Abstract
Summary of background data
The curve pattern of idiopathic scoliosis is important for making decisions concerning bracing. However, whether the curve pattern changes during brace treatment have not been fully documented. The aim of this study was to investigate the changes of curve pattern during brace treatment in skeletally immature patients with adolescent idiopathic scoliosis (AIS).
Methods
From January 2002 to January 2011, AIS patients treated with a Boston or Milwaukee brace were recruited after meeting the following inclusion criteria: older than 10 years of age at initiation of bracing; having a Cobb angle of 25°–40°; with a Risser sign 0–2; being regularly followed until the weaning of brace or the necessity of surgical treatment; and without history of previous treatment. A total of 130 female and 11 male AIS patients were included. The mean age was 12.9 years at initiation of bracing, and the female patients were, on average, 2.7 months past menarche. The mean follow-up period was 2.6 years (range 1.0–5.5 years). The definitions of changes in curve patterns were divided into four categories as follows: (1) shift of the apex of the main curve; (2) change in the curve span of more than two vertebrae; (3) change in the main curve type with regard to the apex location; and (4) change of curve direction. The patients were divided into two groups. Group A was comprised of patients who had experienced one or more categories of curve pattern changes, and Group B was comprised of those who had not.
Results
Of these 39 patients, 14 had apex shifting, 2 underwent curve span changes, 22 experienced changes in the main curve type, and one female had both changes in the apex and curve span. At the initiation of bracing, patients in Group A demonstrated significantly lower menarchal status (P = 0.018) and lower Risser grade (P = 0.025) than those in Group B. The difference in the percentage of patients who underwent Boston bracing between the two groups was statistically significant (41.5 % for Group A vs. 24.0 % for Group B, P = 0.023).
Conclusion
Changes in curve pattern can occur during brace treatment. Patients with less skeletal maturity and those treated with a Boston brace are more susceptible to this phenomenon.
Keywords: Adolescent idiopathic scoliosis, Brace treatment, Curve pattern
Introduction
Adolescent idiopathic scoliosis (AIS) is one of the most common spinal deformities, and is predominantly seen in females. Previous studies have indicated that bracing can potentially alter the natural history of AIS [1, 2], prevent curve progression, and decrease the need for surgical intervention [3–7], although some authors have questioned the efficacy of orthotic treatment [8–11].
When choosing an appropriate orthosis, the curve pattern must be taken into account. The optimal brace, which is usually crafted from customized moulds made of the patient’s trunk, is specifically fit to the specific curve pattern of the patient. The trim lines, pad placement, and areas of relief are all based on the pre-brace clinical evaluation and coronal radiography of the trunk. Therefore, when the coronal curve type or the apical vertebra changes, the orthosis should be adjusted to suit the specific curve pattern. Studies investigating whether the curve pattern changes during brace treatment are limited.
As reported by van Rhijn et al. [12, 13], curve pattern in some scoliosis patients changed during bracing. However, these authors measured the changes in a small group of 50 patients using the King classification system, which is generally applied for the decision of the fusion surgery. Conversely, much of the literature investigating the effectiveness of orthotic management of AIS is usually based on the coronal patterns, which are defined by Scoliosis Research Society (SRS) [14].
The goal of this study was to investigate the incidence of changes in curve pattern based on the SRS classification, and to determine which radiographic or clinical parameters may be prognostic for whether the curve pattern changes during brace treatment in AIS patients.
Materials and methods
The brace treatment records between January 2002 and January 2011 in our scoliosis database were reviewed. All patients included in our analysis conformed with the SRS standardized criteria for AIS bracing [1]: diagnosis of AIS; age greater than 10 years at initiation of bracing; skeletal immaturity (Risser sign 0–2); initial Cobb angle of 25°–40°; more than 75 % compliance with the treatment program; and regular follow-up at a 3-month intervals until the weaning of brace or the necessity of surgical treatment due to the curve progression. At each visit, the actual daily bracing time during the past 3 months was recorded according to the information provided by the patients and their parents, and the compliance was calculated using the ratio of the actual daily bracing time to the recommended daily time in the present study [15]. Patients with developmental delay, chromosomal abnormalities, congenital heart disease, peripheral neuropathy, and myopathies were excluded. Patients who were braced prior to referral to our institution, and those who had undergone orthotic management less than 12 months prior to our study were also excluded. Magnetic resonance imaging scans were not routinely performed; however, they were performed for patients with atypical curvature, double thoracic curve, rapid progression, male gender, and abnormal neurologic findings [16–18]. Based on SRS recommendation [19], the Milwaukee brace was prescribed for patients with a major thoracic curve with an apex above T8, a double thoracic, or a triple curve, while the Boston brace has been reserved mainly for curves with an apex below T9. A total of 141 patients with idiopathic scoliosis (130 females and 11 males) who met the aforementioned criteria were included.
The clinical data including the patient’s gender, age, menarchal status in case of females, and the brace wearing schedule were reviewed. A protocol for brace treatment was prescribed, as reported previously [15]. The duration for which the brace was to be worn was adjusted during each follow-up based on the Risser sign, the menarchal status in females, and whether the Cobb angle was stable compared with earlier data. If the curve remained stable (i.e., the change in the Cobb angle of the main curve was less than 5°) [15, 20], the daily wearing time of the brace would not change for the first 6 months; rather, it would be shortened to 18 h per day for the next 6 months. The patients’ scoliosis was considered to be worse if the Cobb angle increased by more than 6° [15, 20]. If this occurred, then daily bracing time was maintained at 22 h per day. The scoliosis was thought to have improved if the Cobb angle decreased by more than 6° [15, 20] or if the Risser grade was greater than 3 and/or if the females were more than 1 year after menarche in females; for these patients, daily bracing time was shortened by 2–4 h per day at each follow-up.
Out-of-brace standing posterior–anterior and lateral radiographs were obtained in patients during at least every other visit. Lateral radiographs were performed before bracing, at the weaning of the bracing, and for any suspected sagittal plane abnormality. Several parameters were recorded from the standing posterior–anterior radiographs. The Cobb method [21] was used to measure the magnitude of the curve. Curve types were determined by assessing the curve magnitudes and levels. The curve with the largest Cobb angle was selected as the primary curve in patients with double major or triple scoliosis. The Risser sign was also noted on each posterior–anterior radiograph [22]. In some patients, when the leg-length discrepancy was suspected, clinical assessment of bony length inequalities and posterior–anterior pelvic radiographs were made to measure total limb discrepancies. To eliminate the effect of the leg-length discrepancy on the spine, patients were required to wear a heel lift and another X-ray was made to revaluate the curve pattern.
The termination of bracing treatment was defined as the cessation of bracing, when patients were thought to have reached maturity or when patients were recommended to undergo an operation. Our criteria for skeletal maturity were defined by <1 cm of vertical height over 6 months [1] and in females, more than 3 years since menarche (YSM) [23].
Results between the initiation and termination of bracing were compared. Patients were divided into two groups, those with changes in their curve pattern (Group A) and those without (Group B).
Our definition of curve pattern changes was divided into four categories, which were based on the coronal morphological features of the curves. Category 1 included the shift of the apical vertebrae of the main curve, e.g., the apex of the thoracic curve changed from T7 to T9 (Fig. 1). In some cases, the apex was at the level of the intervertebral disc, and the changes could have occurred from the intervertebral disc to the vertebra. However, only changes greater than or equal to one segment of vertebrae could be included in this study, e.g., a change in the apex from L1/2 disc to L2 was not counted as a change in this investigation. Category 2 included changes in curve span of greater than two vertebrae (Fig. 2). Category 3 included changes between the five coronal types defined by SRS based on the apex location: (1) single major thoracic, (2) single thoracolumbar/lumbar, (3) double major thoracic, (4) thoracic and lumbar/thoracolumbar, and (5) a multiple curve pattern of three or more curves (Figs. 3, 4). Category 4 included the changes of curve direction during follow-up, e.g., curves from right to left, vice versa. It was considered to have progressed if the Cobb angle at bracing termination increased by more than 6° compared with the initial Cobb angle.
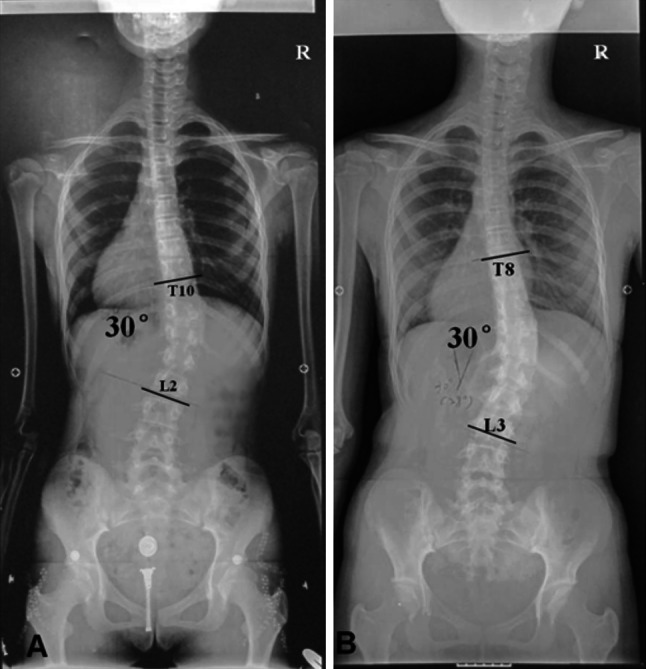
Fig. 1.

a A female patient (age = 12.1 years, 6 months premenarche, and Risser 0) with a single thoracic curve measured 30° with the apex of T7. b After 42 months of Milwaukee bracing, the apex of thoracic curve shifted from T7 to T9 at the cessation of bracing
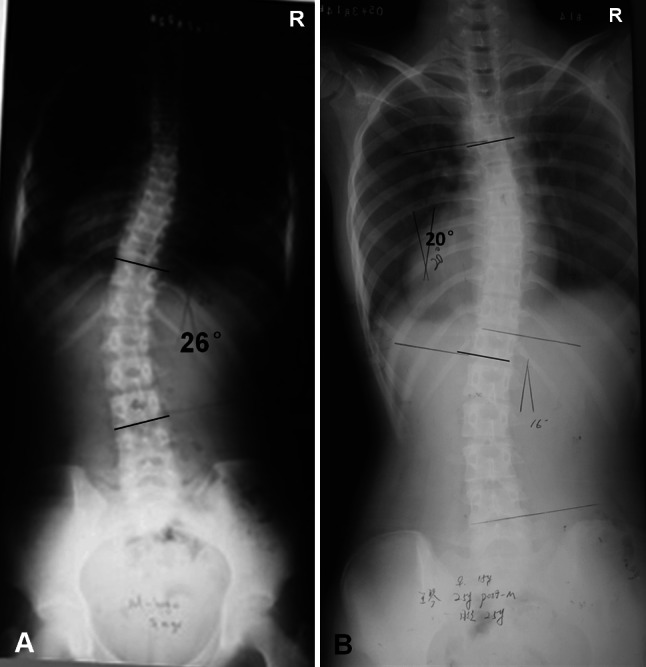
Fig. 2.
a A female patient (age = 14.0 years, 14 months postmenarche, and Risser 2) with a right single thoracic curve measured 30°. The curve span was from T10 to L2. b After 21 months of Boston bracing, the curve span changed from T10–L2 to T8–L3 at the cessation of bracing
Fig. 3.
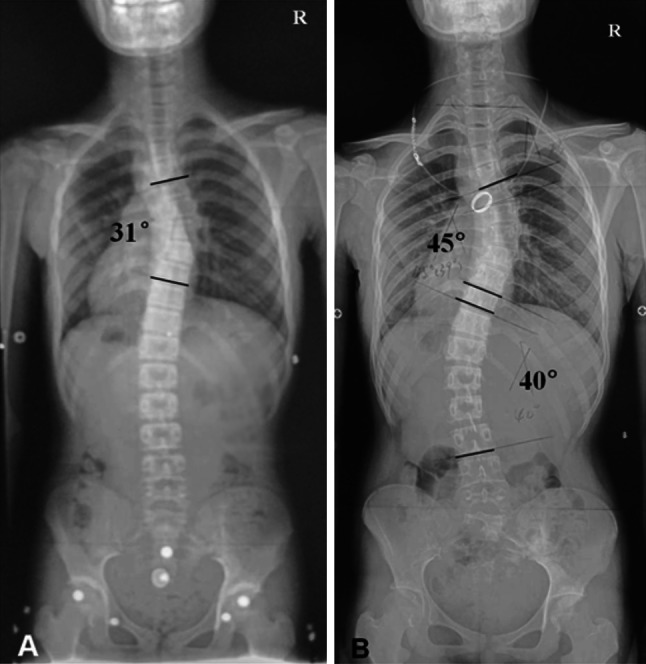
a A female patient (age = 12.3 years, 4 months premenarche, and Risser 1) with a single thoracic curve of 30°. b After 28 months of Milwaukee bracing, she presented with a double major scoliosis
Fig. 4.
a A female patient (age = 10.9 years, 1 month postmenarche, and Risser 0) with a single thoracolumbar curve of 26°. b After 35 months of Boston bracing, the girl presented with a small double curve at the cessation of bracing
Data were compared between Group A and Group B using Student’s t test or a χ 2 test as appropriate, and a P value of less than 0.05 was considered to be statistically significant. The Fisher exact test was used due to the small sample size (n < 5). A binary logistic regression analyses were also used to identify if the occurrence of the curve pattern change was dependent on the following factors: growth status-related factors, including chronological age, menstrual status, and Risser grade at the first visit; curve-related factors, including the initial curve pattern, curve magnitude, progression or not; and the brace type.
Results
At the initiation of bracing, on average, the mean chronologic age was 12.9-year old, and, the females were, on average 2.7 months past menarche (range 46 months before menarche to 14 months after; 44 premenarche and 86 postmenarche). The mean curve magnitude at brace initiation was 28.7° (range 25°–40°; SD 4.5°). Curves were categorized as single major thoracic in 50 patients (35.5 %, 48 females and 2 males), single thoracolumbar/lumbar in 50 (35.5 %, 47 females and 3 males), double major thoracic in 5 (3.6 %, 4 females and 1 male), thoracic and lumbar/thoracolumbar in 33 (23.4 %, 30 females and 3 males), and triple curves in 3 (2.1 %, 1 female and 2 males).
The age at the cessation of brace treatment was 15.6 ± 1.4-year old. The mean curve magnitude at the termination of bracing was 29.9° ± 8.6° (range 7°–54°). Mean time of bracing treatment was 2.5 years (range 1.0–5.5 years) for all patients, including those in whom brace treatment failed early and were treated surgically before completion of brace therapy.
Of these patients, 39 patients (38 females and 1 male, 27.7 %) were found to have changes in curve pattern. The average age at the time of initial recognition of curve pattern change was 13.9 ± 1.4 years, with the mean time of bracing being 1.4 years (range 0.7–2.8 years). Of these, 14 patients had apex shifts, 2 underwent curve span alternation, 22 experienced changes between the five coronal types, and one female had both the changes of apex and curve span. However, none of these patients underwent changes of curve direction. The brace was adjusted promptly when the changes of curve pattern were noted, e.g., the pads were placed to fit where the apical vertebrae were. For brace application, two patients required a change in brace type; one changed from the Boston to the Milwaukee brace, while the other changed from the Milwaukee to the Boston brace.
In the 14 patients with shift in their apical vertebrae, the apex of the curves moved caudad in 10 of the 15 curves, while in the remaining five curves, the apex moved cephalad. Of the two patients with curve span alteration, one experienced an increase in the curve span, while the other one had a decrease in the curve span. Of the 22 patients who experienced changes between the five coronal types, 8 changed from single lumbar/lumbothoracic to double major curve, 4 from single thoracic to double major curve, 4 from double major to single thoracic curve, 2 from single lumbar/thoracolumbar to single thoracic curve, and 4 from single thoracic to double thoracic curve.
Table 1 shows the comparisons of ages, menarchal status, Risser grade and Cobb angles between Group A and B at initiation and termination of bracing. At bracing initiation, patients in Group A had significantly lower menarchal status (P = 0.018) and lower Risser degree (Mann–Whitney U = 1,545.0, P = 0.025) than those in Group B.
Table 1.
Characteristics of 141 patients with AIS in the study
| Changed | Unchanged | P value | |
|---|---|---|---|
| N | 39 | 102 | |
| At initial | |||
| Age (years) | 12.7 ± 1.3 | 13.0 ± 1.5 | 0.242 |
| Cobb angle(°) | 30.1 ± 4.8 | 29.8 ± 4.4 | 0.789 |
| Months after menarche | 0.0 ± 0.8 | 0.3 ± 0.7 | 0.019* |
| At termination | |||
| Age (years) | 15.7 ± 1.4 | 15.5 ± 1.4 | 0.678 |
| Cobb angle(°) | 31.2 ± 6.9 | 29.4 ± 9.1 | 0.249 |
| Months after menarche | 31.6 ± 7.4 | 32.3 ± 8.7 | 0.632 |
| Correction of the cobb angle | 1.2 ± 7.0 | −0.5 ± 7.4 | 0.233 |
* Statistically significant
The impact of the initial curve pattern on the outcome, whether the patients underwent changes in curve pattern, was also analyzed (Table 2). The distributions of the three major curve types (single thoracic, single thoracolumbar/lumbar and double major curves) were similar between the two groups (P = 0.979).
Table 2.
Curve type at brace prescription
| Curve type | Changed | Unchanged | P value |
|---|---|---|---|
| Single thoracic | 11 (21.6 %) | 40 (78.4 %) | 0.979* |
| Single lumbar or thoracolumbar curves | 20 (32.3 %) | 42 (67.7 %) | |
| Double major curves | 7 (19.4 %) | 29 (80.6 %) |
* Statistically significant
As for brace type, there were 41 patients who were initially prescribed the Boston brace, while the remaining 100 patients wore Milwaukee brace. Twenty-two patients (41.5 %) with the Boston and seventeen patients (22.0 %) with the Milwaukee brace underwent changes in curve pattern. The proportion of Boston bracing in Group A was significantly higher than that in Group B (41.5 vs. 24.0 %, P = 0.023) (Table 3).
Table 3.
Relationship between brace type at bracing initiation and changes of curve pattern
| Brace type | Changed | Unchanged | P value |
|---|---|---|---|
| Milwaukee brace | 22 (22.0 %) | 78 (78.0 %) | 0.023* |
| Boston brace | 17 (41.5 %) | 24 (58.5 %) |
* Statistically significant
When curve pattern changes occurred, the mean curve magnitude for the 39 patients in Group A was 27.6° ± 6.5°. Compared with the termination of bracing treatment, the Cobb angle changed to 31.1° (range 20°–45°) for a mean increase of 3.5° (range −6° to 16°). Of these 39 patients, one (2.6 %) was considered improved, as the Cobb angle decreased by more than 6°, while 28 patients (71.8 %) were thought stable because the Cobb angle changed less than 6°. The remaining 10 patients (25.6 %) progressed by more than 6°.
Of the 141 patients, 21 experienced scoliosis progression. Of these 21 patients, 11 (52.4 %) had changes in curve pattern, while 10 of the 120 patients (23.3 %) whose curve stabilized underwent changes in curve pattern. The proportion of patients with curve progression ≥6° or who required surgery in Group A was significantly higher than that in Group B (P = 0.015) (Table 4).
Table 4.
Effectiveness of brace treatment with regard to changes of curve pattern
| Changed | Unchanged | P value | |
|---|---|---|---|
| Non-progressed | 28 (23.3 %) | 92 (76.7 %) | 0.015* |
| Progressed or surgery | 11 (52.4 %) | 10 (47.6 %) |
* Statistically significant
The results from binary logistic regression analysis showed that Risser sign of grade 0 or 1 (OR = 2.554, 95 % CI 1.03–6.31, P = 0.038), Boston brace (OR = 3.505, 95 % CI 1.47–8.34, P = 0.004), premenarche (OR = 2.181, 95 % CI 0.87–5.47, P = 0.094), were identified as risk factors in predicting changes of curve pattern.
Discussion
Orthoses are typically prescribed for skeletally immature AIS patients who have a mild or moderate curve to prevent further curve progression [1]. Although there is controversy concerning its effectiveness [11, 24–27], the fact that bracing produces better results than observation alone has been proven by numerous studies [2, 3, 6, 28]. Most of the studies measured changes in the coronal Cobb angle to assess the effectiveness of orthotic treatment. However, there were limited studies concentrating on the curve pattern changes that occur during orthotic treatment, which is most important for brace design and adjustment. This is the first study to exclusively evaluate the change in curvature based on coronal pattern defined by SRS in AIS patients.
In 2002, van Rhijn et al. [12] investigated changes in curve pattern during treatment with a Boston brace in AIS patients. He found that seven patients underwent changes in King type in a group of 50 patients with AIS. van Rhijn et al. [12] chose King’s classification system to evaluate conservative treatment, as they thought it important to be prepared for surgical intervention if necessary. However, the King classification system is accepted worldwide when determining fusion level. Obviously, it is not appropriate to evaluate the clinical outcome of bracing using the King classification system. The coronal patterns, which are defined by SRS, are widely used for brace design and applied for the evaluation of the results of bracing [5, 7, 29, 30]. In actuality, our study revealed that a portion of AIS patients displayed changes in curve pattern based on the above definition.
Though the mechanisms involved in changes in curve patterns are not clear, some factors by which orthoses correct deformities likely play a role. Wynarsky and Schultz [31] suggest that two different mechanisms might contribute to achieving correction of scoliosis. They are as follows: (1) active mechanisms, such as muscle control to shift the trunk away from the pressure areas; (2) passive mechanisms, such as external forces applied by the brace pads. We hypothesize that the above two mechanisms may play the major role in the changes in curve patterns. In addition, the aggravation of the secondary curve may also contribute to the curve pattern changes, such as from single thoracic to double major curve.
Many authors assume that as scoliosis is developing, the vertebral column tries to rebuild a new balance [12, 32–34]. Thus, in thoracic AIS, a lumbar curve develops to compensate for the deviation of the thoracic vertebrae to reconstruct the balance of the trunk. Possible explanations for this could be that the tuning/balancing mechanism of the spinal column tries to balance the spine, resulting in either spontaneous regression or the prevention of further progression of the curve. If this “tuning/balancing mechanism” fails, the curve will ultimately progress. Not only is this “tuning/balancing mechanism” involved in the progression of scoliosis, but also plays a role in the course of curve pattern changes. In a study using static and dynamic posturographic tests, Gauchard et al. [24] found that double major curves were the most stable curve type compared with other scoliotic curves in terms of global balance control because of biomechanical equilibrium. In the current study, we hypothesize that the evolution from a single curve to a double major curve was due to the aggravation of the secondary curve and improvement in the balance of the spine.
As is well known, various parts of the orthoses, such as the pads, increase tension in different areas. As such, they play a role in curvature change. Wong et al. [35] investigated the effectiveness and biomechanical factors of spinal orthoses in a prospective study. In the study, he found that the Cobb angle while wearing a brace strongly correlated with the pad pressure and strap tension. These findings suggest that the biomechanical function of orthoses may also play a role in the changes in curve patterns e.g., a double major curve may change into a single thoracic curve due to the biomechanical effects of the orthotics. In the present study, four patients experienced double major to single thoracic change, while two had curvature changes from single lumbar/thoracolumbar to single thoracic curve. The changes seemed due to the correction of the lumbar/thoracolumbar curve. In patients with leg-length difference, the re-equilibrium of the legs may also play a role due to its effect on the lumbar curve [36].
The apex location and the curve span were also of great significance in brace selection, as was confirmed by Nie et al. [37] in a study of a three-dimensional patient-specific finite element model of a thoracolumbosacral orthosis. The dynamic change in the apical vertebrae should be taken into account for patient-specific brace designing.
Correlates of curve pattern change
Our study showed that the patients in Group A were skeletally more immature than those in Group B in terms of the Risser sign and menarchal status. The interaction of increased growth potential with the external influences of the orthosis may have led to changes in the curve pattern. As the skeletally immature adolescent has a more flexible scoliosis, his (or her) spine may be more susceptible to curve pattern changes.
Whether the induced curve pattern changes differed with respect to the type of bracing was also investigated. The difference in the percentage of patients with Boston bracing was statistically significant between the two groups. As is well known, the mechanisms underlying the therapeutic effect of the Boston and Milwaukee brace are different [38]; however, whether this is caused by different brace characteristics is unknown.
Despite the unknown reasons for the changes in curve pattern, the present study reveals an interesting finding and confirms the findings of van Rhijn et al. [12]. The results of our study do show that the curve pattern may change during bracing. Therefore, we believe this investigation would serve as a useful reference in clinical practice, and the brace type, the pads, strap tension and other profiles of the orthoses should be adjusted to the new curve pattern.
Our results also show that a proportion of patients with curve progression ≥6° or, who meet criteria to receive surgery in Group A was significantly higher than that in Group B. The possible reason may lie in the less skeletal maturity in Group A. This was in line with a lot of studies [1, 3, 11], which confirmed that subjects who began bracing with greater skeletal immaturity had a higher rate of failure.
It is quite obvious that curve pattern in idiopathic scoliosis evolves rapidly during pubertal growth spurts and is relatively slow after reaching skeletal maturity. The current dilemma is that the incidence of curve pattern changes during the natural history of untreated scoliosis with similar curve magnitudes remains largely unknown. Thus, the limitation of this study lies in the fact that we are not quite sure whether the changes of curve pattern are influenced by bracing or are merely a pure reflection of natural history. Unfortunately, in our country, concerns from patients’ families over the progression of scoliosis have limited us to set up a randomized control trial to investigate the incidence of curve pattern changes in untreated AIS.
Conclusions
During bracing treatment, AIS patients may undergo changes in curve pattern. Our findings show that this phenomenon is more likely to happen in skeletally immature patients with a high-remaining growth potential and in those patients with Boston bracing.
Acknowledgments
This study was supported by Medical Science and technology development Foundation, Nanjing Department of Health (Grant No. ZKX11016) and the Fundamental Research Funds for the Central Universities (Grant No. 021414350009). No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Conflict of interest
None.
Footnotes
X. Zheng and X. Sun contributed equally to this work.
References
- 1.Richards BS, Bernstein RM, D’Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on bracing and nonoperative management. Spine (Phila Pa 1976) 2005;30:2068–2075. doi: 10.1097/01.brs.0000178819.90239.d0. [DOI] [PubMed] [Google Scholar]
- 2.Lonstein JE, Winter RB. The Milwaukee brace for the treatment of adolescent idiopathic scoliosis. A review of one thousand and twenty patients. J Bone Joint Surg Am. 1994;76:1207–1221. doi: 10.2106/00004623-199408000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Danielsson AJ, Hasserius R, Ohlin A, Nachemson AL. A prospective study of brace treatment versus observation alone in adolescent idiopathic scoliosis: a follow-up mean of 16 years after maturity. Spine (Phila Pa 1976) 2007;32:2198–2207. doi: 10.1097/BRS.0b013e31814b851f. [DOI] [PubMed] [Google Scholar]
- 4.Emans JB, Kaelin A, Bancel P, Hall JE, Miller ME. The Boston bracing system for idiopathic scoliosis. Follow-up results in 295 patients. Spine (Phila Pa 1976) 1986;11:792–801. doi: 10.1097/00007632-198610000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Howard A, Wright JG, Hedden D. A comparative study of TLSO, Charleston, and Milwaukee braces for idiopathic scoliosis. Spine (Phila Pa 1976) 1998;23:2404–2411. doi: 10.1097/00007632-199811150-00009. [DOI] [PubMed] [Google Scholar]
- 6.Wiley JW, Thomson JD, Mitchell TM, Smith BG, Banta JV. Effectiveness of the boston brace in treatment of large curves in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2000;25:2326–2332. doi: 10.1097/00007632-200009150-00010. [DOI] [PubMed] [Google Scholar]
- 7.Janicki JA, Poe-Kochert C, Armstrong DG, Thompson GH. A comparison of the thoracolumbosacral orthoses and providence orthosis in the treatment of adolescent idiopathic scoliosis: results using the new SRS inclusion and assessment criteria for bracing studies. J Pediatr Orthop. 2007;27:369–374. doi: 10.1097/01.bpb.0000271331.71857.9a. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg CJ, Dowling FE, Hall JE, Emans JB. A statistical comparison between natural history of idiopathic scoliosis and brace treatment in skeletally immature adolescent girls. Spine (Phila Pa 1976) 1993;18:902–908. doi: 10.1097/00007632-199306000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Noonan KJ, Weinstein SL, Jacobson WC, Dolan LA. Use of the Milwaukee brace for progressive idiopathic scoliosis. J Bone Joint Surg Am. 1996;78:557–567. doi: 10.2106/00004623-199604000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg CJ, Moore DP, Fogarty EE, Dowling FE. Adolescent idiopathic scoliosis: the effect of brace treatment on the incidence of surgery. Spine (Phila Pa 1976) 2001;26:42–47. doi: 10.1097/00007632-200101010-00009. [DOI] [PubMed] [Google Scholar]
- 11.Dolan LA, Weinstein SL. Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence-based review. Spine (Phila Pa 1976) 2007;32:S91–S100. doi: 10.1097/BRS.0b013e318134ead9. [DOI] [PubMed] [Google Scholar]
- 12.van Rhijn LW, Plasmans CM, Veraart BE. Changes in curve pattern after brace treatment for idiopathic scoliosis. Acta Orthop Scand. 2002;73:277–281. doi: 10.1080/000164702320155248. [DOI] [PubMed] [Google Scholar]
- 13.van Rhijn LW, Jansen EJ, Plasmans CM, Veraart BE. Changing curve pattern in infantile idiopathic scoliosis: family report with a follow-up of 15 years. Spine (Phila Pa 1976) 2001;26:E373–E376. doi: 10.1097/00007632-200108150-00021. [DOI] [PubMed] [Google Scholar]
- 14.Coonrad RW, Murrell GA, Motley G, Lytle E, Hey LA. A logical coronal pattern classification of 2,000 consecutive idiopathic scoliosis cases based on the scoliosis research society-defined apical vertebra. Spine (Phila Pa 1976) 1998;23:1380–1391. doi: 10.1097/00007632-199806150-00016. [DOI] [PubMed] [Google Scholar]
- 15.Qiu Y, Sun X, Cheng JC, Zhu F, Li W, Zhu Z, Wang B, Yu Y. Bone mineral accrual in osteopenic and non-osteopenic girls with idiopathic scoliosis during bracing treatment. Spine (Phila Pa 1976) 2008;33:1682–1689. doi: 10.1097/BRS.0b013e31817b5b9e. [DOI] [PubMed] [Google Scholar]
- 16.Wu L, Qiu Y, Wang B, Zhu ZZ, Ma WW. The left thoracic curve pattern: a strong predictor for neural axis abnormalities in patients with “idiopathic” scoliosis. Spine (Phila Pa 1976) 2010;35:182–185. doi: 10.1097/BRS.0b013e3181ba6623. [DOI] [PubMed] [Google Scholar]
- 17.Richards BS, Sucato DJ, Johnston CE, Diab M, Sarwark JF, Lenke LG, Parent S. Right thoracic curves in presumed adolescent idiopathic scoliosis: which clinical and radiographic findings correlate with a preoperative abnormal magnetic resonance image? Spine (Phila Pa 1976) 2010;35:1855–1860. doi: 10.1097/BRS.0b013e3181d4f532. [DOI] [PubMed] [Google Scholar]
- 18.Shurtleff H, Warner M, Poliakov A, Bournival B, Shaw DW, Ishak G, Yang T, Karandikar M, Saneto RP, Browd SR, Ojemann JG. Functional magnetic resonance imaging for presurgical evaluation of very young pediatric patients with epilepsy. J Neurosurg Pediatr. 2010;5:500–506. doi: 10.3171/2009.11.PEDS09248. [DOI] [PubMed] [Google Scholar]
- 19.Lonstein JE (2003) Milwaukee brace treatment of scoliosis. Scoliosis Research Society Bracing Manual. (http://www.srs.org/professionals/education_materials/SRS_bracing_manual/index.htm)
- 20.Yrjonen T, Ylikoski M, Schlenzka D, Poussa M. Results of brace treatment of adolescent idiopathic scoliosis in boys compared with girls: a retrospective study of 102 patients treated with the Boston brace. Eur Spine J. 2007;16:393–397. doi: 10.1007/s00586-006-0167-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cobb JR (1958) Scoliosis; quo vadis. J Bone Joint Surg Am 40-A:507–510 [PubMed]
- 22.Risser JC. The Iliac apophysis; an invaluable sign in the management of scoliosis. Clin Orthop. 1958;11:111–119. [PubMed] [Google Scholar]
- 23.Wang WW, Xia CW, Zhu F, Zhu ZZ, Wang B, Wang SF, Yeung BH, Lee SK, Cheng JC, Qiu Y. Correlation of Risser sign, radiographs of hand and wrist with the histological grade of iliac crest apophysis in girls with adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2009;34:1849–1854. doi: 10.1097/BRS.0b013e3181ab358c. [DOI] [PubMed] [Google Scholar]
- 24.Gauchard GC, Lascombes P, Kuhnast M, Perrin PP. Influence of different types of progressive idiopathic scoliosis on static and dynamic postural control. Spine (Phila Pa 1976) 2001;26:1052–1058. doi: 10.1097/00007632-200105010-00014. [DOI] [PubMed] [Google Scholar]
- 25.Sadeghi H, Allard P, Barbier F, Gatto L, Chavet P, Rivard CH, Hinse S, Simoneau M. Bracing has no effect on standing balance in females with adolescent idiopathic scoliosis. Med Sci Monit. 2008;14:CR293–CR298. [PubMed] [Google Scholar]
- 26.Karol LA. Effectiveness of bracing in male patients with idiopathic scoliosis. Spine (Phila Pa 1976) 2001;26:2001–2005. doi: 10.1097/00007632-200109150-00013. [DOI] [PubMed] [Google Scholar]
- 27.Dickson RA, Weinstein SL. Bracing (and screening)—yes or no? J Bone Joint Surg Br. 1999;81:193–198. doi: 10.1302/0301-620X.81B2.9630. [DOI] [PubMed] [Google Scholar]
- 28.Heary RF, Bono CM, Kumar S. Bracing for scoliosis. Neurosurgery. 2008;63:125–130. doi: 10.1227/01.NEU.0000320387.93907.97. [DOI] [PubMed] [Google Scholar]
- 29.Galante J, Schultz A, Dewald RL, Ray RD. Forces acting in the Milwaukee brace on patients undergoing treatment for idiopathic scoliosis. J Bone Joint Surg Am. 1970;52:498–506. [PubMed] [Google Scholar]
- 30.Mulcahy T, Galante J, DeWald R, Schultz A, Hunter JC. A follow-up study of forces acting on the Milwaukee brace on patients undergoing treatment for idiopathic scoliosis. Clin Orthop Relat Res. 1973;93:53–68. doi: 10.1097/00003086-197306000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Wynarsky GT, Schultz AB. Optimization of skeletal configuration: studies of scoliosis correction biomechanics. J Biomech. 1991;24:721–732. doi: 10.1016/0021-9290(91)90336-L. [DOI] [PubMed] [Google Scholar]
- 32.Jansen RC, van Rhijn LW, Duinkerke E, van Ooij A. Predictability of the spontaneous lumbar curve correction after selective thoracic fusion in idiopathic scoliosis. Eur Spine J. 2007;16:1335–1342. doi: 10.1007/s00586-007-0320-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Modi HN, Suh SW, Yang JH, Hong JY, Venkatesh K, Muzaffar N. Spontaneous regression of curve in immature idiopathic scoliosis—does spinal column play a role to balance? An observation with literature review. J Orthop Surg Res. 2010;5:80. doi: 10.1186/1749-799X-5-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Rhijn LW, Veraart BE, Plasmans CM. Application of a lumbar brace for thoracic and double thoracic lumbar scoliosis: a comparative study. J Pediatr Orthop B. 2003;12:178–182. doi: 10.1097/00009957-200305000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Wong MS, Mak AF, Luk KD, Evans JH, Brown B. Effectiveness and biomechanics of spinal orthoses in the treatment of adolescent idiopathic scoliosis (AIS) Prosthet Orthot Int. 2000;24:148–162. doi: 10.1080/03093640008726538. [DOI] [PubMed] [Google Scholar]
- 36.Papaioannou T, Stokes I, Kenwright J. Scoliosis associated with limb-length inequality. J Bone Joint Surg Am. 1982;64:59–62. [PubMed] [Google Scholar]
- 37.Nie WZ, Ye M, Liu ZD, Wang CT. The patient-specific brace design and biomechanical analysis of adolescent idiopathic scoliosis. J Biomech Eng. 2009;131:041007. doi: 10.1115/1.3049843. [DOI] [PubMed] [Google Scholar]
- 38.Negrini S, Zaina F, Atanasio S. BRACE MAP, a proposal for a new classification of braces. Stud Health Technol Inform. 2008;140:299–302. [PubMed] [Google Scholar]


