Introduction
Cerebrotendinous Xanthomatosis (CTX) is an autosomal recessive disorder of bile acid synthesis1. At least 50 different causative mutations have been identified in the CYP27A1 gene encoding for a sterol 27-hydroxylase important in bile acid synthesis2. Sterol 27-hydroxylase deficiency leads to 5α-cholestanol accumulation in the blood and tissues of affected patients1, including brain, often leading to severe neurological dysfunction that can incapacitate patients by the 4th–5th decade of life1. CTX generally presents clinically in the 2nd–3rd decade; childhood signs and symptoms can include chronic diarrhea, juvenile cataracts, school failure1,3, and potentially xanthomas1. Eighty-five percent of CTX patients develop cataracts of multiple types2, reported to occur as young as age 5–6 years1, with cataracts and chronic diarrhea commonly presenting before neurologic disease3. For this reason, and since diarrhea is non-specific, the clinician may not consider a diagnosis of CTX when cataracts are identified.
Treatment for CTX is available in the form of chenodeoxycholic acid (CDCA)1,4. The FDA recently reapproved CDCA (Manchester Pharmaceuticals, Inc). As treatment of CTX from the preclinical stage prevents the onset of disease complications4, the value of early diagnosis for this disorder cannot be overstated. We describe two cases of CTX affected children enrolled in an IRB approved study at OHSU with bilateral cataracts as presenting signs of disease.
Case 1
A 9 year old female was referred to an ophthalmologist for decreased vision over several months. Past ocular history was unremarkable; full ocular exam 2 years prior was normal. Family history was unremarkable. Past medical history was significant for diarrhea and nonverbal learning disorder. On examination uncorrected distance visual acuity was 20/80 and uncorrected near acuity was 20/50 in each eye. Manifest refraction was 0.75+0.50X90 in each eye, with corrected distance acuity of 20/60 in the right and 20/80 in the left. Complete dilated exam was remarkable for the presence of cataract in each eye and described as a diffuse nuclear haze on slit lamp examination, with mild posterior capsular opacification (figure 1). Retroillumination highlighted posterior capsular findings (figure 2). Sequential bilateral cataract surgery with intraocular lens placement resulted in a corrected visual acuity of 20/20 in each eye. A metabolic workup indicated plasma 5α-cholestanol was markedly elevated at 3.7 mg/dl (normal < 0.2 mg/dl1), suggestive of CTX. Urine testing confirmed CTX with elevated bile alcohol glucuronides present (30.1 μg/ml). CDCA treatment was initiated and diarrhea resolved within one month, with accompanying weight gain. Plasma cholestanol dropped to 0.5 mg/dl within 7 months and after 6 years of treatment is currently stable at <0.2 mg/dl. No further clinical symptoms of CTX have developed.
Figure 1.
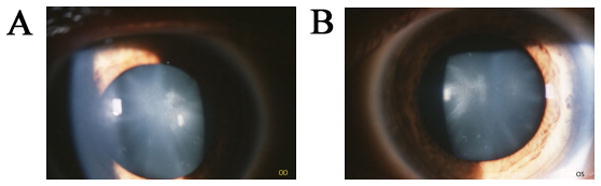
Diffuse nuclear haze and posterior sub capsular capsule opacification in right (A) and left (B) eye.
Figure 2.
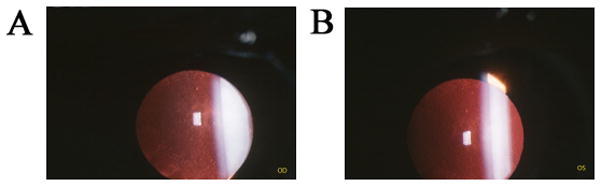
Posterior sub capsular opacification in right (A) and left (B) eye.
Case 2
An 11 year old male was referred to an ophthalmologist for cataract evaluation. High myopia was noted by a previous ophthalmologist at age 4. Family history was significant for high myopia and detached retina in mother and grandmother. Medical history included diarrhea from infancy, delayed language, autism, and seizures. Examination was limited by cooperation; however uncorrected distance visual acuity was at least 20/400 with both eyes open. Dilated examination revealed a refraction of −9.00 +1.00X090 in the right eye, and −9.50+1.25X090 in the left and was remarkable for bilateral cataracts. The lens opacities appeared visually significant with cortical flecks and distorted retinoscopic reflexes. Sequential bilateral cataract surgery was conducted with intraocular lens placement. The corrected visual acuity was 20/30+1 in the right and 20/40 in the left eye. Approximately 5 years later the patient was screened for a cholesterol disorder. Plasma 5α-cholestanol was elevated at 3.1–4.2 mg/dl, consistent with CTX. Elevated bile alcohol glucuronides in urine confirmed CTX. Diarrhea resolved within one month of initiating treatment. Plasma 5α-cholestanol dropped to 0.6 mg/dl within 6–8 months. After 8 months of treatment, the patient remains intellectually impaired, and continues to require an augmentative communication device. Although he still types single words to express wishes and needs, his spoken vocabulary has expanded modestly. His behavioral difficulties (making loud noises/head banging) also appear to be subsiding.
Comment
The prevalence of CTX in the US population is estimated to be as high as 3 to 5 per 100,0005, predicting a minimum number of 8,400 affected individuals. CTX is therefore almost certainly severely under diagnosed with known patients in the US numbering less than 100 (http://ctxinfo.org/ accessed 5.24.2010). The two cases we describe illustrate typical presentations of CTX with bilateral cataracts and highlight the difficulty associated with diagnosing this disorder. Both patients were not diagnosed until several years after symptom onset. One patient was diagnosed shortly after cataracts were identified and, with treatment, has developed no further clinical symptoms of CTX. The other was not diagnosed until 5 years after cataract surgery and suffers significant neurological symptoms associated with disease progression, even after initiation of treatment. Unfortunately treatment after many years of disease progression may not reverse the neurological sequealae4 (though is still recommended).
We urge the ophthalmology community to inquire about diarrhea and developmental delay in all children and young adults with bilateral cataracts and to determine plasma sterol levels in suspect patients or refer the patient to a metabolic disease specialist for evaluation for CTX. Timely diagnosis and treatment of CTX could prevent development of the severe neurological complications associated with this disorder.
Acknowledgments
This work was supported by a Training grant awarded to A.E.D. from the Sterol and Isoprenoid Diseases (STAIR) consortium. STAIR is a part of NIH Rare Diseases Clinical Research Network (RDCRN). Funding and/or programmatic support for this project has been provided by a grant (1U54HD061939) from NICHD and the NIH Office of Rare Diseases Research (ORDR).
References
- 1.Bjorkhem I, Boberg KM, Leitersdorf E. Inborn Errors in Bile Acid Synthesis and Storage of Sterols other than Cholesterol. The Online Metabolic & Molecular Basis of Inherited Disease. 2001;(123):2961–2988. [Google Scholar]
- 2.Gallus G, Dotti M, Federico A. Clinical and Molecular Diagnosis of Cerebrotendinous Xanthomatosis with a review of the mutations in the CYP27A1 gene. Neurol Sci. 2006;(27):143–149. doi: 10.1007/s10072-006-0618-7. [DOI] [PubMed] [Google Scholar]
- 3.Cruysberg J. Cerebrotendinous Xanthomatosis: Juvenile Cataract and Chronic Diarrhea before the onset of Neurologic Disease. Arch Neurol. 2002;(59):527–529. doi: 10.1001/archneur.59.12.1975-a. [DOI] [PubMed] [Google Scholar]
- 4.Berginer VM, Gross B, Morad K, Kfir N, Morkos S, Aaref S, Falik-Zaccai TC. Chronic diarrhea and juvenile cataracts: think cerebrotendinous xanthomatosis and treat. Pediatrics. 2009;(123):143–147. doi: 10.1542/peds.2008-0192. [DOI] [PubMed] [Google Scholar]
- 5.Lorincz M, Rainier S, Thomas D, Fink J. Cerebrotendinous Xanthomatosis: Possible Higher Prevalence Than Previously Recognized. Arch Neurol. 2005;(62):1459–1463. doi: 10.1001/archneur.62.9.1459. [DOI] [PubMed] [Google Scholar]


