Abstract
Background
A significant amount of research has supported the efficacy of couple versus individual treatment for alcohol use disorders, yet little is known about whether involving a significant other during the course of individual treatment can improve outcomes. Likewise, several barriers to couple treatment exist and a more flexible approach to significant other involvement may be warranted.
Methods
This study constituted secondary analyses of the COMBINE data, a randomized clinical trial that combined pharmacotherapy and behavioral intervention for alcohol dependence. Data were drawn from the 16-week individual combined behavioral intervention (CBI), which had 776 participants, 31% of which were female, and 23% were non-White. The current study examined whether attendance by a supportive significant other (SSO) during CBI sessions would predict better outcomes. It was further hypothesized that active SSO involvement, defined by attendance during drink refusal or communication skills training sessions, would predict better outcomes.
Results
SSOs attended at least one session for 26.9% of clients. Clients with SSOs who attended at least one session had significantly fewer drinking days and fewer drinking related problems at the end of treatment. The presence of an SSO during a drink refusal training session predicted significantly better outcomes, as compared to SSO attendance at other sessions and drink refusal training without an SSO present. SSO attendance at a communication training session did not predict better outcomes.
Conclusions
These results suggest that specific types of active involvement may be important for SSO-involved treatment to have greater efficacy than individual treatment.
Keywords: Alcohol Use Disorders, Cognitive Behavior Therapy, Behavioral Couple Therapy, Conjoint Therapy, COMBINE
Introduction
Studies have shown that social support networks are strongly related to an individual’s alcohol use and treatment outcomes for alcohol use disorders (AUDs). General social support (the extent to which an individual perceives his/her social network as being supportive), alcohol-specific social support (the extent to which an individual’s social network approves or disapproves of drinking), and the drinking behavior of the social network members have each been found to be unique predictors of alcohol treatment outcomes (see Hunter-Reel, McCrady, and Hildebrandt, 2009; McCrady, 2004; Longabaugh, Wirtz, Zywiak, and O’Malley, 2010).
Some treatments have attempted to capitalize on the association between social networks and drinking outcomes. Behavioral couple therapy (BCT) is a treatment for alcohol use disorders (AUDs) with a strong evidence base (see review by O’Farrell and Fals-Stewart, 2003). Several randomized clinical trials have supported the efficacy of couple (i.e., conjoint) treatment in comparison to individual interventions in reducing drinking and drinking consequences and improving relationship satisfaction for individuals with AUDs (Epstein and McCrady, 1998; Powers, Vedel, and Emmelkamp, 2008). While research suggests the relative efficacy of conjoint treatment, individual treatment remains the primary modality for AUDs, and several barriers to conjoint treatment for AUDs have been proposed (McCrady et al., in press). Clinician barriers include clinician lack of training and reluctance to use conjoint interventions, institutional barriers refer to more systemic barriers including reimbursement difficulties and complexity of implementation, and client barriers refer to the willingness and/or ability of clients to engage in conjoint treatments.
Client barriers to engaging in conjoint treatment are significant. McCrady et al. (2009) reported that less than one third of women who were screened and found to be eligible for a study of conjoint versus individual cognitive-behavioral therapy for AUDs chose to enter the study. Of these, nearly half reported partner-related reasons for not engaging. McCrady et al. (in press) reported that women in committed relationships were more likely to select individual over couple treatment, reporting that they preferred to work on individual problems, felt a lack of support from their partners, and had logistical and scheduling issues that prevented engaging in conjoint treatment.
Given the benefits as well as barriers to engaging in conjoint treatment, a more flexible approach may be warranted. Allowing flexibility in number and type of sessions attended by a significant other may increase significant other involvement. Further, allowing flexibility in the type of relationship of the significant other involved in treatment may increase the likelihood of social network member involvement. The present study evaluated whether the attendance of supportive significant others (SSOs) in some sessions in a primarily individual treatment was related to better outcomes. Given that previous research suggests active participation is necessary to increase efficacy of conjoint versus individual treatment, which session the SSO attended was examined. Specifically, whether involvement in sessions that were designated to have active SSO involvement in the treatment manual (drink refusal, communication skills training) would predict better outcomes in a combined pharmacotherapy and behavioral treatment trial was examined.
Materials and Methods
The data are from the COMBINE study (“Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence;” COMBINE Study Research Group, 2003), a multi-site randomized trial examining the effects of combining two types of alcohol medications – naltrexone and acamprosate with medical management (MM) and/or combined behavioral intervention (CBI).
Participants
Details about participant recruitment, inclusion and exclusion criteria can be found in Zweben et al. (2005). Briefly, participants were recruited through advertisements at 11 research sites throughout the country. Potential participants (n=4,965) were screened by telephone and 1,383 individuals were recruited. Exclusion criteria were dependence on substances other than alcohol, nicotine, or cannabis; recent use of opioids or study medications; serious mental illness and medical concerns. Inclusion criteria included alcohol dependence, recent heavy drinking (4 drinks for females and 5 drinks for males), a minimum of 14 drinks (females) or 21 drinks (males) average per week prior to beginning abstinence.
The current study used data from the 776 individuals randomly assigned to the CBI condition. CBI was a cognitive-behavioral treatment that incorporated behavioral skills training and motivation enhancement. SSO involvement was encouraged, as it was thought that involvement of SSO would enhance the benefits of CBI (Miller, 2004). Of those assigned to CBI, 619 (79.8%) also received medication management (MM) and pills (placebo, acamprosate, naltrexone). MM was provided to address safety/compliance issues but offered no skills training or SSO involvement. A total of 157 (20.2%) participants were randomized to receive CBI only.
The sample was 31% female, 76.7% non-Hispanic white, 10.7% Hispanic American, 7.7% African American, 1.5% American Indian or Alaska Native, 1.0% Multiracial, 0.5% Asian American or Pacific Islander, and 1.8% “other races”. The mean age of the subsample was 44 years, 70% had at least 12 years of education, and 43% were married.
Treatment conditions
Participants received treatment for 16 weeks with a maximum of 9 MM visits and 20 CBI sessions. They were followed for 52 weeks post-treatment with on-site assessments (or telephone assessments as needed) at 10, 36, and 52 weeks following treatment. CBI was a multiple phase treatment. In the first phase clinicians used motivational interviewing techniques to build client’s motivation for change. The second phase consisted of functional analysis and developing a treatment plan. In the third phase, CBI was individualized to each client’s needs. Treatment procedures were drawn from a menu of nine skills training modules. The selection of modules was based on the results of the functional analysis and clients’ personal preferences.
An important component of CBI was the active involvement of an SSO. During the first and second sessions of CBI the clinician provided a rationale for involving an SSO in treatment, which was to give the SSO more information about the client’s alcohol use and problems, an opportunity to provide feedback about the treatment plans, and an opportunity to provide ongoing support and motivation to change. The clinician and client examined potential SSO candidates using the Important People Interview (Longabaugh and Zywiak, 2002) and a decision tree (Miller, 2004 page F-44) for selecting a person who was deemed supportive based on support of the client’s sobriety, general supportiveness of the client, the person’s own sobriety, and availability to attend sessions and be readily available for the client. The relationship status of the person(s) selected as the SSO attending the CBI session was not recorded in the COMBINE datasets. Based on the Important People Interview (Longabaugh and Zywiak, 2002) responses among those who had an SSO attend treatment: 45.6% identified a spouse, 17.6% a “significant other,” 13.2% a parent, 7.4% a friend, 6.9% a son/daughter, 5.9% a sibling, and 3.5% a co-worker or other relative as the primary, or “identified,” SSO. Clinicians were expected to invite the “identified” SSO to sessions. However, whether the person identified in the Important People Interview was actually the person who attended the session is unknown. During the initial session with an SSO the clinician oriented the SSO to his/her role in the treatment, obtained commitment to support change efforts, and discussed ways to enhance the SSOs skill in providing support.
Only 26.9% of CBI clients (n=214) had an SSO attend at least one session. The average number of sessions attended by an SSO was 2.78 (SD=2.64), with a maximum of 14 (n=1). Of these clients, an SSO attended one session for 51.7% of clients (n =101), two or three sessions for 21.7% of clients (n=45), four or five sessions for 13.1% of clients (n =27), and six or more sessions for 13.5% of clients (n=28).
Of particular interest in the current study was whether “active” SSO participation improved treatment outcomes. Two of the CBI skills training modules, the Drink Refusal and Social Pressures (DREF) module and Communication Training (COMM) module, included explicit instructions on how to actively involve the SSO. Other modules did not describe ways to actively involve an SSO. Thus, we operationalized “active involvement” as an SSO being in attendance for a session that included the DREF or COMM module.
The DREF module incorporated several components, including a description of the rationale that many clients resume drinking in response to social pressure, assessment of the direct and indirect social pressures experienced by the client, assessment of the coping responses most commonly used by the client in response to social pressure, and behavioral rehearsal of positive coping behaviors that can be used in social pressure situations. If an SSO was included in a DREF session then the manual suggests that the client practice drink refusal skills during the session with the SSO providing “highly realistic social pressure” (pg. 165; Miller, 2004).
The COMM module was geared toward helping clients become more aware of effective communication skills. The module covered general communication skills, including clear communication, attending, and how to avoid communication roadblocks. If the SSO was attending treatment then the manual provided specific guidance on incorporating the SSO to “strengthen communication with the client’s primary relationship” (pg. 137; Miller, 2004) as part of the COMM module.
We hypothesized that attendance during a session that included DREF or COMM would involve the SSO by helping the client to practice drinking refusal and improve communication. Thirty-nine percent (n =302) of the CBI sample received the DREF module and 10% (n=30) of these received the module with an SSO present. Only 16% of the CBI sample (n=123) received the COMM module and 31% (n=38) of these received the module with an SSO present.
Measures
A complete list of all assessments can be found in the previous COMBINE publication (COMBINE study Research Group, 2003).
In the current study, the Drinker Inventory of Consequences (DrInC; (Miller et al., 1995) assessed consequences experienced as a result of drinking. Clients reported on a 4-point scale the frequency of 45 drinking consequences. The average internal consistency of DrInC in this sample was adequate (Cronbach α=0.93). The current report includes analyses of DrInC data collected at baseline through one-year post-treatment.
The Form-90 interview (Miller and Del Boca, 1994), was used to gather drinking data in standard drinks over a 90-day interval using a calendar method, and the drinking outcome variables were derived from the Form-90. Numerous studies have found Form-90 to be highly reliable (Tonigan et al., 1997) and correlated with collateral interviews (Maisto, Sobell, and Sobell, 1982). Drinking data was biologically verified (Anton and Youngblood, 2006). Drinking frequency was calculated as the percentage of drinking days (PDD) (the inverse of percentage of days abstinent, one of the primary outcomes in the COMBINE study; Anton et al., 2006). Time elapsed between baseline and the first heavy drinking day (THDD; defined as five or more drinks for men, four or more drinks for women) during or following treatment, percent drinking days (PDD), drinking-related consequences (DrInC), percent heavy drinking days (PHDD), and drinks per drinking day (DDD) were examined as outcome variables.
The Important People Interview (IPI; Longabaugh and Zywiak, 2002) is an interview to identify important people in the individual’s life, and for each identified person the IPI measures frequency of contact, level of importance and supportiveness, drinking and drug use, reactions to the client’s drinking/drug use, and the person’s feelings about the client’s treatment. Given recent findings that network supportiveness, as measured by the IPI, predicted drinking outcomes in the COMBINE trial (Longabaugh et al., 2010), variables from the IPI were included as covariates.
Data Analytic Plan
To examine the association between SSO attendance at CBI sessions and drinking outcomes we estimated a series of models using Mplus version 6.1 (Muthén and Muthén, 2010). First, unconditional latent growth curve models of drinking outcomes were estimated separately for each outcome (PDD, DrInC, PHDD, and DDD) without covariates using a systematic process of model testing whereby intercept-only models were compared to increasingly complex functional forms (e.g., linear slope, linear+quadratic slope, nonlinear slope). For the PDD, PHDD, and DDD outcomes the final model for all three outcomes (modeled separately) was a piecewise model with the intercept centered at the end of treatment, one linear slope for the 16 weeks during treatment, and linear and quadratic slopes for outcomes at the end of treatment to 10, 36, and 52 weeks following treatment. This model provided the best fit to the observed data based on the Root Mean Square Error of Approximation (RMSEA; Browne and Cudeck, 1993) value less than 0.08 and the Comparative Fit Index (CFI; Bentler, 1990) greater than 0.95. The final model for drinking consequences included DrInC scores measured mid-treatment, at the end of treatment and 10, 36, and 52 weeks following treatment. The intercept was centered at the end of treatment assessment and both a linear and quadratic slope of drinking consequences over time were estimated.
To examine the association between SSO attendance at CBI sessions and the time to the first heavy drinking day during or following treatment we estimated a continuous time survival model (Cox, 1972) where the hazard probability for a given day (t) is estimated by the proportion of individuals who did not have a heavy drinking day prior to t, who drank heavily on day t. The hazard probabilities were regressed on the covariates described below, where the logit hazard probabilities varied as a linear function of the covariates. For both the latent growth curve and survival models, whether an SSO ever attended a session (yes or no) was incorporated as a predictor of outcomes and any variables that predicted SSO attendance were included as covariates. Finally, we examined outcomes for individuals who had an SSO attend either a DREF or COMM session, as compared to (1) individuals who received the DREF or COMM without an SSO present, and (2) SSO attendance at other sessions that did not include DREF or COMM.
All parameters were estimated using a weighted maximum likelihood function and all standard errors were computed using a sandwich estimator, which adjusts the standard errors for differences across research sites. Maximum likelihood provides the estimated variance-covariance matrix for the available data and therefore all available data were included in the models (Schafer and Graham, 2002).
Results
Descriptive statistics for the main outcomes are provided in Table 1. Preliminary analyses were conducted to determine baseline differences between those who did and did not have SSOs attend a session on demographic measures and numerous baseline measures (e.g., dependence severity, social network). There were several differences between those who did or did not have an SSO attend a session on income (t (625)= −2.19, p=0.03), treatment attendance (t (767)=−7.09, p < 0.001), number of network members who oppose drinking (t (570)= −2.38, p=0.02), and marital status (χ2(1)=10.28, p=0.001), with SSO attendance associated with higher income, more treatment attendance, more network members who oppose drinking, and being married. All measures that were significantly different between SSO attendance groups and baseline measures of drinking outcomes were included in all subsequent analyses. In addition, COMBINE study treatment conditions (naltrexone, acamprosate, and placebo equivalents) were included as covariates.
Table 1.
Descriptive Statistics (Means (Standard Deviations) for Supportive Significant Other (SSO) Attendance at CBI Sessions
| Measure | Total sample | SSO did not attend session | SSO attended session | d | |||
|---|---|---|---|---|---|---|---|
| N | Mean (SD) | N | Mean (SD) | N | Mean (SD) | ||
| PDD baseline | 776 | 75.29 (25.63) | 569 | 75.94 (25.23) | 207 | 73.49 (26.59) | .09 |
| PDD mid-treatment | 740 | 26.71 (32.36) | 533 | 27.91 (32.23) | 207 | 22.22 (30.40) | .18* |
| PDD end of treatment | 725 | 26.01 (33.08) | 518 | 27.58 (33.73) | 207 | 20.75 (29.74) | .21* |
| PDD 10 weeks posttreatment | 719 | 31.39 (34.57) | 515 | 32.92 (34.49) | 204 | 26.39 (33.56) | .19* |
| PDD 52 weeks posttreatment | 653 | 37.61 (37.83) | 456 | 39.07 (37.24) | 197 | 33.86 (38.68) | .14 |
| DrInC baseline | 774 | 46.89 (20.05) | 567 | 46.09 (20.22) | 207 | 49.17 (19.41) | .16 |
| DrInC mid-treatment | 608 | 12.90 (18.51) | 424 | 14.02 (19.43) | 184 | 10.41 (16.02) | .20* |
| DrInC end of treatment | 583 | 13.53 (18.93) | 408 | 13.09 (18.74) | 175 | 14.26 (19.09) | .06 |
| DrInC 10 weeks posttreatment | 605 | 17.49 (21.30) | 422 | 17.99 (21.32) | 183 | 16.11 (21.04) | .09 |
| DrInC 52 weeks posttreatment | 542 | 20.01 (21.90) | 377 | 20.69 (22.24) | 165 | 18.05 (20.85) | .12 |
Note. d=Cohen’s d measure of effect size;
p < 0.05, differences between SSO attendance subgroups based on independent samples t-test; PDD = percent drinking days; DrInC=Drinker Inventory of Consequences scores; SSO = supportive significant other.
Drinking Outcomes
The growth model of PDD regressed on SSO attendance and the covariates provided a reasonable fit to the data (χ2 (39)=119.20, p < 0.001; CFI=0.98; RMSEA=0.06 (90% CI: 0.05 –0.07). As seen in Table 2, the end of treatment PDD intercept was significantly associated with SSO attendance, such that clients whose SSO attended at least one session were drinking less frequently by the end of treatment. Likewise, the SSO’s level of attendance (i.e., the number of sessions attended by an SSO) also predicted the end of treatment PDD intercept, such that SSO attendance at more sessions was associated with less frequent drinking (lower PDD) at the end of treatment.
Table 2.
Summary of Significant Effects on the Intercept of Drinking Outcomes (i.e., End of Treatment Drinking Levels).
| Predictor | Outcome | β | B (SE) |
|---|---|---|---|
| SSO attendance | PDD | −0.09 | −0.66 (0.33)* |
| DrInC | −0.12 | −3.98 (1.51)** | |
|
| |||
| Number of sessions attended by SSO | PDD | −0.08 | −0.14 (0.05)** |
| DrInC | −0.11 | −0.85 (0.18)** | |
|
| |||
| SSO attendance at drink refusal session vs. not receiving drink refusal session | PDD | 0.43 | 2.84 (0.43)** |
| PHDD | 0.31 | 1.83 (0.34)** | |
| DrInC | 0.37 | 11.33 (1.99)** | |
|
| |||
| SSO attendance at drink refusal session vs. no SSO attendance at drink refusal session | PDD | 0.21 | 1.39 (0.50)** |
| PHDD | 0.12 | 0.69 (0.31)* | |
| DrInC | 0.17 | 5.22 (2.00)** | |
| SSO attendance at communication session vs. not receiving communication session | PDD | 0.11 | 1.29 (0.55)* |
Note.
p < 0.05,
p < 0.01;
β = standardized regression coefficient; B (SE) = unstandardized regression coefficient (standard error); PDD = percent drinking days; DrInC=Drinker Inventory of Consequences scores; SSO = supportive significant other.
The model of drinking consequences also provided an adequate fit to the data (χ2 (22)=56.60, p < 0.001; CFI=0.95; RMSEA=0.053 (90% CI: 0.04 – 0.07). Consistent with the drinking frequency models, SSO attendance at a session was associated with a lower level of DrInC scores at the end of treatment (see Table 2). The number of sessions attended by an SSO were also significantly associated with lower DrInC scores at the end of treatment (see Table 2). The growth models of PHDD and DDD also provided an adequate fit to the data based on CFI > 0.95 and RMSEA < 0.06, however SSO attendance (any attendance and the number of sessions attended by an SSO) was not significantly associated with PHDD or DDD.
In the continuous time survival models SSO attendance at sessions did not predict the time to the first heavy drinking day (hazard odds=1.008, p=0.46).
Drink Refusal and/or Communication Training
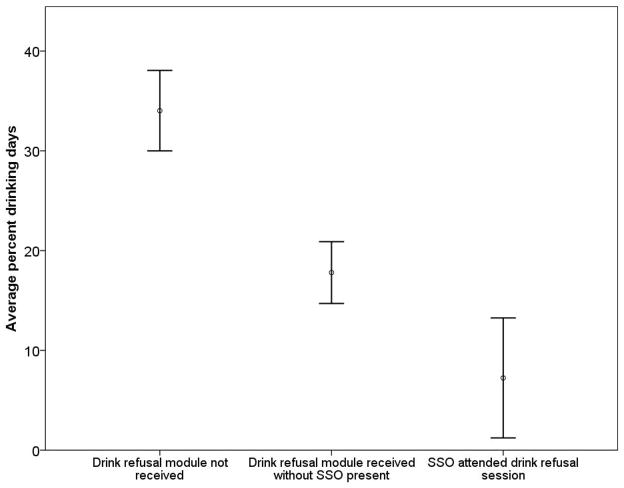
The latent growth and survival models were re-estimated with dummy coded variables that captured SSO attendance at a session that included either drink refusal skills (DREF) or communication skills (COMM) training. For the PDD and PHDD outcomes SSO attendance at a drink refusal training session was significantly associated with lower PDD and PHDD at the end of treatment, as compared to individuals who did not receive the DREF module and compared to individuals who received the DREF module without their SSO present (see Table 2). As seen in Figure 1, individuals who received the DREF module drank significantly less frequently at the end of treatment and individuals who received a DREF session with an SSO present at the session drank significantly less frequently than those who received a DREF session without an SSO present. Likewise, survival analyses indicated that the time to the first heavy drinking day was predicted from SSO attendance at a DREF session (p < 0.001). The average amount of time to first heavy drinking day among individuals who had an SSO attend at least one drink DREF session was 98 days (SD=87 days), whereas the average for those who did not have an SSO attend a DREF session was 66 days (SD=102 days) and the average for those who never received DREF was 41 days (SD=68 days). Thus, receiving a DREF session with an SSO present during the training session delayed the first heavy drinking day by nearly two months (average 57 days difference).
Figure 1.
Average percent drinking days (percentage of days in which a person drank during the last 30 days) in the last month of treatment (week 16) by drink refusal module and SSO attendance. Error bars represent 95% confidence interval.
The DrInC growth model also indicated that SSO attendance at a DREF session was significantly associated with fewer drinking consequences at the end of treatment, as compared to individuals who did not receive the DREF module and compared to individuals who received the DREF module without their SSO present (see Table 2). Thirty-eight percent of individuals who received the DREF module with an SSO present during the DREF session reported zero drinking consequences at the end of treatment and fewer drinking consequences on average (Mean (SD)=9.17 (14.00), range=0 to 53, model estimated mean = 11.68), as compared to those who did not receive the DREF module (Mean (SD)=15.87 (20.99), range=0 to 95, model estimated mean = 17.28) and those who received the DREF module without their SSO present (Mean (SD)=9.77 (14.87), range 0 to 74, model estimated mean = 16.33). SSO attendance at a DREF session did not predict changes in DDD.
SSO attendance at a COMM session was significantly associated with lower PDD at the end of treatment as compared to individuals who did not receive the COMM module (see Table 2). However, there were no differences among those individuals who received the COMM module with or without their SSO present, thus SSO attendance during a COMM module session did not result in improved outcomes within and following treatment. The growth models of DrInC, PHDD, and DDD did not significantly differ across the contrasts that involved SSO attendance at a COMM session.
The survival analyses indicated that receiving the COMM session with an SSO present did not significantly delay the amount of time to the first heavy drinking day.
Discussion
The current study evaluated whether SSO attendance at individual sessions during a behavioral intervention for alcohol dependence predicted drinking outcomes following treatment. Results from growth models indicated that clients who had an SSO attend at least one treatment session drank less frequently and had fewer drinking consequences at the end of treatment, as compared to those clients who did not have an SSO attend treatment. Results also indicated that SSO attendance at a session focused on drink refusal skills predicted significantly lower drinking frequency, less frequent heavy drinking, fewer drinking related consequences, and a longer amount of time until the first heavy drinking day, as compared to treatment sessions that were not attended by an SSO. SSO attendance at a session that focused on communication skills did not have an appreciable effect on drinking outcomes. The attendance of an SSO at treatment sessions was unrelated to the slope of drinking outcomes during or following treatment, suggesting that SSO attendance might predict better overall level of drinking by the end of treatment, but not the rate of change in drinking outcomes (during or following treatment) or continued improvement in outcomes over time. It is unclear why the effects of SSO attendance observed at the end of treatment did not predict continued changes in drinking or maintenance of the differences in drinking following treatment. Given mean differences in outcomes were in the same direction over time, but were not significant, could indicate a lack of power. Indeed a post-hoc power analysis of effect sizes reported in Table 1 indicated we had power < .40 to detect significant differences in outcomes at 52 weeks following treatment.
It is of note that only about a quarter of the sample had an SSO attend CBI session(s). One reason for this was that while SSO involvement was encouraged, it was not required. One of the authors (AZ) chaired the behavioral intervention committee of the COMBINE Study and provided oversight in CBI implementation. In monitoring the CBI approach, he discovered that a sizable proportion of CBI therapists were not successful in involving SSOs in the treatment sessions. Many were unfamiliar with working with families or significant others and consequently were reluctant to add additional complexity to CBI by attempting to deal with issues or concerns raised by clients about involving their SSOs in the treatment sessions.. Finally, no concerted efforts were made by researchers to increase SSO attendance by monitoring the sessions. As such, extensive SSO involvement was primarily restricted to those sites at which either the researchers or study clinicians were familiar with SSO involvement in behavioral interventions, although all sites reported at least some participation by SSOs (ranging from 11.5% to 41.4% participation).
To our knowledge, this is the first study to examine the role of SSO involvement in individual treatment for AUDs. SSO involvement in sessions that focused on drink refusal skills, but not the communications skills, suggests that active SSO involvement might not be sufficient for SSO-involved treatment to have greater efficacy than individual treatment (as suggested by Fals-Stewart, Birchler, and Kelley, 2006). Rather the type of active involvement might be an important predictor of treatment success. It could be the case that rehearsing the action of refusing an SSOs offer to drink in the presence of a clinician is a powerful intervention, even delivered in one session. It could also be that communication skills training is a much more complicated endeavor and a single session in effective communication is not sufficient to produce change.
Limitations
There are several limitations to the current study. First, the small sample sizes within each subgroup (30 clients and SSOs received the DREF module and 38 clients and SSOs received the COMM module) could limit the generalizability of these findings. Although it is important to note that the observed power for comparisons between the 30 clients and SSOs who received the DREF module and those who did not receive the DREF module was greater than .90 for all significant outcomes. Second, we had no control over the availability of specific session data and study participants and their SSOs could choose whether and when to attend treatment sessions. As such, random assignment was not used to assign others to attend particular sessions, and therefore differences in outcomes are potentially attributable to variable(s) unknown to the researchers. Likewise, the relationship status of the SSOs that attended treatment was not available, thus it is impossible to determine whether the effects observed in the current study are stronger or weaker for specific relationship types (e.g., spouse vs. non-married partner). It is interesting to note that baseline motivation was not associated with whether an SSO attended sessions; however it is impossible to determine whether improvements in motivation during the first few weeks of treatment influenced whether clients brought an SSO to treatment and such an increase in motivation could also explain the better outcomes observed among those who had an SSO attend a session.
Another limitation is our definition of “active involvement” as the SSO being in attendance for DREF or COMM session. We chose this definition because the CBI manual explicitly described ways in which the significant other could be actively involved in these sessions, however no data were available on whether the SSO actually engaged in drink refusal skills rehearsal or communication training. Furthermore, even though SSO involvement was described in the DREF and COMM training sections of the manual does not necessary mean that the active ingredients of an SSO attending treatment occurred during these modules. The SSO could have provided general support for abstinence in the earlier sessions, which had a carryover effect in these skill building sessions. Further we have no behavioral data on whether individuals who received the DREF or COMM modules were more likely to use those skills. Finally, the effect sizes of the differences in drinking outcomes for individuals whose SSOs attended a treatment sessions, while significant, were small in magnitude and SSO attendance was only associated with two drinking outcomes: percent drinking days and drinking-related consequences.
Future directions
There are several important future directions. Future research on the blending of individual and conjoint treatment, such as that developed and described by McCrady and colleagues (Hunter-Reel, McCrady, Hildebrandt, and Epstein, 2010) and Fals-Stewart, Birchler, and Kelley (2006) is an important area of inquiry. Studies designed from the outset to assess the involvement of SSOs in some, but not all, sessions would help discern whether timing or dose of SSO involvement is important. It will be of particular importance to actively train, supervise and monitor clinician’s skill and comfort of engaging with SSOs.
In the current study active involvement of an SSO during a drink refusal skills session within a behavioral intervention was shown to predict better drinking outcomes. However, the influence of SSO involvement on medication adherence was not examined, and may be an important area of future inquiry. Additionally, SSOs were not actively involved in medication management sessions and it is important to examine whether active involvement of an SSO other in medication management sessions increases medication adherence and may improve outcomes.
Such future studies should also examine whether specific behaviors on the part of the SSO, both during and outside of sessions, may be predictive of outcomes. Further, assigning SSOs to have varying degrees of involvement within sessions, attendance at varying numbers of sessions, or attendance at varying types of sessions (early sessions, skills-related sessions) may provide more information about the specific mechanisms of SSO involvement that predict better drinking outcomes. Finally, it would be interesting to examine the nature of the relationship between the client and the identified SSO to determine whether specific relationships (e.g., spouse or romantic partner) might be more predictive of outcomes than other relationships (e.g., coworkers or friends). Such work may help us design treatments that maximize the benefit of involving SSOs while minimizing the costs and barriers.
Acknowledgments
This research was supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (R21AA017137). The authors thank members of the COMBINE Study Research Group for their assistance in facilitating access to COMBINE study data.
Contributor Information
Dorian Hunter-Reel, Rutgers University.
Katie Witkiewitz, Washington State University.
Allen Zweben, Columbia University.
References
- Anton RF, O’Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, Gastriend DR, Hosking JD, Johnson BA, LoCastro JS, Longabaugh R, Mason BJ, Mattson ME, Miller WR, Pettinati HM, Randall CL, Swift R, Weiss RD, Williams LD, Zweben A. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295:2003–2017. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- Anton RF, Youngblood M. Factors affecting %CDT status at entry into a multisite clinical treatment trial: Experience from the COMBINE Study. Alcohol Clin Exp Res. 2006;30:1878–1883. doi: 10.1111/j.1530-0277.2006.00225.x. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychol Bul. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage; Beverly Hills, CA: 1993. pp. 136–162. [Google Scholar]
- COMBINE Study Research Group. Testing combined pharmacotherapies and behavioral interventions for alcohol dependence (the COMBINE study): A pilot feasibility study. Alcohol Clin Exp Res. 2003;27:1123–1131. doi: 10.1097/01.ALC.0000078020.92938.0B. [DOI] [PubMed] [Google Scholar]
- Epstein EE, McCrady BS. Behavioral couples treatment of alcohol and drug use disorders: Current status and innovations. Clin Psychol Rev. 1998;18:689–711. doi: 10.1016/s0272-7358(98)00025-7. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, Birchler GR, Kelley ML. Learning Sobriety Together: A randomized clinical trial examining Behavioral Couples Therapy with alcoholic female patients. J Consult Clin Psychol. 2006;74:579–591. doi: 10.1037/0022-006X.74.3.579. [DOI] [PubMed] [Google Scholar]
- Hunter-Reel D, McCrady BS, Hildebrandt T. Emphasizing interpersonal factors: An interpersonal extension of an intra-individual model of relapse. Addiction. 2009;104:1281–1290. doi: 10.1111/j.1360-0443.2009.02611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter-Reel D, McCrady BS, Hildebrandt T, Epstein EE. Indirect effect of social support for drinking on drinking outcomes: The role of motivation. J Stud Alcohol. 2010;71:930–937. doi: 10.15288/jsad.2010.71.930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longabaugh R, Wirtz PW, Zywiak WH, O’Malley SS. Network support as a prognostic indicator of drinking outcomes: The COMBINE Study. J Stud Alcohol Drugs. 2010;71:837–846. doi: 10.15288/jsad.2010.71.837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longabaugh R, Zywiak WH. Adapted for the use of Project COMBINE. Center for Alcohol and Addiction Studies, Brown University; Providence, R.I: 2002. Project COMBINE: A Manual for the Administration of the Important People Instrument. [Google Scholar]
- Maisto SA, Sobell MB, Sobell LC. Reliability of self-reports of low ethanol consumption by problem drinkers over 18 months of follow-up. Drug Alcohol Depend. 1982;9:273–278. doi: 10.1016/0376-8716(82)90066-7. [DOI] [PubMed] [Google Scholar]
- McCrady BS. To have but one true friend: Implications for practice of research on alcohol use disorders and social networks. Psychol Addictive Beh. 2004;18:113–121. doi: 10.1037/0893-164X.18.2.113. [DOI] [PubMed] [Google Scholar]
- McCrady BS, Epstein EE, Cook S, Jensen NK, Hildebrandt T. A randomized trial of individual and couple behavioral alcohol treatment for women. J Consult Clin Psychol. 2009;77:243–256. doi: 10.1037/a0014686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrady BS, Epstein EE, Cook S, Jensen NK, Ladd BO. What do women want? Alcohol treatment choices, treatment entry and retention. Psychol Addictive Beh. doi: 10.1037/a0024037. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR. Combined Behavioral Intervention manual: A clinical research guide for therapists treating people with alcohol abuse and dependence. In: Miller WR, editor. COMBINE Monograph Series. Vol. 1. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2004. p. F-44. [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. J Stud Alcohol Sup. 1994;12:112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. Project MATCH Monograph Series. Vol. 4. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1995. The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse Test Manual. [Google Scholar]
- Muthén LK, Muthén BO. Mplus users guide. 6. Muthén & Muthén; Los Angeles, CA: 2010. [Google Scholar]
- O’Farrell TJ, Fals- Stewart W. Alcohol abuse. J Marital Family Ther. 2003;29:121–146. doi: 10.1111/j.1752-0606.2003.tb00387.x. [DOI] [PubMed] [Google Scholar]
- Powers MB, Vedel E, Emmelkamp PMG. Behavioral couples therapy (BCT) for alcohol and drug use disorders: A meta-analysis. Clin Psychol Rev. 2008;28:952–962. doi: 10.1016/j.cpr.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychol Meth. 2002;7:147–177. [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol consumption measures. In: Allen P, Columbus M, editors. Assessing alcohol problems: A guide for clinicians and researchers. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 1995. [Google Scholar]
- Sobell LC, Sobell MB. Timeline Followback: A calendar method for assessing alcohol and drug use (Users Guide) Addiction Research Foundation; Toronto: 1996. [Google Scholar]
- Tonigan JS, Miller WR, Brown JM. The reliability of Form 90: An instrument for assessing alcohol treatment outcome. J Stud Alcohol. 1997;58:358–364. doi: 10.15288/jsa.1997.58.358. [DOI] [PubMed] [Google Scholar]
- Zweben A, Barrett D, Berger L, Murray KT. Recruiting and retaining participants in a combined behavioral and pharmacological trial. J Stud Alcohol Supp. 2005;15:72–81. doi: 10.15288/jsas.2005.s15.72. [DOI] [PubMed] [Google Scholar]