Abstract
The aim of this paper is to consider the relative benefits of screening for type two diabetes mellitus in women with a previous pregnancy complicated by gestational diabetes mellitus. Recent studies suggest that women who experience GDM are at a greater risk of developing type 2 diabetes within 10–20 years of their index pregnancy. If considered as a stand-alone indicator of the risk of developing type 2 diabetes, GDM is a poor diagnostic test. Most women do not develop GDM during pregnancy and of those that do most do not develop type 2 diabetes. There is, however, a clear need for better early detection of predisposition to disease and/or disease onset to significantly impact on this global pandemic. The putative benefits of multivariate approaches and first trimester and preconception screening to increase the sensitivity of risk assignment modalities for type 2 diabetes are proposed.
1. Introduction
The keystone to improving disease management and health outcomes remains the early and accurate diagnosis of the predisposition to, or onset of, disease. Early detection of disease risk and onset is the first step in implementing efficacious treatment and improving patient outcomes. In the context of screening for prediabetic and diabetic conditions in asymptomatic individuals, early detection may allow the implementation of dietary, lifestyle, and/or pharmacologic interventions that limit or prevent the development of disease-specific pathophysiologies. The rationale for seeking to develop predictive tests for diabetes and other metabolic disorders, thus, is clearly evident.
Recent studies suggest that women who experience gestational diabetes mellitus (GDM) are at a greater risk of developing type 2 diabetes mellitus (type 2 diabetes) within 10–20 years of their index pregnancy [1]. Monitoring glycemic control and intervention strategies to delay or prevent disease onset have been advocated in such women. Type 2 diabetes, however, is a disease of heterogeneous aetiology and GDM is but one risk factor. If considered as a stand-alone indicator of the risk of developing type 2 diabetes, GDM is a poor diagnostic test. Most women do not develop GDM during pregnancy and of those that do most do not develop type 2 diabetes. Postpartum monitoring of women who developed GDM during pregnancy, nevertheless, may be of clinical utility in this higher risk cohort. There is, however, a clear need for better early detection of predisposition to disease and/or disease onset to significantly impact on this global pandemic.
For women (and their partners), pregnancy represents a period of increased interaction with the healthcare system and a period where changes in lifestyle may have significant impact not only on the parents but also on the disease susceptibility of the next generation. This period represents an opportunity to implement more comprehensive educational, lifestyle, and disease susceptibility or onset screening initiatives, either during first trimester or, perhaps more effectively, in the setting of a preconception clinic. The objectives of preconception care are to promote the health of women (and their partners) before conception and thereby improve pregnancy-related outcomes (both current and future) and to reduce the risk of adult-onset disease (e.g., cardiovascular and metabolic) in their children. Over the next decade, the combined effects of an increase in the incidence of type 2 diabetes in younger women [2] and an increased maternal age at first delivery will result in an increased number of pregnancies exposed to the potentially adverse effects of undiagnosed diabetic conditions. Globally, the number of live births each year is estimated to be more than 134 million. Preconception programs, thus, have the potential to specifically target more than 360 million individuals per year (i.e., the parents and the offspring).
The aim of this paper is to consider the relative benefits of screening for type 2 diabetes in women with a previous pregnancy complicated by GDM. The putative benefits of multivariate approaches and preconception screening to increase the sensitivity of risk assignment modalities for type 2 diabetes are proposed.
2. Diabetes Mellitus
2.1. Epidemiology
Diabetes mellitus is one of the most common chronic diseases. The number of adults with diabetes has more than doubled over the past 30 years. Recent reports by Danaei et al. [3] and Shaw et al. [4] estimate the global prevalence of diabetes to be between 285 and 347 million people. By 2030, diabetes is expected to affect 552 million people. The prevalence of this disease is increasing in most countries as changing lifestyles lead to reduced physical activity and increased obesity [4]. Since 1980, the age-standardised fasting plasma glucose concentration has increased by 0.07 mmol/L per decade for men and 0.09 mmol/L per decade for women [3]. These data are consistent with an overall population-based decline in glycemic control.
The incidence of diabetes has also increased dramatically in women of reproductive age (i.e., 18–44 years). For example, in the USA, the rate of diabetes has increased by 70% in women aged 30–39 years over the past decade. It is estimated that 12.6 million women (or 10.8% of women over the age of 20) have diabetes, and of these women, 90–95% have type 2 diabetes. Death rates for women aged 25–44 years with diabetes are more than 3 times that for women without diabetes [5].
2.2. Aetiology of Type 2 Diabetes
The available data are consistent with type 2 diabetes being of genetic origin; however, its precise aetiology remains to be unequivocally established. Behavioural, lifestyle, and environmental factors have all been implicated as modifiers of disease risk. Recent genome-wide screening studies have identified multiple susceptibility variants consistent with type 2 diabetes being of polygenic origin [6–10]. Thus, type 2 diabetes may be a phenotypic manifestation of many different aetiologies that simply share hyperglycemia as a common outcome [11].
A hallmark of the onset of type 2 diabetes is a progressive decrease in insulin-stimulated glucose uptake. High circulating concentrations of glucose induce pancreatic β-cell hypertrophy and/or hyperplasia and increased secretion of insulin. When the capacity of β-cells fails to compensate for the degree of insulin resistance, insulin deficiency and ultimately type 2 diabetes ensue [12]. Pancreatic β-cell failure displays specificity for insulin signaling pathway; while retaining capacity to respond to challenges (such as, β-adrenergic agonists, amino acids, and sulfonylurea drugs), cells lose their capacity to respond to glucose. If not adequately managed, hyperglycaemia may induce a glucotoxicity and lipotoxicity involving oxidative and endoplasmic reticulum stress, overexpression of proinflammatory autacoids, and increased rates of β-cell apoptosis [12, 13].
It is becoming increasingly evident that inflammation plays a key role in the pathogenesis of type 2 diabetes. It is well established that systemic markers of inflammation, including C-reactive protein, haemoglobin, serum amyloid A, proinflammatory cytokines and chemokines are elevated in the blood of type 2 diabetics. The source of these mediators is of multiorgan origin and, at least in part, in response to elevated concentrations of glucose and fatty acids. Both secretagogues promote proinflammatory conditions in many tissues (including pancreatic isLet-7 cells, adipose tissue, liver, and muscle), induce the release of inflammatory autacoids, and alter redox status. Chemokines further promote the recruitment of macrophages to affected tissues and together with T-cell and possibly mast cells may establish a local chronic inflammation that involves the constitutive activation of gene transcription factors such as the nuclear factor κB (NF-κB) family.
NF-κB is a sequence-specific family of transcription factors critically involved in inflammation and innate immune responses. The NF-κB family comprises at least five proteins, of which the most abundant form in unstimulated cells occurs in the cytoplasm as a heterodimer composed of two proteins, p50 and p65 bound to an inhibitory subunit, IκBα. Upon stimulation, IκBα is phosphorylated by an IκB kinase complex, thus, targeting IκBα for ubiquitin-dependent degradation and liberates NF-κB dimers to translocate to the nucleus where they bind to the consensus sequence 5-GGGPuNNPyPyCC-3. This κB motif has been identified in the promoter regions of many proinflammatory mediators, including adhesion molecules (ICAM-1), enzymes (including, inducible nitric oxide synthase, phospholipase A2s, cyclo-oxygenase-2, urokinase plasminogen activator, metalloproteinases, superoxide dismutase), cytokines (e.g., IL-1β, IL-6, TNFα), and chemokines (IL-8) [14].
It is noteworthy that recent studies in breast cancer [15] provide data implicating NF-κB, IL-6, and Let-7 micro-RNA (miRNA) in an epigenetic switch or positive feedback loop that resets inflammatory pathways to a heightened state of responsiveness. In this model, a triggering event induces NF-κB DNA binding activity and Lin28 expression and represses Let-7 miRNA action. One of the actions of Let-7 is to suppress IL6 formation. Thus, inhibition of Let-7 results in higher levels of expression of IL6 than achieved by NF-κB activation alone. IL6 activation of the STAT3 transcription factor is necessary for neoplastic cellular transformation, and IL6 activates NF-κB, thereby completing a positive feedback loop.
We propose that a similar mechanism may induce a sustained inflammatory response, activation of NF-κB-regulated genes, and insulin resistance in type 2 and gestational diabetes. That is, that a primary pathophysiological insult (Figure 1, e.g., obesity, metabolic stress, hyperglycaemia, or hyperlipidaemia) may activate NF-κB-mediated gene expression and proinflammatory regulatory pathways. Subsequent secondary or repetitive insults may induce a persistent, heightened response, the positive feedback loop being established via the induction of the RNA-binding protein Lin28 that suppresses Let-7 microRNA family members. Let-7 miRNA suppresses interleukin-6 expression (binding IL-6 mRNA though its 3′ UTR) and other growth and metabolic mediators. The resulting positive feedback loop between NF-κB and, in particular, IL-6 and the inhibitory effects of Lin 28 and IL-6 on Let-7 is sufficient to result in sustained elevation and responsiveness of these pathways.
Figure 1.

Diabetes-related triggers may initiate a positive feedback loop resulting in heighten responsiveness of the NF-κB by the inhibition of miRNA repressors by NF-κB-induced RNA binding proteins.
In support of this hypothesis, Zhu et al. [16] recently reported that the Lin28/Let-7 axis plays a role in the reprograming of glucose metabolism in malignancy. Lin28a and Lin28b were reported to promote insulin-sensitivity and resistance to high-fat-diet-induced diabetes. Furthermore, muscle-specific inhibition of Lin28a or overexpression of Let-7 results in insulin resistance and impaired glucose tolerance. These effects were mediated, in part, via Let-7 repression of the insulin-PI3K-mTOR pathway, including the insulin receptor, insulin receptor substrate 2, and insulin-like growth factor 1 receptor. In normal adult individuals, Lin28 expression is low and, thus, Let-7 represses the expression of a cassette of gene pathways associated with growth, cell migration, and catabolic metabolism. Under conditions where Lin28 is induced (e.g., via activation of NF-κB response pathways), Let-7 repression of these genes is removed. In the case of type 2 diabetes, triggers such as obesity, oxidative stress, and inflammatory mediators may initiate aberrant activation of the NF-κB pathway and initiate a feedback loop that sustains and progressively increases insulin resistance.
2.3. Management and Intervention
The available data support the contention that the adverse sequelae of diabetes (including microvascular, cardiovascular, and renal disease) can be, at least, ameliorated by adequate glycaemic control [17]. Recent trials have established the benefits of interventions to prevent or delay diabetes and reduce diabetes-related complications and/or associated risk factors [18–21]. Intensive lifestyle modification to promote weight loss and increase physical activity resulted in a 58% reduction in the risk of type 2 diabetes in adults with impaired glucose tolerance [21]. Early diagnosis of predisposition to type 2 diabetes and implementation of effective intervention represent a strategy to abate the incidence of type 2 diabetes and its associated health care burden.
3. Gestational Diabetes Mellitus
3.1. Epidemiology
GDM is glucose intolerance with onset or first recognition during pregnancy [22]. GDM affects ~5% of all pregnancies and its incidence is increasing in parallel with the global increase in obesity and type 2 diabetes. In the USA, GDM affects 135, 000 pregnancies per year. GDM has been associated with not only acute increased risk for complications of pregnancy but also long-term disease risks for both mother and baby (Australian Institute of Health and Welfare, 2010). Perinatal morbidity includes hyperinsulinaemia, macrosomia, hypoglynaemia, hyperbilirubinaemia, and respiratory distress syndrome which in turn may generate subsequent complications. Longer-term morbidity for the offspring includes obesity and diabetes independent of genetic factors [23–26]. GDM in the mother is associated with increased risk of overt diabetes later in life. A higher risk of developing metabolic and cardiovascular disease has been reported for women who develop GDM during pregnancy.
In 2011, the American Diabetes Association (ADA) and the International Association of Diabetes and Pregnancy Study Groups (IADPSG) revised recommendations regarding GDM. It is now recommended that patients at increased risk for type 2 diabetes be screened for diabetes using standard diagnostic criteria at their first prenatal visit. High-risk women are defined as having impaired fasting plasma glucose levels of 5.6 mmol/L to 6.9 mmol/L [100 mg/dL to 125 mg/dL]) or impaired glucose tolerance (2-hour OGTT values of 7.8 mmol/L to 11.0 mmol/L [140 mg/dL to 199 mg/dL]). Women with an HbA1c of 5.7% to 6.4% are also considered at increased risk. In these patients, confirmed fasting glucose levels of ≥7.0 mmol/L (126 mg/dL) or random glucose levels ≥11.1 mmol/L (200 mg/dL) are also diagnostic of diabetes. The ADA and the IADPSG recommended that such high-risk women with diabetes diagnosed on the basis of standard diagnostic criteria receive a diagnosis of overt rather than gestational diabetes.
At 24 to 28 weeks of gestation, all women not known to have diabetes (including high-risk women if the initial testing was normal) should undergo a 75 g OGTT, with diagnosis of GDM based upon the finding of 1 abnormality, rather than the previously recommended 2.
3.2. Aetiology
Normal pregnancy is attended by significant changes in maternal metabolism [27] that are induced, at least in part, by the release of placenta-derived autacoids [28–30]. Early pregnancy is anabolic and associated with the accretion of maternal fat. Late pregnancy is catabolic and characterised by increasing insulin resistance, lipolysis, hyperinsulinaemia, hyperglycaemia, increased postprandial fatty acid concentrations, and declining maternal fat reserves. The net effect of these late gestation changes are increased availability of energy and anabolic substrates to sustain the growth of the feto-placental unit, increased utilisation of glycolytic energy production, and increased free fatty acid availability [31]. Late pregnancy is also associated with a decreased ability to produce glucose via gluconeogenesis, glycogenolysis and lipolysis. This is in part a consequence of an attenuation of hypoglycaemia to induce glucagon, norepinephrine and cortisol.
It has been suggested that GDM and type 2 diabetes may share common pathogenic mechanisms, however, pregnancy may serve to unmask disease in those women who are predisposed and destined to develop type 2 diabetes later in life. Similar to type 2 diabetes, GDM is manifested by the inability of pancreatic β-cell insulin release to compensate for pregnancy-induced insulin resistance resulting in maternal hyperglycaemia and hyperinsulinaemia. Moderate hyperinsulinaemia is considered adaptive during normal pregnancy and a response to increased energy utilisation and demand by the developing fetus. In GDM, the adaptive changes in insulin resistance extend beyond those normally observed [32, 33]. For example, during normal pregnancy, insulin-stimulated glucose transport by skeletal muscle fibers is reduced by ~40%. In women with GDM, glucose transport has been reported to be reduced by up to 65% [34]. Environmental (modifiable) risk factors, including, preconception conditioning, maternal diet and exercise, and other lifestyle factors, may impact on the severity of its manifestation. In most cases, however, symptoms of metabolic dysfunction disappear postpartum following the withdrawal of placental autacoid mediators.
The effects of hyperglycaemia on pregnancy outcome are underpinned by experimental studies that identify putative effector pathways by which exposure to high glucose concentrations may alter placental and maternal adipose tissue phenotype and responsiveness [35–37]. Similar to type 2 diabetes, the role of inflammatory mechanisms in disease progression is evident. Increased biomarkers of oxygen radical damage and an impairment of antioxidant defense have been identified in individuals with type 2 diabetes [38] and in women with GDM [37, 39–41]. Previously, we demonstrated that the placentae of women with GDM display a reduced capacity to respond to oxidative stress in terms of 8-isoprostane and tumour necrosis factor α (TNF α) release [35]. We concluded that GDM placenta may be preconditioned by transient intracellular oxidative stress. The role of oxidative stress in the aetiology of GDM has recently been reviewed [42].
4. Screening for Diabetes
4.1. Screening for GDM
Currently, GDM is diagnosed in the late second or early third trimester of pregnancy. Any pathology is probably already established by this time and reversal of the potential adverse perinatal outcomes may be limited. The lack of a reliable early test for GDM has hampered the development of useful intervention therapies that may impact not only on the acute but long-term health outcomes (Figure 2). Thus, there is a need to diagnose and predict GDM earlier so that appropriate management can be initiated and tailored to the needs of the patient in order to minimise perinatal complications and their sequelae.
Figure 2.
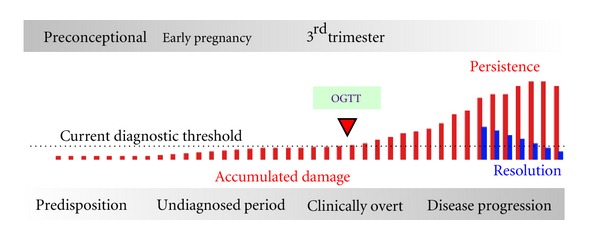
GDM disease progression. GDM is currently diagnosed (Clinically Overt) in 3rd trimester (24–28 weeks of gestation) following an oral glucose tolerance test (OGTT). Using this diagnostic threshold, there is no opportunity to prevent pathological changes (accumulated damage) that may occur during 1st and 2nd trimester (Undiagnosed Period). The implementation of screening tests during early pregnancy or the preconception period affords opportunity to identify women at risk of disease and to evaluate intervention strategies on pregnancy outcome and the long-term health of both mother and baby.
GDM is currently diagnosed by an In Vitro Diagnostic (IVD) Oral Glucose Tolerance Test performed at 24–28 weeks of gestation. A glucose load (75 g) is administered to fasting individuals, and blood glucose concentration is determined at 1 hour and 2 hours [43, 44]. The Third International Workshop-Conference on GDM emphasised the critical importance of developing new diagnostic criteria that are based on the potential to detect pregnancies at risk for adverse perinatal outcome as a result of maternal hyperglycaemia, rather than placing primary emphasis on the identification of mothers at risk for progression to diabetes outside of pregnancy. With the obesity epidemic well entrenched in the Western world and with more women delaying pregnancy and the associated increase in pre-pregnancy body mass index (BMI), the incidence of GDM is increasing irrespective of the diagnostic criteria used.
First trimester pregnancy and preconceptional risk-factors for GDM have been identified including family history of GDM and/or diabetes [45], maternal pregnancy weight gain [46, 47], fasting plasma glucose [48], 1-hour glucose challenge test [49], oral glucose tolerance test [50], and haemoglobin A1c [51] adiponectin [52, 53], C-reactive protein [54], serum triglycerides [55], sex hormone-binding globulin [56], placental growth factor [57] leptin [58], oxidised DNA [59], and follistatin-like-3 levels [60]. Although some have been able to provide a good negative predictive measure for subsequent GDM [61], most tests suffer from poor positive predictive values and are of limited efficacy.
It is now widely acknowledged that single biomarkers are unlikely to deliver significant incremental gain in sensitivity and specificity that will be required for the development of effective screening and classification tests requisite for the implementation of personalised medicine. New approaches based upon the measurement of multiple biomarkers of disease risk afford opportunity to increase diagnostic test sensitivity and specificity. Even the use of two biomarkers can deliver improved performance [62]. The use of modelling algorithms to combine multiple known biomarkers (e.g., candidate-based approaches) similarly may increase diagnostic efficiency and deliver classification models of clinical utility [63–66]. Both candidate-based applications (i.e., in which the identity of the analytes being measured are well-established [67]) and signature profiling applications (i.e., in which characteristic patterns or motifs within a signal profile are identified, see [68]) may be utilised in the development of multivariate modelling strategies for the delivery of more informative diagnostic tests [69].
A recent trend in the development of more efficient diagnostic tests has been the use of algorithm-based multivariate index assays (IVDMIAs). With the development of this new class of IVD, the discipline has sought new biostatistical approaches for assessing and quantifying incremental gains in diagnostic efficiency. Traditionally, the area under the receiver operator characteristic curve (AUC) has been used as a measure and comparator of diagnostic efficiency. Several investigators have argued that this measure alone may be imperfect and inefficient for comparing the true clinical usefulness of alternative marker panels [70, 71]. These authors reviewed several biomarker studies and observed that when evaluating improvement in risk assignment of biomarkers, very large odds ratios were often associated with very small increases in the AUC. This feature of the receiver operator characteristic curve analysis limits its utility in identifying putative beneficial contributions of new biomarkers to algorithm-based models. Pencina et al. [72] therefore, proposed the use of two new methods for evaluating the diagnostic efficiency of biomarkers. These two methods are (i) Net Reclassification Improvement (NRI) and (ii) Integrated Discrimination Improvement (IDI). The NRI is based on counts of the number of true positives showing an increase in probability of an event and the number of true negatives showing a decrease in probability of an event. The IDI is based on the integral of sensitivity and specificity of all possible thresholds. These new biostatistical approaches may facilitate the development of biomarker panels with improved diagnostic efficiency and aid in the screening and earlier detection of diabetic conditions.
IVDMIA approaches are being developed for risk assignment modalities for use in the first trimester of pregnancy, including the evaluation of multiple candidate-based profiling of blood-borne biomarkers. For example, we measured multiple plasma biomarkers at 11 weeks of gestation in women who subsequently experienced a normal pregnancy outcome and women who subsequently developed gestational diabetes [73]. Of the biomarkers considered, algorithms that included adiponectin, insulin, and random blood glucose delivered the greatest diagnostic efficiency when compared to individual biomarkers alone. The IVDMIA increased AUC by more than 10%. This simple example demonstrates the putative benefit of a multimarker approach for improving diagnostic efficiency.
4.2. Screening for Type 2 Diabetes after GDM
As discussed above, GDM may unmask a predisposition to type 2 diabetes and, as such, GDM may be diagnostic for type 2 diabetes. A recent meta-analysis [74] reviewed 20 studies conducted between 1960–2009 to estimate the relative risk of developing type 2 diabetes following GDM. The combined cohort involved more than 675,000 pregnancies of which 31,867 cases of GDM were identified (i.e., 4.7% of all pregnancies included in the analysis). Of these cases of GDM, 10,859 incident cases of type 2 diabetes were identified. The relative risk for type 2 diabetes following GDM was estimated to be 7.43 (compared to women who had normoglycaemic pregnancies). Bellamy et al. [74] suggested that increased awareness of the risk of type 2 diabetes after GDM could provide an opportunity to test and use dietary, lifestyle, and pharmacological interventions that might prevent or delay the onset of type 2 diabetes.
While the conclusion that GDM is a risk factor for type 2 diabetes is supported by the available data, it is pertinent to note that more than 95% of women in the cohort did not develop gestational diabetes and that more that 64% of women who have had GDM do not have type 2 diabetes 20 years postindex pregnancy. The prevalence of type 2 diabetes in women 10–20 years after index pregnancy is estimated to be ~5%; thus, in a cohort of 675,000, ~33,700 incidence cases would be expected, that is, 22,841 cases in this cohort were not associated with a previous GDM pregnancy (i.e., a false positive rate of 0.659). The positive predictive value of GDM as a diagnostic test for type 2 diabetes is only 34% (sensitivity = 0.322 and specificity of 0.967).
Similarly, Göbl et al. [75] recently reported results of a small prospective cohort (n = 110) with 10-year followup of women who experienced GDM in which 78.7% of women did not develop type 2 diabetes. Of the 21.3% who did progress to type 2 diabetes, a multivariate analysis identified 2-hour oral GTT concentration, HDL cholesterol, and age as the best predictors. Women with two or more risk factors were at a higher risk than women with only one.
It has further been proposed that women with a previous GDM pregnancy should be followed up by OGTT postpartum and, if positive, intervention and monitoring strategies implemented. While this may be appropriate, it does not assist the ~68% of women who develop type 2 diabetes in the absence of GDM complicated pregnancies. Specifically targeting and monitoring women with a previous GDM pregnancy is an aid in identifying predisposition to type 2 diabetes but is a poor stand-alone diagnostic test for type 2 diabetes in women. Alternative strategies for early detection screening, intervention, and prevention are requisite to reducing the overall burden of type 2 diabetes at a community level.
The objectives of any disease screening program are to
identify asymptomatic individuals at higher risk of, or predisposition to disease,
afford the opportunity for treatment or prevention of disease thus limiting severity,
reduce disease burden in the community.
A number of opportunities for developing screening applications that target women of reproductive age exist, including the development of preconception screening.
4.3. Preconception Conditioning and Screening
The concept that information defining contemporary environmental conditions is coded in maternal physiology and is sensed and informs and adapts the development of the fetus is not novel [76, 77]. This tenet is the basis of epigenetics and the developmental origins of adult disease [78]. Modifiable maternal and environmental factors reported to affect pregnancy outcome and/or disease risk in the offspring include BMI [79, 80], weight gain during pregnancy [47], diet [81–83] physical activity [84, 85], preexisting diabetes [86, 87], and alcohol consumption [88]. The placenta functions as an environmental sensor for the embryo and not only integrates information encoded within the maternal milieu but its own ontogenic development and function may be altered by such information. Known modifiers of the placental epigenome in human and animal models include micronutrients [89, 90], diet [91], smoking [92], bacterial infection [93], obesity [94], stress [95], diabetes [96], and hypertension [97, 98].
Based upon the available data, a sound case can be made for the implementation and evaluation of preconception care programs that attempt to optimise or, at least, improve general health, life style, and conditioning of women and their partners before conception. The premise underpinning promoting preconception in addition to prenatal care is that for some maternal conditions and exposures, altered programing and/or damage can occur before prenatal care begins. To promote normal placentation and reduce risks of complications of pregnancy, education and appropriate interventions must be identified and implemented prior to conception.
In 2006, the Centers for Disease Control and Prevention (CDC) published a report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care [99, 100]. The panel identified four primary objectives:
improve knowledge, attitudes, and behaviors of men and women related to preconception health,
assure that all women of childbearing age receive preconception care services that will enable them to enter pregnancy in optimal health,
reduce risks identified by a previous poor pregnancy outcome through interventions during the interconception period, which can prevent or minimize health problems for a mother and her future children,
reduce disparities in adverse pregnancy outcomes.
The actual benefits of preconception care programs remain to be established as there is a paucity of randomised control data on the health outcomes and economic benefit of attempts to improve preconception maternal (and paternal) health. Several studies, however, have reported some evidence of positive financial returns for preconception counseling for women with diabetes, based on savings in hospitalisation costs [101, 102]. Similarly, case control studies on the health care costs associated with maternal obesity provide further support, reporting that the cost of prenatal care was 5 times higher in mothers who were overweight before pregnancy than in normal-weight control women [103]. More recently, Moos and Bennett [104] reviewed the evidence supporting preconception care for diabetic women.
The implementation of preconception care programs afford opportunity for more broadly based screening for prediabetic conditions and early intervention to reduce the incidence of type 2 diabetes. The efficacy of screening this cohort has yet to be established it would, however, afford opportunity for longitudinal monitoring of biomarkers. Longitudinal monitoring is an approach that has proved effective in increasing the diagnostic performance of oncology diagnostics [105, 106]. It is likely that such an approach would also improve the positive predictive value for the diagnosis of type 2 diabetes.
5. Conclusion
Type 2 diabetes is a “communicable disease” that is transmitted between individuals and intergenerationally by the adoption of societal and lifestyle behaviors—behaviours that challenge fundamental energy homeostasis. The juxtaposition of a susceptible genetic background with the ability to access a surfeit of energy dense foods without counterpoise energy expenditure predisposes to obesity and failure of glycaemic control. Modifiable risk factors have been identified that may reduce disease severity. Early identification of individuals at higher risk of developing type 2 diabetes will play a critical role in improving disease management and health outcomes. Of significant promise is the development and implementation of high performance IVDMIAs and their use in longitudinal monitoring programs.
Abbreviation
- IVDMIA:
In Vitro Diagnostic Multivariate Index Assay.
References
- 1.Lee AJ, Hiscock RJ, Wein P, Walker SP, Permezel M. Gestational diabetes mellitus: clinical predictors and long-term risk of developing type 2 Diabetes—a retrospective cohort study using survival analysis. Diabetes Care. 2007;30(4):878–883. doi: 10.2337/dc06-1816. [DOI] [PubMed] [Google Scholar]
- 2.Lawrence JM, Contreras R, Chen WS, Sacks DA. Trends in the prevalence of preexisting diabetes and gestational diabetes mellitus among a racially/ethnically diverse population of pregnant women, 1999–2005. Diabetes Care. 2008;31(5):899–904. doi: 10.2337/dc07-2345. [DOI] [PubMed] [Google Scholar]
- 3.Danaei G, Finucane MM, Lu Y, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants. The Lancet. 2011;378(9785):31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 4.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Research and Clinical Practice. 2010;87(1):4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Control CfD. Diabetes and Women's Health Across the Life Stages: A Public Health Perspective, 2002.
- 6.Saxena R, Voight BF, Lyssenko V, et al. Genome-wide association analysis identifies loci for type 2 diabetes and triglyceride levels. Science. 2007;316(5829):1331–1336. doi: 10.1126/science.1142358. [DOI] [PubMed] [Google Scholar]
- 7.Dupuis J, Langenberg C, Prokopenko I, et al. New genetic loci implicated in fasting glucose homeostasis and their impact on type 2 diabetes risk. Nature Genetics. 2010;42(2):105–116. doi: 10.1038/ng.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scott LJ, Mohlke KL, Bonnycastle LL, et al. A genome-wide association study of type 2 diabetes in finns detects multiple susceptibility variants. Science. 2007;316(5829):1341–1345. doi: 10.1126/science.1142382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sladek R, Rocheleau G, Rung J, et al. A genome-wide association study identifies novel risk loci for type 2 diabetes. Nature. 2007;445(7130):881–885. doi: 10.1038/nature05616. [DOI] [PubMed] [Google Scholar]
- 10.Zeggini E, Weedon MN, Lindgren CM, et al. Replication of genome-wide association signals in UK samples reveals risk loci for type 2 diabetes. Science. 2007;316(5829):1336–1341. doi: 10.1126/science.1142364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robertson RP. β-cell deterioration during diabetes: what’s in the gun? Trends in Endocrinology and Metabolism. 2009;20(8):388–393. doi: 10.1016/j.tem.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donath MY, Shoelson SE. Type 2 diabetes as an inflammatory disease. Nature Reviews Immunology. 2011;11(2):98–107. doi: 10.1038/nri2925. [DOI] [PubMed] [Google Scholar]
- 13.Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC. β-cell deficit and increased β-cell apoptosis in humans with type 2 diabetes. Diabetes. 2003;52(1):102–110. doi: 10.2337/diabetes.52.1.102. [DOI] [PubMed] [Google Scholar]
- 14.Ghosh AK. Factors involved in the regulation of type I collagen gene expression: implication in fibrosis. Experimental Biology and Medicine. 2002;227(5):301–314. doi: 10.1177/153537020222700502. [DOI] [PubMed] [Google Scholar]
- 15.Iliopoulos D, Hirsch HA, Struhl K. An epigenetic switch involving NF-κB, Lin28, Let-7 MicroRNA, and IL6 links inflammation to cell transformation. Cell. 2009;139(4):693–706. doi: 10.1016/j.cell.2009.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhu H, Shyh-Chang N, Segre AV, et al. The Lin28/let-7 axis regulates glucose metabolism. Cell. 2011;147(1):81–94. doi: 10.1016/j.cell.2011.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weber MB, Twombly JG, Narayan KMV, Phillips LS. Lifestyle interventions and the prevention and treatment of type 2 diabetes. American Journal of Lifestyle Medicine. 2010;4:468–480. [Google Scholar]
- 18.Holman R, Paul S, Bethel M, Matthews D, Neil H. 10-year follow-up of intensive glucose control in type 2 diabetes. The New England Journal of Medicine. 2008;359(15):1577–1589. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 19.Saito T, Watanabe M, Nishida J, et al. Lifestyle modification and prevention of type 2 diabetes in overweight Japanese with impaired fasting glucose levels: a randomized controlled trial. Archives of Internal Medicine. 2011;171(15):1352–1360. doi: 10.1001/archinternmed.2011.275. [DOI] [PubMed] [Google Scholar]
- 20.Ratner RE, Christophi CA, Metzger BE, et al. Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. Journal of Clinical Endocrinology and Metabolism. 2008;93(12):4774–4779. doi: 10.1210/jc.2008-0772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England Journal of Medicine. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beischer NA, Oats JN, Henry OA, Sheedy MT, Walstab JE. Incidence and severity of gestational diabetes mellitus according to country of birth in women living in Australia. Diabetes. 1991;40(supplement 2):35–38. doi: 10.2337/diab.40.2.s35. [DOI] [PubMed] [Google Scholar]
- 23.Van Assche FA, Aerts L, Holemans K. Maternal diabetes and the effect for the offspring. Verhandelingen. 1992;54(2):95–107. [PubMed] [Google Scholar]
- 24.Van Assche FA, Aerts L, Holemans K. Metabolic alterations in adulthood after intrauterine development in mothers with mild diabetes. Diabetes. 1991;40(2):106–108. doi: 10.2337/diab.40.2.s106. [DOI] [PubMed] [Google Scholar]
- 25.Van Assche FA, Aerts L, Holemans K. The effects of maternal diabetes on the offspring. Bailliere’s Clinical Obstetrics and Gynaecology. 1991;5(2):485–492. doi: 10.1016/s0950-3552(05)80108-7. [DOI] [PubMed] [Google Scholar]
- 26.Van Assche FA, Holemans K, Aerts L. Long-term consequences for offspring of diabetes during pregnancy. British Medical Bulletin. 2001;60:173–182. doi: 10.1093/bmb/60.1.173. [DOI] [PubMed] [Google Scholar]
- 27.Di Cianni G, Miccoli R, Volpe L, Lencioni C, Del Prato S. Intermediate metabolism in normal pregnancy and in gestational diabetes. Diabetes/Metabolism Research and Reviews. 2003;19(4):259–270. doi: 10.1002/dmrr.390. [DOI] [PubMed] [Google Scholar]
- 28.Longo L. Maternal blood volume and cardiac output during pregnancy: a hypothesis of endocrinologic control. The American Journal of Physiology. 1983;245(5):R720–729. doi: 10.1152/ajpregu.1983.245.5.R720. [DOI] [PubMed] [Google Scholar]
- 29.Kirwan JP, Hauguel-de Mouzon S, Lepercq J, et al. TNF-α is a predictor of insulin resistance in human pregnancy. Diabetes. 2002;51(7):2207–2213. doi: 10.2337/diabetes.51.7.2207. [DOI] [PubMed] [Google Scholar]
- 30.Samaan N, Yen SCC, Gonzalez D, Pearson OH. Metabolic effects of placental lactogen (HPL) in man. Journal of Clinical Endocrinology and Metabolism. 1968;28(4):485–491. doi: 10.1210/jcem-28-4-485. [DOI] [PubMed] [Google Scholar]
- 31.Herrera E. Metabolic adaptations in pregnancy and their implications for the availability of substrates to the fetus. European Journal of Clinical Nutrition. 2000;54(supplement 1):S47–S51. doi: 10.1038/sj.ejcn.1600984. [DOI] [PubMed] [Google Scholar]
- 32.Retnakaran R, Qi Y, Connelly PW, Sermer M, Hanley AJ, Zinman B. Risk of early progression to prediabetes or diabetes in women with recent gestational dysglycaemia but normal glucose tolerance at 3-month postpartum. Clinical Endocrinology. 2010;73(4):476–483. doi: 10.1111/j.1365-2265.2010.03834.x. [DOI] [PubMed] [Google Scholar]
- 33.Retnakaran R, Qi Y, Connelly PW, Sermer M, Zinman B, Hanley AJG. Glucose intolerance in pregnancy and postpartum risk of metabolic syndrome in young women. Journal of Clinical Endocrinology and Metabolism. 2010;95(2):670–677. doi: 10.1210/jc.2009-1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Friedman JE, Ishizuka T, Shao JH, Huston L, Highman T, Catalano P. Impaired glucose transport and insulin receptor tyrosine phosphorylation in skeletal muscle from obese women with gestational diabetes. Diabetes. 1999;48(9):1807–1814. doi: 10.2337/diabetes.48.9.1807. [DOI] [PubMed] [Google Scholar]
- 35.Coughlan MT, Permezel M, Georgiou HM, Rice GE. Repression of oxidant-induced nuclear factor-κB activity mediates placental cytokine responses in gestational diabetes. Journal of Clinical Endocrinology and Metabolism. 2004;89(7):3585–3594. doi: 10.1210/jc.2003-031953. [DOI] [PubMed] [Google Scholar]
- 36.Coughlan MT, Oliva K, Georgiou HM, Permezel JM, Rice GE. Glucose-induced release of tumour necrosis factor-alpha from human placental and adipose tissues in gestational diabetes mellitus. Diabetic Medicine. 2001;18(11):921–927. doi: 10.1046/j.1464-5491.2001.00614.x. [DOI] [PubMed] [Google Scholar]
- 37.Coughlan MT, Vervaart PP, Permezel M, Georgiou HM, Rice GE. Altered placental oxidative stress status in gestational diabetes mellitus. Placenta. 2004;25(1):78–84. doi: 10.1016/S0143-4004(03)00183-8. [DOI] [PubMed] [Google Scholar]
- 38.West IC. Radicals and oxidative stress in diabetes. Diabetic Medicine. 2000;17(3):171–180. doi: 10.1046/j.1464-5491.2000.00259.x. [DOI] [PubMed] [Google Scholar]
- 39.Kinalski M, Śledziewski A, Telejko B, et al. Lipid peroxidation, antioxidant defence and acid-base status in cord blood at birth: the influence of diabetes. Hormone and Metabolic Research. 2001;33(4):227–231. doi: 10.1055/s-2001-14953. [DOI] [PubMed] [Google Scholar]
- 40.Biri A, Onan A, Devrim E, Babacan F, Kavutcu M, Durak I. Oxidant status in maternal and cord plasma and placental tissue in gestational diabetes. Placenta. 2006;27(2-3):327–332. doi: 10.1016/j.placenta.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 41.Lappas M, Permezel M, Rice GE. Release of proinflammatory cytokines and 8-isoprostane from placenta, adipose tissue, and skeletal muscle from normal pregnant women and women with gestational diabetes mellitus. The Journal of Clinical Endocrinology and Metabolism. 2004;89(11):5627–5633. doi: 10.1210/jc.2003-032097. [DOI] [PubMed] [Google Scholar]
- 42.Lappas M, Hiden U, Desoye G, et al. The role of oxidative stress in the pathophysiology of gestational diabetes mellitus. Antioxidants & Redox Signaling. 2011;15(12):3061–3100. doi: 10.1089/ars.2010.3765. [DOI] [PubMed] [Google Scholar]
- 43.Coustan DR, Lowe LP, Metzger BE. The hyperglycemia and adverse pregnancy outcome (HAPO) study: can we use the results as a basis for change? Journal of Maternal-Fetal and Neonatal Medicine. 2010;23(3):204–209. doi: 10.3109/14767050903550667. [DOI] [PubMed] [Google Scholar]
- 44.Metzger BE, Persson B, Lowe LP, et al. Hyperglycemia and adverse pregnancy outcome study: neonatal glycemia. Pediatrics. 2010;126(6):E1545–E1552. doi: 10.1542/peds.2009-2257. [DOI] [PubMed] [Google Scholar]
- 45.Caliskan E, Kayikcioglu F, Ozturk N, Koc S, Haberal A. A population-based risk factor scoring will decrease unnecessary testing for the diagnosis of gestational diabetes mellitus. Acta Obstetricia et Gynecologica Scandinavica. 2004;83(6):524–530. doi: 10.1111/j.0001-6349.2004.00389.x. [DOI] [PubMed] [Google Scholar]
- 46.Riskin-Mashiah S, Damti A, Younes G, Auslander R. Pregestational body mass index, weight gain during pregnancy and maternal hyperglycemia. Gynecological Endocrinology. 2011;27(7):464–467. doi: 10.3109/09513590.2010.495436. [DOI] [PubMed] [Google Scholar]
- 47.Morisset AS, Tchernof A, Dubé MC, Veillette J, Weisnagel SJ, Robitaille J. Weight gain measures in women with gestational diabetes mellitus. Journal of Women’s Health. 2011;20(3):375–380. doi: 10.1089/jwh.2010.2252. [DOI] [PubMed] [Google Scholar]
- 48.Sacks DA, Chen W, Wolde-Tsadik G, Buchanan TA. Fasting plasma glucose test at the first prenatal visit as a screen for gestational diabetes. Obstetrics and Gynecology. 2003;101(6):1197–1203. doi: 10.1016/s0029-7844(03)00049-8. [DOI] [PubMed] [Google Scholar]
- 49.Maegawa Y, Sugiyama T, Kusaka H, Mitao M, Toyoda N. Screening tests for gestational diabetes in Japan in the 1st and 2nd trimester of pregnancy. Diabetes Research and Clinical Practice. 2003;62(1):47–53. doi: 10.1016/s0168-8227(03)00146-3. [DOI] [PubMed] [Google Scholar]
- 50.Bhattacharya SM. Fasting or two-hour postprandial plasma glucose levels in early months of pregnancy as screening tools for gestational diabetes mellitus developing in later months of pregnancy. Journal of Obstetrics and Gynaecology Research. 2004;30(4):333–336. doi: 10.1111/j.1447-0756.2004.00205.x. [DOI] [PubMed] [Google Scholar]
- 51.Cypryk K, Czupryniak L, Wilczynski J, Lewinski A. Diabetes screening after gestational diabetes mellitus: poor performance of fasting plasma glucose. Acta Diabetol. 2004;41(1):5–8. doi: 10.1007/s00592-004-0136-0. [DOI] [PubMed] [Google Scholar]
- 52.Retnakaran R, Hanley AJG, Raif N, Connelly PW, Sermer M, Zinman B. Hypoadiponectinaemia in South Asian women during pregnancy: evidence of ethnic variation in adiponectin concentration. Diabetic Medicine. 2004;21(4):388–392. doi: 10.1111/j.1464-5491.2004.1151.x. [DOI] [PubMed] [Google Scholar]
- 53.Williams MA, Qiu C, Muy-Rivera M, Vadachkoria S, Song T, Luthy DA. Plasma adiponectin concentrations in early pregnancy and subsequent risk of gestational diabetes mellitus. Journal of Clinical Endocrinology and Metabolism. 2004;89(5):2306–2311. doi: 10.1210/jc.2003-031201. [DOI] [PubMed] [Google Scholar]
- 54.Wolf M, Sandler L, Hsu K, Vossen-Smirnakis K, Ecker JL, Thadhani R. First-trimester C-reactive protein and subsequent gestational diabetes. Diabetes Care. 2003;26(3):819–824. doi: 10.2337/diacare.26.3.819. [DOI] [PubMed] [Google Scholar]
- 55.Nolan CJ, Riley SF, Sheedy MT, Walstab JE, Bescher NA. Maternal serum triglyceride, glucose tolerance, and neonatal birth weight ratio in pregnancy: a study within a racially heterogeneous population. Diabetes Care. 1995;18(12):1550–1556. doi: 10.2337/diacare.18.12.1550. [DOI] [PubMed] [Google Scholar]
- 56.Thadhani R, Wolf M, Hsu-Blatman K, Sandler L, Nathan D, Ecker JL. First-trimester sex hormone binding globulin and subsequent gestational diabetes mellitus. American Journal of Obstetrics and Gynecology. 2003;189(1):171–176. doi: 10.1067/mob.2003.343. [DOI] [PubMed] [Google Scholar]
- 57.Ong CYT, Lao TT, Spencer K, Nicolaides KH. Maternal serum level of placental growth factor in diabetic pregnancies. Journal of Reproductive Medicine for the Obstetrician and Gynecologist. 2004;49(6):477–480. [PubMed] [Google Scholar]
- 58.Qiu CF, Williams MA, Vadachkoria S, Frederick IO, Luthy DA. Increased maternal plasma leptin in early pregnancy and risk of gestational diabetes mellitus. Obstetrics and Gynecology. 2004;103(3):519–525. doi: 10.1097/01.AOG.0000113621.53602.7a. [DOI] [PubMed] [Google Scholar]
- 59.Qiu CF, Hevner K, Abetew D, Enquobahrie DA, Williams MA. Oxidative DNA damage in early pregnancy and risk of gestational diabetes mellitus: a pilot study. Clinical Biochemistry. 2011;44(10-11):804–808. doi: 10.1016/j.clinbiochem.2011.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thadhani R, Powe CE, Tjoa ML, et al. First-trimester follistatin-like-3 levels in pregnancies complicated by subsequent gestational diabetes mellitus. Diabetes Care. 2010;33(3):664–669. doi: 10.2337/dc09-1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nahum GG, Wilson SB, Stanislaw H. Early-pregnancy glucose screening for gestational diabetes mellitus. Journal of Reproductive Medicine for the Obstetrician and Gynecologist. 2002;47(8):656–662. [PubMed] [Google Scholar]
- 62.Rifai N, Ridker PM. Population distributions of C-reactive protein in apparently healthy men and women in the United States: implication for clinical interpretation. Clinical Chemistry. 2003;49(4):666–669. doi: 10.1373/49.4.666. [DOI] [PubMed] [Google Scholar]
- 63.Kikuchi T, Carbone DP. Proteomics analysis in lung cancer: challenges and opportunities. Respirology. 2007;12(1):22–28. doi: 10.1111/j.1440-1843.2006.00957.x. [DOI] [PubMed] [Google Scholar]
- 64.Kikuchi Y, Kita T, Iwano I, et al. Prediction of clinical course and recurrence of human ovarian cancer by several serum tumor markers. Acta Obstetrica et Gynaecologica Japonica. 1989;41(1):69–76. [PubMed] [Google Scholar]
- 65.Fushiki T, Fujisawa H, Eguchi S. Identification of biomarkers from mass spectrometry data using a “common” peak approach. BMC Bioinformatics. 2006;7, article 358 doi: 10.1186/1471-2105-7-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Listgarten J, Emili A. Statistical and computational methods for comparative proteomic profiling using liquid chromatography-tandem mass spectrometry. Molecular and Cellular Proteomics. 2005;4(4):419–434. doi: 10.1074/mcp.R500005-MCP200. [DOI] [PubMed] [Google Scholar]
- 67.Georgiou HM, Lappas M, Georgiou GM, et al. Screening for biomarkers predictive of gestational diabetes mellitus. Acta Diabetologica. 2008;45(3):157–165. doi: 10.1007/s00592-008-0037-8. [DOI] [PubMed] [Google Scholar]
- 68.Rice GE, Georgiou HM, Ahmed N, Shi G, Kruppa G. Translational proteomics: developing a predictive capacity—a review. Placenta. 2006;27(supplement A):76–86. doi: 10.1016/j.placenta.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 69.Anderon L. Candidate-based proteomics in the search for biomarkers of cardiovascular disease. Journal of Physiology. 2005;563(1):23–60. doi: 10.1113/jphysiol.2004.080473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pencina MJ, D’Agostino RB, D’Agostino RB, Vasan RS. Evaluating the added predictive ability of a new marker: From area under the ROC curve to reclassification and beyond. Statistics in Medicine. 2008;27(2):157–172. doi: 10.1002/sim.2929. [DOI] [PubMed] [Google Scholar]
- 71.Pencina MJ, D’Agostino RB, Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Statistics in Medicine. 2011;30(1):11–21. doi: 10.1002/sim.4085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pencina MJ, D’Agostino RB, Vasan RS. Statistical methods for assessment of added usefulness of new biomarkers. Clinical Chemistry and Laboratory Medicine. 2010;48(12):1703–1711. doi: 10.1515/CCLM.2010.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Georgiou HM, Lappas M, Georgiou GM, et al. Screening for biomarkers predictive of gestational diabetes mellitus. Acta Diabetologica. 2008;45(3):157–165. doi: 10.1007/s00592-008-0037-8. [DOI] [PubMed] [Google Scholar]
- 74.Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. The Lancet. 2009;373(9677):1773–1779. doi: 10.1016/S0140-6736(09)60731-5. [DOI] [PubMed] [Google Scholar]
- 75.Göbl CS, Bozkurt L, Prikoszovich T, Winzer C, Pacini G, Kautzky-Willer A. Early possible risk factors for overt diabetes after gestational diabetes mellitus. Obstetrics and Gynecology. 2011;118(1):71–78. doi: 10.1097/AOG.0b013e318220e18f. [DOI] [PubMed] [Google Scholar]
- 76.Godfrey KM, Forrester T, Barker DJP, et al. Maternal nutritional status in pregnancy and blood pressure in childhood. British Journal of Obstetrics and Gynaecology. 1994;101(5):398–403. doi: 10.1111/j.1471-0528.1994.tb11911.x. [DOI] [PubMed] [Google Scholar]
- 77.Armitage JA, Poston L, Taylor PD. Developmental origins of obesity and the metabolic syndrome: The role of maternal obesity. Frontiers of Hormone Research. 2007;36:73–84. doi: 10.1159/000115355. [DOI] [PubMed] [Google Scholar]
- 78.Nathanielsz PW. Animal models that elucidate basic principles of the developmental origins of adult diseases. ILAR Journal. 2006;47(1):73–82. doi: 10.1093/ilar.47.1.73. [DOI] [PubMed] [Google Scholar]
- 79.Wilson KM, Willett WC, Michels KB. Mothers’ pre-pregnancy BMI and weight gain during pregnancy and risk of breast cancer in daughters. Breast Cancer Research and Treatment. 2011;130:273–279. doi: 10.1007/s10549-011-1582-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cnossen JS, Leeflang MMG, de Haan EEM, et al. Accuracy of body mass index in predicting pre-eclampsia: bivariate meta-analysis. International Journal of Obstetrics & Gynaecology. 2007;114(12):1477–1485. doi: 10.1111/j.1471-0528.2007.01483.x. [DOI] [PubMed] [Google Scholar]
- 81.Bulik CM, Von Holle A, Gendall K, et al. Maternal eating disorders influence sex ratio at birth. Acta Obstetricia et Gynecologica Scandinavica. 2008;87(9):979–981. doi: 10.1080/00016340802334385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Grant SM, Wolever TMS, O’Connor DL, Nisenbaum R, Josse RG. Effect of a low glycaemic index diet on blood glucose in women with gestational hyperglycaemia. Diabetes Research and Clinical Practice. 2011;91(1):15–22. doi: 10.1016/j.diabres.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 83.Haugen M, Vikanes A, Brantsaeter AL, et al. Diet before pregnancy and the risk of hyperemesis gravidarum. British Journal of Nutrition. 2011;106(4):596–602. doi: 10.1017/S0007114511000675. [DOI] [PubMed] [Google Scholar]
- 84.Bertolotto A, Volpe L, Calianno A, et al. Physical activity and dietary habits during pregnancy: effects on glucose tolerance. Journal of Maternal-Fetal and Neonatal Medicine. 2010;23(11):1310–1314. doi: 10.3109/14767051003678150. [DOI] [PubMed] [Google Scholar]
- 85.Bertolotto A, Volpe L, Vignali S, et al. Influence of pre-pregnancy body mass index, physical activity and dietary habits on glucose tolerance during pregnancy. Diabetologia. 2008;51:S466–S466. [Google Scholar]
- 86.Ray JG, O’brien TE, Chan WS. Preconception care and the risk of congenital anomalies in the offspring of women with diabetes mellitus: a meta-analysis. International Journal of Medicine. 2001;94(8):435–444. doi: 10.1093/qjmed/94.8.435. [DOI] [PubMed] [Google Scholar]
- 87.Van Lieshout RJ, Voruganti LP. Diabetes mellitus during pregnancy and increased risk of schizophrenia in offspring: a review of the evidence and putative mechanisms. Journal of Psychiatry and Neuroscience. 2008;33(5):395–404. [PMC free article] [PubMed] [Google Scholar]
- 88.Maconochie N, Doyle P, Prior S, Simmons R. Risk factors for first trimester miscarriage—results from a UK-population-based case-control study. BJOG. 2007;114(2):170–186. doi: 10.1111/j.1471-0528.2006.01193.x. [DOI] [PubMed] [Google Scholar]
- 89.Sundrani DP, Gautam PMC, Mehendale SS, Joshi SR. Altered metabolism of maternal micronutrients and omega 3 fatty acids epigenetically regulate matrix metalloproteinases in preterm pregnancy: a novel hypothesis. Medical Hypotheses. 2011;77(5):878–883. doi: 10.1016/j.mehy.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 90.Kulkarni A, Dangat K, Kale A, Sable P, Chavan-Gautam P, Joshi S. Effects of altered maternal folic acid, vitamin B12 and docosahexaenoic acid on placental global DNA methylation patterns in wistar rats. Plos ONE. 2011;6(3) doi: 10.1371/journal.pone.0017706. Article ID e17706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gallou-Kabani C, Gabory A, Tost J, et al. Sex- and diet-specific changes of imprinted gene expression and dna methylation in mouse placenta under a high-fat diet. Plos ONE. 2010;5(12) doi: 10.1371/journal.pone.0014398. Article ID e14398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Suter M, Abramovici A, Patterson L, et al. Maternal tobacco use modestly alters correlated epigenome wide placental DNA methylation and gene expression. American Journal of Obstetrics and Gynecology. 2011;204(1, supplement):S171–S172. doi: 10.4161/epi.6.11.17819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bobetsis Y, Barros S, Lin D, et al. Bacterial infection promotes DNA hypermethylation. Journal of Dental Research. 2007;86(2):169–174. doi: 10.1177/154405910708600212. [DOI] [PubMed] [Google Scholar]
- 94.O'Reilly JR, Drake AJ, Jones RL, et al. Maternal obesity is associated with altered placental expression and DNA methylation of key genes in fetal growth in human pregnancy during the first trimester, but not at term. Journal of Developmental Origins of Health and Disease. 2011;2:S96–S96. [Google Scholar]
- 95.Gheorghe CP, Goyal R, Mittal A, Longo LD. Gene expression in the placenta: maternal stress and epigenetic responses. International Journal of Developmental Biology. 2010;54(2-3):507–523. doi: 10.1387/ijdb.082770cg. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bouchard L, Thibault S, Guay SP, et al. Placental leptin gene DNA methylation adaptation to gestational diabetes. Obesity. 2010;18:S73–S73. [Google Scholar]
- 97.Wang ZQ, Lu S, Liu CM, et al. Expressional and epigenetic alterations of placental matrix metalloproteinase 9 in preeclampsia. Gynecological Endocrinology. 2010;26(2):96–102. doi: 10.3109/09513590903184100. [DOI] [PubMed] [Google Scholar]
- 98.Yu L, Chen M, Zhao D, et al. The H19 gene imprinting in normal pregnancy and pre-eclampsia. Placenta. 2009;30(5):443–447. doi: 10.1016/j.placenta.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 99.Johnson K, Posner SF, Biermann J, et al. Recommendations to improve preconception health and health care—United States. A report of the CDC/ATSDR preconception care work group and the select panel on preconception care. Morbidity and Mortality Weekly Report. 2006;16(4):454–57. [PubMed] [Google Scholar]
- 100.A Report of the CDC/ATSDR preconception care work group and the select panel on preconception care. Morbidity and Mortality Weekly Report. 2006;55:1–23. Recomendations and Reports. [PubMed] [Google Scholar]
- 101.Elixhauser A, Weschler JM, Kitzmiller JL, et al. Cost-benefit analysis of preconception care for women with established diabetes mellitus. Diabetes Care. 1993;16(8):1146–1157. doi: 10.2337/diacare.16.8.1146. [DOI] [PubMed] [Google Scholar]
- 102.Herman WH, Janz NK, Becker MP, Charron-Prochownik D. Diabetes and pregnancy: preconception care, pregnancy outcomes, resource utilization and costs. Journal of Reproductive Medicine for the Obstetrician and Gynecologist. 1999;44(1):33–38. [PubMed] [Google Scholar]
- 103.Galtier-Dereure F, Boegner C, Bringer J. Obesity and pregnancy: complications and cost. American Journal of Clinical Nutrition. 2000;71(5):1242S–1248S. doi: 10.1093/ajcn/71.5.1242s. [DOI] [PubMed] [Google Scholar]
- 104.Moos MK, Bennett AC. Preconceptional Health Promotion. Springer Science; 2011. Edited by A. Handler , J. Kennelly , N. Peacock. [Google Scholar]
- 105.Church TR, Anderson KE, Caporaso NE, et al. A prospectively measured serum biomarker for a tobacco-specific carcinogen and lung cancer in smokers. Cancer Epidemiology Biomarkers and Prevention. 2009;18(1):260–266. doi: 10.1158/1055-9965.EPI-08-0718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Dorigo O, Berek JS. Personalizing CA125 levels for ovarian cancer screening. Cancer Prevention Research. 2011;4(9):1356–1359. doi: 10.1158/1940-6207.CAPR-11-0378. [DOI] [PubMed] [Google Scholar]


