Abstract
Purpose
To compare the axis-line-distance technique (ALDT) and Cobb method for therapeutic evaluation of scoliosis.
Methods
Fifty-seven patients with scoliosis were treated in our hospital, 47 underwent conservative bracing therapy and 10 underwent surgery. Based on 171 full-spine X-ray images obtained from these 57 cases before treatment, during conservative treatment or surgery, and at final follow-up after removing the brace or after surgery, two radiologists independently measured and calculated the correction rate during treatment and at final follow-up and the rate of correction loss after treatment with the ALDT and Cobb methods. Paired t-test and correlation analysis were performed.
Results
Based on the ALDT, the lateral deviations of the apical vertebrae before treatment, during treatment, and at final follow-up were 31 ± 14 mm, 16 ± 8 mm, and 20 ± 8 mm, respectively; the correction rates during treatment and at final follow-up were 48.7 ± 21.2% and 37.6 ± 14.2%, respectively, and the rate of correction loss after treatment was 11.3 ± 6.5%. The Cobb angles of scoliosis before treatment, during treatment, and at final follow-up were 34 ± 14°, 19 ± 7°, and 22 ± 6°, respectively; the correction rates during treatment and at final follow-up were 44.4 ± 17.3% and 33.9 ± 14.4%, respectively, and the rate of correction loss after treatment was 11.4 ± 4.3%. Calculation of the correction rate during treatment differed significantly between the two radiologists when using the Cobb method (P < 0.05); their calculations of the correction rate and rate of correction loss were not different (P > 0.05). The measurement data of the two radiologists using the Cobb method showed a weak to moderate correlation (r = 0.49, 0.57, and 0.51, respectively). When using the ALDT, there were no significant differences between the radiologists in their measurements of the correction rate during and after treatment (P > 0.05) or in the rate of correction loss. The measurement data of the two radiologists using the ALDT showed a good to excellent correlation (r = 0.92, 0.93, and 0.90, respectively).
Conclusion
The ALDT is better than the Cobb method for therapeutic evaluation of scoliosis during treatment and at follow-up visits.
Keywords: Scoliosis, Radiography, Curative effect assessment, Measurement
Introduction
Scoliosis is a common disease of teenagers and children. The Cobb method is an important measurement for diagnosing scoliosis and for determining whether and what kind of treatment is necessary. Moreover, the change of the Cobb angle is a key criterion used to assess the clinical curative effects of treatment for scoliosis [1, 2, 7, 8, 22]. Several researchers, however, have reported that the Cobb method is prone to errors because there is a high degree of variance in repeated measurements of the spinal curvature obtained. Incorrect measurements inevitably lead to a less reliable scoliosis diagnosis and curative effect assessment [13, 14, 16]. We have therefore developed a new measurement method for scoliosis, named the axis-line-distance technique (ALDT) [9]. This method has precise measuring points, a simple measurement procedure, low measurement error, and good repeatability [9]. In the present study, we further investigate the clinical value of the ALDT for the therapeutic evaluation of scoliosis.
Materials and methods
Study subjects
A total of 57 (21 males and 36 females) idiopathic scoliosis patients ranging in age from 11 to 26 (mean age 15.8 ± 3.5) years who had undergone treatment in our hospital from June 2004 to December 2009 were recruited in the study, and two cases with significant pelvic rotation which affected the determining of the position of the pubic symphysis and the assessing of scoliosis with ALDT were excluded [9]. All of the 57 patients had complete follow-up visit data and their X-ray images qualified according to measurement requirements. Among the 57 patients, 47 were treated with conservative bracing therapy and 10 were treated surgically. A total of 171 full-spine X-ray images of all cases, which were taken before treatment, during conservative treatment or immediately after surgery (referred to hereafter as “during treatment”), and at final follow-up after removing the brace or after surgery, were used for the measurements. The pre-treatment X-ray image refers to the last X-ray image obtained before treatment; the in-conservative-treatment X-ray image refers to the X-ray image obtained within 2 weeks of the bracing treatment, when the brace was worn by the subject; the immediate post-surgical X-ray image refers to the X-ray image obtained within 2 weeks after surgery, and the final follow-up X-ray image refers to the follow-up X-ray image taken at the final follow-up after operation or after removing the brace during the conservative treatment. The patients were followed-up for 4 months to 5.5 years (mean follow-up duration 16.1 ± 2.8 months). The study was approved by our hospital Ethics Committee, and all subjects provided written informed consent prior to their participation in the study.
Imaging equipment and radiography
The imaging devices included a Siemens 500-mA X-ray machine, an AGFA computed radiography (CR) System, full leg and full spine software and image stand, radiology information system (RIS), and a picture archiving and communications system (PACS).
Each time an X-ray image was recorded, the patient was required to stand in front of the image stand in a well-accepted anatomic position (i.e., standing erect while generally relaxing the body, facing forward, the upper limbs at the sides with the palms turned forward (supinated), and the feet pointing forward) [9]. Two or three 14 inch × 17 inch imaging plates (IP) were placed in the image stand to achieve multiple-exposure imaging from the front and the back of the body at the same time with the same focal film distance of 200 cm and exposure conditions of 90–110 kV and 60–80 mA. After recording, the image plates were scanned to generate two to three scan images. The images were then assembled with the full spinal imaging software into a full-spine image.
Measurement design
Adopting the ALDT and Cobb method, two senior radiologists A and B, who have undergone professional measurement training, independently obtained measurements of the curvature deviation and Cobb angle on a PACS work station. The ALDT was performed as follows: A line connecting the midpoint of the superior border of the pubic symphysis and the central point of the seventh cervical vertebra was denoted the axis line and was used as a baseline for measurement [8]. The distance between the axis line and the center of the curved vertebra was used to assess the degree of spinal curvature [9]. In the present study, this distance, measured by two radiologists, was referred to the deviation distance between the apical vertebra (the outermost vertebra from the axis line) of the major curve (the most curved part) and the axis line (Fig. 1). The Cobb method was performed as follows: The upper end vertebra and the lower end vertebra of the curve were determined in the full-spine X-ray image. A line was then drawn parallel to the superior endplate of the upper end vertebra and another line was drawn parallel to the inferior endplate of the lower end vertebra. The angle formed by the intersection of the two lines was the Cobb angle. In the present study, all Cobb measurements were performed without determining the upper and lower vertebra in advance (Fig. 2) [18].
Fig. 1.
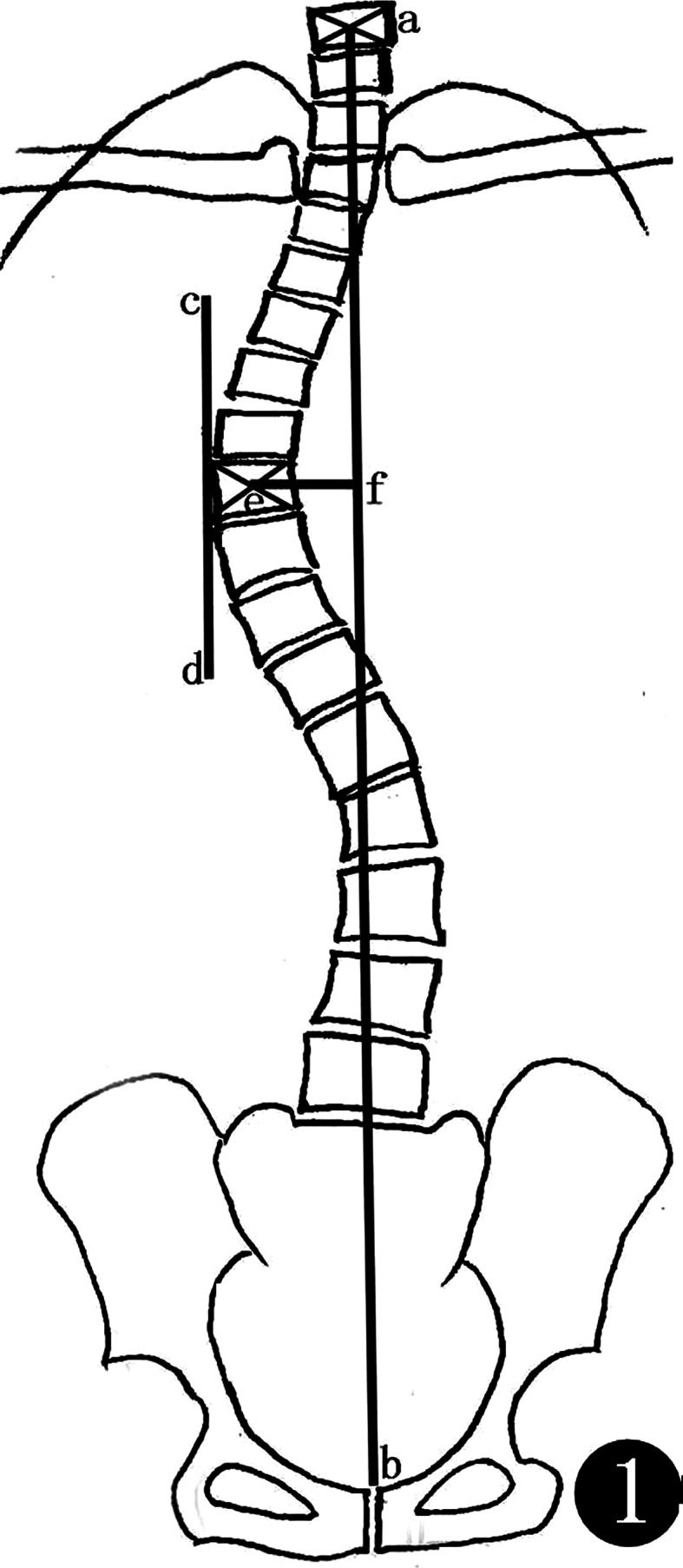
Schematic diagram of the ALDT: a line is drawn to connect the central point (a) of the seventh cervical vertebra and the midpoint (b) of the superior border of the pubic symphysis, and line (ab) is the axis line. To determine the apical vertebra, another line (cd) parallel to the axis line is drawn along the convex side of the vertebra at the peak of a scoliosis curve, and this outermost vertebra is considered the apical vertebra. The crosspoint of diagonal lines of the apical vertebra is considered the central point (e). The vertical distance (ef) between this point and the line (ab) is the deviation distance of the scoliosis
Fig. 2.
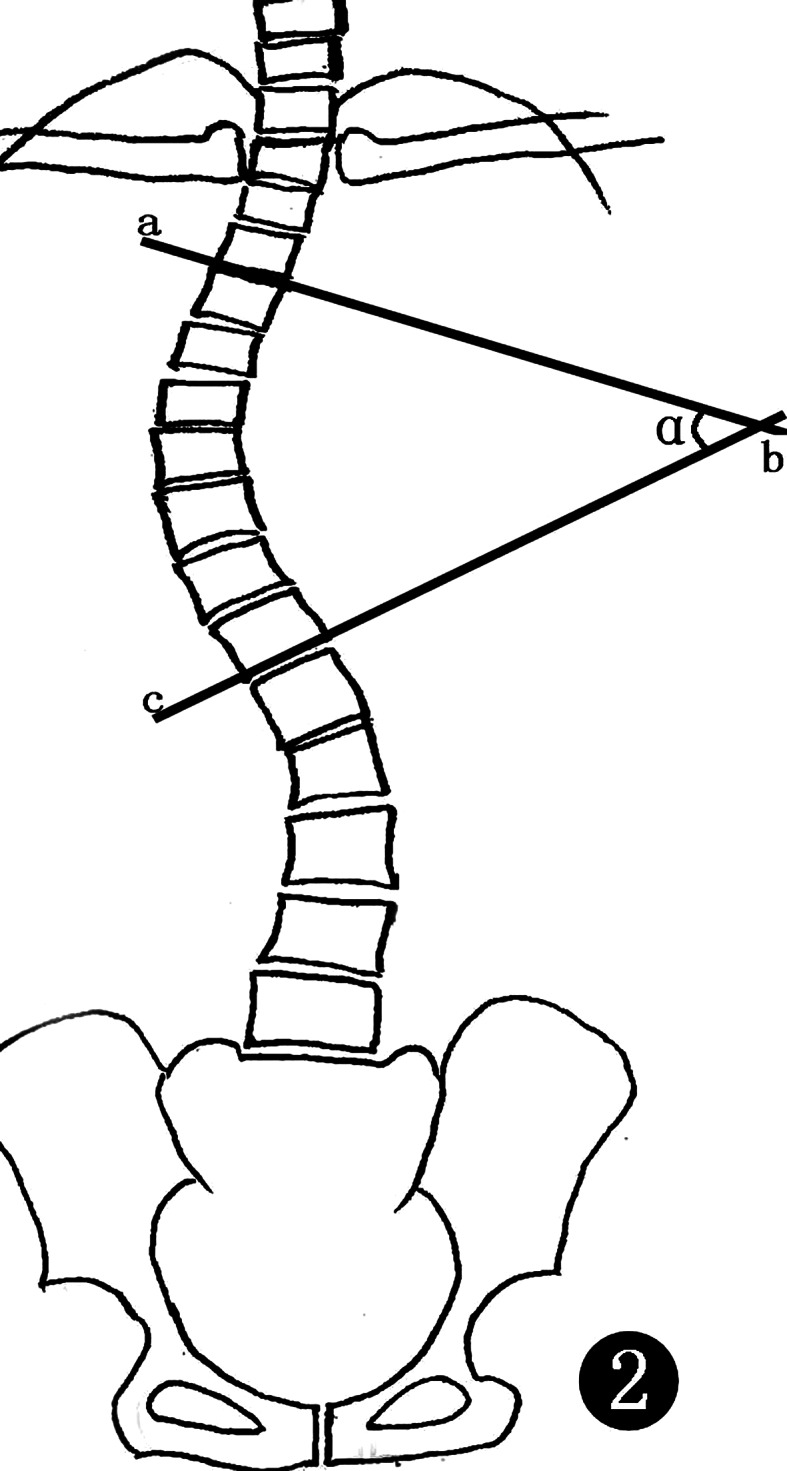
Schematic diagram of the Cobb method: A line (ab) is drawn parallel to the superior endplate of the upper end vertebra and another line (cb) is drawn parallel to the inferior endplate of the lower end vertebra. The angle formed by the intersection of the two lines (ab) and (cd) is the Cobb angle
Statistical analysis
The data measured by the two radiologists were input to a Microsoft Office Excel 2003 spreadsheet to calculate the correction rate during treatment and at final follow-up and the rate of correction loss after treatment. The calculations were performed as follows (Figs. 3, 4) [23]:
Correction angle (or deviation distance) = scoliosis angle (or deviation distance) before treatment − scoliosis angle (or deviation distance) during treatment or at final follow-up,
Correction rate = correction angle (or deviation distance)/scoliosis angle (or deviation distance) before treatment × 100%, and
Rate of correction loss after operation = [scoliosis angle (or deviation distance) at final follow-up − scoliosis angle (or deviation distance) during treatment]/scoliosis angle (or deviation distance) before treatment × 100%.
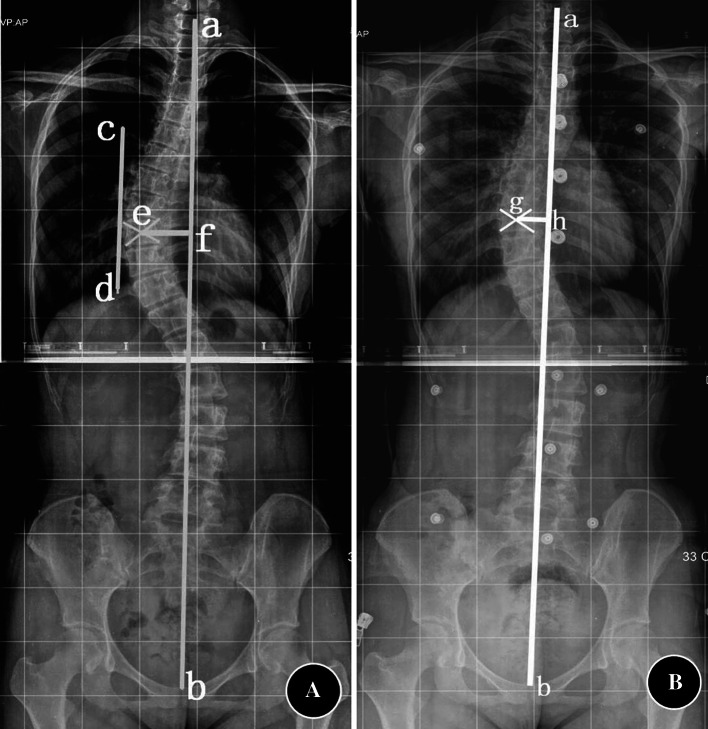
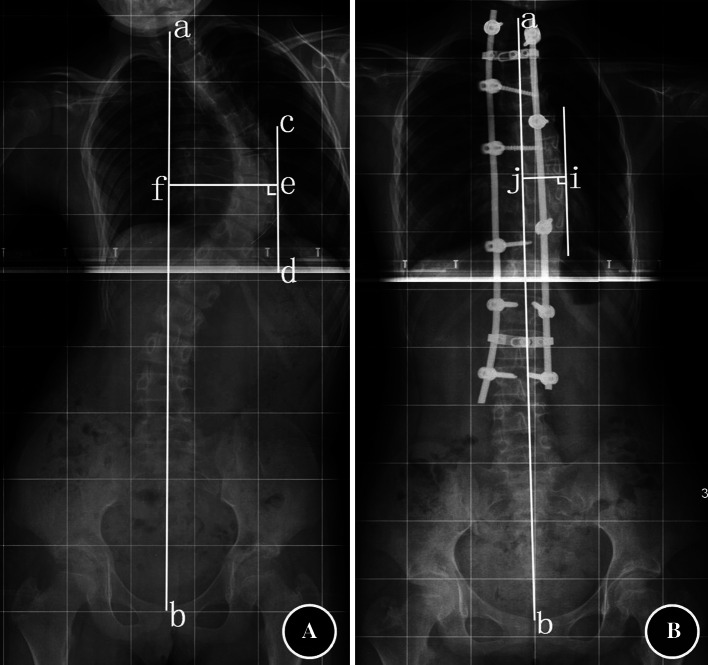
Fig. 3.
Correction rate of conservative treatment obtained using the ALDT. a The deviation distance of the apical vertebrae before treatment is shown as line ef, b the deviation distance of the apical vertebra measured using the same method when wearing the brace is shown as line gh. Therefore, the treatment-induced correction rate is [(ef − gh)/ef] × 100%
Fig. 4.
Correction distance of surgical treatment obtained using the ALDT. a The deviation distance of the apical vertebra along the convex side from the axis line before treatment is shown as line ef, b the deviation distance of the apical vertebrae along the convex side from the axis line measured after surgery and when wearing the brace is shown as line ij. The treatment-induced deviation distance is (ef) – (ij)
A two-tailed mean comparison t-test was performed using SPSS 12.0 software to compare the variance in the correction rate during and after treatment and the rate of correction loss obtained using ALDT and Cobb method between the two radiologists. A P value of 0.05 was considered statistically significant. The calculated data were shown as mean ± standard deviation. The Pearson correlation method was applied to analyze the data with r = 0 − 0.25 indicating no significant correlation, r = 0.25 − 0.49 indicating a weak correlation, r = 0.50 − 0.69 indicating a moderate correlation, r = 0.70 − 0.89 indicating a good correlation, and r = 0.90 − 1.00 indicating an excellent correlation [12].
Results
ALDT measurement
By taking the mean measurements obtained by the two radiologists as the final measuring result, the results were as follows: (a) The lateral deviations of the apical vertebra before treatment, during treatment, and at final follow-up were 31 ± 14 mm, 16 ± 8 mm, and 20 ± 8 mm, respectively; (b) The corrected deviation distance during treatment was 15 ± 6 mm; (c) the lost deviation distance during follow-up visits was 3 ± 1 mm; and (d) the correction rate during treatment and at final follow-up were 48.7 ± 21.2% and 37.6 ± 14.2%, respectively, and the rate of correction loss after treatment was 11.3 ± 6.5%).
Cobb method measurement
By taking the mean measurements obtained by the two radiologists as the final measuring result, the results were as follows: The Cobb angles before treatment, during treatment, and at final follow-up were 34 ± 14°, 19 ± 7°, and 22 ± 6°, respectively. The corrected Cobb angle during treatment was 16 ± 6°, the lost Cobb angle during follow-up visits was 3 ± 1°, the correction rates during treatment and at final follow-up were 44.4 ± 17.3% and 33.9 ± 14.4%, respectively, and the rate of correction loss after treatment was 11.4 ± 4.3%.
Comparison between radiologists A and B
When using the Cobb method, there were no statistical differences (P > 0.05) in the correction rate after treatment and the rate of correction loss, but there was a statistical difference (P < 0.05) in the correction rate during treatment obtained between the two radiologists. On the whole, the measurement data between the two radiologists had a weak to moderate correlation (Table 1). When using the ALDT, there were no statistical differences (P > 0.05) in the correction rate during and after treatment or in the rate of the correction loss obtained between the two radiologists. On the whole, the measurement data between the two radiologists had a good to excellent correlation (Table 1).
Table 1.
Correction rate and correlation obtained by two radiologists with two methods (x ± s, n = 57)
| ALDT (%) | Cobb method (%) | |||||
|---|---|---|---|---|---|---|
| Correction rate during treatment | Correction rate at the last follow-up visit | Rate of correction loss | Correction rate during treatment | Correction rate at the last follow-up visit | Rate of correction loss | |
| Radiologist A | 48.9 ± 15.8 | 37.3 ± 16.2 | 11.8 ± 7.4 | 45.7 ± 16.1 | 34.3 ± 15.2 | 12.0 ± 3.2 |
| Radiologist B | 48.3 ± 24.3 | 37.9 ± 12.2 | 11.2 ± 5.2 | 41.9 ± 18.2 | 29.6 ± 12.4 | 11.3 ± 4.6 |
| Mean | 48.7 ± 21.2 | 37.6 ± 14.2 | 11.3 ± 6.5 | 44.4 ± 17.3 | 33.9 ± 14.4 | 11.4 ± 4.3 |
| t value | 0.17 | 0.13 | −0.02 | 2.25 | 1.52 | 0.62 |
| P value | 0.78 | 0.90 | 0.98 | 0.04 | 0.16 | 0.52 |
| Correlation coefficient r | 0.92 | 0.93 | 0.90 | 0.49 | 0.57 | 0.51 |
Comparison between the ALDT and the Cobb method
Comparison of the two methods indicated that there was no statistical significance (P > 0.05) and a moderate correlation in the correction rate during treatment and at the last follow-up visit and in the rate of correction loss after treatment (Table 2).
Table 2.
Comparison of correction rate and rate of correction loss obtained between two methods (x ± s, n = 57)
| Correction rate during treatment (%) | Correction rate at the last follow-up visit (%) | Rate of correction loss (%) | |
|---|---|---|---|
| ALDT | 48.7 ± 21.2 | 37.6 ± 14.2 | 11.3 ± 6.5 |
| Cobb method | 44.4 ± 17.3 | 33.9 ± 14.4 | 11.4 ± 4.3 |
| t value | 1.34 | 0.71 | 0.22 |
| P value | 0.20 | 0.42 | 0.74 |
| Correlation coefficient r | 0.66 | 0.54 | 0.52 |
Discussion
Scoliosis is a common disease of teenagers and children with morbidity varying from 1.06 to 13.6% [1, 9]; over 80% of teenagers and children with scoliosis suffer from idiopathic scoliosis, which often progresses and worsens with age. The Cobb method is currently the most commonly used for assessing the scoliosis curvature. According to the Scoliosis Research Society (SRS), if a Cobb angle of less than 25°, these patients should undergo conservative treatment. Patients with mature skeletons and a Cobb angle between 25 and 45° should be followed-up every 5 years, and those patients with immature skeletons and a Cobb angle between 25 and 45° should receive bracing treatment and be followed-up every 4 to 6 months. Those patients with a Cobb angle greater than 40–50° should consider undergoing spinal orthomorphia [18]. For both surgical treatment and conservative treatment, the change in the degree of the scoliosis angle is considered a key indicator of the success of treatment. In most related articles [11, 18], a change of 5° was regarded as the judging criterion. Therefore, accurate determination of the degree of lateral curvature of the spine is crucial during follow-up of scoliosis treatment.
Scoliosis is a three-dimensional deformity, including lateral curvature on the coronal plane, forward curvature or backward curvature on the sagittal plane, and rotation of the spine on the axial plane [6, 7, 19]. Among the various methods of measuring the degree of the lateral spinal curvature on the coronal plane, the Cobb method, which was recommended by the SRS, is a clinically widely applied and accepted measurement method [1, 2, 10, 18, 22]. Many researchers, however, have reported significant intra- and inter-observer differences in repeated measurements when using the Cobb method [13, 14, 16]. According to a report by Morrissy et al. [16], the mean inter-observer statistical difference in measurements was 7.2° using the Cobb method if the upper and lower end vertebra were not determined in advance; the mean inter-observer statistical difference in measurements was 6.3°, however, if the upper and lower end vertebra were determined in advance. Loder et al. [14] reported that, if the upper and lower end vertebra were determined when measuring the spinal curvature in patients with congenital scoliosis with the Cobb method, the inter-observer statistical difference in measurements was 9.6° and the intra-observer statistical difference in repeated measurements was 11.8°. If a change of 5° is used as the criterion to assess the curative effect of scoliosis treatment during follow-up visits, the accuracy of therapeutic evaluation will inevitably be affected. In the present study, we found a statistical difference in the correction rate during treatment obtained by the two radiologists after they measured the same X-ray image using the Cobb method. According to previous studies [3, 9, 20], the causes of Cobb measurement errors include body position during radiography, image quality, deviation in determination of the end vertebra, subjectivity in line-drawing, etc. Especially in follow-up patients, variances in determining the upper and lower end vertebra in repeated measurements are bound to affect the accuracy of the therapeutic evaluation. For these reasons, we propose the ALDT to reduce the variance in scoliosis measurements. With precise measuring points, a long interval between repeated measurements or different observers with different levels will not cause significant differences in the results, thus ensuring accurate measurements [9]. According to the present study, the use of ALDT to assess the curative effect on scoliosis did not produce significantly different results, and there was an excellent correlation in the correction rate obtained between the two radiologists.
The curative effect on scoliosis was predominately evaluated by the change in the degree of the Cobb angle in different clinical situations [4, 17]. In the present study, when using the Cobb method, the correction angle during treatment was 16 ± 6°, the correction rate was 44.4 ± 17.3%, and the correction during follow-up visits was 3 ± 1°. When using ALDT, the corrected deviation distance during treatment was 15 ± 6 mm, the correction rate was 48.7 ± 21.2%, and the deviation distance loss during follow-up visits was 3 ± 1 mm. As the units of measurements obtained using the two methods are different, we adopted a new parameter, the rate of correction loss, to facilitate comparison between the two methods. The rate of correction loss obtained using the Cobb method was 11.4 ± 4.3% and that using the ALDT was 11.3 ± 6.5%. In this study, a moderate correlation was observed between the ALDT and Cobb method, and there was no statistical difference in the correction rate during or after treatment, or in the rate of correction loss between the two methods. These findings confirm that ALDT is useful for assessing the curative effect of scoliosis treatment. The measurements of the two radiologists indicated an excellent correction and there was no statistical difference in the correction rate or the correction loss with ALDT, although there was a statistical difference in the correction rate during treatment between the two observers when using the Cobb method and the correlation was only moderate. Therefore, the ALDT is better than the Cobb method to assess the curative effect of scoliosis treatment.
It is worth mentioning that most researches on scoliosis use sacral vertebra (S1) as a reference point [15, 21]; however, we used the pubic symphysis in the ALDT method instead of the center point of S1 as a reference [9]. The main reasons are as follows. Firstly, on the single exposure full-length spinal films adopted in this study, the center point of X-ray is located at the thoracolumbar junction, which will lead to unclear image sharpness of L5 and S1. Much more, the X-ray tiltedly penetrates the sacrococcygeal vertebra, which will also lead to a little overlapping of the L5 and S1 and unclear display of the upper endplate of the S1. Secondly, in some clinical situation, such as sacral vertebra with severe congenital abnormality or obscured by the intestinal contents, it is difficult to identify the center point of S1, but the display of pubic symphysis may not affected. Although this study showed that the ALDT had practical value on the therapeutic evaluation of scoliosis, the evaluation accuracy will be affected by the pelvic rotation or curve types of scoliosis if we use the pubic symphysis as a reference. Especially for patients with severe pelvic rotation, it is difficult to determine of the position of the pubic symphysis; so the ALDT method is not suitable for these patients. It is one of inherit limits of this method [9]. The same influence will exist when S1 is used as a reference, but there’s no concern about the S1 rotation’s influence on the accuracy of evaluation in previous literatures to date [5]. In the next step, further study is needed to assess how the pelvic rotation affects the evaluation.
Acknowledgments
This study is funded by Wenzhou Science and Technology Bureau in China with number of Y20070019.
Conflict of interest
None.
References
- 1.Brooks HL, Azen SP, Gerberg E, et al. Scoliosis: a prospective epidemiological study. J Bone Joint Surg Am. 1975;57:968–972. [PubMed] [Google Scholar]
- 2.Castro FP., Jr Adolescent idiopathic scoliosis, bracing, and the Hueter-Volkmann principle. Spine J. 2003;3:180–185. doi: 10.1016/S1529-9430(02)00557-0. [DOI] [PubMed] [Google Scholar]
- 3.Coillard C, LerouxMA ZabjekKF, et al. SpineCor: a non-rigid brace for the treatment of idiopathic scoliosis: post-treatment results. Eur Spine J. 2003;12:141–148. doi: 10.1007/s00586-002-0467-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dickson RA, Weinstein SL. Bracing (and screening) yes or no? J Bone Joint Surg Br. 1999;81:193–198. doi: 10.1302/0301-620X.81B2.9630. [DOI] [PubMed] [Google Scholar]
- 5.Duong L, Cheriet F, Labelle H, et al. Interobserver and intraobserver variability in the identification of the Lenke classification lumbar modifier in adolescent idiopathic scoliosis. J Spinal Disord Tech. 2009;22:448–455. doi: 10.1097/BSD.0b013e3181831ef7. [DOI] [PubMed] [Google Scholar]
- 6.Gabos PG, Bojescul JA, Bowen JR, et al. Long-term follow-up of female patients with idiopathic scoliosis treated with the Wilmington orthosis. J Bone Joint Surg Am. 2004;86-A:1891–1899. doi: 10.2106/00004623-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005;30:682–688. doi: 10.1097/01.brs.0000155425.04536.f7. [DOI] [PubMed] [Google Scholar]
- 8.Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine. 2005;30:2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 9.He JW, Yan ZH, Liu J, et al. Accuracy and repeatability of a new method for measuring scoliosis curvature. Spine. 2009;34:323–329. doi: 10.1097/BRS.0b013e31819b2504. [DOI] [PubMed] [Google Scholar]
- 10.Hresko MT, Mesiha M, Richards K, et al. A comparison of methods for measuring spinal motion in female patients with adolescent idiopathic scoliosis. J Pediatr Orthop. 2006;26:758–763. doi: 10.1097/01.bpo.0000242432.73563.63. [DOI] [PubMed] [Google Scholar]
- 11.Katz DE, Durrani AA. Factors that influence outcome in bracing large curves in patients with adolescent idiopathic scoliosis. Spine. 2001;26:2354–2361. doi: 10.1097/00007632-200111010-00012. [DOI] [PubMed] [Google Scholar]
- 12.Kuklo TR, Potte BK, Polly DW, et al. Reliability analysis for manual adolescent idiopathic scoliosis measurements. Spine. 2005;30:444–453. doi: 10.1097/01.brs.0000153702.99342.9c. [DOI] [PubMed] [Google Scholar]
- 13.Loder RT, Spiegel D, Gutknecht S, et al. The assessment of intraobserver and interobserver error in the measurement of noncongenital scoliosis in children < or = 10 years of age. Spine. 2004;29:2548–2553. doi: 10.1097/01.brs.0000144828.72721.d8. [DOI] [PubMed] [Google Scholar]
- 14.Loder RT, Urquhart A, Grazlano G, et al. Variability in Cobb angle measurements in children with congenital scoliosis. J Bone Joint Surg Br. 1995;77:768–770. [PubMed] [Google Scholar]
- 15.Min K, Hahn F, Ziebarth K. Short anterior correction of the thoracolumbar/lumbar curve in King 1 idiopathic scoliosis: the behaviour of the instrumented and non-instrumented curves and the trunk balance. Eur Spine J. 2007;16:65–72. doi: 10.1007/s00586-006-0075-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morrissy RT, Goldsmith GS, Hall EC, et al. Measurement of the Cobb angle on radiographs of patients who have scoliosis. Evaluation of intrinsic error. J Bone Joint Surg Am. 1990;72:320–327. [PubMed] [Google Scholar]
- 17.Newton PO, Parent S, Marks M, et al. Prospective evaluation of 50 consecutive scoliosis patients surgically treated with thoracoscopic anterior instrumentation. Spine. 2005;30([17 Suppl]):100–109. doi: 10.1097/01.brs.0000175191.78267.70. [DOI] [PubMed] [Google Scholar]
- 18.Parent S, Newton PO, Wenger DR. Adolescent idiopathic scoliosis: etiology, anatomy, natural history, and bracing. Instr Course Lect. 2005;54:529–536. [PubMed] [Google Scholar]
- 19.Pinheiro AP, Tanure MC, Oliveira AS. Validity and reliability of a computer method to estimate vertebral axial rotation from digital radiographs. Eur Spine J. 2010;19:415–420. doi: 10.1007/s00586-009-1186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richards BS, Bernstein RM, D’Amato CR, et al. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine. 2005;30:2068–2075. doi: 10.1097/01.brs.0000178819.90239.d0. [DOI] [PubMed] [Google Scholar]
- 21.Richards BS, Sucato DJ, Konigsberg DE, et al. Comparison of reliability between the Lenke and King classification systems for adolescent idiopathic scoliosis using radiographs that were not premeasured. Spine. 2003;28:1148–1156. doi: 10.1097/01.BRS.0000067265.52473.C3. [DOI] [PubMed] [Google Scholar]
- 22.Trivedi JM, Thomson JD. Results of Charleston bracing in skeletally immature patients with idiopathic scoliosis. J Pediatr Orthop. 2001;21:277–280. doi: 10.1097/00004694-200105000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Wiley JW, Thomson JD, Mitchell TM, et al. Effectiveness of the Boston brace in treatment of large curves in adolescent idiopathic scoliosis. Spine. 2000;25:2326–2332. doi: 10.1097/00007632-200009150-00010. [DOI] [PubMed] [Google Scholar]