Abstract
Caregivers' practices concerning oral rehydration of young children during diarrheal illness were investigated in a periurban community of low socioeconomic level in Lima, Peru. Data of 330 caregivers of children aged 6–36 months were analyzed; 72.7% of all caregivers would give commercially available oral rehydration solutions (ORSs). However, only 58.6% of those caregivers with children that had experienced diarrhea during the previous week stated that they had used commercially available ORSs, a significantly lower percentage. The main reason for not using commercially available ORSs was that caregivers did not know about them. Of all recipes caregivers provided for homemade ORS, none contained the recommended concentrations of sugar and salt. Educating caregivers about availability, benefits, and use of commercially available ORSs as well as correct preparation of homemade ORS is urgently needed.
Worldwide, approximately 10 million children under the age of 5 years die each year.1 Diarrheal diseases account for 17% of these deaths1 and approximately 12% of deaths among young children in Peru.2 From the very onset of illness, it is crucial to prevent dehydration, one of the main complications from which young children are dying. Since the introduction of oral rehydration solutions (ORSs) in the 1970s and 1980s, child mortality has dropped dramatically.3 In 2003, the World Health Organization (WHO) launched an improved low-osmolarity ORS for treating cholera and non-cholera diarrhea among all age groups.4,5 Low-osmolarity ORS reduces stool output, vomiting, and the need for unscheduled intravenous transfusions with a minimal risk of inducing symptomatic hyponatremia.6,7 Rehydration therapy with ORS is recommended in the integrated management of childhood illness (IMCI)8 and other guidelines.4,9 However, despite improvements made, in many developing countries, use of ORS is still far from satisfactory.3,10,11 Mothers and other caregivers play a key role in the effective prevention of dehydration, because they are the first ones to manage their child's illness. Therefore, as part of a larger study on child nutrition during diarrhea, we also collected data on caregivers' practices regarding oral rehydration of young children during diarrheal illness.
In December of 2009, main caregivers and the youngest child in the household were enrolled through a house by house survey in San Juan de Lurigancho, a periurban community of low socioeconomic level in Lima, Peru. Written informed consent was obtained from all caregivers. Data were collected by trained field workers using a semistructured questionnaire. Caregivers were asked which liquids from a panel of various liquids they had given their child for oral rehydration in the case that the child had experienced diarrhea during the previous week or at the day of the visit. Caregivers with a child that had not experienced diarrhea were asked which liquids they would have used for oral rehydration. Selecting more than one liquid was allowed. Proportions of variables among different groups of caregivers were compared using χ2 test. The study was reviewed and approved by the Institutional Ethics Committee of the Universidad Peruana Cayetano Heredia. Statistical analysis was conducted with Stata 10.0.
Data of 330 caregivers of children aged 6–36 months (mean age = 18.9 ± 8.6 months; range = 6.1–35.8 months) were analyzed; 49.7% (164/330) of children were female. All children had been introduced to solid food, and 62.4% (206/330) were still breastfed. In 81.8% (270/330) of the cases, the mother was the primary caregiver; 95.5% (315/330) of households had access to the public running water system inside their house, and 63.6% (210/330) of households did not store water. However, 24.9% (82/329) of households stored water in open containers, and 6.4% (21/329) of households stored water in closed containers; 17.6% (58/330) of caregivers stated that their child had experienced diarrhea during the previous 7 days. The mean age of these children was 17.5 ± 8.6 months (range = 6.3–35.8 months). While the diarrheal episodes of two children were still ongoing during the day of the study interview, the mean duration of the 56 completed episodes was 3.5 ± 2 days (range = 1–7 days).
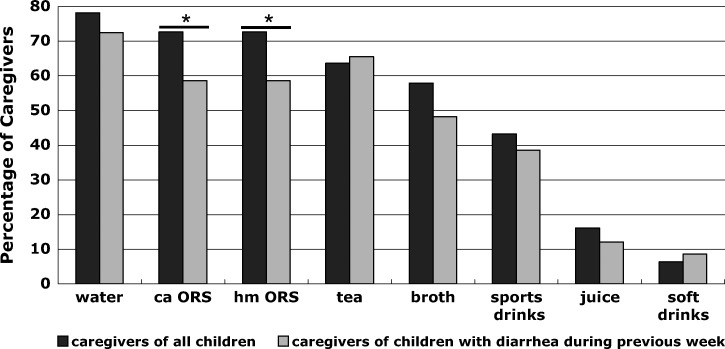
Figure 1 details the liquids that caregivers stated they would use for oral rehydration; 78.2% (258/330) of caregivers would offer water, and 43.2% (142/330) would administer rehydrating sports drinks. Additionally, 72.7% (240/330) of caregivers stated that they would give commercially available ORSs (e.g., WHO-recommended traditional oral rehydration salts that need to be diluted [local product is Salvadora] or preprepared electrolyte solutions that come in different flavors [local products are Frutiflex and Electoral]). The same percentage of caregivers stated that they would give homemade ORS.
Figure 1.
Liquids that caregivers would use to rehydrate their children during diarrheal illness. ca ORS = commercially available oral rehydration solutions; hm ORS = homemade oral rehydration solution; *P = 0.03.
When comparing practices of caregivers with children that had experienced diarrhea during the previous week with those practices of all caregivers or caregivers with children that had not previously experienced diarrhea, significant differences were found. Importantly, significantly fewer caregivers with children that had experienced diarrhea during the previous week stated to have used commercially available ORSs compared with all caregivers (58.6% [34/58] versus 72.7% [240/330], P = 0.03) or caregivers of children who had not experienced diarrhea (58.6% [34/58] versus 75.7% [206/272], P = 0.008). The same results apply to the use of homemade ORS. For all other liquids, differences were not significant. Because answers of caregivers with children that had experienced diarrhea during the previous week are most likely least biased by recall bias and social desirability, it seems reasonable to conclude that only slightly over one-half of the caregivers actually give commercially available ORSs during diarrheal illness.
As the main reason for not using commercially available ORSs, 50% (45/90) of the caregivers stated that they did not know about them. This finding is striking in a periurban community of the capital with easy access to healthcare facilities and pharmacies. It is likely that use of commercially available ORSs could be considerably increased if caregivers were better educated about where to obtain them, what their benefits are, how they are prepared, and that they can be given without prescription; 26.7% (24/90) of caregivers did not use commercially available ORSs, because it “tastes bad and the child rejects it”. This finding may be a potential reason for caregivers to use sports drinks for rehydration. However, sports drinks are not appropriate for young children, and they are relatively expensive. While low-osmolarity ORS has a total osmolarity of 245 mOsm/L,12 sports drinks have a higher osmolarity and osmolality. Gatorade has an osmolality of approximately 330 mOsm/kg,13,14 contains more carbohydrates, and contains less sodium and potassium.14 While electrolyte losses may, therefore, not be adequately compensated, the high-carbohydrate content, like in soft drinks, may worsen diarrhea because of osmotic effect. This problem might be easily solved if age-appropriate, preprepared, fruit-flavored commercially available ORSs were used. Additional reasons for not offering commercially available ORSs are shown in Table 1. There were no significant differences between caregivers with children that had experienced diarrhea during the previous week and caregivers with children that had not experienced diarrhea or all caregivers.
Table 1.
Reasons given by caregivers for why they would not use commercially available ORSs
| Percent | Frequency (N = 90) | |
|---|---|---|
| I don't know about them | 50 | 45 |
| They taste bad, and my child rejects them | 26.7 | 24 |
| Homemade ORS is better or already prepared | 5.6 | 5 |
| Nobody recommended them to me | 3.3 | 3 |
| I don't know where to buy them | 3.3 | 3 |
| I don't think that they help | 2.2 | 2 |
| I don't know how to prepare them | 1.1 | 1 |
When asked about how to prepare homemade ORS, 27% (89/330) of caregivers stated that they did not know. Of the 232 provided recipes, 94.8% (211/232) were rice-based. There is an ongoing debate on whether ORSs based on rice or other complex carbohydrates (starches) are advantageous over glucose-based solutions, such as WHO-recommended ORS. Homemade rice-based solutions have been associated with a lower risk of containing dangerously high concentrations of glucose and/or sodium.15 A recent metaanalysis indicated that rice-based ORSs might decrease the need for unscheduled intravenous transfusions and limit the duration of diarrhea in adults with cholera.16 However, it remained debatable whether this finding was clinically relevant, and the effect was not applicable to children. In addition, most studies compared starch-based with high- instead of the new low-osmolarity ORS.16 Additional research is needed to shed light on this topic.
In our study, it is worrying that the ingredients of the homemade recipes varied widely. None contained the recommended concentrations of sugar and salt in 1 L water (8 level teaspoons of sugar and ½ level teaspoon of salt)17: 80.6% of the given recipes did not contain sugar and salt or either one was missing, 14.2% did contain sugar and salt but the amounts were not specified, and 5.2% did contain sugar and salt but at the wrong amounts. This problem has also been reported in previous studies.11,17 Thus, caregivers' homemade solutions will not provide optimal rehydration during illness, and children will be at higher risk of developing electrolyte imbalances and dehydration, which may lead to death.
Our report has several limitations. We did not inquire in more detail about caregivers' knowledge about the different types of commercially available ORSs. Also, we did not investigate the use of zinc, which is recommended by the WHO to be used in conjunction with low-osmolarity ORS and decreases severity and duration of diarrhea.9 We also did not ask whom caregivers usually seek advice from regarding oral rehydration or whether caregivers with children that had suffered diarrhea during the previous week had consulted a physician. We, therefore, do not know whether caregivers use a certain liquid, because they feel it to be a valid option for oral rehydration or because somebody else (e.g., a physician or pharmacist) had recommended it. The same applies to the recipes for homemade ORS. These important questions will need to be addressed in future research. Of note, the results from this study cannot be generalized to other areas of Peru. However, it can be assumed that usage of commercially available ORSs is much more scarce in small towns and rural settings, where socioeconomic level is even lower and access to education, healthcare facilities, pharmacies, and products such as commercially available ORSs, is very limited.
In conclusion, a significant number of caregivers in this study setting are currently spending their limited resources on products inappropriate for rehydrating young children during diarrheal illness. At the same time, many caregivers are unaware of cheap and age-appropriate ORSs from which their children would benefit. Our findings suggest that there is an urgent need for educating caregivers about the availability, benefits, and use of age-appropriate commercially available ORSs as well as the correct preparation of homemade ORS.
ACKNOWLEDGMENTS
We would like to thank all caregivers and children who participated in this study. The authors thank Mery Ortega, Juanita Cuscano, and Gladys Andrade for their excellent work.
Footnotes
Financial support: B.P. received funding from the International Academy of Life Sciences. T.J.O. and J.R. were funded by the Agencia Española de Cooperación Internacional para el Desarrollo (AECID), Spain, Programa de Cooperación Interuniversitaria e Investigación Científica con Iberoamérica (D/019499/08 and D/024648/09). J.R. also has a Miguel Servet fellowship from the Fondo de Investigaciones Sanotarias, Spain (CP05/0130).
Authors' addresses: Birte Pantenburg, Leipzig University Medical Center, IFB Adiposity Diseases, Leipzig, Germany; Institute of Social Medicine, Occupational Health and Public Health, Public Health Research Unit, University of Leipzig, Leipzig, Germany; and Instituto de Medicina Tropical Alexander von Humboldt, Universidad Peruana Cayetano Heredia, Lima, Peru, E-mail: birte.pantenburg@medizin.uni-leipzig.de. Theresa J. Ochoa, Instituto de Medicina Tropical Alexander von Humboldt, Universidad Peruana Cayetano Heredia, Lima, Peru and School of Public Health, University of Texas, Houston, TX, E-mail: Theresa.J.Ochoa@uth.tmc.edu. Lucie Ecker, Instituto de Investigación Nutricional, Lima, Peru, E-mail: lecker@iin.sld.pe. Joaquim Ruiz, Centre de Recerca en Salut Internacional de Barcelona, Hospital Clinic/Institut d'Investigacions Biomèdiques August Pi i Sunyer, Universitat de Barcelona, Barcelona, Spain and CIBERESP, Barcelona, Spain, E-mail: joruiz@clinic.ub.es.
References
- 1.UNICEF State of the World's Children—Child Survival. 2008. http://www.unicef.org/sowc08/report/report.php Available at. Accessed June 2011.
- 2.WHO Mortality Country Fact Sheet. 2006. http://www.who.int/whosis/mort/profiles/mort_amro_per_peru.pdf Available at. Accessed June 2011.
- 3.Victora CG, Bryce J, Fontaine O, Monasch R. Reducing deaths from diarrhoea through oral rehydration therapy. Bull World Health Organ. 2000;78:1246–1255. [PMC free article] [PubMed] [Google Scholar]
- 4.WHO UNICEF Clinical Management of Acute Diarrhea. 2004. http://www.who.int/child_adolescent_health/documents/who_fch_cah_04_7/en/index.html Available at. Accessed June 2011.
- 5.WHO UNICEF Johns Hopkins School of Public Health USAID Implementing the New Recommendations on the Clinical Management of Diarrhoea—Guidelines for Policy Makers and Programme Managers. 2006. http://www.who.int/child_adolescent_health/documents/9241594217/en/index.html Available at. Accessed March 2011.
- 6.Alam NH, Yunus M, Faruque AS, Gyr N, Sattar S, Parvin S, Ahmed JU, Salam MA, Sack DA. Symptomatic hyponatremia during treatment of dehydrating diarrheal disease with reduced osmolarity oral rehydration solution. JAMA. 2006;296:567–573. doi: 10.1001/jama.296.5.567. [DOI] [PubMed] [Google Scholar]
- 7.Hahn S, Kim Y, Garner P. Reduced osmolarity oral rehydration solution for treating dehydration due to diarrhoea in children: systematic review. BMJ. 2001;323:81–85. doi: 10.1136/bmj.323.7304.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO IMCI Chart Booklet—Standard. 2008. http://www.who.int/child_adolescent_health/documents/IMCI_chartbooklet/en/index.html Available at. Accessed June 2011.
- 9.UNICEF WHO Diarrhoea: Why Children Are Still Dying and What Can Be Done. 2009. http://www.who.int/child_adolescent_health/documents/9789241598415/en/index.html Available at. Accessed June 2011.
- 10.Bachrach LR, Gardner JM. Caregiver knowledge, attitudes, and practices regarding childhood diarrhea and dehydration in Kingston, Jamaica. Rev Panam Salud Publica. 2002;12:37–44. doi: 10.1590/s1020-49892002000700006. [DOI] [PubMed] [Google Scholar]
- 11.McLennan JD. Home management of childhood diarrhoea in a poor periurban community in Dominican Republic. J Health Popul Nutr. 2002;20:245–254. [PubMed] [Google Scholar]
- 12.WHO UNICEF Oral Rehydration Salts—Production of the New ORS. 2006. http://www.who.int/child_adolescent_health/documents/fch_cah_06_1/en/ Available at. Accessed June 2011.
- 13.Mettler S, Rusch C, Colombani PC. Osmolality and pH of sport and other drinks available in Switzerland. Schweiz Z Sportmed. 2006;54:92–95. [Google Scholar]
- 14.Shapiro SD, Wallace KH, Roth TS. Rehydration and refeeding after diarrheal illness. Say no to sports drinks and BRAT. Adv NPs PAs. 2010;1:35–40. [PubMed] [Google Scholar]
- 15.Molla AM, Bari A, Greenough WB, 3rd, Molla AM, Budhiraja P, Sharma PN. Bangladeshi rural mothers prepare safer rice oral rehydration solution. Acta Paediatr. 2000;89:791–794. [PubMed] [Google Scholar]
- 16.Gregorio GV, Gonzales ML, Dans LF, Martinez EG. Polymer-based oral rehydration solution for treating acute watery diarrhoea. Cochrane Database Syst Rev. 2009;2:CD006519. doi: 10.1002/14651858.CD006519.pub2. [DOI] [PubMed] [Google Scholar]
- 17.Dippenaar H, Joubert G, Nel R, Bantobetse ML, Opawole AA, Roshen KS. Homemade sugar-salt solution for oral rehydration: knowledge of mothers and caregivers. S Afr Fam Pract (2004) 2005;47:51–53. [Google Scholar]