Abstract
Auto-transplantation of adipose tissue is commonly used for the treatment of tissue defects in plastic surgery. The survival of the transplanted adipose tissue is not always constant, and one of reasons is the accelerated apoptosis of the implanted preadipocytes. We have recently established highly homogeneous preadipocytes, named ccdPAs. The aim of the current study was to evaluate the regulation of the potency of platelet-rich plasma (PRP) on the apoptosis of ccdPAs in vitro. PRP stimulated the proliferation of the preadipocytes in a dose-dependent manner, and the stimulatory activity of 2% PRP was significantly higher than that of 2% FBS or 2% platelet-poor plasma (PPP). The presence of 2% PRP significantly inhibited serum starvation- or TNF-α/cycloheximide-induced apoptosis in comparison to 2% FBS or 2% PPP. DAPK1 and Bcl-2-interacting mediator of cell death (BIM) mRNAs were reduced in the preadipocytes cultured with 2% PRP in comparison to those cultured in 2% FBS. The gene expression levels were significantly higher in cells cultured without serum in comparison to cells cultured with 2% FBS, and the levels in the cells with 2% PRP were reduced to 5-10% of those in the cells without serum. These results indicated that ccdPAs exhibit anti-apoptotic activities, in addition to increased proliferation, when cultured in 2% PRP in comparison to the same concentration of FBS, and that this was accompanied with reduced levels of DAPK1 and BIM mRNA expression in in vitro culture. PRP may improve the outcome of transplantation of adipose tissue by enhancing the anti-apoptotic activities of the implanted preadipocytes.
Keywords: adipocytes, apoptosis, Bcl-2-like protein 11, death-associated protein kinase, platelet-rich plasma, tissue transplantation
Introduction
Aspirated fat is a common source of autologous tissue transplantation for the correction of tissue defects in plastic and reconstructive surgery (Billings and May, 1989; Patrick, 2000, 2001). Aspirated fat contains multipotential preadipocytes and progenitor cells, which have been utilized as a source of cell-based regenerative medicine (Stashower et al., 1999; Zuk et al., 2001; Gimble et al., 2007; Yoshimura et al., 2009; Bauer-Kreisel et al., 2010; Sterodimas et al., 2010). Although several different techniques of fat grafting have been developed, the outcomes of the transplantation vary widely. The most important factor required for successful grafting is to optimize the survival of the transplanted preadipocytes and other cells in the graft. In previous studies, we and others have shown that various cytokines are involved in the efficient cell survival of the implants (Kimura et al., 2003; Yamaguchi et al., 2005; Cho et al., 2006; Torio-Padron et al., 2007; Kuramochi et al., 2008; Ning et al., 2009).
Platelet rich plasma (PRP) (Eppley et al., 2006; Foster et al., 2009; Redler et al., 2011) has been widely applied for practical medicine, such as aesthetic plastic surgery and the treatment of soft-tissue ulcers (Welsh, 2000; Man et al., 2001; Margolis et al., 2001; Bhanot and Alex, 2002; Martinez-Zapata et al., 2009; Sclafani, 2009). Once activated, platelets secrete various bioactive cytokines, including platelet-derived growth factor (PDGF) and transforming growth factor beta 1 (TGF-β1), which increase angiogenesis and cell proliferation relevant to soft tissue regeneration. PRP has been applied for fat grafting, and in fact, has been shown to improve the survival of implanted adipose tissue in patients (Abuzeni and Alexander, 2001; Sadati et al., 2006; Cervelli et al., 2009). Thus, the use of PRP has been broadened to the tissue-engineering field using adipose tissue-derived multi-potential cells (Anitua et al., 2006; Muller et al., 2009). PRP is also expected to function as an autologous fibrin-based scaffold for transplanted cells (Anitua et al., 2006; Wu et al., 2009; Kang et al., 2011). In fact, recent our study showed that fibrin-based scaffold decreased the apoptotic cell death of murine ccdPAs in mice transplantation model (Aoyagi et al., 2011).
We have recently identified proliferative preadipocytes, ceiling culture-derived proliferative adipocytes (ccdPAs), as homogeneous cells suitable for ex vivo gene therapy applications via autologous transplantation (Asada et al., 2011; Kuroda et al., 2011). The ccdPAs are characterized by their high proliferative capacity with spontaneous adipogenic potential in scaffold fibrin gel culture (Aoyagi et al., 2012). The establishment of a highly homogenous preadipocyte line made it possible to perform examinations to identify the optimal scaffolds and cytokines that can be used to improve the survival of transplanted preadipocytes. We herein studied the effects of PRP, and an autologous cytokine cocktail, on the apoptotic properties of preadipocytes using the ccdPAs.
Results
PRP inhibits fibrin scaffold gel shrinkage and improves the viability of ccdPAs in 3-dimensional culture
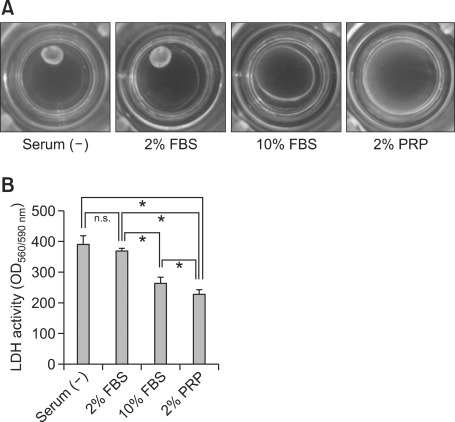
We have recently established a 3-dimensional (3-D) culture system for ccdPAs using fibrin gel (FG) (Aoyagi et al., 2012). Using the 3-D culture system, the effects of PRP on the gel shrinkage and cell viability were analyzed in comparison to FBS. The FG/ccdPAs were formed and maintained in culture medium containing 10% FBS for 16 hr. The culture medium was replaced with fresh medium containing 2% PRP, 2% FBS or 10% FBS, or with medium without serum, and cells were subsequently incubated for an additional 24 hr.
The resulting gel sizes varied among the cultures grown in each type of medium. The gels without serum or with 2% FBS showed a drastic volume reduction, while the volumes of the gels cultured with 10% FBS or 2% PRP were not obviously reduced (Figure 1A). The culture supernatants were collected from each well and LDH activity was measured to evaluate the viability of cells. The LDH activity significantly decreased in the culture medium with 2% PRP in comparison to the medium with 2% or 10% FBS (Figure 1B). TUNEL staining of the gel sections showed the number of apoptotic cells to significantly decrease in the medium with 2% PRP in comparison to the medium with 2% FBS (1.5 ± 1.1% vs 9.8 ± 1.9%, P < 0.05). These results suggested that 2% PRP inhibits the shrinkage of FG/ccdPAs gels, and improves the cell viability in comparison to the same concentration of FBS.
Figure 1.
The effects of platelet-rich plasma (PRP) on the 3-dimensional culture of ccdPAs. 100 µl of fibrin gels containing 1 × 107 cells/ml of ccdPAs (FG/ccdPAs) were formed in cell culture insert and incubated in DMEM/HAM with 10% FBS for 16 hrs. The medium was replaced by DMEM/HAM in the presence or absence of different concentrations of FBS or PRP. (A) Photographs of FG/ccdPAs in the inserts were taken after 24 hr of culture. (B) The culture supernatant was collected from each well and the LDH activities expressed by the fluorescence of resorufin generated by coupled enzymatic reaction were examined. *P < 0.05.
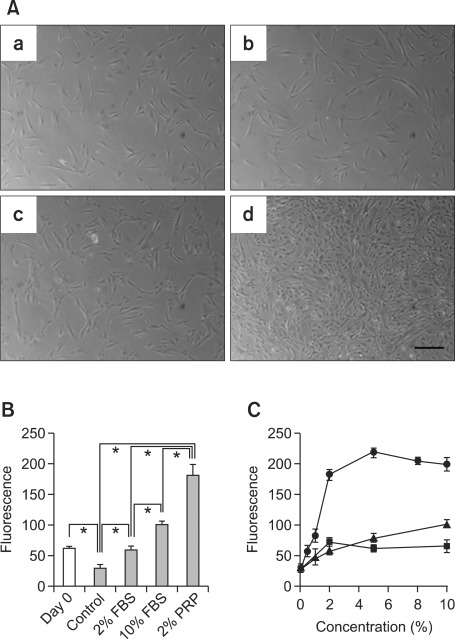
PRP has a high proliferation-inducing potential for ccdPAs in plate culture
In order to evaluate the function of PRP on cell survival in the gel, we next examined the effects of PRP on the proliferation of ccdPAs in comparison to FBS. The cells (2.5 × 105 cells) were seeded and incubated with DMEM/HAM containing 20% FBS in 10 cm dishes for 16 hr. The media was replaced with medium containing 2% PRP, 2% FBS, or 10% FBS, and the cells were then cultured for 3 days. The cell appearance was not apparently changed among the ccdPAs cultured for 3 days in plates with media containing 2% PRP, 2% FBS, or 10% FBS (Figure 2A). To examine the cell proliferation, 2 × 103 cells of ccdPAs were seeded onto 96 well plates and incubated at 37℃ for 24 hr. The media was replaced with medium with or without 2% PRP, 2% FBS, or 10% FBS (Day 0), and the cells were cultured for 3 days. The number of cells in each well was evaluated by measuring the DNA content. In contrast to the observation that the cell numbers on Day 3 were not significantly changed in comparison to those at Day 0 in the cultures incubated in medium containing 2% FBS, the cell numbers were significantly increased in cells cultured in the medium with 10% FBS or 2% PRP, and notably, the number of cells on Day 3 in the medium containing 2% PRP was significantly increased in comparison to the cells cultured with 10% FBS (Figure 1B). The cell numbers in the media with various concentrations of PRP showed a dose-dependent increase up to 5% PRP; the number of cells present in the media with 0.5-1% PRP was almost equivalent to that of the cells cultured with 5-10% FBS (Figure 2C). These results indicated that the proliferation-inducing potential of PRP for ccdPAs was higher in comparison to that of FBS.
Figure 2.
Platelet-rich plasma (PRP) promotes the proliferation of ccdPAs. (A) Photographs of ccdPAs were taken after 3 days in culture containing DMEM/F12-HAM in the absence of serum (a) or the presence of 2% (b) or 10% (c) FBS or 2% (d) PRP. The scale bar indicates 200 µm. (B) Cells were seeded into 96 well plates and incubated in DMEM/F12-HAM containing 20% FBS for 24 hr. The culture medium was then replaced with DMEM/F12-HAM in the absence of serum (control) or presence of 2% FBS or 10% FBS or 2% PRP. After 3 days in CO2 incubator, the cell number in each well was examined by DNA content in comparison to those on day 0 (open bar). The values for the serum (-), 10% FBS, and 2% PRP groups were significantly different compared with those on Day 0 (*P < 0.05). (C) The cell numbers were examined in wells cultured in DMEM/F12-HAM containing various concentrations of PRP (circle), FBS (triangle), and PPP (square) after 3 days of culture similarly as Figure 2B. The growth stimulatory effect was not significantly different between 10% and 20% FBS and PPP (data not shown).
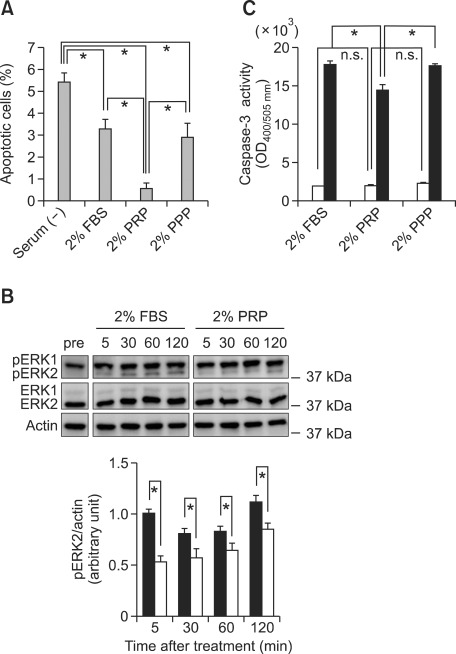
PRP inhibits the apoptosis of ccdPAs
The high proliferation-inducing property of PRP for ccdPAs in culture prompted us to further analyze PRP for protective effects against apoptosis in ccdPAs, since PRP is rich in cytokines and proteinases involved not only in proliferation, but also in regulating apoptosis (Eppley et al., 2004, 2006; Foster et al., 2009; Redler et al., 2011). The protection of the cells from death may contribute to their longer survival after transplantation, together with a high potential for proliferation. To investigate the possibility, the ccdPAs (1 × 106 cells) were seeded and incubated in a 10 cm dish with DMEM/HAM medium containing 20% FBS for 16 hr, and subsequently incubated with the medium with or without 2% FBS, 2% PRP, or 2% PPP. After incubation for 8 hr, the cells were collected and stained with Annexin V-FITC. The flow cytometric analysis showed that 5.5% of cells were identified as Annexin V positive in the medium without serum (Figure 3A). The number of apoptotic cells was significantly decreased in the media with 2% FBS, 2% PRP, or 2% PPP in comparison to that in the cells cultured in serum-free medium. Among the various supplements, 2% PRP drastically reduced the number of apoptotic cells in comparison to 2% FBS or 2% PPP. ERK1/2 phosphorylation was examined to further analyze the protective effect of PRP against apoptosis, because the activation of the cascade is important for apoptosis via various intracellular signals including TNF-α (Cawthorn and Sethi, 2008; Mebratu and Tesfaigzi, 2009; Cagnol and Chambard, 2010). The cells were incubated with 2% PRP, FBS, or PPP for 2 hr, and apoptosis was induced by TNF-α and cycloheximide. Phosphorylation was detected following treatment with TNF-α and cycloheximide for 5 min in the cells cultured with 2% FBS. A densitometric analysis showed the amount of phosphorylated ERK2, and not phosphorylated ERK1, to significantly decrease in the medium with 2% PRP in comparison to the medium with 2% FBS (Figure 3B). The caspase-3 activity induced by TNF-α and cycloheximide for 3 hr were also significantly decreased in ccdPAs in the medium with 2% PRP in comparison to the cells cultured with 2% FBS or 2% PPP (Figure 3C). Thus, the apoptosis of ccdPAs was inhibited by culturing them in the medium with 2% PRP in vitro.
Figure 3.
PRP decreased the apoptotic cell death and caspase 3 activity induced by TNF-α and cycloheximide in ccdPAs. (A) ccdPAs were seeded and incubated for 16 hr with medium containing 20% FBS, and the medium was then replaced with fresh medium without serum (Serum (-)) or with media containing 2% PRP, FBS, or PPP, and the cells were subsequently incubated at 37℃ for 8 hr. The cells were then collected, stained by Annexin V-FITC and propidium iodide (PI), and analyzed using a Tali™ Image Based Cytometer (Life technologies). FITC-positive/PI-negative cells were considered to be apoptotic cells. *P < 0.05. (B) After incubation for 16 hr with medium containing 20% FBS, ccdPAs were pretreated for 2 hr with the medium containing 2% PRP or FBS. The cells were treated with TNF-α and cycloheximide for 5, 30, 60, and 120 min in the medium with 2% FBS (closed bar) or 2% PRP (open bar). Cell lysates were prepared at each time point as well as pretreatment (pre) and then were subjected to an immunoblot analysis of phosphorylated or unphosphorylated form of ERK1/2, and Actin. Results of densitometric analysis of phosphorylated form of ERK2 (pERK2) is shown below. After normalization of signals of pERK2 by Actin, each value of pERK2 was expressed as the fold increase of that at 5 min with 2% FBS. *P < 0.05. (C) After pretreatment for 2 hr with the medium containing 2% PRP, FBS, or PPP, the cells were incubated for 3 hr in the absence (open bars) or presence (closed bars) of TNF-α and cycloheximide, which induce apoptotic cell death. The caspase-3 activity in the lysates of collected cells were measured. *P < 0.05.
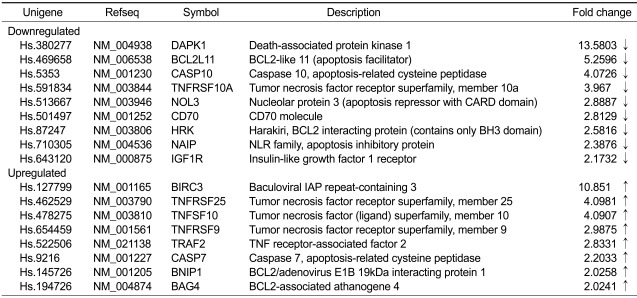
PRP almost completely inhibits the expression of the pro-apoptotic genes, DAPK1 and BIM, in ccdPAs after serum starvation
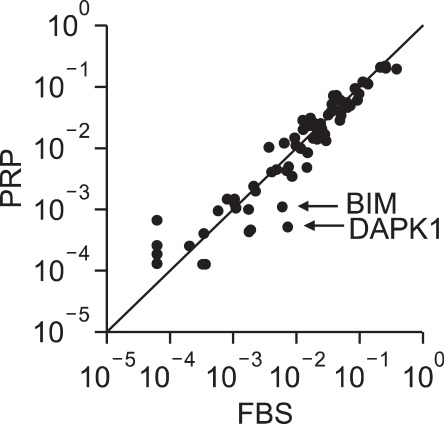
In order to identify the molecules involved in the anti-apoptotic effects of PRP on ccdPAs in culture, the expression profiles of representative apoptosisrelated genes were examined using a PCR array profiler. The cells (2.5 × 105 cells) were seeded into 10 cm dishes and incubated in DMEM/HAM containing 20% FBS for 16 hr. The media was replaced with DMEM/HAM containing 2% PRP or FBS, the cells were incubated for 3 days, and the total RNA was isolated from the cultured cells to analyze the expression of apoptosis-related genes. Two independent experiments showed that, among the 84 genes examined, there were 8 genes with a more than 2-fold increase in expression, and 9 genes with a more than 2-fold decrease in expression in the cells cultured in the medium with 2% PRP compared with those cultured in the medium with 2% FBS (Table 1). We focused our interest on two genes, DAPK1 (reduced to 7.4% of the expression level observed with FBS) and BCL2L11 (also called BIM, reduced to 18.9% of the level observed with FBS), as representative genes with the obvious downregulation in the medium with 2% PRP (Figure 4). DAPK1 and BIM have been shown to be one of master regulators of cell death (Gozuacik and Kimchi, 2006), and is essential for BAX-dependent cell death (Kim et al., 2009; Ren et al., 2010), respectively.
Table 1.
Apoptosis-related genes affected by PRP
Genes identified as having a change in expression > 2-fold induced by the addition of PRP in comparison to 2% FBS are shown.
Figure 4.
The results of the analysis of the expression of apoptosis-related genes affected by PRP. Total RNA was extracted from the cells cultured in the presence of 2% FBS or 2% PRP for 72 hr. The total RNA was subjected to cDNA synthesis and subsequent quantification of the mRNA expression for various apoptosis-related genes. The fold-changes in the quantified mRNA amounts compared to the average value of house-keeping genes were plotted for each gene (x-axis; cultured in 2% FBS, y-axis; cultured in 2% PRP).
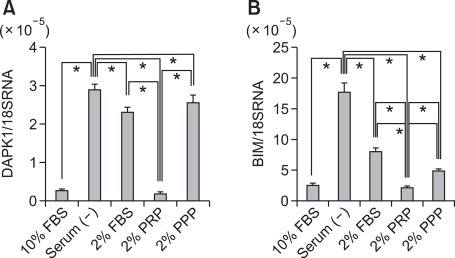
The role of DAPK1 and BIM genes in apoptosis of preadipocytes was investigated by examining the effect of serum starvation of cells incubated with PRP on the expressions of these genes. The ccdPAs (2.5 × 105 cells) were seeded into 10 cm dishes and incubated in DMEM/HAM containing 20% FBS for 16 hr. The medium was replaced by medium containing 10% FBS (control), 2% FBS, 2% PRP, or 2% PPP, the cells were cultured for 3 days and the expression of DAPK1 and BIM were analyzed. The DAPK1 mRNA level was increased 10.6-fold by serum starvation in comparison to the level in the cells cultured with 10% FBS, and the mRNA level was decreased to that of 10% FBS by the presence of 2% PRP. It is worth noting that, although the mRNA levels of DAPK1 in the cells cultured with 2% FBS and 2% PPP significantly decreased in comparison to those cultured without serum, the reductions were by 20.4% and 11.9%, respectively, which were less than that (93.6%) induced by culture in 2% PRP. The BIM mRNA levels were also drastically increased in the cells cultured in serum free medium in comparison to those cultured in the medium with 10% FBS (Figure 2C). The mRNA levels were reduced to those observed in the cells cultured with 10% FBS by the addition of 2% PRP. Again, the potential of 2% PRP to inhibit the mRNA expression of the target gene (by 87.2%) was significantly higher than that of the 2% FBS (54.1%) or 2% PPP (72.2%). Thus, PRP almost completely inhibited the expression of apoptosis-related genes induced by serum starvation.
Discussion
PRP inhibited the volume reduction of the 3D gels embedded with ccdPAs, the homogeneous preadipocytes, in comparison to the same concentration of FBS, and this was accompanied by increased cell viability in the gel. These observations prompted us to analyze the effects of PRP on the apoptosis and proliferation of the ccdPAs. The results showed that 2% PRP had a higher inhibitory effect on the apoptotic cell death of ccdPAs than 2% FBS or 2% PPP (Figure 3). A comparison between 2% PRP and 2% FBS by a gene expression profile analysis revealed that PRP downregulated 11% of the 84 representative apoptosis-related genes and upregulated 10% of the 84 representative apoptosis-related genes (Figure 4 and Table 1). The most drastically reduced genes were DAPK1, the protein product of which plays important roles in a wide range of signal transduction pathways with diverse outcomes, such as apoptosis, autophagy and immune responses (Lin et al., 2010), and BIM, encoding one of the BH3-only proteins, which is a critical regulator of apoptosis in many cell types (Ramesh et al., 2009). The induction of these genes by apoptotic stimuli was almost completely prevented in the presence of PRP (Figure 5).
Figure 5.
Serum starvation induced the expression of the DAPK1 and BIM genes, which was prevented by culture with 2% PRP. The ccdPAs were seeded and incubated for 16 hr in DMEM/HAM containing 20% FBS, and the culture medium was then replaced with medium without serum (Serum (-)), or with 2% or 10% FBS, 2% PRP, or 2% PPP, followed by incubation for an additional 72 hr. Quantitative reverse transcription-polymerase chain reaction (RT-PCR) was performed to evaluate the mRNA expression levels of DAPK1 (A) and BIM (B). The quantification of the given genes was expressed as relative mRNA level compared with a control after normalization to 18S RNA. *P < 0.05.
PRP, a concentrate of physiological cytokines, has been widely utilized as an injectable material in the clinic since the 1970s to enhance soft and hard tissue healing (Andia et al., 2010; Lopez-Vidriero et al., 2010; Redler et al., 2011; Yu et al., 2011), mainly by stimulating cell proliferation and angiogenesis in the injured tissues. PRP promotes the growth of various cells, including tissue-derived progenitor cells (Liu et al., 2002; Lucarelli et al., 2003; Doucet et al., 2005; Frechette et al., 2005; Vogel et al., 2006; Kakudo et al., 2008; Kurita et al., 2008; Cervelli et al., 2009; Chieregato et al., 2011), and increases the revascularization of the transplanted tissues (Bir et al., 2009). Based on these findings, the clinical applications of PRP have been broadened to recommend its use as an additive to tissue/cell transplantation therapies in plastic and reconstructive surgeries, and more recently in regenerative medicine. In fact, PRP has been shown to improve the fat graft survival (Abuzeni and Alexander, 2001; Sadati et al., 2006; Cervelli et al., 2009; Nakamura et al., 2010; Pires Fraga et al., 2010; Oh et al., 2011) and bone and periodontal regenerations via cell transplantation (Tobita et al., 2008; Chen et al., 2010; Yamada et al., 2010; Arvidson et al., 2011).
In order to apply PRP for clinical transplantation therapy using preadipocytes cultured in vitro, it is necessary to elucidate the effects of PRP on cell survival in the grafts. However, the mechanisms by which PRP increases graft survival have not been well-characterized so far. The current study showed that PRP strongly induces the proliferation of ccdPAs, preadipocytes which were previously shown to be more adipogenic than ASCs (Asada et al., 2011), compared with FBS at an equivalent concentration. Vogel et al. (2006) described that, because the addition of 2% PRP did not result in sufficient thrombocyte-clot formation to maintain a clot in the medium, a higher concentration of PRP, 3%, was evaluated for the stimulation of the MSC proliferation. In this study, to evaluate the efficacy of lower concentrations of PRP, the PRP was activated by thrombin to release cytokines (Aiba-Kojima et al., 2007) prior to the experiments. As a result, 2% PRP showed almost the same effects on proliferation as 10% PRP, indicating its usability as a substitute for FBS in the expansion of preadipocytes for clinical applications. Finally, 2% PRP showed anti-apoptotic activities on the preadipocytes, providing evidence that it can be used as an efficacious additive in the cell transplantation cocktail.
We observed that the expression of the DAPK1 and BIM genes was substantially upregulated by serum starvation in ccdPAs. However, the addition of PRP in the growth media effectively inhibited the apoptosis and downregulated the expression of these genes. TGF-β has been shown to induce the expression of DAPK1 and BIM, and to lead to subsequent apoptosis in other cell types (Jang et al., 2002; Wildey et al., 2003; Ramjaun et al., 2007; Yu et al., 2008). PRP may therefore inhibit the TGF-β-induced apoptosis cascade(s) during serum starvation in ccdPAs. Further analyses are needed to elucidate the mechanism(s) underlying the inhibitory potential of PRP on the expression levels of the representative apoptotic genes. The gene expression analysis also showed that PRP regulated the expression levels of genes involved in TNF signaling (TNFRSF10A, TNFRSF25, TNFSF10, TNFRSF9, and TRAF2), and of the Bcl protein superfamily, with its related proteins (HRK, BNIP1, and BAG4) (Table 1). The changes in the expression of these genes may also improve the survival of ccdPAs by modulating the apoptotic stimuli, considering that TNF-α signaling plays an important role in the regulation of the adipose tissue mass (Warne, 2003).
In conclusion, PRP inhibits cell apoptosis as well as or better than FBS, and also promotes the proliferation of the ccdPAs. The gene expression analyses identified that the DAPK1 and BIM genes were the most highly downregulated apoptosis-related genes by PRP treatment in the preadipocytes. The identified characteristics of PRP with regard to the preadipocytes have advantages including increases in the cell number and improved cell survival in the transplanted grafts. Together with our findings for the efficacies of fibrin scaffold in transplantation of ccdPAs (Aoyagi et al., 2011), the use of PRP for cell preparation and implantation of fat tissues and/or propagated cells may provide the graft with stable long-term survival after auto-transplantation.
Methods
Cell culture
Subcutaneous adipose tissues were obtained from healthy donors after informed consent was obtained, with approval from the ethics committee of Chiba University School of Medicine, and all studies were performed according to the guidelines of the Declaration of Helsinki. The preparation of the ceiling culture-derived proliferative adipocytes (ccdPAs) was performed as described previously (Kuroda et al., 2011). Dulbecco's modified Eagle's medium/F12-HAM (DMEM/HAM, Sigma-Aldrich, St. Louis, MO) supplemented with 20% fetal bovine serum (FBS, SAFC Biosciences, Lenexa, KS) and 40 µg/ml gentamicin (GENTACIN, Schering-Plough Co., Kenilworth, NJ) was used as the culture media, unless otherwise noted in the text.
Preparation of PRP
Human PRP and PPP were prepared from healthy donors as follows; 52 ml of blood was obtained from the donors and mixed with 8 ml of Anticoagulant Citrate Dextrose Solution Formula A (ACD-A, TERUMO, Tokyo, Japan) solution, and transferred to 15 ml tubes. The tubes were centrifuged at 300 × g for 15 min at 20℃. The plasma and the buffy coat below the plasma were collected and transferred to new tubes. Secondary centrifugation was performed at 2000 × g for 15 min at 20℃. The clear supernatant (plasma) was decanted off until 6 ml was left and the middle portion of supernatant (plasma) was taken to be used as PPP. Finally, the remaining supernatant including the buffy coat was taken to be used as PRP. The platelet number of each product was automatically measured (XS 800i, sysmex Japan). The PRP utilized in this study contained 8.6 × 106 platelets/µl, which was approximately 7-fold concentrated from the original concentration in whole human plasma. Preparations of serum lysates containing platelet-released growth factors were essentially performed according to the method described by Aiba-Kojima et al. (2007). In brief, 2 U/ml of thrombin (Astellas Pharma Inc. Tokyo, Japan) was added to PRP and PPP, and the samples were agitated for 1 hr at 37℃ and then incubated overnight at 4℃. Platelet bodies and any remaining fibrin were eliminated by centrifugation (2000 × g for 10 min), and the supernatants were obtained for the PRP and PPP. The serum samples were frozen at -20℃ and thawed at 37℃ before use. The growth medium was supplemented with 2 U/ml of heparin (Novo-Heparin, 5,000 units/5 ml for Injection, Mochida Pharm. Co. Tokyo, Japan).
Culture on fibrin scaffolds
Bolheal (The Chemo-Sero-Therapeutic Research Institute, Kumamoto, Japan) was used as a clinically available material to generate the fibrin gel. Fibrinogen and thrombin solutions were diluted with Ringer's Solution (Fuso Pharmaceutical Industries, Osaka, Japan) containing 0.5% human serum albumin (Mitsubishi Tanabe Pharma., Tokyo, Japan). The ccdPAs were suspended at 1 × 107 cells/ml by the diluted fibrinogen and thrombin solution. The final concentration of fibrinogen was 4 mg/ml and the thrombin solution was used at 1 U/ml. To form fibrin clots, 50 µl of the cell-fibrinogen suspension was added to each cell culture insert (Falcon 3104; Becton Dickinson, Franklin Lakes, NJ), then shortly thereafter, 50 µl of the cell-thrombin suspension was added into the insert, mixed by pipetting, and incubated at room temperature for 2 h. The inserts with fibrin clots were put on 12 well culture plates, and culture media were added to the inserts and wells. The plates were incubated at 37℃ for 12 h in a 5% CO2 incubator, and the media were replaced by fresh media containing FBS or PRP.
LDH assay
LDH released into the culture supernatant from the FG/ccdPA was measured using the CytoTox-One Homogeneous Membrane Integrity Assay kit (Promega, Madison, WI). A 100 µl sample of each culture supernatant was collected and added into to a 96-well plate. An equal volume of CytoTox-One Reagent was added and incubated for 10 min. Fifty µl of Stop Solution was added and the sample fluorescence was measured on a fluorescence microplate reader (SPECTRA max GEMINI XPS, Molecular Devices, Carlsbad, CA) using a wavelength of 560 nm/590 nm for excitation/emission. The original culture medium before the serum concentration was changed served as a pre-treatment control sample and the control value was subtracted from the value obtained after incubation with the medium containing different concentrations of serum.
Cell proliferation assay
The cell proliferation was examined using the CyQUANTR Cell Proliferation Assay Kit (Life Technologies, Carlsbad, CA). Cells were seeded into 96 well plates at a density of 2 × 103 cells per well with DMEM/HAM/20% FBS. After 24 h, the culture medium was removed and changed to fresh DMEM/HAM without serum, or with FBS, PRP or PPP. After 3 days, the microplates were gently inverted and blotted onto paper towels to remove the medium from the wells. The microplates were then frozen and stored at -80℃ and thawed at room temperature prior to analysis. CyQUANT GR dye/cell-lysis buffer was added to each well. Cells were incubated at room temperature for 5 min and the sample fluorescence was measured on a fluorescence microplate reader (SPECTRA max GEMINI XPS, Molecular Devices) using wavelength of 480 nm/520 nm for excitation/emission.
Induction of apoptosis, and the annexin V binding and caspase 3 activity assays
The cells were seeded into 10 cm dishes at a density of 1 × 106 cells per well with DMEM/HAM/20%FBS. After 24 h, the culture medium was removed and changed to fresh DMEM/HAM with 2% FBS, 2% PRP or 2%PPP. After 2 h, apoptosis was induced by the addition of 100 ng/ml TNF-α (Peprotech, Rocky Hill, NJ) and 100 µg/ml cycloheximide (CHX, Sigma-Aldrich). After 3 h, the culture supernatant was collected, and the cells were detached by TrypZean treatment. The detached cells were suspended in the collected culture supernatant. Subsequently, the cells were stained with Annexin V-FITC using a Tali™ Apoptosis kit (Life Technologies). Stained cells were analyzed by a Tali™ Image Based Cytometer (Life technologies). Cell lysates at the concentration of 1 × 104 cells/µl were prepared from the cells treated to induce apoptosis, and the caspase 3 activity levels were measured by a caspase-3/CPP32 Fluorometric Assay Kit (Biovision, Mountain View, CA). To examine the phosphorylation status of ERK1/2, the cells were scraped off at each time point in PBS and washed. The cells were pelleted and lysed by RIPA buffer (Wako Pure Chemical Industries, Ltd. Osaka, Japan), and the protein concentration was determined by Quant-iT Protein Assay Kit (Life technologies), and 5 µg of protein were analyzed by Western blotting using anti-ERK1 and anti-ERK1/2 (pT202/pY204) as primary antibodies (BD Biosciences, Franklin Lakes, NJ). Mouse TrueBlot ULTRA HRP-conjugated Anti-Mouse IgG (eBioscience, Inc. San Diego, CA) was used as a secondary antibody, and the signals were detected by SuperSignal® West Femto Maximum Sensitivity Substrate (Thermo Fisher Scientific Inc.) with LAS1000 apparatus (FUJI film, Tokyo, Japan). ERK signals were normalized using Actin signals detected by Anti-Actin monoclonal antibody (clone AC-40, Sigma-Aldrich).
Gene expression analysis
Cells (2.5 × 105 cells) were seeded into 10 cm dish with DMEM/HAM/20% FBS and cultured for 16 h. The culture medium was changed to fresh DMEM/HAM supplemented with 2% FBS or 2% PRP, and the cells were further incubated for 72 h. The total RNA from cultured cells was extracted using a RT2 RNA Isolation Kit (SA Bioscience, Frederick, MD). Complementary DNA was generated from 1 µg of total RNA using the RT2 First Strand Kit. An Apoptosis Reverse Transcriptase RT2 profiler PCR array and RT2 Real-Time SYBR Green/ROX PCR Mix (SA Bioscience, Frederick, MD) were used to identify the genes affected by PRP according to manufacturer's instruction. The data were analyzed by web-based data analysis software provided by the manufacturer. The probe and primer sets used to quantify the mRNA for the DAPK1 and BIM genes were purchased from Applied Biosystems (Life Technologies). The quantification of given genes was expressed as the relative mRNA level compared with a control after normalization to 18S RNA. All the real-time PCR were performed using an ABI 7500 real-time PCR apparatus.
Statistical analysis
The data are presented as the means ± S.D. Statistical comparisons were made by Student's t-test or an ANOVA followed by the post-hoc Tukey test using the SPSS software program. In all cases, P-values < 0.05 were considered to be significant.
Acknowledgements
We thank Dr. Fumiaki Matsumoto, Mr. Shunichi Konno, Dr. Shigeaki Tanaka, and Mr. Masayuki Aso for helpful and valuable suggestions about our research. This study was supported by Health and Labour Sciences Research Grants for Translational Research, Japan (H. B.), and in part by the Global COE Program (Global Center for Education and Research in Immune System Regulation and Treatment), MEXT, Japan (Y.O., Y.N., and H.B.).
Abbreviations
- BIM
Bcl-2-interacting mediator of cell death
References
- 1.Abuzeni PZ, Alexander RW. Enhancement of autologous fat transplantation with platelet rich plasma. Am J Cosmet Surg. 2001;18:59–70. [Google Scholar]
- 2.Aiba-Kojima E, Tsuno NH, Inoue K, Matsumoto D, Shigeura T, Sato T, Suga H, Kato H, Nagase T, Gonda K, Koshima I, Takahashi K, Yoshimura K. Characterization of wound drainage fluids as a source of soluble factors associated with wound healing: comparison with platelet-rich plasma and potential use in cell culture. Wound Repair Regen. 2007;15:511–520. doi: 10.1111/j.1524-475X.2007.00259.x. [DOI] [PubMed] [Google Scholar]
- 3.Andia I, Sanchez M, Maffulli N. Tendon healing and platelet-rich plasma therapies. Expert Opin Biol Ther. 2010;10:1415–1426. doi: 10.1517/14712598.2010.514603. [DOI] [PubMed] [Google Scholar]
- 4.Anitua E, Sanchez M, Nurden AT, Nurden P, Orive G, Andia I. New insights into and novel applications for platelet-rich fibrin therapies. Trends Biotechnol. 2006;24:227–234. doi: 10.1016/j.tibtech.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 5.Aoyagi Y, Kuroda M, Asada S, Bujo H, Tanaka S, Konno S, Tanio M, Ishii I, Aso M, Saito Y. Fibrin glue increases the cell survival and the transduced gene product secretion of the ceiling culture-derived adipocytes transplanted in mice. Exp Mol Med. 2011;43:161–167. doi: 10.3858/emm.2011.43.3.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aoyagi Y, Kuroda M, Asada S, Tanaka S, Konno S, Tanio M, Aso M, Okamoto Y, Nakayama T, Saito Y, Bujo H. Fibrin grue is a candidate scaffold for long-term therapeutic protein expression in spontaneously differentiated adipocytes in vitro. Exp Cell Res. 2012;318:8–15. doi: 10.1016/j.yexcr.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 7.Arvidson K, Abdallah BM, Applegate LA, Baldini N, Cenni E, Gomez-Barrena E, Granchi D, Kassem M, Konttinen YT, Mustafa K, Pioletti DP, Sillat T, Finne-Wistrand A. Bone regeneration and stem cells. J Cell Mol Med. 2011;15:718–746. doi: 10.1111/j.1582-4934.2010.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asada S, Kuroda M, Aoyagi Y, Fukaya Y, Tanaka S, Konno S, Tanio M, Aso M, Satoh K, Okamoto Y, Nakayama T, Saito Y, Bujo H. Ceiling culture-derived proliferative adipocytes retain high adipogenic potential suitable for use as a vehicle for gene transduction therapy. Am J Physiol Cell Physiol. 2011;301:C181–C185. doi: 10.1152/ajpcell.00080.2011. [DOI] [PubMed] [Google Scholar]
- 9.Bauer-Kreisel P, Goepferich A, Blunk T. Cell-delivery therapeutics for adipose tissue regeneration. Adv Drug Deliv Rev. 2010;62:798–813. doi: 10.1016/j.addr.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 10.Bhanot S, Alex JC. Current applications of platelet gels in facial plastic surgery. Facial Plast Surg. 2002;18:27–33. doi: 10.1055/s-2002-19824. [DOI] [PubMed] [Google Scholar]
- 11.Billings E, Jr, May JW., Jr Historical review and present status of free fat graft autotransplantation in plastic and reconstructive surgery. Plast Reconstr Surg. 1989;83:368–381. doi: 10.1097/00006534-198902000-00033. [DOI] [PubMed] [Google Scholar]
- 12.Bir SC, Esaki J, Marui A, Yamahara K, Tsubota H, Ikeda T, Sakata R. Angiogenic properties of sustained release platelet-rich plasma: characterization in-vitro and in the ischemic hind limb of the mouse. J Vasc Surg. 2009;50:870–879.e2. doi: 10.1016/j.jvs.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 13.Cagnol S, Chambard JC. ERK and cell death: mechanisms of ERK-induced cell death-apoptosis, autophagy and senescence. FEBS J. 2010;277:2–21. doi: 10.1111/j.1742-4658.2009.07366.x. [DOI] [PubMed] [Google Scholar]
- 14.Cawthorn WP, Sethi JK. TNF-a and adipocyte biology. FEBS Lett. 2008;582:117–131. doi: 10.1016/j.febslet.2007.11.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cervelli V, Gentile P, Scioli MG, Grimaldi M, Casciani CU, Spagnoli LG, Orlandi A. Application of platelet-rich plasma in plastic surgery: clinical and in vitro evaluation. Tissue Eng Part C Methods. 2009;15:625–634. doi: 10.1089/ten.TEC.2008.0518. [DOI] [PubMed] [Google Scholar]
- 16.Chen FM, Zhang J, Zhang M, An Y, Chen F, Wu ZF. A review on endogenous regenerative technology in periodontal regenerative medicine. Biomaterials. 2010;31:7892–7927. doi: 10.1016/j.biomaterials.2010.07.019. [DOI] [PubMed] [Google Scholar]
- 17.Chieregato K, Castegnaro S, Madeo D, Astori G, Pegoraro M, Rodeghiero F. Epidermal growth factor, basic fibroblast growth factor and platelet-derived growth factor-bb can substitutefor fetal bovine serum and compete with human platelet-rich plasma in the ex vivo expansion of mesenchymal stromal cells derived from adipose tissue. Cytotherapy. 2011;13:933–943. doi: 10.3109/14653249.2011.583232. [DOI] [PubMed] [Google Scholar]
- 18.Cho SW, Kim I, Kim SH, Rhie JW, Choi CY, Kim BS. Enhancement of adipose tissue formation by implantation of adipogenic-differentiated preadipocytes. Biochem Biophys Res Commun. 2006;345:588–594. doi: 10.1016/j.bbrc.2006.04.089. [DOI] [PubMed] [Google Scholar]
- 19.Doucet C, Ernou I, Zhang Y, Llense JR, Begot L, Holy X, Lataillade JJ. Platelet lysates promote mesenchymal stem cell expansion: a safety substitute for animal serum in cell-based therapy applications. J Cell Physiol. 2005;205:228–236. doi: 10.1002/jcp.20391. [DOI] [PubMed] [Google Scholar]
- 20.Eppley BL, Woodell JE, Higgins J. Platelet quantification and growth factor analysis from platelet-rich plasma: implications for wound healing. Plast Reconstr Surg. 2004;114:1502–1508. doi: 10.1097/01.prs.0000138251.07040.51. [DOI] [PubMed] [Google Scholar]
- 21.Eppley BL, Pietrzak WS, Blanton M. Platelet-rich plasma: a review of biology and applications in plastic surgery. Plast Reconstr Surg. 2006;118:147e–159e. doi: 10.1097/01.prs.0000239606.92676.cf. [DOI] [PubMed] [Google Scholar]
- 22.Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA. Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med. 2009;37:2259–2272. doi: 10.1177/0363546509349921. [DOI] [PubMed] [Google Scholar]
- 23.Frechette JP, Martineau I, Gagnon G. Platelet-rich plasmas: growth factor content and roles in wound healing. J Dent Res. 2005;84:434–439. doi: 10.1177/154405910508400507. [DOI] [PubMed] [Google Scholar]
- 24.Gimble JM, Katz AJ, Bunnell BA. Adipose-derived stem cells for regenerative medicine. Circ Res. 2007;100:1249–1260. doi: 10.1161/01.RES.0000265074.83288.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gozuacik D, Kimchi A. DAPk protein family and cancer. Autophagy. 2006;2:74–79. doi: 10.4161/auto.2.2.2459. [DOI] [PubMed] [Google Scholar]
- 26.Jang CW, Chen CH, Chen CC, Chen JY, Su YH, Chen RH. TGF-b induces apoptosis through Smad-mediated expression of DAP-kinase. Nat Cell Biol. 2002;4:51–58. doi: 10.1038/ncb731. [DOI] [PubMed] [Google Scholar]
- 27.Kakudo N, Minakata T, Mitsui T, Kushida S, Notodihardjo FZ, Kusumoto K. Proliferation-promoting effect of platelet-rich plasma on human adipose-derived stem cells and human dermal fibroblasts. Plast Reconstr Surg. 2008;122:1352–1360. doi: 10.1097/PRS.0b013e3181882046. [DOI] [PubMed] [Google Scholar]
- 28.Kang YH, Jeon SH, Park JY, Chung JH, Choung YH, Choung HW, Kim ES, Choung PH. Platelet-rich fibrin is a Bioscaffold and reservoir of growth factors for tissue regeneration. Tissue Eng Part A. 2011;17:349–359. doi: 10.1089/ten.TEA.2010.0327. [DOI] [PubMed] [Google Scholar]
- 29.Kim H, Tu HC, Ren D, Takeuchi O, Jeffers JR, Zambetti GP, Hsieh JJ, Cheng EH. Stepwise activation of BAX and BAK by tBID, BIM, and PUMA initiates mitochondrial apoptosis. Mol Cell. 2009;36:487–499. doi: 10.1016/j.molcel.2009.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kimura Y, Ozeki M, Inamoto T, Tabata Y. Adipose tissue engineering based on human preadipocytes combined with gelatin microspheres containing basic fibroblast growth factor. Biomaterials. 2003;24:2513–2521. doi: 10.1016/s0142-9612(03)00049-8. [DOI] [PubMed] [Google Scholar]
- 31.Kuramochi D, Unoki H, Bujo H, Kubota Y, Jiang M, Rikihisa N, Udagawa A, Yoshimoto S, Ichinose M, Saito Y. Matrix metalloproteinase 2 improves the transplanted adipocyte survival in mice. Eur J Clin Invest. 2008;38:752–759. doi: 10.1111/j.1365-2362.2008.02023.x. [DOI] [PubMed] [Google Scholar]
- 32.Kurita M, Aiba-Kojima E, Shigeura T, Matsumoto D, Suga H, Inoue K, Eto H, Kato H, Aoi N, Yoshimura K. Differential effects of three preparations of human serum on expansion of various types of human cells. Plast Reconstr Surg. 2008;122:438–448. doi: 10.1097/PRS.0b013e31817d618d. [DOI] [PubMed] [Google Scholar]
- 33.Kuroda M, Aoyagi Y, Asada S, Bujo H, Tanaka S, Konno S, Tanio M, Ishii I, Machida K, Matsumoto F, Satoh K, Aso M, Saito Y. Ceiling culture-derived proliferative adipocytes are a possible delivery vehicle for enzyme replacement therapy in lecithin: cholesterol acyltransferase deficiency. Open Gene Ther J. 2011;4:1–10. [Google Scholar]
- 34.Liu Y, Kalen A, Risto O, Wahlstrom O. Fibroblast proliferation due to exposure to a platelet concentrate in vitro is pH dependent. Wound Repair Regen. 2002;10:336–340. doi: 10.1046/j.1524-475x.2002.10510.x. [DOI] [PubMed] [Google Scholar]
- 35.Lin Y, Hupp TR, Stevens C. Death-associated protein kinase (DAPK) and signal transduction: additional roles beyond cell death. FEBS J. 2010;277:48–57. doi: 10.1111/j.1742-4658.2009.07411.x. [DOI] [PubMed] [Google Scholar]
- 36.Lopez-Vidriero E, Goulding KA, Simon DA, Sanchez M, Johnson DH. The use of platelet-rich plasma in arthroscopy and sports medicine: optimizing the healing environment. Arthroscopy. 2010;26:269–278. doi: 10.1016/j.arthro.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 37.Lucarelli E, Beccheroni A, Donati D, Sangiorgi L, Cenacchi A, Del Vento AM, Meotti C, Bertoja AZ, Giardino R, Fornasari PM, Mercuri M, Picci P. Platelet-derived growth factors enhance proliferation of human stromal stem cells. Biomaterials. 2003;24:3095–3100. doi: 10.1016/s0142-9612(03)00114-5. [DOI] [PubMed] [Google Scholar]
- 38.Man D, Plosker H, Winland-Brown JE. The use of autologousplatelet-rich plasma (platelet gel) and autologous platelet-poor plasma (fibrin glue) in cosmetic surgery. Plast Reconstr Surg. 2001;107:229–237. doi: 10.1097/00006534-200101000-00037. discussion 238-9. [DOI] [PubMed] [Google Scholar]
- 39.Margolis DJ, Kantor J, Santanna J, Strom BL, Berlin JA. Effectiveness of platelet releasate for the treatment of diabetic neuropathic foot ulcers. Diabetes Care. 2001;24:483–488. doi: 10.2337/diacare.24.3.483. [DOI] [PubMed] [Google Scholar]
- 40.Martinez-Zapata MJ, Marti-Carvajal A, Sola I, Bolibar I, Angel Exposito J, Rodriguez L, Garcia J. Efficacy and safety of the use of autologous plasma rich in platelets for tissue regeneration: a systematic review. Transfusion. 2009;49:44–56. doi: 10.1111/j.1537-2995.2008.01945.x. [DOI] [PubMed] [Google Scholar]
- 41.Mebratu Y, Tesfaigzi Y. How ERK1/2 activation controls cell proliferation and cell death: Is subcellular localization the answer? Cell Cycle. 2009;8:1168–1175. doi: 10.4161/cc.8.8.8147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Muller AM, Davenport M, Verrier S, Droeser R, Alini M, Bocelli-Tyndall C, Schaefer DJ, Martin I, Scherberich A. Platelet lysate as a serum substitute for 2D static and 3D perfusion culture of stromal vascular fraction cells from human adipose tissue. Tissue Eng Part A. 2009;15:869–875. doi: 10.1089/ten.tea.2008.0498. [DOI] [PubMed] [Google Scholar]
- 43.Nakamura S, Ishihara M, Takikawa M, Murakami K, Kishimoto S, Yanagibayashi S, Kubo S, Yamamoto N, Kiyosawa T. Platelet-rich plasma (PRP) promotes survival of fat-grafts in rats. Ann Plast Surg. 2010;65:101–106. doi: 10.1097/SAP.0b013e3181b0273c. [DOI] [PubMed] [Google Scholar]
- 44.Ning H, Liu G, Lin G, Yang R, Lue TF, Lin CS. Fibroblast growth factor 2 promotes endothelial differentiation of adipose tissue-derived stem cells. J Sex Med. 2009;6:967–979. doi: 10.1111/j.1743-6109.2008.01172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Oh DS, Cheon YW, Jeon YR, Lew DH. Activated platelet-rich plasma improves fat graft survival in nude mice: a pilot study. Dermatol Surg. 2011;37:619–625. doi: 10.1111/j.1524-4725.2011.01953.x. [DOI] [PubMed] [Google Scholar]
- 46.Patrick CW., Jr Adipose tissue engineering: the future of breast and soft tissue reconstruction following tumor resection. Semin Surg Oncol. 2000;19:302–311. doi: 10.1002/1098-2388(200010/11)19:3<302::aid-ssu12>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 47.Patrick CW., Jr Tissue engineering strategies for adipose tissue repair. Anat Rec. 2001;263:361–366. doi: 10.1002/ar.1113. [DOI] [PubMed] [Google Scholar]
- 48.Pires Fraga MF, Nishio RT, Ishikawa RS, Perin LF, Helene A, Jr, Malheiros CA. Increased survival of free fat grafts with platelet-rich plasma in rabbits. J Plast Reconstr Aesthet Surg. 2010;63:e818–e822. doi: 10.1016/j.bjps.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 49.Ramesh S, Wildey GM, Howe PH. Transforming growth factor b (TGFb)-induced apoptosis: the rise & fall of Bim. Cell Cycle. 2009;8:11–17. doi: 10.4161/cc.8.1.7291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ramjaun AR, Tomlinson S, Eddaoudi A, Downward J. Upregulation of two BH3-only proteins, Bmf and Bim, during TGF beta-induced apoptosis. Oncogene. 2007;26:970–981. doi: 10.1038/sj.onc.1209852. [DOI] [PubMed] [Google Scholar]
- 51.Redler LH, Thompson SA, Hsu SH, Ahmad CS, Levine WN. Platelet-rich plasma therapy: a systematic literature review and evidence for clinical use. Phys Sportsmed. 2011;39:42–51. doi: 10.3810/psm.2011.02.1861. [DOI] [PubMed] [Google Scholar]
- 52.Ren D, Tu HC, Kim H, Wang GX, Bean GR, Takeuchi O, Jeffers JR, Zambetti GP, Hsieh JJ, Cheng EH. BID, BIM, and PUMA are essential for activation of the BAX- and BAK-dependent cell death program. Science. 2010;330:1390–1393. doi: 10.1126/science.1190217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sadati KS, Corrado AC, Alexander RW. Platelet-rich plasma (PRP) utilized to promote greater graft volume retention in autologous fat grafting. Am J Cosmet Surg. 2006;23:203–211. [Google Scholar]
- 54.Sclafani AP. Applications of platelet-rich fibrin matrix in facial plastic surgery. Facial Plast Surg. 2009;25:270–276. doi: 10.1055/s-0029-1242033. [DOI] [PubMed] [Google Scholar]
- 55.Stashower M, Smith K, Williams J, Skelton H. Stromal progenitor cells present within liposuction and reduction abdominoplasty fat for autologous transfer to aged skin. Dermatol Surg. 1999;25:945–949. doi: 10.1046/j.1524-4725.1999.99098.x. [DOI] [PubMed] [Google Scholar]
- 56.Sterodimas A, de Faria J, Nicaretta B, Pitanguy I. Tissue engineering with adipose-derived stem cells (ADSCs): current and future applications. J Plast Reconstr Aesthet Surg. 2010;63:1886–1892. doi: 10.1016/j.bjps.2009.10.028. [DOI] [PubMed] [Google Scholar]
- 57.Tobita M, Uysal AC, Ogawa R, Hyakusoku H, Mizuno H. Periodontal tissue regeneration with adipose-derived stem cells. Tissue Eng Part A. 2008;14:945–953. doi: 10.1089/ten.tea.2007.0048. [DOI] [PubMed] [Google Scholar]
- 58.Torio-Padron N, Borges J, Momeni A, Mueller MC, Tegtmeier FT, Stark GB. Implantation of VEGF transfected preadipocytes improves vascularization of fibrin implants on the cylinder chorioallantoic membrane (CAM) model. Minim Invasive Ther Allied Technol. 2007;16:155–162. doi: 10.1080/13645700701384116. [DOI] [PubMed] [Google Scholar]
- 59.Vogel JP, Szalay K, Geiger F, Kramer M, Richter W, Kasten P. Platelet-rich plasma improves expansion of human mesenchymal stem cells and retains differentiation capacity and in vivo bone formation in calcium phosphate ceramics. Platelets. 2006;17:462–469. doi: 10.1080/09537100600758867. [DOI] [PubMed] [Google Scholar]
- 60.Warne JP. Tumour necrosis factor a: a key regulator of adipose tissue mass. J Endocrinol. 2003;177:351–355. doi: 10.1677/joe.0.1770351. [DOI] [PubMed] [Google Scholar]
- 61.Welsh WJ. Autologous platelet gel: clinical function and usage in plastic surgery. Cosmet Dermatol. 2000;13:13–18. [Google Scholar]
- 62.Wildey GM, Patil S, Howe PH. Smad3 potentiates transforming growth factor b (TGFβ)-induced apoptosis and expression of the BH3-only protein Bim in WEHI 231 B lymphocytes. J Biol Chem. 2003;278:18069–18077. doi: 10.1074/jbc.M211958200. [DOI] [PubMed] [Google Scholar]
- 63.Wu W, Zhang J, Dong Q, Liu Y, Mao T, Chen F. Platelet-rich plasma - A promising cell carrier for micro-invasive articular cartilage repair. Med Hypotheses. 2009;72:455–457. doi: 10.1016/j.mehy.2008.11.032. [DOI] [PubMed] [Google Scholar]
- 64.Yamada Y, Nakamura S, Ito K, Sugito T, Yoshimi R, Nagasaka T, Ueda M. A feasibility of useful cell-based therapy by bone regeneration with deciduous tooth stem cells, dental pulp stem cells, or bone-marrow-derived mesenchymal stem cells for clinical study using tissue engineering technology. Tissue Eng Part A. 2010;16:1891–1900. doi: 10.1089/ten.TEA.2009.0732. [DOI] [PubMed] [Google Scholar]
- 65.Yamaguchi M, Matsumoto F, Bujo H, Shibasaki M, Takahashi K, Yoshimoto S, Ichinose M, Saito Y. Revascularization determines volume retention and gene expression by fat grafts in mice. Exp Biol Med (Maywood) 2005;230:742–748. doi: 10.1177/153537020523001007. [DOI] [PubMed] [Google Scholar]
- 66.Yoshimura K, Suga H, Eto H. Adipose-derived stem/progenitor cells: roles in adipose tissue remodeling and potential use for soft tissue augmentation. Regen Med. 2009;4:265–273. doi: 10.2217/17460751.4.2.265. [DOI] [PubMed] [Google Scholar]
- 67.Yu J, Zhang L, Chen A, Xiang G, Wang Y, Wu J, Mitchelson K, Cheng J, Zhou Y. Identification of the gene transcription and apoptosis mediated by TGF-β-Smad2/3-Smad4 signaling. J Cell Physiol. 2008;215:422–433. doi: 10.1002/jcp.21325. [DOI] [PubMed] [Google Scholar]
- 68.Yu W, Wang J, Yin J. Platelet-rich plasma: a promising product for treatment of peripheral nerve regeneration after nerve injury. Int J Neurosci. 2011;121:176–180. doi: 10.3109/00207454.2010.544432. [DOI] [PubMed] [Google Scholar]
- 69.Zuk PA, Zhu M, Mizuno H, Huang J, Futrell JW, Katz AJ, Benhaim P, Lorenz HP, Hedrick MH. Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng. 2001;7:211–228. doi: 10.1089/107632701300062859. [DOI] [PubMed] [Google Scholar]