Abstract
Purpose
The objective of this study was to evaluate 2 years post-surgical loss of three-dimensional correction in adolescent idiopathic scoliosis (AIS) patients using multi-planar reconstruction computed tomography (CT).
Methods
Twenty-seven AIS patients treated by segmental pedicle screw (PS) constructs were included in this study. Correction in the axial plane was evaluated using the “relative apical vertebral rotation angle” (rAVR), defined as the difference between the axial rotation angles of the upper instrumented vertebra and the apical vertebra on reconstructed axial CT images. The Cobb angle of the main curve and apical vertebral translation was measured to evaluate the coronal correction. Thoracic kyphosis was also measured for the evaluation of sagittal profile. Measurements were performed before surgery, and 1 week and 2 years after surgery. The relationships between the correction losses and skeletal maturity, and variety of spinal constructs were also evaluated.
Results
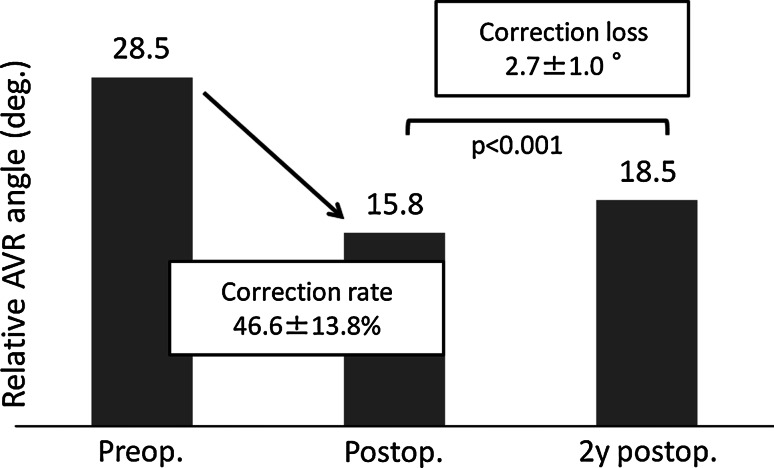
The mean preoperative Cobb angle of the major curve was 59.1° ± 11.2° before and 13.0° ± 7.2° immediately after surgery. Two years later, the mean Cobb angle had increased significantly, to 15.5° ± 7.8°, with a mean correction loss of 2.5° ± 1.5° (p < 0.001). The mean preoperative rAVR of 28.5° ± 8.4° was corrected to 15.8° ± 7.8° after surgery. It had increased significantly to 18.5 ± 8.4 by 2 years after surgery, with a mean correction loss of 2.7° ± 1.0° (p < 0.001). The mean correction losses for both the Cobb angle and rAVR were significantly greater in the skeletally immature patients. The significant correlations were recognized between the correction losses and the proportion of multi-axial screws, and the materials of constructs.
Conclusions
Statistically significant loss of correction in the Cobb angle and apical vertebral axial rotation angle (AVR) were recognized 2 years after surgery using PS constructs. The correction losses, especially AVR, were more evident in the skeletally immature patients, and in patients treated with more multi-axial screws and with titanium constructs rather than with stainless constructs.
Keywords: Adolescent idiopathic scoliosis, Apical vertebral rotation, Correction loss, Coronal correction
Background
Pedicle screw (PS) constructs can provide superior three-dimensional correction and maintenance of the correction compared with hook and wire constructs in the surgical treatment of adolescent idiopathic scoliosis (AIS) [1–6]. However, correction loss has been noted in the coronal plane on X-rays, even when PS constructs are used [2–6], although correction loss in the axial plane has not been well described.
Historically, the Harrington rod and Luque rod instrumentation achieved correction in the coronal plane; but, neither method effectively derotated the vertebrae sufficiently to correct the rib hump [7–9]. Furthermore, a significant correction loss in the coronal deformity was observed. Cotrel-Dubousset (CD) instrumentation was invented specifically for the three-dimensional correction of spinal deformity, but its ability to derotate vertebrae was still considered to be insufficient and significant correction loss was observed [10–14]. Recently, CD constructs have been combined with PSs for the fixation of the lumbar spine [15, 16] and with hooks and sublaminar wires for the fixation of the thoracic spine [17, 18], thereby, enabling remarkable improvement of curve correction compared with the classical CD constructs [15–18]. However, effective correction of the axial plane rotational deformity was achieved after the emergence of the segmental thoracic PS constructs with the derotation maneuver [19, 20]. Since PS can obtain a three-column purchase and a longer moment arm [21], superior rotational correction force can be applied to the spinal column than with hook or wire constructs, and the construct is expected to maintain the correction effectively after surgery.
The purpose of this study was to evaluate the correction loss of spinal correction at 2 years after surgery, especially focusing on the apical vertebral axial rotation angle (AVR) using the relative AVR angle (rAVR) defined as the difference between the axial rotation angle of the upper instrumented vertebra and the apical vertebra to reduce the positional influence. We studied patients with AIS who had undergone posterior correction surgery with segmental PS constructs, at 1 week and 2 years after surgery, using multi-planar reconstructed axial computed tomography (CT) images.
Materials and methods
Twenty-seven patients (5 male and 22 female) with AIS who underwent posterior correction and fusion surgeries with PS constructs were included in this study. The mean age at the time of surgery was 13.4 years (range 10–17 years). The curve types were classified by the Lenke classification which was developed to provide a comprehensive and reliable means to categorize all surgical AIS curves. Lenke type I (18 patients); single thoracic curve, type V (5 patients); lumbar curve, and type VI (4 patients); double major curve in thoracic and lumbar spine. The skeletal maturity was indicated by Risser sign which was graded from 0 to 5 by the progression in the ossification of the apophysis of the iliac crest. Risser grades for these patients were Risser 0 (7 patients), Risser 2 (5 patients), Risser 3 (4 patients), and Risser 4 (11 patients).
Standing postero-anterior and lateral X-ray films and CT images showing a 1-mm thickness using a CT unit of Aquillion 64 (Toshiba Medical Systems, Tokyo, Japan) and Light Speed VCT (GE Healthcare, Milwaukee) were obtained from all patients before surgery, and 1 week and 2 years after surgery. The parameters on X-rays for evaluating corrections were Cobb angles of major curves (Fig. 1), kyphosis of the thoracic spine (T5–T12), apical vertebral translation (AVT), and rAVR. AVT was defined as a distance between the center of the apical vertebra and the C7 plumb line for the thoracic major curve and center of sacral vertical line (CSVL) for the lumbar major curve on standing X-rays. AVR were measured using the Aaro and Dahlborn method [22] on the reconstructed CT images showing the plane parallel to the endplate of each vertebra. Since the AVR changes, depending on the patient’s pelvic position during the CT examination, we used the rAVR, to minimize measurement errors. The rAVR was defined as the difference between the axial rotation angle of the upper instrumented vertebra and the apical vertebra (Figs. 2, 3). All measurements were performed using image-analysis software (Real INTAGE, Tokyo, Japan) [23, 24]. The axial images for every vertebra were obtained as follows. First, reconstructed images showing the axial plane parallel to the upper end plate of the vertebrae in the coronal plane were obtained. These images were further reconstructed to show the axial plane parallel to the upper end plate of each vertebra in the sagittal plane. The angle of trunk rotation (ATR) was evaluated using Adam’s forward bending test before surgery, and 1 month and 2 years after surgery, to assess the clinical relevance of our radiographic evaluation.
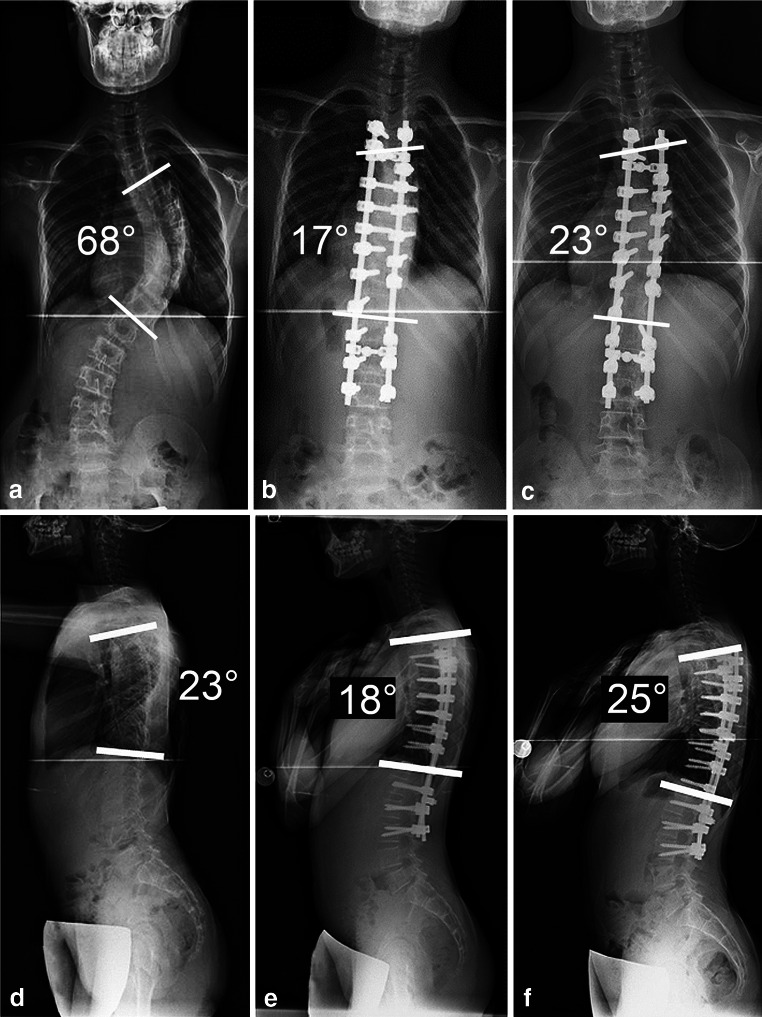
Fig. 1.
Loss of Cobb angle correction. A 10-year-old girl with Risser 0. The preoperative Cobb angle of 68° at the main thoracic curve (a) was corrected to 17° after surgery (b). Two years later, the Cobb angle had increased to 23° with a correction loss of 5° (c). The preoperative thoracic kyphosis angle at T5–T12 of 23° before surgery (d) was decreased to 18° after surgery (e). Two years later, the thoracic kyphosis increase to 25° mainly at proximal thoracic area (f)
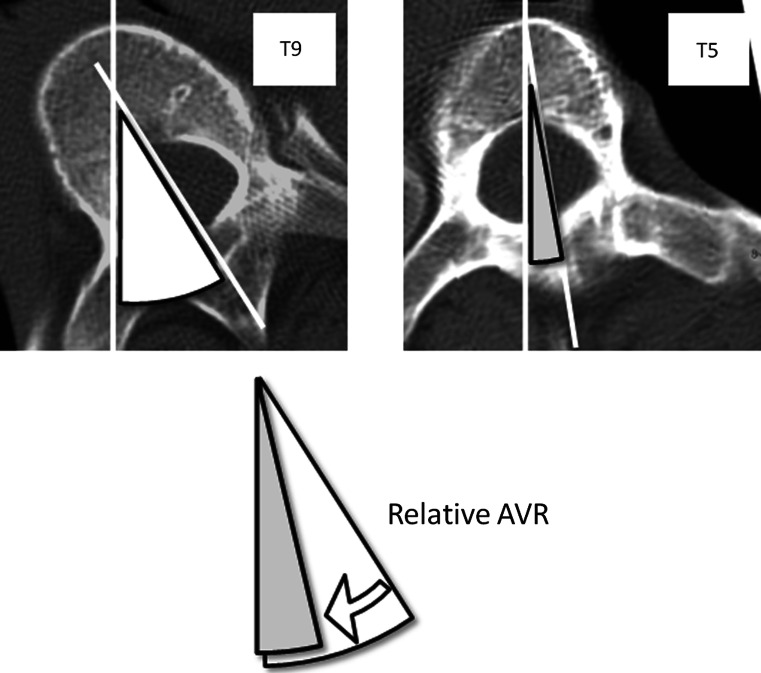
Fig. 2.
Relative AVR angle. Relative AVR angle is defined as the difference of the angles between the UIV (T5) and the apical vertebra (T9)
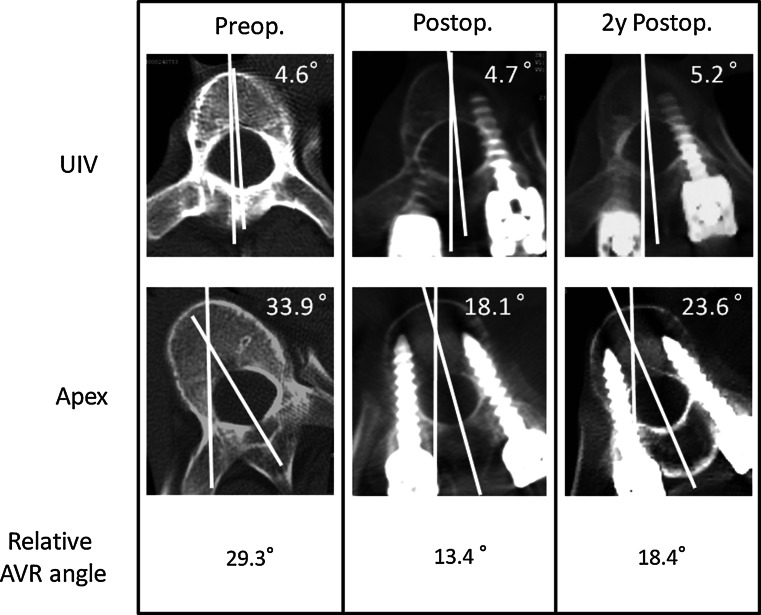
Fig. 3.
Loss of relative AVR angle. A 10-year-old girl with Risser 0. Preoperative relative AVR angle was 29.3°, which was calculated from the difference of rotational angles between the UIV and the apical vertebra. The relative AVR angle was corrected to 13.4° after surgery. Two years later, the relative AVR angle had increased to 18.4° with the correction loss of 5°
To determine the risk factors for the correction losses, the relationship between the loss of correction parameters (rAVR, Cobb angle, AVT, thoracic kyphosis, and ATR) and the factors below were evaluated: (1) skeletal maturity, (2) chronological age at surgery, (3) materials of spinal instrumentations (titanium or stainless), (4) number of fused vertebrae, (5) length of PSs (shorter screws; 30 mm or shorter, or longer screws; longer than 30 mm) (Table 1), (6) types of PSs (multi-axial or mono-axial) (Table 1), (7) preoperative and postoperative values, and the amount of correction obtained by surgery. To evaluate the relationship between skeletal maturity and the correction losses, the patients were divided into two groups for comparison: those with Risser 0–2 (12 patients) or with Risser 3–4 (15 patients).
Table 1.
Variety of construct combinations used for surgeries
| Case | Material | Rod diameter (mm) | Mono-axial screw (diameter: mm, length: mm) | Multi-axial screw (diameter: mm, length: mm) | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5.5, 25 | 5.5, 30 | 5.5, 35 | 5.5, 40 | 5.5, 45 | 6.5, 35 | 6.5, 40 | 6.5, 45 | 6.5, 50 | Total | 5.5, 25 | 5.5, 30 | 5.5, 35 | 5.5, 40 | 5.5, 45 | 6.5, 35 | 6.5, 40 | 6.5, 45 | 7.5, 45 | 7.5, 50 | Total | |||
| 1 | Titanium | 5.5 | 6 | 2 | 1 | 4 | 9 | 6 | 9 | ||||||||||||||
| 2 | Titanium | 5.5 | 2 | 1 | 1 | 5 | 2 | 5 | |||||||||||||||
| 3 | Stainless steel | 5.5 | 2 | 4 | 3 | 3 | 1 | 4 | 2 | 2 | 13 | ||||||||||||
| 4 | Stainless steel | 5.5 | 4 | 6 | 1 | 3 | 2 | 1 | 2 | 14 | |||||||||||||
| 5 | Stainless steel | 5.5 | 1 | 6 | 7 | 4 | 4 | 8 | |||||||||||||||
| 6 | Stainless steel | 5.5 | 9 | 8 | 1 | 5 | 2 | 9 | |||||||||||||||
| 7 | Titanium | 5.5 | 10 | 2 | 10 | 2 | 5 | 4 | 11 | ||||||||||||||
| 8 | Stainless steel | 5.5 | 4 | 4 | 1 | 4 | 5 | 3 | 2 | 13 | |||||||||||||
| 9 | Stainless steel | 5.5 | 11 | 9 | 9 | 11 | |||||||||||||||||
| 10 | Titanium | 5.5 | 10 | 2 | 1 | 7 | 2 | 3 | 2 | 13 | |||||||||||||
| 11 | Titanium | 5.5 | 4 | 1 | 6 | 1 | 7 | 3 | 1 | 1 | 1 | 1 | 14 | ||||||||||
| 12 | Stainless steel | 5.5 | 2 | 15 | 10 | ||||||||||||||||||
| 13 | Stainless steel | 5.5 | 9 | 2 | 1 | 1 | 8 | 4 | 1 | 3 | 13 | ||||||||||||
| 14 | Stainless steel | 5.5 | 7 | 3 | 1 | 4 | 1 | 3 | 11 | ||||||||||||||
| 15 | Stainless steel | 5.5 | 12 | 1 | 5 | 4 | 1 | 13 | |||||||||||||||
| 16 | Titanium | 5.5 | 1 | 2 | 7 | 1 | 5 | 1 | 2 | 2 | 11 | ||||||||||||
| 17 | Stainless steel | 5.5 | 3 | 3 | 2 | 2 | 4 | 1 | 1 | 1 | 1 | 10 | |||||||||||
| 18 | Titanium | 5.5 | 8 | 3 | 4 | 6 | 2 | 4 | 15 | ||||||||||||||
| 19 | Titanium | 5.5 | 7 | 2 | 4 | 3 | 1 | 9 | |||||||||||||||
| 20 | Titanium | 5.5 | 2 | 9 | 1 | 3 | 1 | 1 | 1 | 12 | |||||||||||||
| 21 | Titanium | 5.5 | 6 | 2 | 2 | 4 | 2 | 1 | 1 | 10 | |||||||||||||
| 22 | Titanium | 5.5 | 2 | 6 | 1 | 3 | 7 | 1 | 4 | 2 | 12 | ||||||||||||
| 23 | Titanium | 5.5 | 1 | 10 | 9 | 2 | 6 | 1 | 11 | ||||||||||||||
| 24 | Titanium | 5.5 | 4 | 4 | 4 | 2 | 2 | 8 | |||||||||||||||
| 25 | Titanium | 5.5 | 10 | 4 | 1 | 1 | 1 | 1 | 10 | ||||||||||||||
| 26 | Titanium | 5.5 | 2 | 2 | 2 | 1 | 5 | 1 | 2 | 2 | 7 | ||||||||||||
| 27 | Titanium | 5.5 | 3 | 7 | 2 | 4 | 2 | 2 | 12 | ||||||||||||||
The clinical significance of the correction losses was evaluated using SRS-22 scores 2 years after surgery. The correlations between the correction losses and each SRS-22 domain and the total score were evaluated using a Spearman’s rank correlation coefficient.
Surgical procedures included segmental placement of the PS, placement of the first rod on the concave side for the thoracic curve, rod rotation, direct vertebral derotation, and placement of the second rod as described previously [25].
All the measurements were performed by the first author (GC). Intra-observer reliability was assessed by measuring the CT scans of 10 patients at different times. The coefficient of variation was 3.9 % for the axial rotation angle. Inter-observer reliability was assessed by comparing the measurement results from the CT scans of 10 patients by the first (GC) and second (KW) authors. The coefficient of variation was 4.7 % for the axial rotation angle of the vertebra. All the coefficients were <5 %, indicating good inter- and intra-observer reliability.
A one-tailed paired t test was used to analyze the difference in X-ray parameters and the rAVR among before surgery, and 1 week and 2 years after surgery. P < 0.05 was considered to be significant. A two-way repeated measures ANOVA was used to analyze the difference between the Risser 0–2 group and the Risser 3–4 group, and between the stainless steel group and the titanium group regarding the correction losses. To evaluate the relationship between the correction losses and factors potentially related to the losses, a Spearman’s rank correlation coefficient was used. The relationship between the correction loss of the ATR angle and the correction loss of the rAVR was also evaluated using a Spearman’s rank correlation coefficient.
Results
Loss of correction in the coronal and sagittal planes
The mean preoperative Cobb angle of the major curve was 59.1° ± 11.2° (range 45.5°–80.6°). After surgery, the curves were corrected to a mean Cobb angle of 13.0° ± 7.2° (range 3.3°–31.0°) with a mean correction rate of 78.7 % (range 55.8–92.3 %) (Fig. 4). Two years after surgery, the mean Cobb angle had increased significantly to 15.5° ± 7.8° (range 6.3°–35.9°), with a mean correction loss of 2.5° ± 1.6° (range 0.7°–6.2°) (p < 0.001). The mean preoperative AVT of 56.6 ± 17.5 mm was decreased to 15.3 ± 9.4 mm at 1 week after surgery. Two years after surgery, the mean value had increased significantly to 19.1 ± 12.3 mm, with a mean loss of 3.9 ± 8.4 mm (p < 0.001). In addition, the mean preoperative thoracic kyphosis angle (T5-12), 25.7° ± 11.8° (range 10.8°–60.2°), was decreased significantly to 20.6° ± 8.8° (range 7.6°–43.6°) at 1 week after surgery (p = 0.006). Two years later, the mean value had increased to 22.2 ± 9.0 (range 8.9°–44.9°), which was not significantly different from the previous value (p = 0.48).
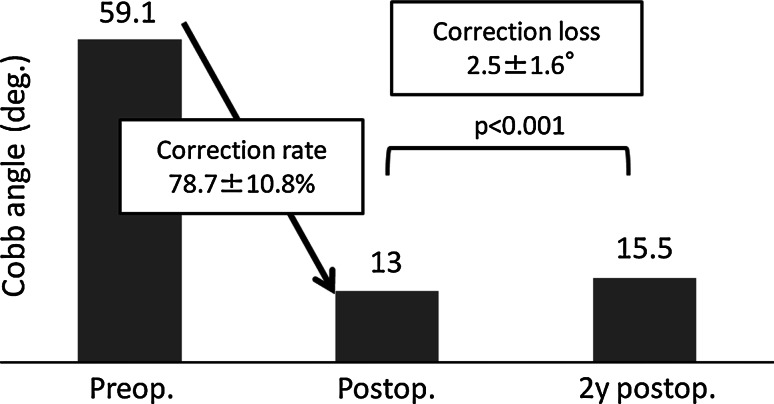
Fig. 4.
Cobb angle correction changes. The mean preoperative Cobb angle of 63.6° was corrected to 14° with a mean correction rate of 78.1 %. Two years after the surgery, the mean Cobb angle had increased to 16.6° with a mean correction loss of 2.6°
Loss of correction in the axial plane
The mean preoperative rAVR, 28.5° ± 8.4° (range 18.5°–49.1°), was corrected to 15.8° ± 7.8° (range 5.7°–34.8°) at 1 week after surgery, with a mean correction rate of 46.6 ± 13.8 % (range 26.4–78.9 %) (Fig. 5). Two years later, this angle had increased significantly, to 18.5° ± 8.4° (range 8.3°–39.2°), with a mean correction loss of 2.7° ± 1.0° (range 1.3°–4.8°) (p < 0.001). The mean preoperative ATR angle, 19.3 ± 7.3 (range 8.0°–45.0°), was corrected to 5.4° ± 3.8° (range 1.0°–17.0°) at 1 week after surgery, with a mean correction rate of 72.2 ± 14.4 % (range 46.2–94.1 %). Two years later, the mean ATR angle had increased significantly, to 7.9° ± 4.4° (range 2.0°–20.0°), with a mean correction loss of 2.4° ± 1.4° (range 0.0°–7.0°) (p < 0.001). The correction loss of the ATR angle correlated significantly with that of the rAVR (correlation coefficient = 0.442, p = 0.0243).
Fig. 5.
Relative AVR angle correction changes. The mean preoperative AVR angle of 33° was corrected to 18.4° with a mean correction rate of 43.6 % after surgery. Two years later, the mean relative AVR had increased to 21.3° with a mean correction loss of 2.9°
Evaluation of factors influence postoperative correction losses
Skeletal maturity The Risser 0–2 group consisted of 12 patients and the Risser 3–4 was consisted of 15 patients. The Risser 0–2 group included seven pre-menarchial females, and six patients with open triradiate cartilage. The mean correction loss of rAVR in the Risser 0–2 group was significantly larger than that in the Risser 3–5 group (3.18° ± 0.27° vs. 2.27° ± 0.69°, p = 0.007) (Table 2). The mean correction loss of Cobb angle in the Risser 0–2 group was also significantly larger than that in the Risser 3–5 group (3.12° ± 1.52° vs. 1.87° ± 0.98°, p = 0.0153). The mean correction loss of ATR in the Risser 0–2 group was significantly larger than that in the Risser 3–5 group (3.42 ± 1.68 vs. 1.87 ± 1.06, p = 0.005). Although the mean correction loss of AVT and kyphosis angle was larger in the Risser 0–2 group, no significant differences were recognized between the two groups.
Chronological age at surgery No significant correlation was recognized between the chronological age at surgery and the correction losses of rAVR, Cobb angle, AVT, kyphosis, and ATR (Table 3).
Materials of spinal instrumentations The titanium constructs were used in 16 patients and the stainless steel constructs were used in 11 patients for the surgeries. The mean correction loss of rAVR in the titanium group was significantly greater than that of the stainless steel group (2.29 ± 0.65 vs. 2.93 ± 0.99, p = 0.0183) (Table 4).
Number of fused vertebrae The mean number of fused vertebrae was 9.7 ± 2.4 vertebrae (range 5–14 vertebrae) (Table 3). No significant correlation was recognized between the number of fused vertebrae and the correction losses.
Length of PSs Totally, 458 PSs were used for all 27 patients with the mean number of 17.0 ± 3.5 PSs per patient (Tables 1, 3). The number of screws used for each screw length was as follows: 25 mm: 5, 30 mm: 145, 35 mm: 171, 40 mm: 101, 45 mm: 28, and 50 mm: 2. No significant correlation was observed between the proportion of shorter PS (30 mm or shorter) and the correction losses (Table 3).
Types of PSs Among 458 PSs, 164 screws were multi-axial type (35.2 %), and 294 screws were mono-axial type (64.8 %) (Table 1). The proportion of multi-axial screw was significantly correlated with the correction loss of rAVR and ATR with the correlation coefficients of 0.415 and 0.563, respectively (Table 2).
Preoperative and postoperative values, and the amount of correction obtained by surgery (Table 3) The preoperative and postoperative rAVR were significantly correlated with the correction losses of rAVR with correlation coefficients of 0.597 and 0.516, respectively, i.e. larger preoperative rAVR or postoperative rAVR were correlated with larger correction losses of rAVR. Preoperative and postoperative ATR were also significantly correlated with the correction loss of ATR with the correlation coefficients of 0.525 and 0.426, respectively. Larger preoperative kyphosis and decrease in kyphosis after surgery were correlated with the increase in kyphosis at 2 years after surgery.
Table 2.
Correction parameters and bone maturity
| Risser 0–2 | Risser 3–5 | p value | |
|---|---|---|---|
| rAVR (°) | |||
| Preoperation | 31.78 ± 10.31 | 26.09 ± 5.42 | 0.076 |
| Postoperation | 18.42 ± 10.55 | 13.7 ± 3.98 | 0.121 |
| Postoperative 2 years | 21.60 ± 11.34 | 15.97 ± 1.08 | 0.086 |
| Correction loss at 2 years | 3.18 ± 0.27 | 2.27 ± 0.69 | 0.007* |
| Cobb angle (°) | |||
| Preoperation | 64.38 ± 10.1 | 55.32 ± 10.09 | 0.029* |
| Postoperation | 15.84 ± 8.18 | 10.79 ± 5.65 | 0.692 |
| Postoperative 2 years | 18.96 ± 8.73 | 12.65 ± 5.79 | 0.333 |
| Correction Loss at 2 years | 3.12 ± 1.52 | 1.87 ± 0.98 | 0.015* |
| AVT (mm) | |||
| Preoperation | 58.98 ± 17.84 | 54.61 ± 17.63 | 0.530 |
| Postoperation | 16.27 ± 10.11 | 14.49 ± 9.03 | 0.635 |
| Postoperative 2 years | 23.02 ± 15.04 | 16.05 ± 8.93 | 0.147 |
| Correction loss at 2 years | 6.75 ± 11.79 | 1.55 ± 2.96 | 0.110 |
| Thoracic kyphosis angle (°) | |||
| Preoperation | 22.61 ± 11.84 | 27.17 ± 9.05 | 0.267 |
| Postoperation | 16.83 ± 6.62 | 23.61 ± 9.48 | 0.046* |
| Postoperative 2 years | 18.43 ± 6.92 | 25.30 ± 9.57 | 0.047* |
| Correction loss at 2 years | 1.69 ± 0.45 | 1.60 ± 0.78 | 0.695 |
| ATR (°) | |||
| Preoperation | 22.92 ± 8.99 | 16.47 ± 3.96 | 0.019* |
| Postoperation | 7.67 ± 4.16 | 3.67 ± 2.32 | 0.004* |
| Postoperative 2 years | 11.08 ± 5.05 | 5.53 ± 2.61 | 0.001* |
| Correction loss at 2 years | 3.42 ± 1.68 | 1.87 ± 1.06 | 0.005* |
* Significant difference by a two-way repeated measures ANOVA
Table 3.
Correlation between the correction losses and chronological age at surgery, screw types, screw lengths, preoperative and postoperative value, and amount of correction obtained by surgery
| Correction loss of rAVR | Correction loss of Cobb angle | Correction loss of AVT | Correction loss of Kyphosis | Correction loss of ATR | |
|---|---|---|---|---|---|
| Chronological age at surgery | |||||
| p | 0.5148 | 0.4355 | 0.4508 | 0.9913 | 0.1817 |
| R | −0.128 | −0.153 | −0.148 | −0.002 | −0.262 |
| Number of fused vertebrae | |||||
| p | 0.6903 | 0.3464 | 0.6461 | 0.6512 | 0.3838 |
| R | 0.078 | 0.185 | 0.09 | 0.089 | 0.171 |
| Proportion of multi-axial screw (%) | |||||
| p | 0.0341* | 0.0666 | 0.4592 | 0.5806 | 0.0041* |
| R | 0.415 | −0.36 | 0.145 | −0.108 | 0.563 |
| Proportion of screw length of 30 mm or shorter | |||||
| p | 0.7823 | 0.2742 | 0.5532 | 0.896 | 0.0776 |
| R | 0.054 | 0.214 | 0.116 | −0.026 | 0.346 |
| Preoperative valuea | |||||
| p | 0.0023* | 0.0069* | 0.244 | 0.0083* | 0.0075* |
| R | 0.597 | 0.530 | −0.228 | 0.518 | 0.525 |
| Postoperative valueb | |||||
| p | 0.0085* | 0.2074 | 0.3365 | 0.1189 | 0.0297* |
| R | 0.516 | 0.247 | −0.188 | −0.306 | 0.426 |
| Amount of correction obtained by surgeryc | |||||
| p | 0.2992 | 0.056 | 0.5568 | 0.0055* | 0.0555 |
| R | 0.204 | 0.375 | −0.115 | 0.545 | 0.376 |
R Spearman’s rank correlation coefficient, p p value
* Significant correlation by Spearman’s rank correlation
aPreoperative value of each parameter in the row
bPostoperative value of each parameter in the row
cAmount of correction obtained by surgery of each parameter in the row
Table 4.
Correction parameters and material of the spinal instrumentations
| Stainless steel construct | Titanium rod construct | p value | |
|---|---|---|---|
| rAVR (°) | |||
| Preoperation | 26.26 ± 4.92 | 30.24 ± 9.83 | 0.229 |
| Postoperation | 14.16 ± 5.11 | 16.93 ± 9.25 | 0.379 |
| Postoperative 2 years | 16.46 ± 1.58 | 19.86 ± 10.07 | 0.315 |
| Correction loss at 2 years | 2.29 ± 0.65 | 2.93 ± 0.99 | 0.018* |
| Cobb angle (°) | |||
| Preoperation | 59.02 ± 10.99 | 59.58 ± 11.21 | 0.899 |
| Postoperation | 15.31 ± 8.10 | 11.47 ± 6.33 | 0.179 |
| Postoperative 2 years | 18.01 ± 9.15 | 13.70 ± 6.39 | 0.161 |
| Correction loss at 2 years | 2.70 ± 1.51 | 2.23 ± 1.29 | 0.356 |
| AVT (mm) | |||
| Preoperation | 58.87 ± 22.87 | 54.96 ± 13.30 | 0.579 |
| Postoperation | 13.97 ± 11.54 | 16.18 ± 7.85 | 0.558 |
| Postoperative 2 years | 15.81 ± 9.86 | 21.44 ± 13.54 | 0.250 |
| Correction loss at 2 years | 1.84 ± 2.46 | 5.25 ± 10.63 | 0.324 |
| Thoracic kyphosis angle (°) | |||
| Preoperation | 23.76 ± 11.24 | 26.09 ± 10.10 | 0.580 |
| Postoperation | 18.49 ± 7.14 | 22.04 ± 9.85 | 0.316 |
| Postoperative 2 years | 19.96 ± 7.47 | 23.81 ± 9.90 | 0.286 |
| Correction loss at 2 years | 1.47 ± 0.67 | 1.77 ± 0.55 | 0.183 |
| ATR (°) | |||
| Preoperation | 20.00 ± 9.37 | 18.88 ± 5.77 | 0.702 |
| Postoperation | 6.36 ± 4.37 | 4.81 ± 3.33 | 0.305 |
| Postoperative 2 years | 8.82 ± 5.67 | 7.44 ± 4.07 | 0.467 |
| Correction loss at 2 years | 2.46 ± 1.44 | 2.63 ± 1.67 | 0.749 |
* Significant difference by a two-way repeated measures ANOVA
Clinical significance
As show in Table 5, no significant correlations were observed between loss of correction and any domains or total scores of SRS-22.
Table 5.
Correlation between correction losses and SRS 22 scores
| Correction loss of AVR | Correction loss of Cobb angle | Correction loss of AVT | Correction loss of Kyphosis | Correction loss of ATR | |
|---|---|---|---|---|---|
| SRS 22 | |||||
| Self-image | |||||
| p | 0.7716 | 0.9126 | 0.5918 | 0.579 | 0.6344 |
| R | 0.057 | 0.022 | −0.105 | −0.109 | −0.093 |
| Function | |||||
| p | 0.4447 | 0.7704 | 0.752 | 0.934 | 0.2043 |
| R | −0.15 | −0.057 | 0.062 | 0.207 | −0.249 |
| Pain | |||||
| p | 0.5039 | 0.7608 | 0.207 | 0.2642 | 0.9568 |
| R | −0.139 | 0.063 | 0.228 | 0.233 | −0.11 |
| Mental health | |||||
| p | 0.9137 | 0.6234 | 0.2027 | 0.1968 | 0.7895 |
| R | 0.023 | −0.102 | 0.266 | 0.269 | 0.056 |
| Total score | |||||
| p | 0.5079 | 0.7121 | 0.4566 | 0.7928 | 0.8299 |
| R | −0.138 | −0.077 | 0.155 | 0.055 | −0.045 |
R Spearman’s rank correlation coefficient, p p value
Discussion
The results of the present study indicated significant correction losses have occurred 2 years after surgery on both the coronal plane (Cobb angle of 2.5°) and the axial plane (rAVR of 2.7°), even though segmental PS constructs were used for the posterior correction and fusion surgeries. Furthermore, significant correction loss of ATR was also observed 2 years after surgery, in correlation with the loss of rAVR. Since the axial plane rotational deformity will cause not only pulmonary dysfunction but also a prominent rib hump [26–30], which leads to patient dissatisfaction, correction of the axial plane deformity as well as the coronal deformity is important.
The methods for measuring vertebral rotation still have been controversial. Majority of the studies evaluating the vertebral rotation had been performed using Nash–Moe [31] or Perdriolle methods [32] in standing X-ray films. However, the measurement on X-rays has disadvantages of difficulty in detecting precise rotational changes and reduced accuracy in large degrees of rotation. Recently, the vertebral rotation has been evaluated on CT images using Aaro–Dahlborn [22] method. The measurements on CT images provide improved accuracy of rotation. However, the angles were influenced by the pelvic position, or rotational motion of unfused spine after surgery. Thus, we used a rAVR to minimize the measurement errors.
In the present study, we divided the patients into two groups, Risser 0–2 and Risser 3–4, to evaluate the relationship between skeletal maturity and the correction loss. We found that the Risser 0–2 group had a greater loss of the Cobb angle, rAVR, and ATR correction compared with the Risser 3–4 group. On the other hand, no significant correlation was observed between the correction losses and chronological age at the time of surgery. Although the Risser sign and chronological age are the most common parameters for the prediction of residual bone growth and curve progression in AIS [33], the chronological age may be an inappropriate parameter for predicting the correction losses. One of the reasons for the correction losses of the rAVR and the Cobb angles in the present study may be the so-called crankshaft phenomenon since the correction losses were significantly correlated to the bone maturity in the present study. The other reason may be plasticity of the growing spine, which helps maintaining a spinal balance. The residual growth potential in immature patients may counteract to the imbalance caused by drastic correction obtained with PS constructs. The result of the present study indicated that the preoperative values of all correction parameters were positively correlated with the correction losses indicating that the larger deformities had larger potential to rebalance the spine. The effect also might have occurred also in the axial plane. As shown in Fig. 1, the pelvic rotation increased after surgery. The increased torsion of the vertebrae below UIV including pelvis occurred possibly to compensate or to rebalance the derotation of the main curve caused by surgical correction 2 years after surgery. The similar phenomenon was reported by Asher et al. [34]. They considered this phenomenon to be compensation caused by extension of the corrective thoracolumbar/lumbar rotational load into the lumbosacral fractional curve below. In this case, the pelvic torsion increased after surgery with the coronal off balance toward the right side. However, at 2 years after surgery, the pelvic torsion has decreased to the normal range with the restoration of the coronal balance.
Significant correlations were also observed between correction losses of AVR and ATR and mechanical weaker fixation methods such as the use of titanium implants and multi-axial screws.
In conclusion, despite the use of segmental PS constructs, which provide rigid three-column fixation of the spine, for posterior correction and fusion surgeries, significant loss of the Cobb angle and AVR angle were observed at 2 years after surgery when compared with the correction soon after surgery. The correction losses, especially regarding AVR, were more evident in the skeletally immature patients, in the patients who had larger deformities, in those treated with more multi-axial screws and with titanium constructs. To prevent the correction losses, especially in skeletal immature patients with lager deformities, use of stainless steel implants and of more mono-axial screws rather than multi-axial screws may be recommended.
Although the impact of correction losses of AVR on SRS 22 scores was negative at 2 years after surgery, a longer follow-up study is warranted to elucidate the clinical significance of the losses of correction in skeletally immature patients.
Conflict of interest
None.
Footnotes
K. Watanabe is also a co-first author.
References
- 1.Cuartas E, Rasouli A, O’Brien M, Shufflebarger HL. Use of all-PS constructs in the treatment of adolescent idiopathic scoliosis. J Am Acad Orthop Surg. 2009;17:550–561. doi: 10.5435/00124635-200909000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Liljenqvist U, Lepsien U, Hackenberg L, Niemeyer T, Halm H. Comparative analysis of PS and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J. 2002;11:336–343. doi: 10.1007/s00586-002-0415-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karatoprak O, Unay K, Tezer M, Ozturk C, Aydogan M, Mirzanli C (2008) Comparative analysis of PS versus hybrid instrumentation in adolescent idiopathic scoliosis surgery. Int Orthop 32:523–528 (discussion 529). doi:10.1007/s00264-007-0359-0 [DOI] [PMC free article] [PubMed]
- 4.Dobbs MB, Lenke LG, Kim YJ, Kamath G, Peelle MW, Bridwell KH. Selective posterior thoracic fusions for adolescent idiopathic scoliosis: comparison of hooks versus PSs. Spine (Phila Pa 1976) 2006;31:2400–2404. doi: 10.1097/01.brs.0000240212.31241.8e. [DOI] [PubMed] [Google Scholar]
- 5.Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K (2004) Comparative analysis of PS versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 29:2040–2048 [DOI] [PubMed]
- 6.Kim YJ, Lenke LG, Kim J, Bridwell KH, Cho SK, Cheh G, Sides B. Comparative analysis of PS versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine(Phila Pa 1976) 2006;31:291–298. doi: 10.1097/01.brs.0000197865.20803.d4. [DOI] [PubMed] [Google Scholar]
- 7.Gotze C, Gotze HG, Halm H. Effect of Harrington instrumentation spondylodesis on scoliotic thoracic deformity. A retrospective 5-year analysis. Z Orthop Ihre Grenzgeb. 1999;137:423–429. doi: 10.1055/s-2008-1037385. [DOI] [PubMed] [Google Scholar]
- 8.Marchesi DG, Transfeldt EE, Bradford DS, Heithoff KB (1992) Changes in vertebral rotation after Harrington and Luque instrumentation for idiopathic scoliosis. Spine (Phila Pa 1976) 17:775–780 [DOI] [PubMed]
- 9.McMaster MJ. Luque rod instrumentation in the treatment of adolescent idiopathic scoliosis. A comparative study with Harrington instrumentation. J Bone Joint Surg Br. 1991;73:982–989. doi: 10.1302/0301-620X.73B6.1955449. [DOI] [PubMed] [Google Scholar]
- 10.Harvey CJ Jr, Betz RR, Clements DH, Huss GK, Clancy M (1993) Are there indications for partial rib resection in patients with adolescent idiopathic scoliosis treated with Cotrel-Dubousset instrumentation? Spine (Phila Pa 1976) 18:1593–1598 [DOI] [PubMed]
- 11.Humke T, Grob D, Scheier H, Siegrist H. Cotrel-Dubousset and Harrington Instrumentation in idiopathic scoliosis: a comparison of long-term results. Eur Spine J. 1995;4:280–283. doi: 10.1007/BF00301034. [DOI] [PubMed] [Google Scholar]
- 12.Willers U, Hedlund R, Aaro S. Mid-term effects of Cotrel-Dubousset instrumentation on the configuration of the spine and the thoracic cage in thoracic idiopathic scoliosis. Eur Spine J. 1993;2:99–103. doi: 10.1007/BF00302711. [DOI] [PubMed] [Google Scholar]
- 13.Willers U, Transfeldt EE, Hedlund R. The segmental effect of Cotrel-Dubousset instrumentation on vertebral rotation, rib hump and the thoracic cage in idiopathic scoliosis. Eur Spine J. 1996;5:387–393. doi: 10.1007/BF00301966. [DOI] [PubMed] [Google Scholar]
- 14.Wood KB, Transfeldt EE, Ogilvie JW, Schendel MJ, Bradford DS (1991) Rotational changes of the vertebral-pelvic axis following Cotrel-Dubousset instrumentation. Spine (Phila Pa 1976) 16:S404–S408 [PubMed]
- 15.Barr SJ, Schuette AM, Emans JB (1997) Lumbar PSs versus hooks. Results in double major curves in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 22:1369–1379 [DOI] [PubMed]
- 16.Lowenstein JE, Matsumoto H, Vitale MG, Weidenbaum M, Gomez JA, Lee FY, Hyman JE, Roye DP., Jr Coronal and sagittal plane correction in adolescent idiopathic scoliosis: a comparison between all PS versus hybrid thoracic hook lumbar screw constructs. Spine (Phila Pa 1976) 2007;32:448–452. doi: 10.1097/01.brs.0000255030.78293.fd. [DOI] [PubMed] [Google Scholar]
- 17.Cheng I, Kim Y, Gupta MC, Bridwell KH, Hurford RK, Lee SS, Theerajunyaporn T, Lenke LG (2005) Apical sublaminar wires versus PSs—which provides better results for surgical correction of adolescent idiopathic scoliosis? Spine (Phila Pa 1976) 30:2104–2112 [DOI] [PubMed]
- 18.Ilharreborde B, Even J, Lefevre Y, Fitoussi F, Presedo A, Pennecot GF, Mazda K. Hybrid constructs for tridimensional correction of the thoracic spine in adolescent idiopathic scoliosis: a comparative analysis of universal clamps versus hooks. Spine (Phila Pa 1976) 2010;35:306–314. doi: 10.1097/BRS.0b013e3181b7c7c4. [DOI] [PubMed] [Google Scholar]
- 19.Asghar J, Samdani AF, Pahys JM, D’Andrea LP, Guille JT, Clements DH, Betz RR. Computed tomography evaluation of rotation correction in adolescent idiopathic scoliosis: a comparison of an all PS construct versus a hook-rod system. Spine (Phila Pa 1976) 2009;34:804–807. doi: 10.1097/BRS.0b013e3181996c1b. [DOI] [PubMed] [Google Scholar]
- 20.Lee SM, Suk SI, Chung ER (2004) Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental PS fixation in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 29:343–349 [DOI] [PubMed]
- 21.Liljenqvist U, Hackenberg L, Link T, Halm H. Pullout strength of PSs versus pedicle and laminar hooks in the thoracic spine. Acta Orthop Belg. 2001;67:157–163. [PubMed] [Google Scholar]
- 22.Aaro S, Dahlborn M (1981) Estimation of vertebral rotation and the spinal and rib cage deformity in scoliosis by computer tomography. Spine (Phila Pa 1976) 6:460–467 [DOI] [PubMed]
- 23.Mizu-Uchi H, Matsuda S, Miura H, Higaki H, Okazaki K, Iwamoto Y. Three-dimensional analysis of computed tomography-based navigation system for total knee arthroplasty: the accuracy of computed tomography-based navigation system. J Arthroplasty. 2009;24:1103–1110. doi: 10.1016/j.arth.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 24.Mizu-uchi H, Matsuda S, Miura H, Higaki H, Okazaki K, Iwamoto Y. The effect of ankle rotation on cutting of the tibia in total knee arthroplasty. J Bone Joint Surg Am. 2006;88:2632–2636. doi: 10.2106/JBJS.E.01288. [DOI] [PubMed] [Google Scholar]
- 25.Watanabe K, Matsumoto M, Tsuji T, Ishii K, Takaishi H, Nakamura M, Toyama Y, Chiba K. Ball tip technique for thoracic PS placement in patients with adolescent idiopathic scoliosis. J Neurosurg Spine. 2010;13:246–252. doi: 10.3171/2010.3.SPINE09497. [DOI] [PubMed] [Google Scholar]
- 26.Takahashi S, Suzuki N, Asazuma T, Kono K, Ono T, Toyama Y. Factors of thoracic cage deformity that affect pulmonary function in adolescent idiopathic thoracic scoliosis. Spine (Phila Pa 1976) 2007;32:106–112. doi: 10.1097/01.brs.0000251005.31255.25. [DOI] [PubMed] [Google Scholar]
- 27.Koumbourlis AC. Scoliosis and the respiratory system. Paediatr Respir Rev. 2006;7:152–160. doi: 10.1016/j.prrv.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 28.Cimic M, Kovac V, Smiljanic I, Kovac I, Cimic A, Smoljanovic T. Relationship between clinical contourometric measurements and vertebral rotation in adolescent idiopathic scoliosis. Coll Antropol. 2009;33(Suppl 2):127–133. [PubMed] [Google Scholar]
- 29.Grivas TB, Vasiliadis ES. Cosmetic outcome after conservative treatment of idiopathic scoliosis with a dynamic derotation brace. Stud Health Technol Inform. 2008;135:387–392. [PubMed] [Google Scholar]
- 30.Soultanis K, Pyrovolou N, Karamitros A, Konstantinou V, Lenti A, Soucacos PN. The use of thoracoplasty in the surgical treatment of idiopathic scoliosis. Stud Health Technol Inform. 2006;123:327–333. [PubMed] [Google Scholar]
- 31.Nash CL, Jr, Moe JH. A study of vertebral rotation. J Bone Joint Surg Am. 1969;51:223–229. [PubMed] [Google Scholar]
- 32.Perdriolle R, Vidal J (1985) Thoracic idiopathic scoliosis curve evolution and prognosis. Spine (Phila Pa 1976) 10:785–791 [DOI] [PubMed]
- 33.Ylikoski M. Growth and progression of adolescent idiopathic scoliosis in girls. J Pediatr Orthop B. 2005;14:320–324. doi: 10.1097/01202412-200509000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Asher MA, Lai SM, Carlson BB, Gum JL, Burton DC (2010) Transverse plane pelvic rotation increase (TPPRI) following rotationally corrective instrumentation of adolescent idiopathic scoliosis double curves. Scoliosis 5:18. doi:10.1186/1748-7161-5-18 [DOI] [PMC free article] [PubMed]