month HRSD score in the regression equation for EQ-rumination. For EQ-wider experiences, the interaction term for the standardized residual of MBCT versus ADM was significant, beta = .49, t = 2.43, p < .05 and there was a trend for the wider experiences standardized residual overall, p < .10. There were no significant predictors for TMS-Decentering. For TMS-Curiosity, the standardized residual was a significant predictor, beta = .41, t = 2.32, p < .05, as was the interaction term for the standardized residual of MBCT versus ADM, beta = .57, t = 3.15, p < .01. Thus, changes in wider experiences and curiosity were associated with lower HRSD scores when comparing MCBT versus ADM. In order to be comprehensive, several additional treatment group contrasts were examined (e.g., MBCT vs. PLA, ADM vs. PLA) using this analytical framework; no significant group by mediator interactions emerged.
Discussion
In this study, we examined whether the psychological skills acquired in MBCT are also present in patients receiving somatic treatments for prevention of depressive relapse and whether these skills mediate MBCT's effectiveness. During the acute phase of the study, depressed patients who received ADM experienced decreased rumination and increased wider experiences. Our analysis suggested that these changes were a by product of overall reductions in depressive symptoms. However, the absence of a control group tempers this interpretation, and since this is the first study to examine metacognitive change during ADM treatment, clarifying the nature of treatment specific changes warrants further investigation.
During the maintenance phase of the study (when pharmacologically remitted patients were randomized to one of the three prevention conditions), we found that both Wider Experiences and Decentering increased in MBCT but did not change in either ADM or PLA. Finally, examining the relationship between these meta-cognitive variables and clinical outcomes, we found that changes in Wider Experiences and Curiosity predicted HRSD scores at 6-month follow-up. Although Decentering changed in MBCT, this did not predict depressive symptoms at the 6 month follow-up. Also surprising, rumination (which was reduced significantly during acute treatment in the study), did not demonstrate MBCT specific changes and did not predict subsequent symptoms. This is not consistent with previous findings regarding rumination, and might reflect psychometric issues specific to the EQ measure.
One account of MBCT's effectiveness is that mindfulness training facilitates exposure based learning and extinction (Treanor, 2011). When patients encounter aversive emotional states, decentering allows them to label and observe the experience, while curiosity maintains the experience in attentional focus on a moment to moment basis. Our results also raise some intriguing questions about the EQ and TMS measures of mindfulness. While both Wider Experiences and Curiosity were associated with outcome; their intercorrelations over the various time points suggest that the items on these scales may be measuring distinct constructs. Perhaps this reflects state (TMS) versus trait (EQ) differences in how these questionnaires were designed, or this speaks to the need to use multi-dimensional measures to assess a multifaceted construct such as mindfulness. At minimum, identifying which item content is unique to each measure (kindness, compassion in the EQ) and which item content overlaps on the TMS and EQ (non-identification with thinking) is needed and will help to clarify the link between mindfulness training and depression prognosis.
This study has several limitations. Because the investigation was a secondary analysis from the larger MBCT efficacy trial (Segal et al., 2010) the amount of information we gathered was restricted. For example, the ethical need to quickly re-treat participants who relapsed reduced both our sample size and statistical power. Additionally, since ADM was tapered during the first 4 sessions of MBCT, the learning of new skills during this period occurred concurrently with ADM withdrawal. It is possible that preoccupation with discontinuation symptoms, which were noted by the MBCT therapists, affected how the participants in this study responded to the EQ and TMS scales. Finally, the mindfulness measures may have had demand characteristics given that the content of items does relate to the material discussed and experienced in the MBCT group.
Our findings suggest that an increased capacity for decentering and curiosity may be particularly useful in preventing relapse. As others have found, relationships to negative thoughts may be as, or more, important than belief in thought content (e.g., Teasdale et al., 2002). Future studies would do well to chart the path by which patients utilize these skills to adopt lifestyle and behavioural strategies that support recovery.
Table 5. Interactive Effects of Potential Mediators in the Prediction of Depressive Symptoms from Randomization to 6 Month Follow-up.
| Order of Entry | Predictor | B | beta | t | p | Cumulative R2 | F for Increment in R2 for set | df | Partial Correlation (pr) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | HRSD T2 | .39 | .24 | 1.34 | .19 | .06 | .19 | 1,34 | .08 |
| 2 | Δ EQ-Wider | 1.29 | .27 | 1.59 | .12 | .09 | 1.43 | 2,32 | ..10 |
| Group | -1.35 | -.25 | -1.54 | .13 | -.24 | ||||
| 3 | Δ EQ-Wider x Group | 2.38 | 1.13 | .39 | .04 | .21 | 4.45* | 1,31 | .35 |
| 1 | HRSD T2 | .17 | .12 | .70 | .69 | .01 | .37 | 1,31 | .13 |
| 2 | Δ TMS-Curiosity | 1.38 | .37 | 2.07 | .05 | .08 | 1.26 | 2,29 | .36 |
| Group | -.97 | -.20 | -1.22 | .23 | -.23 | ||||
| 3 | Δ TMS-Curiosity x Group | 2.30 | .48 | 2.70 | .01 | .19 | 7.30** | 1,28 | .45 |
Note.
p < 0.05;
p < 0.01;
p < 0.001
Note. EQ= Experiences Questionnaire, TMS= Toronto Mindfulness Scale, HRSD T2 = Hamilton Rating Scale for Depression, randomization session (pre-treatment). Group = Mindfulness Based Cognitive Therapy (MBCT), Medication, Placebo. Δ = standardized residualized change in mediator variable from randomization to post treatment (i.e., eight weeks). All analyses use depression severity (HRSD T3 6 months) as the outcome.
Acknowledgments
This study was funded by Grant #066992 (R01: Dr. Segal) from the National Institute of Mental Health, Bethesda, MD.
We thank the following colleagues for contributing to this research. Robert Cook, Lawrence Martin and Jennifer Brasch served as study psychiatrists. Shelly Ferris, Kate Szacun-Shimizu, and Karyn Hood served as study coordinators. Susan Woods and Theresa Casteels served as MBCT study therapists. Lori Hoar, Joanne Nault, Rebecca Pedersen and Zoe Laksman served as project interviewers, Bao Chau Du and Heidy Morales provided research support. Tom Buis and Andrew Pedersen provided programming and data analytic support. David Streiner provided statistical and study design consultation.
Footnotes
In the parent trial, participants who remitted were classified as having had either an unstable or stable remission, based on the presence or absence of ‘symptom flurries’ during the approximately 5 months between initial remission and randomization. Patients who had a stable remission were those who maintained an HRSD score of ≤ 7 across this interval, while unstable remitters achieved the same HRSD threshold but had occasional elevated scores across this interval that were not sufficient to qualify for relapse. These patients were considered in remission if 1) their score subsequent to an elevation was ≤ 7 and 2) the range of elevated scores fell between 8 and 14. This classification divided the entire sample in half (49% stable remitters and 51% unstable remitters).
Patients were excluded if they had a current diagnosis of Bipolar Disorder, Substance Abuse Disorder, Schizophrenia or Borderline Personality Disorder or a trial of ECT within the past six months, or currently practiced meditation more than once per week or yoga more than twice per week. A full description of inclusion and exclusion criteria, treatment fidelity, and can be found in Segal et al., (2010).
Given the nature of this study, the range of T2 HRSD and T3 HRSD would be restricted since only participants who fully remitted were retained in this study. The correlations displayed may underestimate the relation between the other variables.
In order to demonstrate mediation, the TMS and EQ must be measured during treatment, be significantly altered by treatment, and must temporally precede the outcome. Further, the mediator must also then show a main and/or interactive effect with treatment on outcome; (i.e., the mediator and/or interaction term in the regression should be significant) while treatment need not have a significant overall or main effect on outcome. A main effect of mediation is demonstrated when treatment significantly changes the mediator but the effect of the mediator on outcome does not significantly differ across treatment types. In contrast, an interactive mediation effect occurs when treatment not only significantly impacts on the mediator but also changes the relationship between the mediator and outcome such that it differs across treatments. In the present study, an interactive effect would demonstrate that treatment significantly affects the development of mindfulness skills, and that the relationship between our mediator and symptom change differs across treatments.
Given that there are a limited number of contrasts possible, these analyses compared MBCT to Medication, with Placebo as the baseline condition (e.g., -1, 1, 0); however, it should be noted that several alternative comparisons that were considered (e.g., ADM compared to PLA, MBCT compared to PLA) were not found to be significant,.
In the parent trial, nature of remission (stable vs. unstable) was an important factor in subsequent relapse and efficacy of the three conditions. However, this had no significant impact in any of our analyses related to changes in meta-cognitive variables and symptom change.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
Contributor Information
Peter J. Bieling, St. Joseph's Healthcare, Hamilton, Ontario
Lance L. Hawley, Centre for Addiction and Mental Health, Toronto, Ontario
Richard T. Bloch, Centre for Addiction and Mental Health, Toronto, Ontario
Kathleen M. Corcoran, Centre for Addiction and Mental Health, Toronto, Ontario
Robert D. Levitan, Centre for Addiction and Mental Health, Toronto, Ontario
L. Trevor Young, University of Toronto.
Glenda M. MacQueen, University of Calgary
Zindel V. Segal, Centre for Addiction and Mental Health, Toronto, Ontario
References
- Allen M, Bromley A, Kuyken W, Sonnenberg S. Participants' experiences of mindfulness-based cognitive therapy: “It changed me in just about every way possible”. Behavioral and Cognitive Psychotherapy. 2009;37:413–30. doi: 10.1017/S135246580999004X. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Moore MT, Dulmen MHM, Segal ZV, Ma SH, Teasdale JD, et al. Initial psychometric properties of the Experiences Questionnaire: Validation of a self-report measure of decentering. Behavior Therapy. 2007;38:234–246. doi: 10.1016/j.beth.2006.08.003. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychology. 2008;27(Suppl 2):S101–S108. doi: 10.1037/0278-6133.27.2(Suppl.).S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuyken W, Watkins E, Holden E, White K, Taylor RS, Byford S, et al. How does mindfulness-based cognitive therapy work? Behaviour Research and Therapy. 2010;48:1105–1112. doi: 10.1016/j.brat.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Lau MA, Bishop SR, Buis T, Anderson ND, Carlson L, et al. The Toronto mindfulness scale: Development and validation. Journal of Clinical Psychology. 2006;62:1445–1467. doi: 10.1002/jclp.20326. [DOI] [PubMed] [Google Scholar]
- Michalak J, Heidenreich T, Meibert P, Schulte D. Mindfulness predicts relapse/recurrence in major depressive disorder after mindfulness-based cognitive therapy. Journal of Nervous and Mental Disease. 2008;196:630–633. doi: 10.1097/NMD.0b013e31817d0546. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Bieling PJ, Young T, MacQueen G, Cooke R, Martin L, et al. Antidepressant monotherapy versus sequential pharmacotherapy and Mindfulness-Based Cognitive Therapy, or placebo, for relapse prophylaxis in recurrent depression. Archives of General Psychiatry. 2010;67:1256–1264. doi: 10.1001/archgenpsychiatry.2010.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Williams JM, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York: Guilford Press; 2002. [Google Scholar]
- Shahar B, Britton WB, Sbarra D, Figueredo AJ, Bootzin RR. Mechanisms of change in Mindfulness-Based Cognitive Therapy for depression: Preliminary evidence from a randomized controlled trial. International Journal of Cognitive Therapy in press. [Google Scholar]
- Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, Segal ZV. Metacognitive awareness and prevention of relapse in depression: empirical evidence. Journal of Consulting and Clinical Psychology. 2002;70:275–287. doi: 10.1037//0022-006x.70.2.275. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology. 2000;68:615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- Treanor M. The potential impact of mindfulness on exposure and extinction learning in anxiety disorders. Clinical Psychology Review. 2011;31:617–625. doi: 10.1016/j.cpr.2011.02.003. [DOI] [PubMed] [Google Scholar]