Abstract
Introduction
In order to minimize perioperative invasiveness and improve the patients’ functional capacity of daily living, we have performed minimally invasive lumbar decompression and posterolateral fusion (MIS-PLF) with percutaneous pedicle screw fixation for degenerative spondylolisthesis with spinal stenosis. Although several minimally invasive fusion procedures have been reported, no study has yet demonstrated the efficacy of MIS-PLF in degenerative spondylolisthesis of the lumbar spine. This study prospectively compared the mid-term clinical outcome of MIS-PLF with those of conventional PLF (open-PLF) focusing on perioperative invasiveness and patients’ functional capacity of daily living.
Materials and methods
A total of 80 patients received single-level PLF for lumbar degenerative spondylolisthesis with spinal stenosis. There were 43 cases of MIS-PLF and 37 cases of open-PLF. The surgical technique of MIS-PLF included making a main incision (4 cm), and neural decompression followed by percutaneous pedicle screwing and rod insertion. The posterolateral gutter including the medial transverse process was decorticated and iliac bone graft was performed. The parameters analyzed up to a 2-year period included the operation time, intra and postoperative blood loss, Oswestry-Disability Index (ODI), Roland-Morris Questionnaire (RMQ), the Japanese Orthopaedic Association score, and the visual analogue scale of low back pain. The fusion rate and complications were also reviewed.
Results
The average operation time was statistically equivalent between the two groups. The intraoperative blood loss was significantly less in the MIS-PLF group (181 ml) when compared to the open-PLF group (453 ml). The postoperative bleeding on day 1 was also less in the MIS-PLF group (210 ml) when compared to the open-PLF group (406 ml). The ODI and RMQ scores rapidly decreased during the initial postoperative 2 weeks in the MIS-PLF group, and consistently maintained lower values than those in the open-PLF group at 3, 6, 12, and 24 months postoperatively. The fusion rate was statistically equivalent between the two groups (98 vs. 100%), and no major complications occurred.
Conclusion
The MIS-PLF utilizing a percutaneous pedicle screw system is less invasive compared to conventional open-PLF. The reduction in postoperative pain led to an increase in activity of daily living (ADL), demonstrating rapid improvement of several functional parameters. This superiority in the MIS-PLF group was maintained until 2 years postoperatively, suggesting that less invasive PLF offers better mid-term results in terms of reducing low back pain and improving patients’ functional capacity of daily living. The MIS-PLF utilizing percutaneous pedicle screw fixation serves as an alternative technique, eliminating the need for conventional open approach.
Keywords: Minimally invasive spine surgery, Posterolateral fusion, Percutaneous pedicle screw, Degenerative spondylolisthesis, Lumbar spine
Introduction
In recent years, several minimally invasive spine surgeries have gained popularity. The purpose of minimally invasive spine surgery is to minimize the skin incision and perioperative pain, thereby achieving an early recovery and improvement of patients’ QOL. Recently, minimally invasive spine surgery such as endoscopic spine surgery has evolved into minimally or less invasive spinal instrumentation surgery.
Minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) has been reported by several authors [1, 7–9, 14]. Subsequently, Foley et al. [4] introduced a percutaneous pedicle screw insertion and rod assembly system (CD Horizon Sextant, Medtronic, Memphis, TN, USA) for MIS-TLIF. After the introduction of the Sextant system, several authors reported their experience of using it for MIS-TLIF [6, 10–13]. However, the use of the Sextant system for lumbar posterolateral fusion (PLF) has been scarcely reported in the literature. Foley et al. [5] reported a revision case of L5-S1 anterior peudarthrosis treated by MIS-PLF using the Sextant system, achieving a successful fusion.
For the treatment of lumbar degenerative spondylolisthesis, we have several available surgical strategies including posterior decompression alone, PLF, and posterior interbody fusion, based on the spinal slippage and instability, spinal alignment, and sagittal facet joint inclination. Although the debate regarding the surgical strategy is not settled yet, many cases of degenerative spondylolisthesis have been treated by PLF without an interbody fusion requiring a facet resection and intervertebral disc destruction [15–17]. Our concept was to make PLF less invasive with a clinically equivalent outcome, thereby improving patients’ function and quality of life.
Since 2005, we have performed MIS-PLF for lumbar degenerative spondylolisthesis with spinal stenosis using a percutaneous pedicle screw insertion and rod assembly system. The main incision has been minimized to 4 cm to make the surgery less invasive and promote better functional capacity postoperatively. The objective of this study was to prospectively compare the mid-term clinical result of MIS-PLF with those of conventional PLF, focusing on the surgical invasiveness and patients’ functional capacity of daily living.
Materials and methods
Patient demographics
Since May 2005, a total of 80 patients received a single-level posterior decompression and PLF for lumbar degenerative spondylolisthesis with spinal stenosis. The slipped vertebrae were L4 in 76 patients and L3 in 4 patients. There were 27 males and 53 females. The average age at surgery was 65 years (37–84). The patients were required to demonstrate the apparent intermittent neurological claudication and/or radicular neurological symptoms preoperatively, which were explained by neural compression due to spondylolisthesis with spinal stenosis. The patients complaining the low back pain alone preoperatively were not included in this study. The patients were prospectively assigned to receive one of the following surgical techniques: MIS-PLF and open-PLF. This assignment was performed by a patient after the preoperative explanations including a risk and benefit of both procedures. This study design received permission by the ethics committee in the University. Forty-three cases underwent MIS-PLF and 37 patients underwent open-PLF. There were no statistical differences between two surgical groups in terms of gender, age, vertebral level, and the degree of spondylolisthesis (% slip) (Table 1).
Table 1.
Backgroud data comparison of two surgical groups
| MIS | Open | Significance | |
|---|---|---|---|
| Pt number | 43 | 37 | |
| Gender (M:F) | 14:29 | 12:25 | NS |
| Age | 63 ± 9 | 66 ± 9 | NS |
| Preop JOA score | 11.1 ± 3.8 | 12.6 ± 3.4 | NS |
| Preop ODI score | 52.0 ± 13.2 | 48.9 ± 10.8 | NS |
| Preop RDQ score | 12.2 ± 4.5 | 13.7 ± 3.9 | NS |
| Preop LBP VAS | 73.1 ± 17.6 | 73.7 ± 20.2 | NS |
| Preop % Slip | 17.9 ± 4.9 | 18.4 ± 6.6 | NS |
Mean ± SD
NS no significant difference between two groups
Surgical procedures
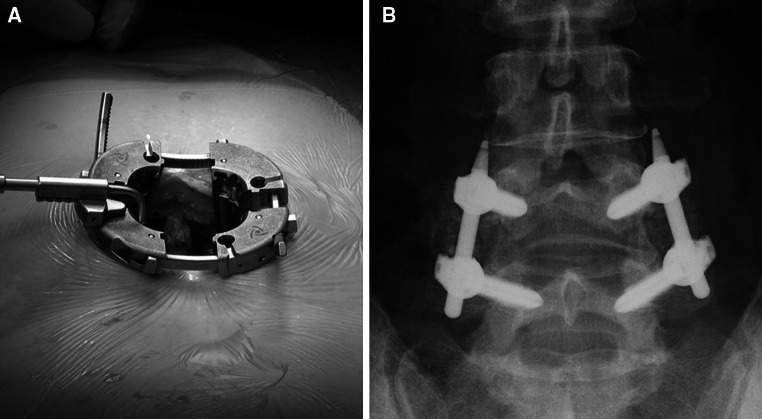
The surgical technique of MIS-PLF included a midline incision (4 cm) and neural decompression by bilateral medial facetectomy. After this, small parasagittal incision of 1.2 cm was made under A-P fluoroscopy and the PAK needle (Medtronic) was placed on the medial edge of the transverse process. Then, it was gradually advanced to the pedicle and posterior half of the vertebral body. After the guide wire was placed, drilling and tapping procedures were performed followed by pedicle screw placement using a screw extender (Medtronic). L4 and L5 pedicle screws were unilaterally placed, and the rod was then inserted and tightened by means of the Sextant system (Medtronic) (Fig. 1). Using the same incision, the cancellous bone was harvested from the posterior aspect of the iliac crest. After creating the bilateral posterolateral gutter, which included the medial half of the transverse process, the lamina, and facet joints were carefully decorticated using a specially designed expandable retractor (Pipeline, Depuy Spine, Inc., Raynham, MA, USA). The morcellated cancellous bone was grafted bilaterally (Fig. 2). The subjects in the open-PLF group underwent a conventional PLF following posterior neural decompression including a midline skin incision (average 12 cm) and bilateral pedicle screw fixation using a polyaxial pedicle screw and rod system. The graft bone was harvested from the posterior aspect of the iliac bone using the same skin incision.
Fig. 1.

Percutaneous rod placement and instrumentation with the Sextant system (Medtronic, Memphis, TN, USA)
Fig. 2.
a The use of an expandable retractor provides an enlarged surgical area and sufficient illumination for MIS-PLF. b After the meticulous decortication of bilateral posterolateral gutters, the morcellated cancellous iliac bone was grafted bilaterally in the MIS-PLF group
Quantitative analyses of clinical outcome
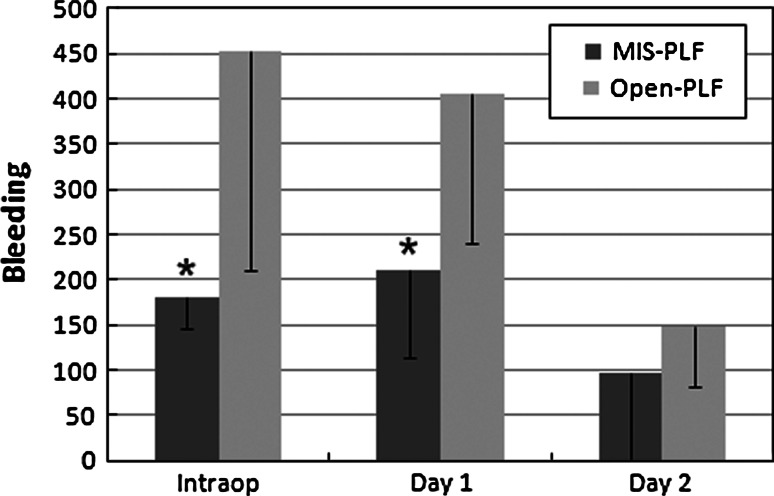
The surgical parameters included the operation time, intraoperative and postoperative blood loss at days 1 and 2, and days required for drainage tube removal. The laboratory data for serum hemoglobin (s-Hb), C-reactive protein (CRP), and creatine phosphokinase (CPK) were also recorded preoperatively, and then on postoperative days 1, 3, 7, and 14 (Fig. 3). The following parameters were analyzed: Japanese Orthopaedic Association (JOA) score, Oswestry-Disability Index (ODI), Roland-Morris Questionnaire (RMQ), and visual analogue scale of low back pain (LBP VAS). Except for the JOA scores, the questionnaires were filled out by each patient without supervision by a medical doctor. The ODI and RMQ were evaluated preoperatively, and postoperatively at weeks 2, 3, and 6, and then at 12 and 24 months. LBP VAS was evaluated preoperatively, and on postoperative days 1, 3, 7, and 14 and then at 6 and 12 months. The preoperative JOA score, ODI, RMQ, and LBP VAS demonstrated no statistical differences between two surgical groups (Table 1). The fusion status was evaluated by X-ray and CT scans at the final follow-up visit. The surgical complication rate was also reviewed.
Fig. 3.
Intraoperative and postoperative blood loss (days 1 and 2) in the MIS-PLF and open-PLF groups. Asterisks indicate the statistically significant difference between the MIS-PLF and open-PLF groups at the P = 0.01 level
Statistical analysis
Each parameter was compared using the unpaired student’s t test between the two surgical groups.
Results
The average postoperative follow-up period was 32 (24–49) and 40 (24–60) months in the MIS-PLF and open-PLF groups, respectively. The average operation time was 172 ± 33 and 176 ± 37 min in the MIS-PLF and open-PLF groups, respectively, which was not statistically different. The intraoperative and postoperative blood losses are indicated in Table 3. The average intraoperative blood loss was 181 and 453 mL in the MIS-PLF and open-PLF groups, respectively, which was statistically different (P < 0.01). The postoperative blood loss in the MIS-PLF group was significantly less than that in the open-PLF group on day 1 (P < 0.01). The average days required for drainage tube removal were 3.4 and 4.8 in the MIS-PLF and open-PLF groups, respectively, which was statistically different (P < 0.01).
Table 3.
Comparison of average operation time and intraoperative blood loss between MIS and open fusion surgeries (data from previous TLIF studies and the present study)
| Author | Operation time (min) | Intraoperative blood loss (ml) | ||
|---|---|---|---|---|
| MIS | Open | MIS | Open | |
| Isaacsa | 300 | 276 | 226 | 1,147 |
| Scheuflera | 104 | 132 | 55 | 125 |
| Park Ya | 192 | 149 | 432 | 737 |
| Dhall | 199 | 237 | 194 | 505 |
| Fan | 204 | 195 | 496 | 887 |
| Penga | 216 | 170 | 150 | 681 |
| Schizas | 348 | 312 | 456 | 961 |
| Present studya | 174 | 175 | 181 | 453 |
aStudy utilizing the percutaneous spinal instrumentation
Laboratory data are represented in Table 2. The preoperative s-Hb was statistically similar between the two surgical groups, however, it was lower in the open-PLF group compared to the MIS-PLF group on postoperative day 1 (P < 0.01). After day 3, the level gradually recovered in both groups. The maximum postoperative serum CRP levels were 6.6 and 7.6 in the MIS-PLF and open-PLF groups, respectively; however, this difference was not significant. CRP levels in the MIS-PLF group tended to decrease more rapidly; however, there was no statistical difference found between the two groups. The CRP levels on day 14 were 0.4 and 0.3 in the MIS-PLF and open-PLF groups, respectively, demonstrating that a reduction occurred in both groups. The CPK levels elevated to maximum values of 807 and 854 in the MIS-PLF and open-PLF groups, respectively, which were not statistically different. The CPK levels on day 3, 7, and 14 were statistically equivalent in both groups.
Table 2.
Comparison of laboratory data between MIS-PLF and open-PLF groups
| s-Hb | CRP | CPK | ||||
|---|---|---|---|---|---|---|
| MIS | Open | MIS | Open | MIS | Open | |
| Preop | 13.5 ± 1.2 | 13.1 ± 1.5 | 0.1 ± 0.2 | 0.1 ± 0.1 | 150.7 ± 116.5 | 110.3 ± 74.1 |
| Post 1D | 10.8 ± 1.2* | 10.2 ± 1.4 | 2.9 ± 1.4 | 2.8 ± 1.2 | 807.4 ± 487.6 | 854.0 ± 628.9 |
| Post 3D | 10.2 ± 1.1 | 9.8 ± 1.4 | 6.6 ± 2.8 | 7.6 ± 3.5 | 457.8 ± 270.3 | 400.6 ± 208.1 |
| Post 1w | 10.3 ± 1.1 | 9.8 ± 1.2 | 1.5 ± 1.4 | 1.8 ± 2.5 | 112.9 ± 63.0 | 98.3 ± 55.7 |
| Post 2w | 10.7 ± 2.1 | 10.6 ± 1.2 | 0.4 ± 0.4 | 0.3 ± 0.4 | 73.7 ± 41.0 | 58.5 ± 28.9 |
Mean ± SD
* Significantly different from open-PLF at P < 0.05
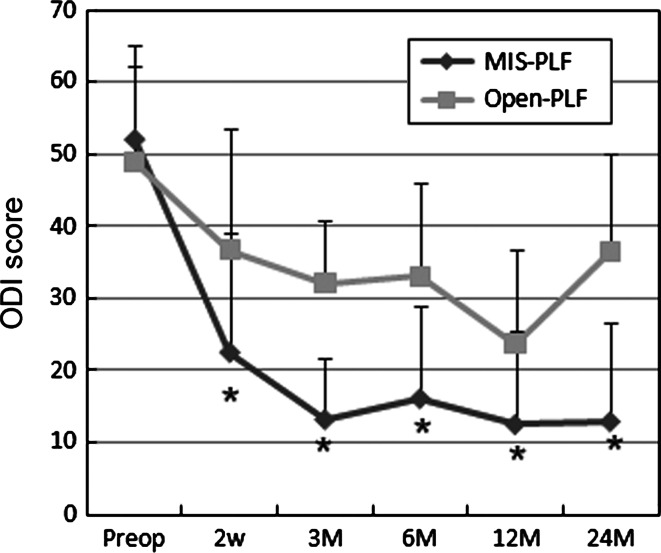
The average preoperative JOA scores were 11.1 and 12.6 in the MIS-PLF and open-PLF groups, respectively, which were statistically similar (Table 1). The average follow-up JOA scores were 23.5 and 22.8 in the MIS-PLF and open-PLF groups, respectively, which were also statistically equivalent. The recovery rates of the JOA score were 63.1 and 59.9% in each group, respectively. The time-related change of ODI value indicated in Fig. 4. The average preoperative ODI values were 52.0 and 48.9 for each group, respectively, which were statistically equivalent. At 2 weeks postoperatively, the ODI value in the MIS-PLF group reduced dramatically. There was a statistical significant difference in ODI values between the two groups at 2 weeks postoperatively (P < 0.01). At 3 months, the MIS-PLF group demonstrated further decrease to an average of 13.2; however, the average score for the open-PLF group remained 32.1, which was a statistically significant. This difference was maintained at 6, 12, and 24 months postoperatively (P < 0.01).
Fig. 4.
Time-related change of ODI from the preoperative phase until 24 months postoperatively in the MIS-PLF and open-PLF groups. Asterisks depict the statistically significant differences between the MIS-PLF and open-PLF groups at each time period (P < 0.01)
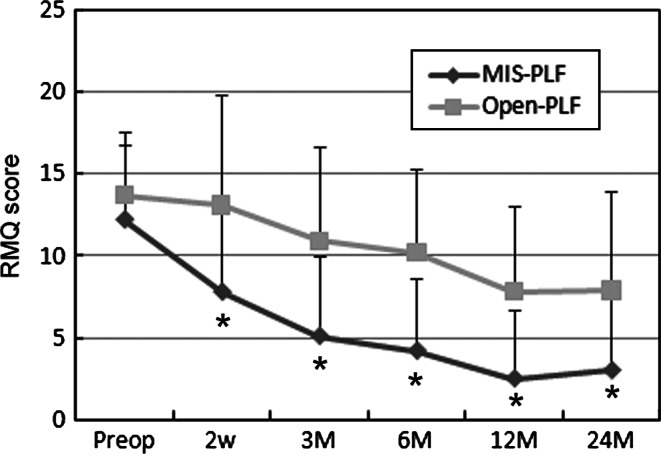
The average preoperative RMQ values were 12.2 and 13.7, respectively, which were statistically equivalent (Fig. 5). At 2 weeks postoperatively, the RMQ value in the MIS-PLF group reduced to 7.8. There was a statistical difference of RMQ value at 2 weeks between two groups (P < 0.01). At 3 months, MIS-PLF group showed further decrease to 5.1; however, the Open-PLF group remained at 10.9. There was also significant difference between two groups. This difference was maintained until 6, 12, and 24 months postoperatively (P < 0.01).
Fig. 5.
Time-related change of RMQ scores from the preoperative stage until 24 months postoperatively in the MIS-PLF and open-PLF groups. Asterisks depict statistically significant differences between the MIS-PLF and open-PLF groups at each time period (P < 0.01)
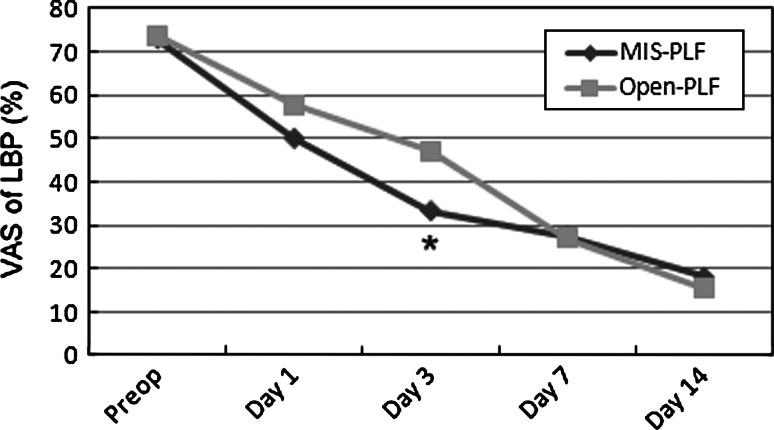
The preoperative LBP VAS of low back pain were 73.0 and 73.7 in the MIS-PLF and open-PLF groups, respectively (Fig. 6). Postoperatively, both groups demonstrated a rapid reduction in their LBP VAS, which was maintained until day 14; however, the decrease was more pronounced in the MIS-PLF group. The LBP VAS on day 3 in the MIS-PLF group was statistically lower than that in the open-PLF group (P < 0.02).
Fig. 6.
Average low back pain VAS at preoperative, and postoperative days 1, 3, 7, and 14 in the MIS-PLF and open-PLF groups. Asterisks depict statistically significant differences between the MIS-PLF and open-PLF groups at the P = 0.02 level
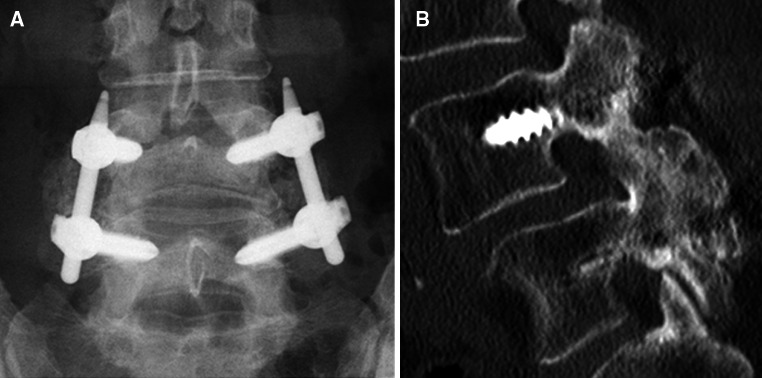
Radiological evaluation demonstrated that solid fusion was achieved in 42 out of 43 cases (98%) in the MIS-PLF group, and in all 37 cases (100%) in the open-PLF group. The one case of pseudarthrosis in the MIS-PLF group had no symptoms, there was no implant failures or displacement, and no revision surgery was required. Although the radiographic assessment of fusion had a limitation in accuracy due to the presence of hardware, the parasagittal CT scans were relatively useful for assessing the bony continuity between consecutive facet joints and transverse processes (Fig. 7).
Fig. 7.
Follow-up radiograph and parasagittal CT image of MIS-PLF at 29 months postoperatively. a A-P radiograph demonstrating a solid and continuous posterolateral fusion. b A parasagittal CT image of the solid continuity of fusion
There were no major complications, such as neural and vascular injury or deep wound infections. However, two cases in the MIS-PLF group demonstrated some surgical difficulty in rod passage during the percutaneous rod placement procedure. In these cases, the rods were placed directly on heads of pedicle screws via extended midline skin incisions involving lateral intramuscular exposure, but without conversion to a major open procedure. Both cases successfully led to solid bony fusion without implant failures.
Discussion
In recent years, there have been several case series and comparative studies on minimally invasive lumbar spine fusions [1, 6–14]. In the present study, percutaneous pedicle screw-rod instrumentation was used for MIS-PLF. Through a 4 cm main incision, neural decompression was performed with medial facetectomies, and the iliac bone was grafted at bilateral decorticated lateral gutters using a specially designed expandable retractor. When compared to the open-PLF group that required average incision of 12 cm, a statistically equivalent fusion rate (97%) was achieved in the MIS-PLF group (vs. 100% in the open-PLF group). Table 3 summarizes the surgical times and intraoperative blood loss of MIS-PLF and Open-PLF in this study with comparative data from previously published TLIF reports [2, 3, 6, 10–13]. In previous TLIF studies, the MIS procedure tended to take more surgical time than open TLIF [3, 6, 10, 11, 13]; however, some authors reported a shorter surgical time [2, 12]. There has been a significant learning curve reported for minimally invasive interbody fusion [2, 3, 6, 10–13], which could be influencing the surgical time variation. In the present study, a statistically equivalent surgical time was demonstrated between the MIS-PLF and open-PLF groups. However, there is an obvious learning curve in the percutaneous pedicle screw-rod instrumentation and bone grafting in small surgical area. After overcoming the initial learning curve, the surgical time in our study became sufficiently short.
In terms of the intraoperative blood loss, previous studies reported less blood loss for MIS surgery compared to open surgery [2, 3, 6, 10–13] (Table 3). In the present study, there was significantly less blood loss in the MIS-PLF group, both intraoperatively, and on day 1 postoperatiovely, when compared to the open-PLF group (P < 0.05). Even with the posterolateral exposure for PLF preparation, the MIS-PLF group successfully reduced the intraoperative blood loss.
In the present study, the LBP VAS demonstrated a more rapid reduction in the MIS-PLF group over the initial seven days postoperatively than it did in the open-PLF group. The significant difference was observed at day 3 (P < 0.05). Although the VAS evaluation intrinsically contains the uncertainty from a wide variation of data, the MIS fusions including our study generally reduce the LBP VAS through postoperative day 1–7, when compared to open procedures. Specifically, MIS-PLF in the present study had a tendency of reducing the postoperative pain over the early postoperative period between days 1 and 3.
There are few studies that have evaluated LBP-specific functional parameters such as the ODI to assess the impact of minimally invasive procedures [3, 11, 13]. Fan et al. [3] reported the ODI changes between MIS and Open groups until 12 months postoperatively. Although the MIS group exhibited a lower ODI score compared to the open group, there was no statistical difference between the two groups. Peng and Schizas [11, 13] also demonstrated a reduction in ODI scores at 24 months postoperatively in both MIS and Open groups; however, there was no statistical difference between the MIS and Open groups. The present study clearly demonstrated that there is a significant reduction in ODI values in patients who have undergone MIS-PLF when compared to those undergoing open-PLF surgery between 2 weeks until 24 months postoperatively, when the study observation period ended. This superiority of LBP-specific functional parameters may be explained by the minimum incision of skin and lumbosacral fascia as well as a reduction of paravertebral muscle damage using a retractor [3, 8]. However, in the future comparison with large number of patients, this significance should be re-evaluated and the factors influencing LBP-specific functional parameters should be analyzed precisely.
There have been several surgical complications reported for the MIS fusion procedure. Schwender et al. [14] reported a surgical complication rate of 6.1%, including pedicle screw malposition, cage displacement, and iatrogenic foraminal stenosis in 49 cases of MIS-fusion using the Sextant system. Dhall et al. [2] reported a surgical complication rate of 14.2%, which included pedicle screw malposition, cage displacement, and a dural tear in mini-open fusion procedure. Many authors are experienced in using the different MIS techniques, and many have concluded that there is a significant learning curve involved in minimally invasive fusion procedures. The present study demonstrated a lower complication rate of 3.8% (including the difficulty in rod passage in two patients and one case of pseudoarthrosis) in the MIS-PLF group. There are some technical pitfalls in percutaneous spinal instrumentation systems such as the Sextant system. The surgeons have to pay attention to the screw extender alignment, especially where there is a greater amount of displaced cephalad vertebra. When the extenders are not perfectly aligned, an additional small incision for extender or re-alignment should be made.
The major limitation of this study was a non-randomized setting in the study design. Importantly, the quantitative assessments of VAS and LBP-specific functional questionnaires based on patients’ subjective evaluation could be influenced by patients’ assignment into groups. The patients assigned into MIS-PLF group may expect less pain and better function, influencing the positive quantitative data.
In summary, the mid-term clinical outcomes of MIS-PLF were prospectively compared to those of open-PLF, focusing on surgical invasiveness and the resultant patients’ functional capacity. The MIS-PLF procedure was demonstrated to be far less invasive when compared to conventional open-PLF. The superior outcomes for postoperative low back pain and functional parameters in the MIS-PLF group was maintained until 2 years, suggesting that it has a better mid-term effect on back muscle preservation.
Conflict of interest
None.
References
- 1.Deutsch H, Musacchio MJ., Jr Minimally invasive transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Neurosurg Focus. 2006;20:E10. doi: 10.3171/foc.2006.20.3.11. [DOI] [PubMed] [Google Scholar]
- 2.Dhall SS, Wang MY, Mummaneni PV. Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up. J Neurosurg Spine. 2008;9:560–565. doi: 10.3171/SPI.2008.9.08142. [DOI] [PubMed] [Google Scholar]
- 3.Fan S, Hu Z, Zhao X, et al. Multifidus muscle changes and clinical effects of one-level posterior lumbar interbody fusion: minimally invasive procedure versus conventional open approach. Eur Spine J. 2009;19:316–324. doi: 10.1007/s00586-009-1191-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Foley KT, Gupta SK, Justis JR, et al. Percutaneous pedicle screw fixation of the lumbar spine. Neurosurg Focus. 2001;10:1–8. doi: 10.3171/foc.2001.10.4.11. [DOI] [PubMed] [Google Scholar]
- 5.Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine. 2003;28:S26–S35. doi: 10.1097/01.BRS.0000076895.52418.5E. [DOI] [PubMed] [Google Scholar]
- 6.Isaacs RE, Podichetty VK, Santiago P, et al. Minimally invasive microendoscopy-assisted transforaminal lumbar interbody fusion with instrumentation. J Neurosurg Spine. 2005;3:98–105. doi: 10.3171/spi.2005.3.2.0098. [DOI] [PubMed] [Google Scholar]
- 7.Jang JS, Lee SH. Minimally invasive transforaminal lumbar interbody fusion with ipsilateral pedicle screw and contralateral facet screw fixation. J Neurosurg Spine. 2005;3:218–223. doi: 10.3171/spi.2005.3.3.0218. [DOI] [PubMed] [Google Scholar]
- 8.Kim DY, Lee SH, Chung SK, et al. Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine. 2005;30:123–129. doi: 10.1097/01.brs.0000157172.00635.3a. [DOI] [PubMed] [Google Scholar]
- 9.Park P, Foley KT. Minimally invasive transforaminal lumbar interbody fusion with reduction of spondylolisthesis: technique and outcome after a minimum of 2 years’ follow-up. Neurosurg Focus. 2008;25:E16. doi: 10.3171/FOC/2008/25/8/E16. [DOI] [PubMed] [Google Scholar]
- 10.Park Y, Ha JW. Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine. 2007;32:537–543. doi: 10.1097/01.brs.0000256473.49791.f4. [DOI] [PubMed] [Google Scholar]
- 11.Peng CW, Yue WM, Poh SY, et al. Multifidus muscle changes and clinical effects of one-level posterior lumbar interbody fusion: minimally invasive procedure versus open transforaminal lumbar interbody fusion. Spine. 2009;34:1385–1389. doi: 10.1097/BRS.0b013e3181a4e3be. [DOI] [PubMed] [Google Scholar]
- 12.Scheufler KM, Dohmen H, Vougioukas VI. Percutaneous transforamial lumbar interbody fusion for the treatment of degenerative lumbar instability. Neurosurgery. 2007;60:203–212. doi: 10.1227/01.NEU.0000255388.03088.B7. [DOI] [PubMed] [Google Scholar]
- 13.Schizas C, Tzinieris N, Tsiridis E, et al. Minimally invasive versus open transforaminal lumbar interbody fusion: evaluating initial experience. Int Orthop. 2009;33:1683–1688. doi: 10.1007/s00264-008-0687-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwender JD, Holly LT, Rouben DP, et al. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech. 2005;18:S1–S6. doi: 10.1097/01.bsd.0000132291.50455.d0. [DOI] [PubMed] [Google Scholar]
- 15.Stauffer RN, Coventry MB. Posterolateral lumbar spine fusion. J Bone Joint Surg. 1972;54A:1195–1204. [PubMed] [Google Scholar]
- 16.Watkins MB. Posterolateral fusion of the lumbar and lumbosacral spine. J Bone Joint Surg. 1953;35A:1014–1018. [PubMed] [Google Scholar]
- 17.Wiltse LL, Bteman JG. Experience with transverse-process fusion of the lumbar spine. J Bone Joint Surg. 1965;47A:848–849. [Google Scholar]